Abstract
Purpose/Objectives
To identify factors associated with diagnostic delay after an incomplete or abnormal mammogram among women participating in a state mammography screening program.
Research Approach
Retrospective case-control design using bivariate and multivariate logistic regression analyses to explore the associations between age, race, ethnicity, marital status, breast cancer history, and self-reported breast symptoms and delay.
Setting
A statewide program of free screening mammography for women who are under- or uninsured.
Participants
11,460 women enrolled in a free, statewide screening program from 2002–2006.
Methodologic Approach
Using the Tennessee Breast and Cervical Cancer Screening Program database, further analyses were conducted.
Main Research Variables
The outcome measure was delay in completion of all diagnostic tests and was defined as women who did not complete testing within 60 days. Findings: Thirty-seven percent of women required follow-up, and of a subset used in the analysis, 30% experienced delay of more than 60 days. Controlling for marital status, age, and breast cancer history, women who experienced delay were more likely to be African American versus Caucasian (odds ratio [OR] = 1.45, 95% confidence interval [CI] = 1.13, 1.85) or Hispanic (OR = 0.72, 95% CI = 0.55, 0.93) and to have self-reported breast symptoms (OR = 1.50, 95% CI = 1.27, 1.77).
Conclusions
In a sample of women with low income needing mammography follow-up, delay was associated with three intrapersonal variables, potentially reducing the effectiveness of mammography screening for women who were African American, or Hispanic, or had self-reported breast symptoms.
Interpretation
Nurses providing cancer screening examinations are uniquely positioned to assess the knowledge, beliefs, and resources of women using the program and to navigate women through barriers to completion. Knowledge of factors associated with delay is valuable for planning interventions and allocating program resources.
Breast cancer is the most frequently diagnosed cancer in women, representing 26% of all female cancers. Furthermore, 192,370 new cases of invasive breast cancer will be diagnosed in women in 2009 (Jemal et al., 2009). As with all cancers, a disparity in breast cancer incidence and mortality exists (American Cancer Society [ACS], 2009a; Jemal et al.). The overall incidence of breast cancer is 12%, lower in African American women than Caucasian women, but higher in African Americans aged 40 years or older (ACS, 2009b). However, in the most recent reporting period, 2000–2003, African American women had a 36% higher death rate than Caucasians. The overall five-year relative survival after breast cancer is 77% for African American women and 90% for Caucasians. The survival differential is attributed to many variables, including access to early detection services, treatment differences, lack of insurance, and tumor and clinical characteristics (Bradley, Given, & Roberts, 2001; Chu, Lamar, & Freeman, 2003).
Screening Mammography
A baseline screening mammogram is recommended for all women aged 40 years and older, and annual mammograms are recommended for women aged 45 years and older (ACS, 2009a). Mammograms have been shown to identify breast cancer effectively at an early stage, with subsequent improvement in survival and cure rates (Buseman, Mouchawar, Calonge, & Byers, 2003; Elmore, Armstrong, Lehman, & Fletcher, 2005; Gotzsche & Nielsen, 2006.) Four percent to 7.1% of women are diagnosed with breast cancer after screening mammography (Eheman et al., 2006). Because the lowest rates of reported mammography occur in uninsured women and in those with no usual medical care, much effort has been made to provide free screening mammography to underserved populations, including low-income and minority women (Peek & Han, 2004). However, because use of screening mammography does not explain the known variation in time of diagnosis or in mortality, it is important to explore other variables that may be contributing to the divergent outcome.
Mammogram results are interpreted by radiologists using the American College of Radiologists Breast Imaging Reporting and Data System (BIRADS™) categories. About 8.5%–15% of women who receive routine screening mammograms have findings that require further testing (Kerlikowske, Smith-Bindman, Ljung, & Grady, 2003). According to 2002 figures, 38% of the 48 million women aged 40 years and older were estimated to have mammograms; approximately three million of the women will have an incomplete or positive test (Taplin et al., 2002); 30%–50% never return for follow-up testing (Arnsberger et al., 2006; Burack, Simon, Stano, George, & Coombs, 2000). In addition, many women delay the completion of recommended testing for weeks to months. Incomplete screening and delayed follow-up negate the potential benefits of identifying breast cancer at the earliest, most treatable stage.
Delay may occur at any point in the progression of testing and may be because of patient, provider, or system influences. The usual follow-up after an incomplete or abnormal mammogram screening includes diagnostic procedures such as additional mammography views (compression or magnification) and breast ultrasonography, sometimes followed by biopsy (core or excisional). The sequence of tests and procedures continues until a diagnosis of cancer is confirmed or ruled out.
Delay
Contributing to confusion in the interpretation of the timeliness of follow-up care after an abnormal screening result is the lack of an acceptable time for completion of follow-up testing (Wujcik & Fair, 2008). In general, delay is measured from the time of the index mammogram to the diagnosis of cancer or the last diagnostic test ruling out cancer, but a consensus has not been reached regarding the definition of unacceptable delay. Several definitions of timely completion of follow-up testing after abnormal mammography were found, ranging from 2–12 months (Poon et al., 2004; Strzelczyk & Dignan, 2002). No definition of delay makes meaningful comparisons with results of other research investigations difficult.
An earlier meta-analysis demonstrated that a three- to six-month delay from the onset of symptoms of breast cancer (such as a lump) to the start of treatment increases rates of recurrence and death by 10% (Richards, Westcombe, Love, Littlejohns, & Ramirez, 1999). In addition, delay also is associated with increased tumor size, advance in stage of disease at diagnosis, and poorer long-term prognosis. However, controversy exists regarding the effect of delay on survival (Kothari & Fentiman, 2003). For women ultimately diagnosed with breast cancer, a delay of more than 60 days after abnormal or incomplete screening could have severe consequences, such as a late-stage diagnosis of breast cancer, decreasing the chance for curative treatment and increasing the risk of death (Wujcik & Fair, 2008).
The current study employed a retrospective case control design using an existing database of under- or uninsured women participating in a statewide free breast screening program to answer the following questions.
What are the intrapersonal factors that predict delay or completion of diagnostic procedures?
What is the relationship of delay to the stage and size of the tumors of women diagnosed with breast cancer?
The Tennessee Breast and Cervical Screening Program (TBCSP) recommendation for completion of testing is within 60 days of a suspicious or abnormal finding (M.J. Dewey, personal communication, April 2007). Because the program goal is to facilitate completion of testing in 60 or fewer days, delay was defined as more than 60 days for completion- and characteristics of women who delayed were investigated. An ecologic framework (Sallis & Owen, 2002; Zapka & Lemon, 2004) guided the selection of important variables because the framework incorporates education about health practices as well as the need to change organizational behavior and the physical and social environments of the communities. The perspective includes five levels of influence factors for health-related behaviors and conditions: intrapersonal or individual, interpersonal, institutional or organizational, community, and public policy.
Factors at each level can affect health behavior, which is true for the behavior of completing screening mammography. This article reports on the influence of intrapersonal factors on delay.
Methods
Participants were selected from a large sample of women participating in a state-run screening mammography program drawn from 2002–2006. The data reflected information compiled from community enrollment centers to a central facility. The TBCSP provided the data dictionary used to define and record each data element.
The dataset included 13,987 encounters representing a mammography event, including women who had been rescreened one or more times. To minimize the chance of a woman being counted more than once, the first recorded mammogram was retained in the dataset, with subsequent records removed, leaving 11,610 women.
The data for the study were provided from the Tennessee Department of Health as a de-identified aggregate dataset. The institutional review board considered the study exempt from review.
Variables
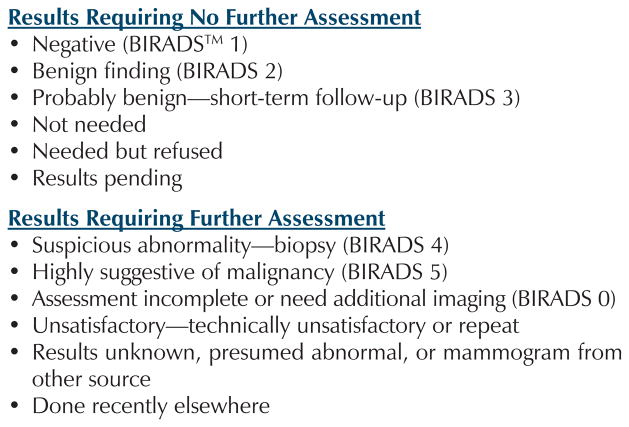
The dataset included information on mammogram results, whether diagnostic tests were performed, and final diagnosis. The sample represented women who did not have a prior diagnosis of cancer, who required further testing after an incomplete or abnormal mammogram coded as BIRADS 0, 4, or 5. Mammogram results were reported in 12 categories such as assessment incomplete/need additional follow-up or BIRADS 0, negative assessment or BIRADS 1, and benign assessment or BIRADS 2. Six categories indicated that a woman required additional testing (see Figure 1).
Figure 1.
Coding Categories for Mammogram Results
The outcome of interest was delay, defined as exceeding 60 days, in completion of testing after receiving an incomplete or abnormal result. Cases were women who did not complete testing within 60 days, and controls were defined as women who completed all testing within 60 days. To assess delay, a time-to-completion variable was created. The start day was the service date. The variable coded as delay if more than 60 days occurred from index screening to completion of testing and as no delay if 60 days or fewer elapsed prior to completion of testing.
Six intrapersonal variables were included in the analyses, including self-reported information on race, ethnicity, marital status, and age.
Statistical Analysis
Data analysis was conducted with SPSS® version 12.0. Univariate analysis was completed with chi squares to examine the association between intrapersonal factors (age, race, ethnicity, marital status, self-reported breast symptoms, and history of cancer variables) and the outcome of delay versus no delay. Multivariate analysis was completed with logistic regression based on the backward Wald statistic. Because this was an exploratory study, analysis began with a full model and variables were eliminated from the model in an iterative process. In using the backward Wald statistic, the fit of the model is tested after the elimination of each variable to ensure the model still adequately fits the data. The adjusted odds ratios of delay or no delay for each individual variable and for variables in the model were estimated with logistic regression models.
Statistical approaches could not be applied because of inadequate numbers of women diagnosed with cancer. Therefore, descriptive analysis was used to discuss the relationship of delay to stage and size of the tumor of women diagnosed with breast cancer.
Results
Demographic results are presented in Table 1. The sample was predominantly Caucasian (85%), non-Hispanic (89%), married (42%), and younger than age 50 years (59%). Most women had no current symptoms of breast cancer (66%) or personal or family history (65%).
Table 1.
Characteristics of Women Needing Follow-Up and With No Delay and Delay
| Variable | Sample (N = 11,610)
|
Women Needing Follow-Up (n = 4,036)a
|
Women With No Delay (n = 2,809)
|
Women With Delay (n = 1,227)
|
||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| Age (years) | ||||||||
| Less than 40 | 3,586 | 31 | 1,316 | 32 | 949 | 34 | 367 | 30 |
| 40–49 | 3,232 | 28 | 1,403 | 35 | 974 | 35 | 429 | 35 |
| 50 or older | 4,792 | 41 | 1,317 | 33 | 886 | 32 | 431 | 35 |
| Marital status | ||||||||
| Married | 4,988 | 42 | 1,798 | 45 | 1,273 | 45 | 525 | 43 |
| Single | 4,159 | 36 | 1,411 | 35 | 964 | 34 | 447 | 36 |
| Divorced | 1,529 | 13 | 537 | 13 | 379 | 13 | 158 | 13 |
| Widowed | 467 | 4 | 129 | 3 | 81 | 3 | 48 | 4 |
| Separated | 339 | 3 | 119 | 3 | 82 | 3 | 37 | 3 |
| Unknown | 128 | 1 | 42 | 1 | 30 | 1 | 12 | 1 |
| Race | ||||||||
| Caucasian | 9,946 | 85 | 3,496 | 87 | 2,456 | 87 | 1,040 | 85 |
| African American | 995 | 9 | 306 | 8 | 190 | 7 | 116 | 9 |
| Other | 669 | 6 | 232 | 6 | 162 | 6 | 70 | 6 |
| Ethnicity | ||||||||
| Non-Hispanic | 10,375 | 89 | 3,602 | 89 | 2,518 | 90 | 1,084 | 88 |
| Hispanic | 1,195 | 10 | 415 | 10 | 274 | 10 | 141 | 11 |
| Unknown | 40 | 1 | 19 | 1 | 17 | 1 | 2 | 1 |
| Breast cancer history | ||||||||
| None | 7,493 | 65 | 2,573 | 64 | 1,782 | 63 | 791 | 64 |
| Family | 1,482 | 13 | 650 | 16 | 454 | 16 | 196 | 16 |
| Personal | 288 | 3 | 140 | 3 | 98 | 3 | 42 | 3 |
| Unknown | 2,347 | 20 | 673 | 17 | 475 | 17 | 198 | 16 |
| Breast symptoms | ||||||||
| Yes | 3,451 | 30 | 2,862 | 71 | 2,068 | 74 | 794 | 65 |
| No | 7,633 | 66 | 1,094 | 27 | 692 | 25 | 402 | 33 |
| Unknown | 526 | 4 | 80 | 2 | 49 | 2 | 31 | 2 |
Of 11,610 women, 4,336 needed follow-up (37%); however, for this analysis, only women with time to completion greater than one day were included (n = 4,036).
Note. Because of rounding, not all percentages total 100; because of missing data, not all n values total the sample.
Findings showed that of 11,610 women, 4,336 (37%) needed follow-up. However, only women with time to completion greater than one day were included (n = 4,036). Of those women, 1,227 (30%) experienced delay more than 60 days for completion of all tests. Women with delay were predominantly Caucasian (85%), non-His-panic (88%), and married (43%); had no history of breast cancer (64%); and presented with breast symptoms (65%). Women aged 39 years or younger had the least delay with equal delay in the groups aged 40 years or older.
The first research question addressed the intrapersonal factors that predicted delay or completion of diagnostic procedures. Using bivariate chi squares, findings showed that variables significantly associated with delay were race (x2[2, N = 4,036] = 8.86, p = 0.01), age (x2[2, N = 4,036] = 7.14, p = 0.03), and lack of breast symptoms (x2[2, N = 4,036] = 30.40, p < 0.001). The variables marital status, breast cancer history, and ethnicity were not significant.
In multivariate analysis, the effects of age were explained by race and self-reported breast symptoms. African American women were 45% more likely to experience delay. Furthermore, almost half of the women experienced delay if they needed follow-up but did not report breast symptoms. Ethnicity was significant with more Hispanic women experiencing delay than women of other ethnicities (odds ratio [OR] = 0.72) (see Table 2).
Table 2.
Multivariate Logistic Regression: Delay
| Variable | β | Wald | OR | CI |
|---|---|---|---|---|
| Race | ||||
| African American versus Caucasian | 0.368 | 3.528 | 1.45 | 1.13, 1.85 |
| Ethnicity | ||||
| Non-Hispanic versus Hispanic | −0.333 | 1.313 | 0.72 | 0.55, 0.93 |
| Breast symptoms | ||||
| No, yes | 0.406 | 1.303 | 1.50 | 1.27, 1.77 |
| Constant | −0.721 | 5.807 | ||
CI—confidence interval; OR—odds ratio
The second research question addressed the relationship of delay to stage and size of the tumor of women diagnosed with breast cancer. Because of the small number of women diagnosed with cancer (n = 124), the association was examined with descriptive statistics. Results for stage and tumor size were recorded for 115 women and, of them, 7 (6%) had delay and 108 (94%) had no delay. Demographic characteristics of women who were diagnosed with cancer were similar to the overall sample. Women ultimately diagnosed with cancer were predominantly married, Caucasian, and non-Hispanic with no family or personal history of breast cancer. However, 57% of women diagnosed with cancer were older than age 50 years, and almost 90% of women presented with self-reported breast symptoms. Findings showed that 58% percent of the women were diagnosed with advanced (stage III and IV) cancer. Because of the small number of women diagnosed with cancer, conclusions could not be reached regarding the relationship of delay and stage of cancer.
Discussion
In the sample, the percentage of women requiring follow-up was much higher than the 10%–15% follow-up rate after screening mammography reported by others (Eheman et al., 2006; Kerlikowske et al., 2003; Strzelczyk & Dignan, 2002). However, the federally funded and state-administered program is not only a screening program for uninsured women older than age 50 years but also allows screening for younger women who may be at higher risk. The high-risk women are aged 40–49 years with symptoms or a family history of breast cancer and women younger than age 40 years with breast symptoms. An unexpected finding in the study was that two-thirds of the women in the sample were younger than age 50 years. Because those women required an existing risk factor or symptom of potential breast cancer to be eligible for free mammography, it follows that a higher number of women needing further diagnostic testing would be expected.
Predictors of Delay
The study tested the relationship between intrapersonal variables and delay. Results were consistent with previous research, indicating that delay is associated with the African American race (Gorin, Heck, Cheng, & Smith, 2006; Gwyn et al., 2004; Strzelczyk & Dignan, 2002; Yabroff et al., 2004) and Hispanic ethnicity (Yabroff et al.; Gorin et al.) and is not associated with family history of cancer (Haas, Cook, Puopolo, Burstin, & Brennan, 2000; Olivotto et al., 2002; Poon et al., 2004; Schootman, Myers-Geadelmann, & Fuortes, 2000) or marital status (Wujcik & Fair, 2008). Results in the literature are conflicting regarding the relationship of delay and age. The finding that an absence of self-reported breast symptoms is associated with delay in completion of follow-up testing has not been reported previously.
Race
African American women are consistently found to experience more delay in completion of testing after incomplete or abnormal findings. In a previous review of the literature, the relationship of race and delay in mammographic resolution was measured in only 5 of 22 studies (Wujcik & Fair, 2008). The results were consistent in all studies with up to four times more delay reported for African American women than Caucasian women (Gorin et al., 2006; Gwyn et al., 2004; Strzelczyk & Dignan, 2002; Yabroff et al., 2004). Although race and income commonly are linked in reports of healthcare disparities, income was not considered in the current study (Smedley, Stith, & Nelson, 2005) because only women who met federal poverty guidelines were eligible for the program.
Hispanic ethnicity
Less research has been conducted examining the relationship of ethnicity with delay. The finding that non-Hispanic women were 28% less likely to experience delay is consistent with other findings. Yabroff et al. (2004) found that Hispanics were 48% less likely to follow up after incomplete findings. Hispanic women had an 18% diagnostic delay (initial consultation to biopsy-proven diagnosis), a 19.7% treatment delay (diagnosis to start of treatment), and a 6.5% combined delay (Gorin et al., 2006). Bedell, Wood, Lezotte, Sedlacek, and Orleans (1995) analyzed the delay in three settings: a public hospital, a university hospital, and a private clinic. The public and university hospitals had more delay, and the public hospital served mostly Hispanic women. In the dataset, race and ethnicity were separate variables. Others, such as the National Breast and Cervical Cancer Early Detection Program, combine race and ethnicity, making comparisons among different studies difficult.
Breast symptoms
Breast symptoms are defined as self-reporting one or more of the following symptoms: breast lump(s), nipple discharge, skin changes, or nipple changes. The findings indicate that more women with no self-reported symptoms were more likely to experience delay. Presence of breast symptoms is another variable where little study has been done to determine the association with delay. Caplan et al. (1995) reported that fewer women experienced delay with the presence of a lump, whereas Schootman et al. (2000) found that women who felt a lump were twice as likely to be noncompliant. Rojas, Mendelblatt, Cagney, Kerner, and Freeman (1996) reported a trend that compliers (women who completed testing in four months or less) were more likely to have a lump (p = 0.10). None of the studies, including the current study, reported the correlation between self-reported symptoms and abnormal clinical breast examination. The relationship of delay and self-reported breast symptoms remains an area requiring further study.
Family history
The findings suggest no relationship between family history of breast cancer and delay, which is supported by others (Haas et al., 2000; Olivotto et al., 2002; Poon et al., 2004; Schootman et al., 2000). Two studies reporting a relationship between family history of breast cancer and delay were found. Strzelczyk and Dignan (2002) reported increased incidence of delay if no family history of breast cancer was reported (risk ratio [RR] = 1.61, 95% confidence interval [CI] = 1.43, 1.81), whereas Yabroff et al. (2004) reported a trend toward increased incidence of delay with a family history of breast cancer (OR = 1.41, 95% CI = 0.81, 2.26). Further study is needed to determine whether a family history of cancer creates fear of diagnosis that results in delayed follow-up or, conversely, a lack of family history decreases the urgency to follow up.
Age
The current study showed more delay in women older than age 50 years. The result is consistent with others (Strzelczyk & Dignan, 2002; Burack et al., 2000). However, five studies reported more delay in women younger than age 50 years (Caplan et al., 1995; Gwyn et al., 2004; Haas et al., 2000; Schootman et al., 2000; Yabroff et al., 2004). Because women in the current study who were younger than age 50 can participate only if they have risk factors of family or personal history of cancer or breast symptoms, follow-up of abnormal/incomplete results may be more urgent in younger women. Reaching strong conclusions regarding the results remains difficult because the only studies available for comparison do not use the same definitions for delay and do not differentiate between a true screening mammography program and a program that provides diagnostic and screening mammography.
Marital status
Marital status was not found to be a significant predictor of delay after incomplete or abnormal screening mammography. The finding is consistent with a review of 18 studies reporting the relationship of demographic variables and delay where marital status was not found to be a significant variable (Wujcik & Fair, 2008). Although other research has shown that married people enjoy overall better health and longer life expectancy than unmarried people (Johnson, Backlund, Sorlie, & Loveless, 2000), more social support when coping with cancer (Drageset & Lindstrom, 2005), and a survival advantage (Bloom, Stewart, Johnston, Banks, & Fobair, 2001; Kravdal, 2001; Osborne, Ostir, Du, Peek, & Goodwin, 2005), marital status did not influence the time to completion of tests after abnormal or incomplete mammography results.
Implications for Nursing
The knowledge gained from this study adds to an understanding of the intrapersonal factors that predict delay in women with low incomes participating in a state screening mammography program. Although the findings suggest who is at risk for delay (African American, Hispanic, or no self-reported breast symptoms), they do not provide an understanding of why the women are at risk for delay. Additional research is needed to further understand the effect of delay as well as develop effective interventions tailored to overcome factors influencing delay.
Nurses at the National Breast and Cervical Cancer Screening Program enrollment sites are uniquely positioned to assess the knowledge, beliefs, and resources of women using the program and to help women navigate through any organizational barriers potentially hindering completion of follow-up testing. Professional and lay navigators are being used to facilitate movement through the healthcare system from the time of abnormal cancer screening result to the diagnosis of cancer or completion of testing to rule out a cancer diagnosis (Wells et al., 2008). For example, an African American woman who participates in screening mammography may have overcome culturally based fears of cancer and the healthcare system only to be met with new obstacles to completing the testing. A nurse navigator can explain the need for further tests and the meaning of any results. The navigator also can help women identify barriers and coach them in strategies to overcome them.
A woman who does not have breast symptoms may be less likely to be concerned about an abnormal mammography result, but the navigator can ensure the patient schedules and keeps return appointments. Knowledge of factors that delay completion of screening testing for breast cancer are valuable to National Breast and Cervical Cancer Early Detection Program healthcare providers and program administrators to plan interventions and allocate program resources.
Conclusion
Screening mammography is not a simple procedure for women who have received an abnormal or incomplete result. It becomes a series of tests, procedures, and consultations that require time, resources, and emotional energy to complete. This study adds to the understanding of screening mammography behavior in underserved populations. Intrapersonal factors of race, ethnicity, and self-reported breast symptoms at the time of examination were important predictors of delay, whereas age, marital status, and history of breast cancer were not. Further exploration of the predictors is needed to consider whether they are patient or provider variables. Analysis of the characteristics of women participating in a federally funded, state-administered screening program provides a unique opportunity to identify the predictors of delay and plan future program interventions to reduce time to completion as well as potentially impact cancer morbidity and mortality in minority and medically underserved women.
Acknowledgments
The authors gratefully acknowledge Mary Jane Dewey, MPA, director of the Tennessee Breast and Cervical Cancer Screening Program, for her assistance.
This research was funded by American Cancer Society Doctoral Scholarship (DSCN-04-158-01), University of Utah Oncology Nursing PhD Using Distance Technology National Cancer Society Grant (1R25CA93831-01) (principal investigator [PI] Mooney), and the National Cancer Institute (U54 CA915408-04) (PI Moses).
Contributor Information
Debra Wujcik, Director of clinical trials at Vanderbilt-Ingram Cancer Center and an associate professor in the School of Nursing at Vanderbilt University in Nashville, TN.
Yu Shyr, Professor of cancer research and director of the Cancer Biostatistics Center at Vanderbilt-Ingram Cancer Center and professor and chief of the Division of Cancer Biostatistics in the Department of Biostatistics at Vanderbilt University Medical Center in Nashville.
Ming Li, Associate professor in the Department of Biostatistics at Vanderbilt University Medical Center.
Margaret F. Clayton, Assistant professor and College of Nursing at the University of Utah in Salt Lake City.
Lee Ellington, Associate professor, College of Nursing at the University of Utah in Salt Lake City.
Usha Menon, Associate professor in the Department of Biobehavioral Health Science in the College of Nursing at the University of Illinois–Chicago; and.
Kathi Mooney, Professor in the College of Nursing at the University of Utah.
References
- American Cancer Society. Cancer facts and figures 2009. 2009a Retrieved September 12, 2009, from http://www.cancer.org/downloads/STT/500809web.pdf.
- American Cancer Society. Cancer facts and figures for African Americans 2009–2010. 2009b Retrieved September 29, 2009, from http://www.cancer.org/downloads/STT/cffaa_2009-2010.pdf.
- Andersen MR, Yasui Y, Meischke H, Kuniyuki A, Etzioni R, Urban N. The effectiveness of mammography promotion by volunteers in rural communities. American Journal of Preventive Medicine. 2000;18(3):199–207. doi: 10.1016/s0749-3797(99)00161-0. [DOI] [PubMed] [Google Scholar]
- Arnsberger P, Fox P, Ryder P, Nussey B, Zhang X, Otero-Sabogal R. Timely follow-up among multicultural women with abnormal mammograms. American Journal of Health Behavior. 2006;30(1):51–61. doi: 10.5555/ajhb.2006.30.1.51. [DOI] [PubMed] [Google Scholar]
- Bedell MB, Wood ME, Lezotte DC, Sedlacek SM, Orleans MM. Delay in diagnosis and treatment of breast cancer: Implications for education. Journal of Cancer Education. 1995;10(4):223–228. doi: 10.1080/08858199509528378. [DOI] [PubMed] [Google Scholar]
- Bloom JR, Stewart SL, Johnston M, Banks P, Fobair P. Sources of support and the physical and mental well-being of young women with breast cancer. Social Science and Medicine. 2001;53(11):1513–1524. doi: 10.1016/s0277-9536(00)00440-8. [DOI] [PubMed] [Google Scholar]
- Bradley CJ, Given CW, Roberts C. Disparities in cancer diagnosis and survival. Cancer. 2001;91(1):178–188. doi: 10.1002/1097-0142(20010101)91:1<178::aid-cncr23>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- Burack RC, Simon MS, Stano M, George J, Coombs J. Follow-up among women with an abnormal mammogram in an HMO: Is it complete, timely, and efficient? American Journal of Managed Care. 2000;6(10):1102–1113. [PubMed] [Google Scholar]
- Buseman S, Mouchawar J, Calonge N, Byers T. Mammography screening matters for young women with breast carcinoma: Evidence of downstaging among 42–49-year-old women with a history of previous mammography screening. Cancer. 2003;97(2):352–358. doi: 10.1002/cncr.11050. [DOI] [PubMed] [Google Scholar]
- Caplan LS, Helzlsouer KJ, Shapiro S, Freedman LS, Coates RJ, Edwards BK. System delay in breast cancer in whites and blacks. American Journal of Epidemiology. 1995;142(8):804–812. doi: 10.1093/oxfordjournals.aje.a117719. [DOI] [PubMed] [Google Scholar]
- Chu KC, Lamar CA, Freeman HP. Racial disparities in breast carcinoma survival rates: Separating factors that affect diagnosis from factors that affect treatment. Cancer. 2003;97(11):2853–2860. doi: 10.1002/cncr.11411. [DOI] [PubMed] [Google Scholar]
- Drageset S, Lindstrom TC. Coping with a possible breast cancer diagnosis: Demographic factors and social support. Journal of Advanced Nursing. 2005;51(3):217–226. doi: 10.1111/j.1365-2648.2005.03495.x. [DOI] [PubMed] [Google Scholar]
- Eheman CR, Benard VB, Blackman D, Lawson HW, Anderson C, Helsel W, et al. Breast cancer screening among low-income or uninsured women: Results from the National Breast and Cervical Cancer Early Detection Program, July 1995–March 2002 (United States) Cancer Causes and Control. 2006;17(1):29–38. doi: 10.1007/s10552-005-4558-y. [DOI] [PubMed] [Google Scholar]
- Elmore JG, Armstrong K, Lehman CD, Fletcher SW. Screening for breast cancer. JAMA. 2005;293(10):1245–1256. doi: 10.1001/jama.293.10.1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorin SS, Heck JE, Cheng B, Smith SJ. Delays in breast cancer diagnosis and treatment by racial/ethnic group. Archives of Internal Medicine. 2006;166(20):2244–2252. doi: 10.1001/archinte.166.20.2244. [DOI] [PubMed] [Google Scholar]
- Gotzsche PC, Nielsen M. Screening for breast cancer with mammography. Cochrane Database of Systematic Reviews. 2006;(4):CD001877. doi: 10.1002/14651858.CD001877.pub2. [DOI] [PubMed] [Google Scholar]
- Gwyn K, Bondy ML, Cohen DS, Lund MJ, Liff JM, Flagg EW, et al. Racial differences in diagnosis, treatment, and clinical delays in a population-based study of patients with newly diagnosed breast carcinoma. Cancer. 2004;100(8):1595–1604. doi: 10.1002/cncr.20169. [DOI] [PubMed] [Google Scholar]
- Haas JS, Cook EF, Puopolo AL, Burstin HR, Brennan TA. Differences in the quality of care for women with an abnormal mammogram or breast complaint. Journal of General Internal Medicine. 2000;15(5):321–328. doi: 10.1046/j.1525-1497.2000.08030.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ. Cancer statistics, 2009. CA: Cancer Journal for Clinicians. 2009;59(4):225–249. doi: 10.3322/caac.20006. [DOI] [PubMed] [Google Scholar]
- Johnson NJ, Backlund E, Sorlie PD, Loveless CA. Marital status and mortality: The national longitudinal mortality study. Annals of Epidemiology. 2000;10(4):224–238. doi: 10.1016/s1047-2797(99)00052-6. [DOI] [PubMed] [Google Scholar]
- Kerlikowske K, Smith-Bindman R, Ljung BM, Grady D. Evaluation of abnormal mammography results and palpable breast abnormalities. Annals of Internal Medicine. 2003;139(4):274–284. doi: 10.7326/0003-4819-139-4-200308190-00010. [DOI] [PubMed] [Google Scholar]
- Kothari A, Fentiman IS. Diagnostic delays in breast cancer and impact on survival. International Journal of Clinical Practice. 2003;57(3):200–203. [PubMed] [Google Scholar]
- Kravdal O. The impact of marital status on cancer survival. Social Science and Medicine. 2001;52(3):357–368. doi: 10.1016/s0277-9536(00)00139-8. [DOI] [PubMed] [Google Scholar]
- Olivotto IA, Gomi A, Bancej C, Brisson J, Tonita J, Kan L, et al. Influence of delay to diagnosis on prognostic indicators of screen-detected breast carcinoma. Cancer. 2002;94(8):2143–2150. doi: 10.1002/cncr.10453. [DOI] [PubMed] [Google Scholar]
- Osborne C, Ostir GV, Du X, Peek MK, Goodwin JS. The influence of marital status on the stage at diagnosis, treatment, and survival of older women with breast cancer. Breast Cancer Research and Treatment. 2005;93(1):41–47. doi: 10.1007/s10549-005-3702-4. [DOI] [PubMed] [Google Scholar]
- Peek ME, Han JH. Disparities in screening mammography. Current status, interventions, and implications. Journal of General Internal Medicine. 2004;19(2):184–194. doi: 10.1111/j.1525-1497.2004.30254.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poon EG, Haas JS, Puopolo AL, Gandhi TK, Burdick E, Bates DW, et al. Communication factors in the follow-up of abnormal mammograms. Journal of General Internal Medicine. 2004;19(4):316–323. doi: 10.1111/j.1525-1497.2004.30357.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richards MA, Westcombe AM, Love SB, Littlejohns P, Ramirez AJ. Influence of delay on survival in patients with breast cancer: A systematic review. Lancet. 1999;353(9159):1119–1126. doi: 10.1016/s0140-6736(99)02143-1. [DOI] [PubMed] [Google Scholar]
- Rojas M, Mandelblatt J, Cagney K, Kerner J, Freeman H. Barriers to follow-up of abnormal screening mammograms among low-income minority women. Cancer Control Center of Harlem. Ethnicity and Health. 1996;1(3):221–228. doi: 10.1080/13557858.1996.9961790. [DOI] [PubMed] [Google Scholar]
- Sallis JF, Owen N. Ecogogical models of health behavior. In: Glanz K, Rimer BK, Lewis FM, editors. Health behaviors and health education: Theory, research, and practice. 3. San Francisco: Jossey-Bass; 2002. pp. 462–484. [Google Scholar]
- Schootman M, Myers-Geadelmann J, Fuortes L. Factors associated with adequacy of diagnostic workup after abnormal breast cancer screening results. Journal of the American Board of Family Practice. 2000;13(2):94–100. doi: 10.3122/15572625-13-2-94. [DOI] [PubMed] [Google Scholar]
- Smedley BD, Stith AY, Nelson AR. Unequal treatment: Confronting racial and ethnic disparities in health care. Washington, DC: National Academies Press; 2005. [PubMed] [Google Scholar]
- Strzelczyk JJ, Dignan MB. Disparities in adherence to recommended follow-up on screening mammography: Interaction of sociodemographic factors. Ethnicity and Disease. 2002;12(1):77–86. [PubMed] [Google Scholar]
- Taplin SH, Ichikawa LE, Kerlikowske K, Ernster VL, Rosenberg RD, Yankaskas BC, et al. Concordance of breast imaging reporting and data system assessments and management recommendations in screening mammography. Radiology. 2002;222(2):529–535. doi: 10.1148/radiol.2222010647. [DOI] [PubMed] [Google Scholar]
- Wells KJ, Battaglia TA, Dudley DJ, Garcia R, Greene A, Calhoun E, et al. Patient navigation: State of the art or is it science? Cancer. 2008;113(8):1999–2010. doi: 10.1002/cncr.23815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wujcik D, Fair AM. Barriers to diagnostic resolution after abnormal screening mammography: A review of the literature. Cancer Nursing. 2008;31(5):E16–E30. doi: 10.1097/01.NCC.0000305764.96732.45. Retrieved October 20, 2009, from http://journals.lww.com/cancernursingonline/Abstract/2008/09000/Barriers_to_Diagnostic_Resolution_After_Abnormal.15.aspx. [DOI] [PubMed] [Google Scholar]
- Yabroff KR, Breen N, Vernon SW, Meissner HI, Freedman AN, Ballard-Barbash R. What factors are associated with diagnostic follow-up after abnormal mammograms? Findings from a U.S. National Survey. Cancer Epidemiology, Biomarkers and Prevention. 2004;13(5):723–732. [PubMed] [Google Scholar]
- Zapka JG, Lemon SC. Interventions for patients, providers, and healthcare organizations. Cancer. 2004;101(5 Suppl):1165–1187. doi: 10.1002/cncr.20504. [DOI] [PubMed] [Google Scholar]