Abstract
Background
For anatomists, the cardia is a portion of the stomach. However, at the histological level, the cardiac mucosa, described as columnar-lined with mucus-producing glands (CLMMG), is for some pathologists part of the stomach (already present at birth) and for others a metaplastic change of the esophagus induced by gastro-esophageal reflux (GER).
Materials and Methods
The distal esophagus and the proximal stomach of 5 adult male baboons were removed en bloc at autopsy. The distance between the most distal part of the squamous epithelium of the esophagus and the first oxyntic fundic gastric gland (representing the entire CLMMG) was assessed using an ocular microscale.
Results
The length of the CLMMG varied from 1.2 mm to 12.4 mm. The CLMMG had replaced the squamous epithelium of the distal esophagus in all 5 baboons.
Discussion
Regurgitation with rumination is a natural physiological, daily, recurrent process in baboons that leads to GER. The luminal cytoplasmic vacuoles with neutral mucins contained in the columnar cells and the neutral mucins produced by the mucin glands buffer the low pH of the gastric juices that reflux into the distal esophagus. This protective action against the acid refluxate cannot be achieved by the squamous epithelium.
Conclusion
The results of this preliminary investigation suggest that in baboons, CLMMG is an adaptation process of the esophageal mucosal to the low pH microenvironment conveyed by protracted GER.
Keywords: Metaplasia, esophagus, reflux, baboons
The esophagus extends from the cricoid cartilage to its junction with the stomach and is covered with stratified (non-keratinized) squamous epithelium (1). The stomach extends from the esophageal-gastric junction to the pylorus and is divided into four anatomical regions (1, 2): the cardia, the fundus, the body and the antrum. The cardiac mucosa (CM) is covered with columnar-lined epithelium having mucous-secreting glands and the fundic mucosa (fundus and body) is built of oxyntic glands and principal cells. The antral mucosa is covered with similar glands as those seen in the cardia (1, 3).
Some pathologists affirm that the CM is a normal histological component in human newborns (4–7), whereas others assert that the squamous epithelium of the esophagus and the oxyntic mucosa of the proximal stomach meet at the gastroesophageal-junction region at birth (8, 9). The latter authors claim that in humans, the CM is a metaplastic mucosal transformation of the squamous epithelium of the esophagus induced by the damage caused by protracted gastroesophageal reflux (GER). The percentage of patients having CM at histology varies in the literature from 35% (10) to 81% (11).
Heartburn is an occasional symptom experienced by the majority of individuals in many populations, with a prevalence of 40% among Swedes (11), 34% among Germans (12) and of 36% among North Americans (13). Although in baboons regurgitation with rumination is a physiological process leading to GER (14, 15), heartburn is not a symptom that can be easily identified in these animals.
While reviewing histological sections from the entire esophageal-gastric region in non-human primates (NHP) (16, 17), it was noticed that the distal esophagus in some animals was lined by a mucosa very similar to CM in humans.
The purpose of this work was to assess the length of the columnar-lined mucosa with mucous glands in a group of baboons.
Materials and Methods
The distal esophagus, together with the proximal stomach, were removed en bloc at autopsy in 5 female baboons (Papio spp.) which had died from natural causes. The baboons lived in colonies at the Southwest National Primate Research Center, Southwest Foundation for Biomedical Research. The conditions of animal housing have been reported elsewhere (18). All procedures were carried out in accordance with the Institutional Animal Care and Use Committee guidelines.
The specimens were fixed in 10% neutral buffered formalin, processed conventionally, embedded in paraffin, cut at 5 μm, stained with hematoxylin and eosin (H&E) and evaluated under light microscopy.
Assessement of the length of the CLMMG
The distance between the distal end of the squamous epithelium of the esophagus and the first fundic gastric gland (i.e. built with oxyntic cells and principal cells) was recorded in mm with the aid of an ocular microscale in the 5 animals.
Results
The mean age of the 5 baboons was 11.2 years (range 6–17 years).
Histological findings
The CLMMG was found replacing the distal esophagus.
The size of the CLMMG in the 5 baboons was 4.2 mm, 10.0 mm, 6.7 mm, 13.5 mm and 7.5 mm, respectively (mean 8.4 mm, range 4.2–13.5 mm) (Figure 1).
Figure 1.
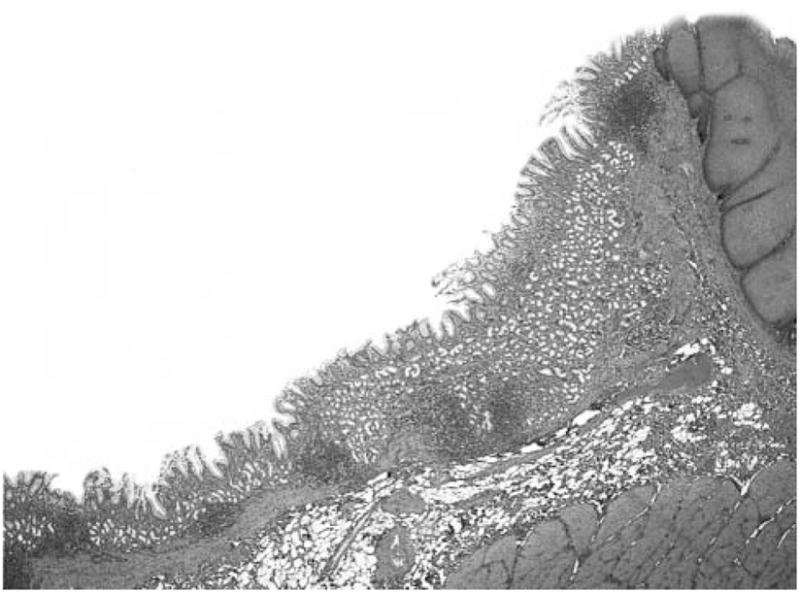
Extended columnar-lined mucosa with mucous glands (CLMMG) in a 12-year-old baboon. Note the squamous epithelium on the right (H&E, ×4).
Discussion
Much discussion has centred on the origin of the cardiac mucosa in humans. For some pathologists this mucosa is present at birth (4–7) while for others it is a metaplastic change due to the damage of the squamous epithelium of the distal esophagus evoked by protracted GER (8, 9, 19). This controversy appears to have originated from the fact that the cardia, an anatomical term (1, 2) has been used to designate a mucosa phenotype that according to many authors does not exists at birth (8, 9).
Today, tumors of the cardia region are coded with those in the stomach. On the other hand, it has been postulated that many carcinomas, initially classified as cancers of the gastric cardia, are in reality esophageal cancers (20). In this respect, Heidi et al. (21) reported in 1993 a detailed comparative study on the basis of 492 squamous carcinomas of the esophagus, 66 esophageal adenocarcinomas, 359 adenocarcinomas of the cardia, and 1288 infracardial gastric adenocarcinomas. These authors concluded that esophageal adenocarcinomas and adenocarcinomas of cardia should be considered as one separate entity. Hence, according to these authors (21), the cardia belongs to the esophagus rather than to the stomach. Recent data from the Surveillance Epidemiology and End Results program (22) indicate that the incidence of esophageal adenocarcinoma among white American men increased 463%, from 1.01 per 100,000 person-years during 1975–1979 to 5.69 per 100,000 person-years during 2000–2004. Due to this apparent epidemic development, many researchers have given priority to the study of this columnar-lined mucosa.
In this investigation it was found that the length of the CLMMG varied considerably in baboons, from 4.2 mm to 13.5 mm. The length was not related to the age of the animals.
The physiological, recurring, daily regurgitation of the gastric secretion seemed to have been the cause for the metaplastic transformation of the mucosa of the distal esophagus in these animals. The luminal cytoplasmic vacuoles with neutral mucins contained in the columnar cells (23) and the neutral mucins produced by the mucin glands, would buffer the low pH of the gastric juices that reflux into the distal esophagus. This protecting action against the acid refluxate cannot be achieved by the squamous epithelium.
In conclusion, the results of this preliminary investigation suggest that in baboons CLMMG is an adaptation process of the esophageal mucosal to the low pH microenvironment conveyed by protracted GER.
References
- 1.Owen DA. Stomach. In: Sternberg StephenS., editor. Hisology for Patologists. 2. Lippincott-Raven Publ; Philadelphia: 1977. pp. 481–493. [Google Scholar]
- 2.Standring S. Oesophagus and stomach. In: Standring Susan., editor. Gray’s Anatomy. 39. Edinburgh: 2005. pp. 986–990.pp. 1143–1160. [Google Scholar]
- 3.Rubio CA, Jaramillo E, Suzuki G, Lagergren P, Nesi G. Antralization of the gastric mucosa of the incisura angularis and its gastrin expression. Int J Clin Exp Pathol. 2009;2:65–70. [PMC free article] [PubMed] [Google Scholar]
- 4.De Hertogh G, Van Eyken P, Ectors N, Tack J, Geboes K. On the existence and location of cardiac mucosa: an autopsy study in embryos, fetuses, and infants. Gut. 2003;52:791–796. doi: 10.1136/gut.52.6.791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marsman WA, van Sandick JW, Tytgat GN, Kate FJ, van Lanschot JJ. The presence and mucin histochemistry of cardiac type mucosa at the esophagogastric junction. Am J Gastroenterol. 2004;99 :212–217. doi: 10.1111/j.1572-0241.2004.04053.x. [DOI] [PubMed] [Google Scholar]
- 6.Odze RD. Pathology of the gastroesophageal junction. Semin Diagn Pathol. 2005;22:256–265. doi: 10.1053/j.semdp.2006.04.007. [DOI] [PubMed] [Google Scholar]
- 7.Srivastava A, Odze RD, Lauwers GY, Redston M, Antonioli DA, Glickman JN. Morphologic features are useful in distinguishing Barrett esophagus from carditis with intestinal metaplasia. Am J Surg Pathol. 2007;31:1733–1741. doi: 10.1097/PAS.0b013e318078ce91. [DOI] [PubMed] [Google Scholar]
- 8.Chandrasoma P. Cardiac mucosal changes in a pediatric population. Am J Surg Pathol. 2003;27:274–275. doi: 10.1097/00000478-200302000-00022. [DOI] [PubMed] [Google Scholar]
- 9.Ringhofer C, Lenglinger J, Izay B, Kolarik K, Zacherl J, Eisler M, Wrba F, Chandrasoma PT, Cosentini EP, Prager G, Riegler M. Histopathology of the endoscopic esophagogastric junction in patients with gastroesophageal reflux disease. Wien Klin Wochenschr. 2008;120:350–359. doi: 10.1007/s00508-008-0997-2. [DOI] [PubMed] [Google Scholar]
- 10.Jain A, Patwari AK, Bajaj P, Kashyap R, Anand VK. Association of gastroesophageal reflux disease in young children with persistent respiratory symptoms. J Trop Pediatr. 2002;48:39–42. doi: 10.1093/tropej/48.1.39. [DOI] [PubMed] [Google Scholar]
- 11.Glickman JN, Fox V, Antonioli DA, Wang HH, Odze RD. Morphology of the cardia and significance of carditis in pediatric patients. Am J Surg Pathol. 2002;26:1032–1039. doi: 10.1097/00000478-200208000-00008. [DOI] [PubMed] [Google Scholar]
- 12.Ronkainen J, Aro P, Storskrubb T, Johansson SE, Lind T, Bolling-Sternevald E, Vieth M, Stolte M, Talley NJ, Agréus L. Prevalence of Barrett’s esophagus in the general population: an endoscopic study. Gastroenterology. 2005;129:1825–1831. doi: 10.1053/j.gastro.2005.08.053. [DOI] [PubMed] [Google Scholar]
- 13.Wienbeck M, Barnert J. Epidemiology of reflux disease and of reflux esophagitis. Scand J Gastroenterol. 1989;156(supplement):7–13. doi: 10.3109/00365528909091032. [DOI] [PubMed] [Google Scholar]
- 14.Nebel O, Fornes M, Castell D. Symptomatic gastroesophageal reflux: incidence and precipitating factors. Am J Dig Dis. 1976;21:953–956. doi: 10.1007/BF01071906. [DOI] [PubMed] [Google Scholar]
- 15.Glover EJ, Leland MM, Dick EJ, Jr, Hubbard GB. Gastroesophageal reflux disease in baboons (Papio sp.): a new animal model. J Med Primatol. 2008;37:18–24. doi: 10.1111/j.1600-0684.2007.00217.x. [DOI] [PubMed] [Google Scholar]
- 16.Glover E, Leland M, Hubbard G. An association between gastric regurgitation and disease in nonhuman primates. Am J Primatol. 2005;66:174–179. [Google Scholar]
- 17.Rubio CA, Dick EJ, Orrego A, Hubbard GB. The frequency of lymphocytic and reflux esophagitis in non-human primates. Int J Clin Exp Pathol. 2008;1:531–535. [PMC free article] [PubMed] [Google Scholar]
- 18.Hubbard GB, Steele KE, Davis KJ, 3rd, Leland MM. Spontaneous pancreatic islet myloidosis in 40 baboons. J Med Primatol. 2002;31:84–90. doi: 10.1034/j.1600-0684.2002.01020.x. [DOI] [PubMed] [Google Scholar]
- 19.Spechler S. Diseases of the esophageal mucosa. In: Shearman DJ, Finlayson N, Camillieri M, Carter D, editors. Diseases of the Gastrointestinal Tract and Liver. New York: Churchill Livingstone; 1977. pp. 191–203. [Google Scholar]
- 20.Chandrasoma P, Wickramasinghe K, Ma Y, DeMeester T. Adenocarcinomas of the distal esophagus and gastric cardia are predominantly esophageal carcinomas. Am J Surg Pathol. 2007;31:569–575. doi: 10.1097/01.pas.0000213394.34451.d2. [DOI] [PubMed] [Google Scholar]
- 21.Heidl G, Langhans P, Mellin W, Bünte H, Grundmann E. Adenocarcinomas of esophagus and cardia in comparison with gastric carcinoma. J Cancer Res Clin Oncol. 1993;120:95–99. doi: 10.1007/BF01200731. [DOI] [PubMed] [Google Scholar]
- 22.Morris-Brown L, Devesa S, Chow WS. Incidence of adenocarcinoma of the esophagus among white Americans by sex, stage and age. J Nat Cancer Inst. 2008;100:1184–1187. doi: 10.1093/jnci/djn211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rubio CA, Saraga EP, Lindholm J. Improved method for mapping gastric intestinal metaplasia using selective histochemical morphometry. Anal Quant Cytol Histol. 1990;12:122–126. [PubMed] [Google Scholar]


