Abstract
Bone marrow derived myeloid cells progressively accumulate in tumors, where they establish an inflammatory microenvironment that is favorable for tumor growth and spread. These cells are comprised primarily of monocytic and granulocytic myeloid derived suppressor cells (MDSCs) or tumor-associated macrophages (TAMs), which are generally associated with a poor clinical outcome. MDSCs and TAMs promote tumor progression by stimulating immunosuppression, neovascularization, metastasis and resistance to anti-cancer therapy. Strategies to target the tumor-promoting functions of myeloid cells could provide substantial therapeutic benefit to cancer patients.
Keywords: Macrophage, Myeloid derived suppressor cells, Tumor angiogenesis, Tumor microenvironment, Tumor inflammation, Cancer
Inflammation and cancer
Chronic inflammation is a causative or exacerbating factor in a host of complex human diseases, including solid tumors and leukemias/lymphomas, chronic bacterial and parasitic infections, rheumatoid arthritis, Crohn’s disease, asthma and central nervous system (CNS) disorders such as Alzheimers’ disease, Parkinson’s disease and multiple sclerosis. In each of these diseases, affected tissues are heavily invested with inflammatory myeloid cells, which include resident or bone marrow derived macrophages [1-4]. In addition, all tumors are heavily invested with myeloid cells, including tumor-associated macrophages (TAMs) [5,6]. Myeloid cells stimulate cancer initiation, malignant progression, metastasis and resistance to therapy [7]. Thus, targeting molecular pathways regulating the tumor promoting functions of myeloid cells holds promise for solid tumor therapy.
Macrophages in normal and tumor biology
Macrophages are myeloid lineage cells that arise from bone marrow derived monocytic progenitor cells that differentiate into tissue macrophages, antigen-presenting dendritic cells and bone resorbing osteoclasts [8,9]. Macrophages can be activated in response to environmental signals, including microbial products and cytokines. Activated macrophages can be loosely divided into M1 (classically activated) and M2 (alternatively activated) phenotype [1]. Classical activation occurs in response to bacterial moieties such as lipopolysacharide (LPS) and immune stimuli such as interferon γ (IFNγ). M1 macrophages mediate resistance against intracellular parasites and tumors and elicit tissue disruptive reactions by secreting tumoricidal agents such as tumor necrosis factor α (TNF-α), interleukin-12 (IL-12), and reactive nitrogen and oxygen intermediates (RNI, ROI). In addition, M1 macrophages promote T-helper-l (Thl) responses. In general, M2 macrophages exhibit an immunosuppressive phenotype and release factors that include IL-l0 and Arginase-1 [10,11].
M2 macrophages are the predominant type of macrophage found in tumors [6]. M1 macrophages are abundant at sites of chronic inflammation and in early tumors [12,13], but then switch to an M2-like phenotype during tumor progression [14-16]. Although IL-4, IFNγ, and several other tumor-derived cytokines and growth factors modulate macrophage phenotypes in vitro and in vivo[1,17], the molecular mechanisms that promote M1 or M2 TAM subsets within the tumor microenvironment are incompletely understood.
Although TAMs can convert into M1 or M2 phenotypes, and thereby execute almost diametrically opposed biological functions, unique cell surface markers that distinguish the two TAM phenotypes remain elusive. Flow cytometric analysis does indicate that M1-like TAMs express an F4/80 + CD11c+MRClow phenotype, while M2-like TAMs express an F4/80 + CD11cnegMRChigh phenotype [18].
Myeloid derived suppressor cells
Myeloid derived suppressor cells (MDSC) are CD11b+Gr1+ immunosuppressive, incompletely differentiated myeloid progenitor cells originally identified in tumor bearing mice [19]. MDSC accumulate in the blood, spleen, lymph nodes, bone marrow and tumors of tumor-bearing animals and patients [20-24]. MDSCs inhibit innate and adaptive immunity, promoting tumor immune escape. MDSC are a heterogeneous population of cells that lack the expression of cell surface markers that are specifically expressed on macrophages or DC [25]. In mice, MDSC are uniformly characterized by the expression of Gr1 and CD11b. Gr1 includes the macrophage and neutrophil markers Ly6C and Ly6G, respectively, whereas CD11b (also known as integrin αM) is characteristic for the myeloid- cell linage. In recent years, several other surface molecules have been used to identify additional subset of immunosuppressive MDSC, including CD80 [26], CD115 (also known as macrophage colony stimulating factor (M-CSF) receptor) and CD124 (IL-4 receptor alpha chain, IL-4Rα) [27]. In addition, nuclear morphology has also been used to characterize mouse MDSC. Mononuclear CDllb+Gr1midLy6G+/−Ly6ChighCD49d+ cells are considered “monocytic” whereas polymorphonuclear CDllb+Gr1highLy6G+Ly6CnegCD49dneg MDSC are considered granulocytic [28-30]. Subpopulations of MDSC can give rise to CD11b+Gr1lowF4/80+MHCII+ macrophages with potent immunosuppressive properties, underscoring the potential biological continuum of immature myeloid cells, monocytes, and macrophages [20,25,31].
In patients with glioblastoma, breast cancer, colon cancer, lung cancer or kidney cancer, MDSC have been defined as LinnegCDllb+HLA-DRnegCD33+ cells that express the common myeloid marker CD33 but lack mature monocyte and lymphoid cell linage markers (Linneg = CD14neg, CD3neg, CD19neg) and lack the MHC class II molecule HLA-DR [32]. In patients with renal cancer, polymorphonuelcar MDSC have been shown to express CD11b+ CD14negCD15+CD66b+ VEGFR1+[33] whereas in patients with melanoma, prostate cancer, hepatocellular carcinoma or head and neck cancer, immunosuppressive monocytic CD11b+ CD14+ HLA-DRlow/neg MDSC were found [21,34-36]. These cells are associated with increased tumor burden and poor prognosis in patients with breast and colorectal cancer [24,37].
Mechanisms of myeloid cell recruitment
Immune cell trafficking in vivo is regulated by chemokines and cytokines, and by members of the integrin, immunoglobulin and selectin adhesion molecule families [38,39]. A diverse array of chemotactic factors that are expressed either by tumor cells or tumor infiltrating immune cells stimulate myeloid cell recruitment into tumors. These factors include CCL2 (MIP-1), CCL5 (RANTES), CCL12, IL-8, IL-lβ, CXCL12 (SDF-1α), and CXCL5 (ENA-78) [40-44].
While malignant tumor cells express myeloid cell chemoattractants, tumor infiltrating immune cells also express a variety of chemotactic factors, which can further foster myeloid cell recruitment and accumulation in the tumor microenvironment. For example, myeloid cell derived IL-1β stimulates myeloid cell recruitment in vivo and pharmacological inhibition of IL-1β reduced the infiltration of myeloid cells into the tumor microenvironment and inhibited tumor progression in a lung cancer tumor model [42]. Tumor derived factors, such as G-CSF, can also stimulate long-range effects in the bone marrow, leading to myeloid cell expression of Bv8, a factor that stimulates myelopoiesis and mobilization [45,46].
Recent efforts have also been made to identify tumor-derived factors that specifically recruit myeloid cells in response to chemotherapeutic treatments. CCL2 and CCL12 were highly upregulated in doxorubicin treated MMTV-PyMT animals; genetic depletion of CCR2 or pharmacological blockade of GPCR-mediated signaling with pertussis toxin, reduced myeloid cell recruitment in response to chemotherapy and increased the sensitivity of tumors [41]. Paclitaxel treatment of MMTV-PyMT animals induced colony stimulating factor 1 (CSF-l) and IL-34 expression, which together stimulated CSF1 receptor (CSF1R)-dependent macrophage infiltration [47]. Blockade of CSF1R signaling in combination with paclitaxel improved survival of mammary tumor-bearing mice. Myeloid cells thus play a central role in resistance to chemotherapy.
Roles of integrins in myeloid cell recruitment
The integrin adhesion molecule family is an extensive group of structurally related receptors for extracellular matrix (ECM) proteins and immunoglobulin superfamily molecules. Integrins are divalent cation-dependent heterodimeric membrane glycoproteins comprised of non-covalently associated α and β subunits that promote cell attachment and migration on the surrounding extracellular matrix. Eighteen α and eight β subunits can associate to form twenty-four unique integrin heterodimers [48,49]. Integrins on bone marrow-derived immune cells promote tumor inflammation by facilitating myeloid cell trafficking to the tumor microenvironment [42,50,51]. Myeloid cells express a number of functional integrins, including α2β1, α4β1, α5β1, αvβ3, αvβ5, αMβ2 (CD11b) and αXβ2 (CD11c) [52-54]. Recent studies from our laboratory indicate that integrin α4β1, a receptor for vascular cell adhesion molecule 1 (VCAM-1) and CS-l fibronectin, selectively promotes the homing of myeloid cells to the tumor microenvironment [42,55]. Human and murine myeloid cells adhered to endothelial cells in vitro and to tumor endothelium in vivo via integrin α4β1. Genetic and pharmacological blockade of integrin α4βl significantly suppressed tumor inflammation, growth and metastasis. In addition, combination of anti-integrin α4 antibody and chemotherapeutic agents markedly reduced tumor burden compared to chemotherapeutic treatment alone [42]. Thus, these studies indicate that suppression of myeloid cell trafficking to the tumor microenvironment with integrin α4βl antagonists could be a useful adjuvant approach in cancer therapy.
Signaling molecules in myeloid cell recruitment
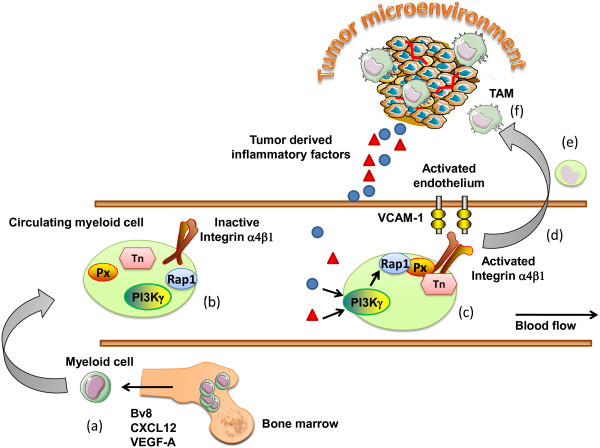
Integrins are expressed in an inactive confirmation on circulating immune cells [49,56,57]. Inflammatory factors released by tissues activate G protein coupled receptors (GPCRs), receptor tyrosine kinases (RTKs) or Toll-like receptor/interleukin1 receptor family members (TLR/IL1Rs), which initiate myeloid cell recruitment during inflammation [50]. We recently demonstrated that PI3Kγ promotes inflammation downstream of diverse receptors by stimulating inside-out activation of integrin, α4β1, granulocytic and monocytic cell adhesion to endothelium and invasion into tumors [51]. Pharmacological or genetic blockade of PI3Kγ suppressed adhesion and recruitment of monocytic and granulocytic cells into inflamed tissues. These findings suggested that targeting the trafficking of myeloid cells into tumors might provide significant benefit in the treatment of a wide variety of diseases. While all the steps in integrin activation have yet to be deciphered, PI3Kγ activates the small GTPase, Rap1, which promotes talin binding to integrin β1 − subunit cytoplasmic domains, thereby inducing a shift in the conformation of the extracellular domain of the integrin and increasing ligand binding affinity [58,59]. In addition, paxillin binding to the α4 cytoplasmic tail enhances integrin α4 activation, as disruption of the paxillin binding site in the integrin α4 cytoplasmic tail partially prevents talin binding and inhibits adhesion under flow in vitro and in vivo (Figure 1) [42,60,61].
Figure 1 .
Mechanisms regulating the recruitment of myeloid cells to the tumor microenvironment. (a) Myeloid cells are activated and mobilized from the bone marrow in response to tumor derived factor such as Bv8, SDF-1α, GM-CSF. (b) Circulating myeloid cells express integrin adhesion molecules in an inactive confirmation, with low binding affinity. (c) In response to diverse chemotactic factors released from the tumor microenvironment, myeloid PI3Kγ activates the adhesion molecule integrin α4β1. (d) Myeloid cells are now able to bind to the activated tumor endothelium expressing the integrin α4β1 ligand VCAM-1. (e) Myeloid cells extravasate from the blood stream and migrate toward the tumor microenvironment, (f) where they differentiate in response to the cytokines/chemokine milieu to tumor associated macrophages. Px, Paxillin; Tn, Talin; TAM, tumor associated macrophages.
Roles of myeloid cells in tumor progression
Angiogenesis
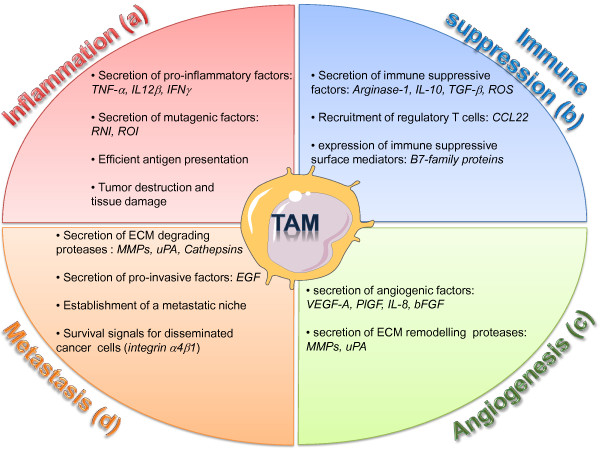
MDSC and TAMs play major roles in vascular remodeling during tumor progression. MDSC and TAMs release a number of potent pro-angiogenic cytokines, such as VEGF-A, VEGF-C, TNF-α, Placenta derived growth factor β (PlGF), chemokines (CXCL12, CXCL8), and bFGF [62,63]. TAMs also express a broad array of proteases known to play roles in the angiogenic process, including urokinase-type plasminogen activator (uPA), the matrix metalloproteinases MMP-2, MMP-7, MMP-9 and MMP-12 and elastase [64,65]. uPA and MMP support angiogenesis by remodeling and breaking down the extracellular matrix (ECM). Degradation of ECM leads to the mobilization of growth factors and facilitates the migration of vascular cells into new environments [66,67] (Figure 2c).
Figure 2 .
Diverse roles of TAMs in the tumor microenvironment. TAMs are critical regulator of tumor initiation and progression. (a) Inflammatory TAMs can initiate a chronic smoldering inflammation that creates a mutagenic and growth-promoting environment. (b) In established tumors, immune suppressive TAMs secrete factors which inhibit the activation of cytotoxic T cells and promotes the recruitment of regulatory T cells. (c) Pro-angiogenic TAMs stimulate the formation of new blood vessels by secreting angiogenic growth factors and ECM remodeling proteases. (d) TAMs support invasion and metastasis of malignant cells by destructing the ECM though proteases, by secreting invasion-inducing factors, and by supporting the establishment of a pro-metastatic niche. ROI, reactive oxygen intermediates; RNI, reactive nitrogen intermediates; ECM, extracellular matrix.
Immune suppression
MDSC and TAMs are both major regulators of the immune response [2].
MDSC suppress T cell proliferation in part by expression of Arginase-1 [68]. L-arginine plays a critical role in the inhibition of cytotoxic T cells by MDSC. Arginase converts L-arginine into L-ornithine and urea, thereby depleting L-arginine from the microenvironment and preventing iNOS from converting L-arginine to NO, an immunostimulant [69]. Depletion of arginine by Arginase I inhibits expression of the T-Cell Receptor (TCR) CD3zeta chain and T cell proliferation [70]. MDSC produced ROS also inhibits CD8+ T cell function by catalyzing the nitration of the TCR and thereby preventing T cell peptide-MHC interactions [71]. Moreover, several known tumor-derived factors, such as TGF-β, IL-3, IL-6, IL-l0, Platelet derived growth factor β, and granulocyte macrophage colony stimulating factor (GM-CSF) can induce the production of ROS by MDSC [8,72].
Beside inhibition of T cell activation, MDSC secrete immune suppressive cytokine with can inhibit immune surveillance. Secretion of the type 2 cytokine IL-l0 down-regulates the production of the type 1 cytokine IL-12 in macrophages. In addition, IL-l0 and VEGF-A inhibit the maturation of DC [68]. TGF-β has also been associated with MDSC immune suppressive functions. In fibrosarcoma and colon carcinoma tumor models, MDSC produced TGF-β in response to IL-13 stimulation, which resulted in decreased tumor immunosurveillance of cytotoxic T –cells [73,74].
Myeloid cells in relapse or resistance to therapy
CD11b+Grl+ myeloid cells and TAMs play key roles in regulating the response of tumors to therapy, including anti-angiogenic and chemotherapeutic treatments. Accumulation of CD11b+Grl+ cells in tumors inhibits responsiveness to anti-angiogenic blockade by anti-VEGF-A antibodies [75]. Bv8, a protein expressed by myeloid cells in the bone marrow, stimulated the expansion and mobilization of CD11b+Grl+ cells in the bone marrow and mediated resistance to anti-VEGFA therapy [76,77].
Macrophages and anti-cancer therapy
The significance of the vascular remodeling functions of TAMs in cancer therapy has recently emphasized by several studies. Tumor blood vessels are mostly disorganized and immature compared to non-pathological angiogenesis. Blood vessels are more torturous, with reduced pericyte coverage, and reduced erratic blood flow [78]. A recent studied showed that blood vessel normalization can be modulated by targeting the angiopoietin/Tie2 pathway. Interestingly, the angiopoietin receptor Tie2 is not only expressed on endothelial cells, but also a subpopulation of tumor infiltrating macrophages with vascular remodeling function. Targeting the Angiopoietin/Tie2 pathway by a fully humanized anti-ANG2 monoclonal antibody inhibited tumor angiongenesis, growth, and metastasis, and disabled the pro-angiogenic functions of tumor infiltrating macrophages, thus impeding the emergence of evasive resistance to anti-angiogenic therapy [79]. Genetic depletion of VEGF-A gene under the macrophage specific promoter LysM-Cre attenuates tumor angiogenesis and results in a morphologically more normal vasculature___. Tumors with normalized blood vessels showed increased sensitivity to chemotherapeutic treatment [80]. Similarly, histidine-rich glycoprotein HRG, a host-produced protein deposited in tumor stroma, can induce a reprogramming of the vascular remodeling functions of TAMs, resulting in vascular normalization and improved responses to chemotherapy [18]. In another report, blockade of CSF-1 signaling in a breast cancer tumor model, resulted in reduced numbers of intra-tumoral macrophage, normalized tumor vasculature, and increased responses to chemotherapy [47]. Notably, beside vascular normalization, both studies also showed enhanced anti-tumor immune responses, thus indicating the complexity of crosstalk’s by diverse cell types within the tumor microenvironment, and the power of targeting one subtype to thereby subvert biological functions of other stromal cells.
A mechanism independent of vascular normalization was proposed by Johanna Joyce and colleagues. The authors identified that TAMs secreted factors that protect tumors from chemotherapy. In the PyMT breast cancer models, tumors treated with the chemotoxic agent paclitaxel had more TAMs than control tumors. These TAMs expressed increased levels of proteases, specifically cysteine cathepsin B. Expression of cathepsin B was suggested to be necessary to protect cancer cells in vitro and in vivo from several chemotoxic agents, including paclitaxel, etoposide, and doxorubicin [81].
Conclusions
Myeloid cells promote tumor progression and alter the response of tumors to anti-cancer therapies. Identification and targeting of myeloid cells represents an emerging and attractive therapeutic approach to fight cancer. Therapeutic strategies targeting TAMs include inhibition of their recruitment to the tumor microenvironment, blockade of their pro-tumoral effector functions, and reprogramming of macrophage/MDSC polarization and thus restoring their anti-tumorigenic functions. Targeting myeloid cell recruitment can reduce tumor progression and improve the efficacy of chemotherapeutic treatments [41,51]. Similarly, partial reprogramming of macrophage polarization towards an M1-like phenotype enhances chemotherapy and reduces tumor growth [18,82]. Importantly, some of the anti-tumorigenic functions of macrophages critically depend on the presence of cytotoxic CD8+ T-cells, which are part of the adaptive immune system [47,83].
Competing interests
Both authors declare that they have no competing interests.
Authors’ contribution
MCS and JVS reviewed the literature on myeloid cells in tumor inflammation, prepared the manuscript, and drew the illustrations. All authors read and approved the final manuscript.
Contributor Information
Michael C Schmid, Email: mschmid@ucsd.edu.
Judith A Varner, Email: jvarner@ucsd.edu.
References
- Biswas SK, Mantovani A. Macrophage plasticity and interaction with lymphocyte subsets: cancer as a paradigm. Nat Immunol. 2010;11(10):889–896. doi: 10.1038/ni.1937. [DOI] [PubMed] [Google Scholar]
- Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer. Cell. 2010;140(6):883–899. doi: 10.1016/j.cell.2010.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray PJ, Wynn TA. Protective and pathogenic functions of macrophage subsets. Nat Rev Immunol. 2011;11(11):723–737. doi: 10.1038/nri3073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wynn TA, Barron L. Macrophages: master regulators of inflammation and fibrosis. Semin Liver Dis. 2010;30(3):245–257. doi: 10.1055/s-0030-1255354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mantovani A. et al. Cancer-related inflammation. Nature. 2008;454(7203):436–444. doi: 10.1038/nature07205. [DOI] [PubMed] [Google Scholar]
- Mantovani A, Sica A. Macrophages, innate immunity and cancer: balance, tolerance, and diversity. Curr Opin Immunol. 2010;22(2):231–237. doi: 10.1016/j.coi.2010.01.009. [DOI] [PubMed] [Google Scholar]
- Hanahan D, Coussens LM. Accessories to the crime: functions of cells recruited to the tumor microenvironment. Cancer Cell. 2012;21(3):309–322. doi: 10.1016/j.ccr.2012.02.022. [DOI] [PubMed] [Google Scholar]
- Gabrilovich DI, Ostrand-Rosenberg S, Bronte V. Coordinated regulation of myeloid cells by tumours. Nat Rev Immunol. 2012;12(4):253–268. doi: 10.1038/nri3175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geissmann F. et al. Development of monocytes, macrophages, and dendritic cells. Science. 2010;327(5966):656–661. doi: 10.1126/science.1178331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karp CL, Murray PJ. Non-canonical alternatives: what a macrophage is 4. J Exp Med. 2012;209(3):427–431. doi: 10.1084/jem.20120295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon S, Martinez FO. Alternative activation of macrophages: mechanism and functions. Immunity. 2010;32(5):593–604. doi: 10.1016/j.immuni.2010.05.007. [DOI] [PubMed] [Google Scholar]
- Greten FR. et al. IKKbeta links inflammation and tumorigenesis in a mouse model of colitis-associated cancer. Cell. 2004;118(3):285–296. doi: 10.1016/j.cell.2004.07.013. [DOI] [PubMed] [Google Scholar]
- Karin M, Greten FR. NF-kappaB: linking inflammation and immunity to cancer development and progression. Nat Rev Immunol. 2005;5(10):749–759. doi: 10.1038/nri1703. [DOI] [PubMed] [Google Scholar]
- Lin EY. et al. Macrophages regulate the angiogenic switch in a mouse model of breast cancer. Cancer Res. 2006;66(23):11238–11246. doi: 10.1158/0008-5472.CAN-06-1278. [DOI] [PubMed] [Google Scholar]
- Qian B. et al. A distinct macrophage population mediates metastatic breast cancer cell extravasation, establishment and growth. PLoS One. 2009;4(8):e6562. doi: 10.1371/journal.pone.0006562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruffell B, Affara NI, Coussens LM. Differential macrophage programming in the tumor microenvironment. Trends Immunol. 2012;33(3):119–126. doi: 10.1016/j.it.2011.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qian BZ, Pollard JW. Macrophage diversity enhances tumor progression and metastasis. Cell. 2010;141(1):39–51. doi: 10.1016/j.cell.2010.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rolny C. et al. HRG inhibits tumor growth and metastasis by inducing macrophage polarization and vessel normalization through downregulation of PlGF. Cancer Cell. 2011;19(1):31–44. doi: 10.1016/j.ccr.2010.11.009. [DOI] [PubMed] [Google Scholar]
- Peranzoni E. et al. Myeloid-derived suppressor cell heterogeneity and subset definition. Curr Opin Immunol. 2010;22(2):238–244. doi: 10.1016/j.coi.2010.01.021. [DOI] [PubMed] [Google Scholar]
- Bronte V. et al. Identification of a CD11b(+)/Gr-1(+)/CD31(+) myeloid progenitor capable of activating or suppressing CD8(+) T cells. Blood. 2000;96(12):3838–3846. [PMC free article] [PubMed] [Google Scholar]
- Mandruzzato S. et al. IL4Ralpha + myeloid-derived suppressor cell expansion in cancer patients. J Immunol. 2009;182(10):6562–6568. doi: 10.4049/jimmunol.0803831. [DOI] [PubMed] [Google Scholar]
- Corzo CA. et al. HIF-1alpha regulates function and differentiation of myeloid-derived suppressor cells in the tumor microenvironment. J Exp Med. 2010;207(11):2439–2453. doi: 10.1084/jem.20100587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corzo CA. et al. Mechanism regulating reactive oxygen species in tumor-induced myeloid-derived suppressor cells. J Immunol. 2009;182(9):5693–5701. doi: 10.4049/jimmunol.0900092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diaz-Montero CM. et al. Increased circulating myeloid-derived suppressor cells correlate with clinical cancer stage, metastatic tumor burden, and doxorubicin-cyclophosphamide chemotherapy. Cancer Immunol Immunother. 2009;58(1):49–59. doi: 10.1007/s00262-008-0523-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Movahedi K. et al. Identification of discrete tumor-induced myeloid-derived suppressor cell subpopulations with distinct T cell-suppressive activity. Blood. 2008;111(8):4233–4244. doi: 10.1182/blood-2007-07-099226. [DOI] [PubMed] [Google Scholar]
- Yang R. et al. CD80 in immune suppression by mouse ovarian carcinoma-associated Gr-1 + CD11b + myeloid cells. Cancer Res. 2006;66(13):6807–6815. doi: 10.1158/0008-5472.CAN-05-3755. [DOI] [PubMed] [Google Scholar]
- Gallina G. et al. Tumors induce a subset of inflammatory monocytes with immunosuppressive activity on CD8+ T cells. J Clin Invest. 2006;116(10):2777–2790. doi: 10.1172/JCI28828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sawanobori Y. et al. Chemokine-mediated rapid turnover of myeloid-derived suppressor cells in tumor-bearing mice. Blood. 2008;111(12):5457–5466. doi: 10.1182/blood-2008-01-136895. [DOI] [PubMed] [Google Scholar]
- Youn JI. et al. Subsets of myeloid-derived suppressor cells in tumor-bearing mice. J Immunol. 2008;181(8):5791–5802. doi: 10.4049/jimmunol.181.8.5791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haile LA. et al. CD49d is a new marker for distinct myeloid-derived suppressor cell subpopulations in mice. J Immunol. 2010;185(1):203–210. doi: 10.4049/jimmunol.0903573. [DOI] [PubMed] [Google Scholar]
- Van Ginderachter JA. et al. Peroxisome proliferator-activated receptor gamma (PPARgamma) ligands reverse CTL suppression by alternatively activated (M2) macrophages in cancer. Blood. 2006;108(2):525–535. doi: 10.1182/blood-2005-09-3777. [DOI] [PubMed] [Google Scholar]
- Almand B. et al. Increased production of immature myeloid cells in cancer patients: a mechanism of immunosuppression in cancer. J Immunol. 2001;166(1):678–689. doi: 10.4049/jimmunol.166.1.678. [DOI] [PubMed] [Google Scholar]
- Ochoa AC. et al. Arginase, prostaglandins, and myeloid-derived suppressor cells in renal cell carcinoma. Clin Cancer Res. 2007;13(2 Pt 2):721s–726s. doi: 10.1158/1078-0432.CCR-06-2197. [DOI] [PubMed] [Google Scholar]
- Filipazzi P. et al. Identification of a new subset of myeloid suppressor cells in peripheral blood of melanoma patients with modulation by a granulocyte-macrophage colony-stimulation factor-based antitumor vaccine. J Clin Oncol. 2007;25(18):2546–2553. doi: 10.1200/JCO.2006.08.5829. [DOI] [PubMed] [Google Scholar]
- Hoechst B. et al. A new population of myeloid-derived suppressor cells in hepatocellular carcinoma patients induces CD4(+)CD25(+)Foxp3(+) T cells. Gastroenterology. 2008;135(1):234–243. doi: 10.1053/j.gastro.2008.03.020. [DOI] [PubMed] [Google Scholar]
- Vuk-Pavlovic S. et al. Immunosuppressive CD14 + HLA-DRlow/- monocytes in prostate cancer. Prostate. 2010;70(4):443–455. doi: 10.1002/pros.21078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solito S. et al. A human promyelocytic-like population is responsible for the immune suppression mediated by myeloid-derived suppressor cells. Blood. 2011;118(8):2254–2265. doi: 10.1182/blood-2010-12-325753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luster AD, Alon R, von Andrian UH. Immune cell migration in inflammation: present and future therapeutic targets. Nat Immunol. 2005;6(12):1182–1190. doi: 10.1038/ni1275. [DOI] [PubMed] [Google Scholar]
- Weber C, Koenen RR. Fine-tuning leukocyte responses: towards a chemokine’interactome’. Trends Immunol. 2006;27(6):268–273. doi: 10.1016/j.it.2006.04.002. [DOI] [PubMed] [Google Scholar]
- Du R. et al. HIF1alpha induces the recruitment of bone marrow-derived vascular modulatory cells to regulate tumor angiogenesis and invasion. Cancer Cell. 2008;13(3):206–220. doi: 10.1016/j.ccr.2008.01.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakasone ES. et al. Imaging tumor-stroma interactions during chemotherapy reveals contributions of the microenvironment to resistance. Cancer Cell. 2012;21(4):488–503. doi: 10.1016/j.ccr.2012.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmid MC. et al. Combined blockade of integrin-alpha4beta1 plus cytokines SDF-1alpha or IL-1beta potently inhibits tumor inflammation and growth. Cancer Res. 2011;71(22):6965–6975. doi: 10.1158/0008-5472.CAN-11-0588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang L. et al. Abrogation of TGF beta signaling in mammary carcinomas recruits Gr-1 + CD11b + myeloid cells that promote metastasis. Cancer Cell. 2008;13(1):23–35. doi: 10.1016/j.ccr.2007.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang XQ. et al. The high level of RANTES in the ectopic milieu recruits macrophages and induces their tolerance in progression of endometriosis. J Mol Endocrinol. 2010;45(5):291–299. doi: 10.1677/JME-09-0177. [DOI] [PubMed] [Google Scholar]
- Shojaei F. et al. G-CSF-initiated myeloid cell mobilization and angiogenesis mediate tumor refractoriness to anti-VEGF therapy in mouse models. Proc Natl Acad Sci U S A. 2009;106(16):6742–6747. doi: 10.1073/pnas.0902280106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shojaei F. et al. Bv8 regulates myeloid-cell-dependent tumour angiogenesis. Nature. 2007;450(7171):825–831. doi: 10.1038/nature06348. [DOI] [PubMed] [Google Scholar]
- Denardo DG. et al. Leukocyte Complexity Predicts Breast Cancer Survival and Functionally Regulates Response to Chemotherapy. Cancer Discov. 2011;1:54–67. doi: 10.1158/2159-8274.CD-10-0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimizu Y, Rose DM, Ginsberg MH. Integrins in the immune system. Adv Immunol. 1999;72:325–380. doi: 10.1016/s0065-2776(08)60024-3. [DOI] [PubMed] [Google Scholar]
- Shattil SJ, Kim C, Ginsberg MH. The final steps of integrin activation: the end game. Nat Rev Mol Cell Biol. 2010;11(4):288–300. doi: 10.1038/nrm2871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ley K. et al. Getting to the site of inflammation: the leukocyte adhesion cascade updated. Nat Rev Immunol. 2007;7(9):678–689. doi: 10.1038/nri2156. [DOI] [PubMed] [Google Scholar]
- Schmid MC. et al. Receptor tyrosine kinases and TLR/IL1Rs unexpectedly activate myeloid cell PI3kgamma, a single convergent point promoting tumor inflammation and progression. Cancer Cell. 2011;19(6):715–727. doi: 10.1016/j.ccr.2011.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avraamides CJ, Garmy-Susini B, Varner JA. Integrins in angiogenesis and lymphangiogenesis. Nat Rev Cancer. 2008;8(8):604–617. doi: 10.1038/nrc2353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desgrosellier JS, Cheresh DA. Integrins in cancer: biological implications and therapeutic opportunities. Nat Rev Cancer. 2010;10(1):9–22. doi: 10.1038/nrc2748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foubert P, Varner JA. Integrins in tumor angiogenesis and lymphangiogenesis. Methods Mol Biol. 2012;757:471–486. doi: 10.1007/978-1-61779-166-6_27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin H. et al. Integrin alpha4beta1 promotes monocyte trafficking and angiogenesis in tumors. Cancer Res. 2006;66(4):2146–2152. doi: 10.1158/0008-5472.CAN-05-2704. [DOI] [PubMed] [Google Scholar]
- Luque A. et al. Activated conformations of very late activation integrins detected by a group of antibodies (HUTS) specific for a novel regulatory region (355–425) of the common beta 1 chain. J Biol Chem. 1996;271(19):11067–11075. doi: 10.1074/jbc.271.19.11067. [DOI] [PubMed] [Google Scholar]
- Arnaout MA, Mahalingam B, Xiong JP. Integrin structure, allostery, and bidirectional signaling. Annu Rev Cell Dev Biol. 2005;21:381–410. doi: 10.1146/annurev.cellbio.21.090704.151217. [DOI] [PubMed] [Google Scholar]
- Ye F. et al. Recreation of the terminal events in physiological integrin activation. J Cell Biol. 2010;188(1):157–173. doi: 10.1083/jcb.200908045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye F, Kim C, Ginsberg MH. Reconstruction of integrin activation. Blood. 2012;119(1):26–33. doi: 10.1182/blood-2011-04-292128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feral CC. et al. Blocking the alpha 4 integrin-paxillin interaction selectively impairs mononuclear leukocyte recruitment to an inflammatory site. J Clin Invest. 2006;116(3):715–723. doi: 10.1172/JCI26091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manevich E. et al. Talin 1 and paxillin facilitate distinct steps in rapid VLA-4-mediated adhesion strengthening to vascular cell adhesion molecule 1. J Biol Chem. 2007;282(35):25338–25348. doi: 10.1074/jbc.M700089200. [DOI] [PubMed] [Google Scholar]
- Lewis JS. et al. Expression of vascular endothelial growth factor by macrophages is up-regulated in poorly vascularized areas of breast carcinomas. J Pathol. 2000;192(2):150–158. doi: 10.1002/1096-9896(2000)9999:9999<::AID-PATH687>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- Sunderkotter C. et al. Macrophages and angiogenesis. J Leukoc Biol. 1994;55(3):410–422. doi: 10.1002/jlb.55.3.410. [DOI] [PubMed] [Google Scholar]
- Giraudo E, Inoue M, Hanahan D. An amino-bisphosphonate targets MMP-9-expressing macrophages and angiogenesis to impair cervical carcinogenesis. J Clin Invest. 2004;114(5):623–633. doi: 10.1172/JCI22087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hildenbrand R. et al. Urokinase and macrophages in tumour angiogenesis. Br J Cancer. 1995;72(4):818–823. doi: 10.1038/bjc.1995.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esposito I. et al. Inflammatory cells contribute to the generation of an angiogenic phenotype in pancreatic ductal adenocarcinoma. J Clin Pathol. 2004;57(6):630–636. doi: 10.1136/jcp.2003.014498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang S. et al. Contributions of stromal metalloproteinase-9 to angiogenesis and growth of human ovarian carcinoma in mice. J Natl Cancer Inst. 2002;94(15):1134–1142. doi: 10.1093/jnci/94.15.1134. [DOI] [PubMed] [Google Scholar]
- Ostrand-Rosenberg S, Sinha P. Myeloid-derived suppressor cells: linking inflammation and cancer. J Immunol. 2009;182(8):4499–4506. doi: 10.4049/jimmunol.0802740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munder M. Arginase: an emerging key player in the mammalian immune system. Br J Pharmacol. 2009;158(3):638–651. doi: 10.1111/j.1476-5381.2009.00291.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez PC. et al. L-arginine consumption by macrophages modulates the expression of CD3 zeta chain in T lymphocytes. J Immunol. 2003;171(3):1232–1239. doi: 10.4049/jimmunol.171.3.1232. [DOI] [PubMed] [Google Scholar]
- Nagaraj S. et al. Altered recognition of antigen is a mechanism of CD8+ T cell tolerance in cancer. Nat Med. 2007;13(7):828–835. doi: 10.1038/nm1609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sauer H, Wartenberg M, Hescheler J. Reactive oxygen species as intracellular messengers during cell growth and differentiation. Cell Physiol Biochem. 2001;11(4):173–186. doi: 10.1159/000047804. [DOI] [PubMed] [Google Scholar]
- Fichtner-Feigl S. et al. Restoration of tumor immunosurveillance via targeting of interleukin-13 receptor-alpha 2. Cancer Res. 2008;68(9):3467–3475. doi: 10.1158/0008-5472.CAN-07-5301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terabe M. et al. Transforming growth factor-beta production and myeloid cells are an effector mechanism through which CD1d-restricted T cells block cytotoxic T lymphocyte-mediated tumor immunosurveillance: abrogation prevents tumor recurrence. J Exp Med. 2003;198(11):1741–1752. doi: 10.1084/jem.20022227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shojaei F. et al. Tumor refractoriness to anti-VEGF treatment is mediated by CD11b + Gr1+ myeloid cells. Nat Biotechnol. 2007;25(8):911–920. doi: 10.1038/nbt1323. [DOI] [PubMed] [Google Scholar]
- Qu X. et al. Induction of Bv8 expression by granulocyte-colony stimulating factor in CD11b + Gr1+ cells: Key role of Stat3 signaling. J Biol Chem. 2012;287(23):19574–19584. doi: 10.1074/jbc.M111.326801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shojaei F. et al. Role of Bv8 in neutrophil-dependent angiogenesis in a transgenic model of cancer progression. Proc Natl Acad Sci U S A. 2008;105(7):2640–2645. doi: 10.1073/pnas.0712185105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jain RK. Normalization of tumor vasculature: an emerging concept in antiangiogenic therapy. Science. 2005;307(5706):58–62. doi: 10.1126/science.1104819. [DOI] [PubMed] [Google Scholar]
- Mazzieri R. et al. Targeting the ANG2/TIE2 axis inhibits tumor growth and metastasis by impairing angiogenesis and disabling rebounds of proangiogenic myeloid cells. Cancer Cell. 2011;19(4):512–526. doi: 10.1016/j.ccr.2011.02.005. [DOI] [PubMed] [Google Scholar]
- Stockmann C. et al. Deletion of vascular endothelial growth factor in myeloid cells accelerates tumorigenesis. Nature. 2008;456(7223):814–818. doi: 10.1038/nature07445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shree T. et al. Macrophages and cathepsin proteases blunt chemotherapeutic response in breast cancer. Genes Dev. 2011;25(23):2465–2479. doi: 10.1101/gad.180331.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Squadrito ML. et al. miR-511-3p Modulates Gentic Programs of Tumor-Associated Macrophages. Cell Reports. 2012;1:141–154. doi: 10.1016/j.celrep.2011.12.005. [DOI] [PubMed] [Google Scholar]
- DeNardo DG. et al. CD4(+) T cells regulate pulmonary metastasis of mammary carcinomas by enhancing protumor properties of macrophages. Cancer Cell. 2009;16(2):91–102. doi: 10.1016/j.ccr.2009.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]