Abstract
Activation of the sonic hedgehog (Shh) pathway is required for the growth of numerous tissues and organs and recent evidence indicates that this pathway is often recruited to stimulate growth of cancer stem cells (CSCs) and to orchestrate the reprogramming of cancer cells via epithelial mesenchymal transition (EMT). The objectives of this study were to examine the molecular mechanisms by which (-)-epigallocatechin-3-gallate (EGCG), an active compound in green tea, inhibits self-renewal capacity of pancreatic CSCs, and synergizes with quercetin, a major polyphenol and flavonoid commonly detected in many fruits and vegetables. Our data demonstrated that EGCG inhibited the expression of pluripotency maintaining transcription factors (Nanog, c-Myc and Oct-4), and self-renewal capacity of pancreatic CSCs. Inhibition of Nanog by shRNA enhanced the inhibitory effects of EGCG on self-renewal capacity of CSCs. EGCG inhibited cell proliferation and induced apoptosis by inhibiting the expression of Bcl-2 and XIAP, and activating caspase-3. Interestingly, EGCG also inhibited the components of Shh pathway (smoothened, patched, Gli1 and Gli2) and Gli transcriptional activity. Furthermore, EGCG inhibited EMT by inhibiting the expression of Snail, Slug and ZEB1, and TCF/LEF transcriptional activity, which correlated with significantly reduced CSC’s migration and invasion, suggesting the blockade of signaling involved in early metastasis. Furthermore, combination of quercetin with EGCG had synergistic inhibitory effects on self-renewal capacity of CSCs through attenuation of TCF/LEF and Gli activities. Since aberrant Shh signaling occurs in pancreatic tumorigenesis, therapeutics that target Shh pathway may improve the outcomes of patients with pancreatic cancer by targeting CSCs.
Keywords: RNAi, cancer stem cells, pancreatic cancer, pluripotency maintaining factors, Sonic hedgehog pathway, EGCG, epithelial-mesenchymal transition
Introduction
Cancer of the pancreas is the fourth leading cause of cancer-related mortality in the United States with a 5-year survival less than 5%1, 2. In 2010, more than 43,000 new cases were estimated to develop pancreatic cancer, and approximately 36,800 Americans deaths were occurred in the United States 1. Pancreatic cancer has one of the poorest prognoses among all cancers3. Only 20% of pancreatic cancer patients are eligible for surgical resection, which currently remains the only potentially curative therapy4. Unfortunately, many pancreatic cancers are not resectable at the time of diagnosis. There are limited treatment options available for this disease because chemo- and radiotherapies are largely ineffective, and metastatic disease frequently redevelops even after surgery3, 5. Therefore, developing effective strategies to prevent pancreatic cancer is urgently needed.
Cancer stem cells (CSCs) have been proposed to be the cause of therapy failure, cancer relapse and drug resistance6. Therefore, understanding the pathogenesis of the preinvasive stage, and developing effective strategies to prevent pancreatic neoplasms are of paramount importance. Recently, CSCs and epithelial-mesenchymal transition (EMT)-type cells, which shares molecular characteristics with CSCs, have been proposed to play critical roles in drug resistance and early cancer metastasis as demonstrated in several human malignancies including pancreatic cancer. Thus, the discovery of molecular knowledge related to CSC characteristics and EMT in pancreatic cancer is becoming an important area of research, and such knowledge is likely to be helpful in the discovery of novel molecular targets and strategies for the prevention of pancreatic cancer by targeting CSCs.
An increasing amount of scientific evidence indicates that tumors contain a small number of tumor-forming and self-renewing CSCs within a population of non-tumor-forming cancer cells7. We and others have recently identified CSCs in several types of human cancers including pancreatic cancer8, 9. It has been suggested that conventional chemotherapies kill differentiated or differentiating cells. These cells form the bulk of the tumor, but are unable to generate new cells. However, CSCs remain untouched, and therefore can cause a relapse of cancer7. Removal of CSCs becomes more and more crucial to chemo- and radio-therapy. Unlike most cells within the tumor, pancreatic CSCs are resistant to well-defined chemotherapy and radiotherapy, and may contribute to tumor metastasis and tumor recurrence after treatment10. They can also regenerate all the cell types in the tumor through their stem cell-like behavior. For this reason, drugs that selectively target CSCs offer a greater promise for cancer therapy and/or prevention.
Sonic hedgehog (Shh) is a member of the Hedgehog (Hh) family of secreted signaling proteins having diverse functions during vertebrate development11. Hh signaling also functions postembryonically in tissue homeostasis through effects on stem or progenitor cells12. Inappropriate activity of the Hh signaling pathway also has been linked to tumor types that arise sporadically or in genetically predisposed individuals11. Shh signaling is launched by binding of the secreted Shh peptide to the 12-span transmembrane protein Patched (Ptch), resulting in loss of Ptch activity and consequent phosphorylation and posttranscriptional stabilization of Smoothened (Smo)13. As a result, expression of Hh target genes is initialized through posttranslational activation of the Gli family of zinc-finger transcription factors14. Pathway activation via Smo thus can occur either by Hh protein stimulation or through loss of Ptch activity. In a transgenic mouse model of pancreatic cancer, inhibition of Hh signaling was found to reduce tumor-associated stromal tissues and ameliorate gemcitabine uptake in tumor cells15. In another study, inhibition of Shh was associated with prolonged survival of mice16. Activation of Shh signaling pathway is involved in the regulation of the proliferation of the pancreatic CSCs17. These data suggest that pharmacological inhibitors of Shh pathway would be of great interest for the treatment and/or prevention of pancreatic cancer.
Flavonoids are attractive candidates for cancer prevention. Quercetin, 3, 3′, 4′, 5, 7-pentahydroxylflavone, is a flavonoid commonly present in fruits and vegetables, such as onion, tea, apples and berries. It exhibits anti-inflammatory, anti-oxidative and anti-cancer activities18, 19. Quercetin enhances TRAIL-mediated apoptosis in colon cancer cells by inducing the accumulation of death receptors in lipid rafts20. Quercetin exert antitumor activity, inhibit proliferation and induce apoptosis in human pancreatic cancer cells21. Quercetin itself showed growth inhibitory activity on both drug-sensitive and MDR cells22. Epidemiological studies have estimated that the daily dietary intake of quercetin by an individual ranges from 4 to 68 mg23. The flavonol intake reduces the risk for developing pancreatic cancer. Quercetin has also been shown to act as a chemosensitizer for the ABC pump-proteins in a number of MDR tumor cell lines. Quercetin attenuates oxidative damage induced by treatment of embryonic chicken spermatogonial cells with 4-nitro-3-phenylphenol24. Furthermore, quercetin interacts directly with transporter proteins to inhibit drug efflux mediated by either MDR1 or MRP1 or BCRP. Furthermore, quercetin can enhance the effects of sulforaphane and EGCG in inhibiting the pancreatic and prostate CSC characteristics, respectively25, 26.
Unfortunately, the intracellular mechanisms by which (-)-epigallocatechin-3-gallate (EGCG), an active compound in green tea, inhibits growth and invasion, and induces apoptosis in pancreatic CSCs have never been examined. The main objectives of this application are to examine the molecular mechanisms by which EGCG inhibits pancreatic CSC growth and invasion, and induces apoptosis, and synergizes with quercetin in inhibiting CSC characteristics. Our data indicate that: (i) EGCG inhibits proliferation and induces apoptosis in pancreatic cancer through multiple mechanisms; (ii) EGCG inhibits the expression of pluripotency maintaining factors (Nanog, c-Myc and Oct-4), EMT markers (Snail, Slug and ZEB1), Bcl-2 and XIAP; (iii) EGCG inhibits the self-renewal capacity of pancreatic CSC by inhibiting Shh pathway and TCF/LEF activity; and (iv) EGCG synergizes with quercetin to inhibit pancreatic CSC characteristics by blocking Shh pathway and TCF/LEF activity. These data suggest that EGCG can be a beneficial agent for the prevention and/or treatment of pancreatic cancer by targeting CSCs.
Materials and Methods
Reagents
Antibodies against GAPDH and Nanog were purchased from Cell Signaling Technology, Inc. (Danvers, MA). EGCG and quercetin were purchased from LKT Laboratories, Inc. (St. Paul, MN). Enhanced chemiluminescence (ECL) Western blot detection reagents were from Amersham Life Sciences Inc. (Arlington Heights, IL). Terminal Deoxynucleotidyl Transferase Biotin-dUTP Nick End Labeling (TUNEL) assay kit was purchased from EMD Biosciences / Calbiochem (San Diego, CA). All other chemicals were purchased from Sigma-Aldrich (St Luis, MO).
Cell culture
Human pancreatic cancer stem cells (CD133+/CD44+/CD24+/ESA+) were obtained from Celprogen Inc. (San Pedro, CA). They were isolated from primary tumors and have been described previously9. These CSCs consist of a bulk pancreatic cancer stem cell population, and thus can not be considered as a cell line. The CSCs were cultured in DMEM supplemented with 1% N2 Supplement (Invitrogen), 2% B27 Supplement (Invitrogen), 20 ng/ml human platelet growth factor (Sigma-Aldrich), 100 ng/ml epidermal growth factor (Invitrogen) and 1% antibiotic-antimycotic (Invitrogen) at 37°C in a humidified atmosphere of 95% air and 5% CO2.
Tumor spheroid assay
Spheroid forming assays were performed as described elsewhere (9, 10). In brief, cells were plated in six-well ultralow attachment plates (Corning Inc., Corning, NY) at a density of 1,000 cells/ml in DMEM supplemented with 1% N2 Supplement (Invitrogen), 2% B27 Supplement (Invitrogen), 20 ng/ml human platelet growth factor (Sigma-Aldrich), 100 ng/ml epidermal growth factor (Invitrogen) and 1% antibiotic-antimycotic (Invitrogen) at 37°C in a humidified atmosphere of 95% air and 5% CO2. Spheroid were collected after 7 days and dissociated with Accutase (Innovative Cell Technologies, Inc.). The cells obtained from dissociation were sieved through a 40-μm filter, and counted by coulter counter using trypan blue dye.
Soft agar colony assay for assessment of tumorigenic potential in vitro
To examine the anchorage independent growth, the pancreatic CSCs from primary tumors were suspended (103 cells/ml) in 2 ml of 0.3% agar with 1% N2 Supplement (Invitrogen), 2% B27 Supplement (Invitrogen), 20 ng/ml human platelet growth factor (Sigma-Aldrich), 100 ng/ml epidermal growth factor (Invitrogen) and 1% antibiotic-antimycotic (Invitrogen) overlaid into six-well plates containing a 0.5% agar base. After treatment, plates were incubated for 3 weeks and colonies >0.2 mm in diameter were stained with 0.001% crystal violet blue and counted.
Western blot analysis
Western blots were performed as we described elsewhere (38, 85). In brief, cells were lysed in RIPA buffer containing 1 X protease inhibitor cocktail, and protein concentrations were determined using the Bradford assay (Bio-Rad, Philadelphia, PA). Proteins were separated by 12.5% SDS/PAGE and transferred to membranes (Millipore, Bedford, MA) at 55 V for 4 h at 4°C. After blocking in 5% nonfat dry milk in TBS, the membranes were incubated with primary antibodies at 1:1,000 dilution in TBS overnight at 4°C, washed three times with TBS-Tween 20, and then incubated with secondary antibodies conjugated with horseradish peroxidase at 1:5,000 dilution in TBS for 1 hour at room temperature. Membranes were washed again in TBS-Tween 20 for three times at room temperature. Protein bands were visualized on X-ray film using an enhanced chemiluminescence detection system.
Transwell Migration assay
For transwell migration assays, 1 × 105 pancreatic CSCs were plated in the top chamber onto the noncoated membrane (24-well insert; pore size, 8 μm; Corning Costar) and allowed to migrate toward serum-containing medium in the lower chamber. Cells were fixed after 24 hours of incubation with methanol and stained with 0.1% crystal violet (2 mg/ml, Sigma-Aldrich). The number of cells invading through the membrane was counted under a light microscope (three random fields per well).
Transwell invasion assay
For invasion assay, 1 × 105 cells were plated in the top chamber onto the Matrigel coated Membrane (24-well insert; pore size, 8 μm; Corning Costar). Each well was coated freshly with Matrigel (60 μg; BD Bioscience) before the invasion assay. Pancreatic CSCs were plated in medium without serum or growth factors, and medium supplemented with serum was used as a chemoattractant in the lower chamber. The cells were incubated for 48 hours and cells that did invade through the pores were removed by a cotton swab. CSCs on the lower surface of the membrane were fixed with methanol and stained with crystal violet. The number of cells invading through the membrane was counted under a light microscope (40X, three random fields per well).
Isolation of RNA
The total RNA was isolated from the pancreatic cancer stem cells using Trizol (Life Technologies) according to the manufacturer’s instructions. The RNA pellets were then frozen and stored at -80°C until use.
Evaluation of mRNA expression levels by quantitative Real Time-PCR
For the quantification of gene amplification, Real-time PCR was performed using an ABI 7300 Sequence Detection System in the presence of SYBR- Green. Briefly, RNA was isolated and reverse transcribed. cDNA reactions were amplified with QPCR SYBR Green Mix (Applied Biosystems). The following gene-specific primers were used:
Bcl-2 (5’- AGA TGG GAA CAC TGG TGG AG -3’, 5’- TCT TCA CCT CCA GGC TCA GT -3’)
Survivin (5’- TCC CTG GCT CCT CTA CTG TT -3’, 5’- TGT CTC CTC ATC CAC CTG AA -3’)
XIAP (5’- GGG TTT GTC TTG ACC TGG AA -3’, 5’- CTC CCA AAG TGC TGG GAT TA -3’)
Nanog (5’-ACC TAC CTA CCC CAG CCT TT -3’, 5’- CAT GCA GGA CTG CAG AGA TT -3’)
Sox-2 (5’- AAC CCC AAG ATG CAC AAC TC -3’, 5’- GCT TAG CCT CGT CGA TGA AC -3’)
c-Myc (5’- CGA CGA GAC CTT CAT CAA AA -3’, 5’- TGC TGT CGT TGA GAG GGT AG -3’)
Oct4 (5’- GGA CCA GTG TCC TTT CCT CT -3’, 5’- CCA GGT TTT CTT TCC CTA GC -3’)
Smothened (5’-TCG CTA CCC TGC TGT TAT TC -3’, 5’-GAC GCA GGA CAG AGT CTC AT -3’)
Patched1 (5’-TGA CCT AGT CAG GCT GGA AG-3’, 5’-GAA GGA GAT TAT CCC CCT GA-3’)
Patched2 (5’-AGG AGC TGC ATT ACA CCA AG-3’, 5’-CCC AGG ACT TCC CAT AGA GT-3’)
Gli1 (5’-CTG GAT CGG ATA GGT GGT CT -3’, 5’- CAG AGG TTG GGA GGT AAG GA -3’)
Gli2 (5’-GCC CTT CCT GAA AAG AAG AC -3’, 5’- CAT TGG AGA AAC AGG ATT GG -3’)
Snail (5’-ACC CCA CAT CCT TCT CAC TG -3’, 5’- TAC AAA AAC CCA CGC AGA CA -3’)
ZEB1 (5’-GCA CAA CCA AGT GCA GAA GA -3’, 5’- CAT TTG CAG ATT GAG GCT GA -3’)
Slug (5’-ACA CAC ACA CAC CCA CAG AG -3’, 5’- AAA TGA TTT GGC AGC AAT GT -3’)
HK-GAPD (5’-GAG TCA ACG GAT TTG GTC GT-3’, 5’-TTG ATT TTG GAG GGA TCT CG-3’)
Target sequences were amplified at 95°C for 10 min, followed by 40 cycles of 95°C for 15 s and 60°C for 1 min. HK-GAPD was used as endogenous normalization control. All assays were performed in triplicate and were calculated on the basis of ΔΔCt method. The n-fold change in mRNAs expression was determined according to the method of 2-ΔΔCT.
Lentiviral reporter assay (p-GreenFire1 Lenti-Reporter)
The cop-GFP and luciferase genes were cloned downstream of CSL/RBP-Jκ-response element, containing four CSL/RBP-Jκ binding motifs (pGreen Fire1-4xNotch-mCMV-EF1-Neo; System Biosciences, Mountain View, CA). For in vitro assays, stably transduced pancreatic CSCs were plated at 5-10,000 cells per well in 12-well plates and treated with various doses of drugs. After incubation, CSCs were analyzed for either GFP expression by fluorometer or luciferase activity by luminometer.
Viral production and infection
HEK 293T cells were transduced with plasmids of interest in the presence of lipofectamine. Viral supernatants were collected, mixed with PEG and concentrated by ultracentrifugation to produce virus stocks with titers of 1 × 108 to 1 × 109 infectious units per milliliter. Viral supernatant was collected for three days by ultracentrifugation and concentrated 100-fold. Titers were determined on HEK293T cells. Human pancreatic CSCs were transduced with a mixture of viral particles and polybrene with two rounds of infections.
Caspase-3/7 Assay
Cells (3 × 104 per well) were seeded in a 96-well plate with 200 μl culture medium. Approximately 16 h later, cells were treated with various doses of drugs. Casapse-3/7 activity was measured by a fluorometer as per manufacturer’s instructions (Invitrogen).
Statistical analysis
The mean and SD were calculated for each experimental group. Differences between groups were analyzed by one or two way ANOVA, followed by Bonferoni’s multiple comparison tests using PRISM statistical analysis software (GrafPad Software, Inc., San Diego, CA). Significant differences among groups were calculated at P < 0.05.
Results
EGCG inhibits the formation of primary and secondary tumor spheroids and colonies by pancreatic cancer stem cells
The ability of cells to self-renew is one of the main characteristics of CSCs. Therefore, we first sought to examine whether EGCG inhibits the growth of CSCs isolated from human primary pancreatic tumors by measuring sphere formation and cell viability in those spheroids. CSCs were grown in pancreatic cancer stem cell defined medium in suspension, and treated with EGCG. At the end of incubation period, primary and secondary spheroids in each well were photographed. EGCG inhibited the growth (size) of spheroids in suspension in a dose dependent manner (Fig. 1A). The spheroids from each treatment group were collected and resuspended for counting cell viability. EGCG inhibited CSC’s viability in primary and secondary spheroids in a dose-dependent manner (Fig. 1B). These data suggest that EGCG can be effective in inhibiting the growth of pancreatic CSCs.
Fig. 1.
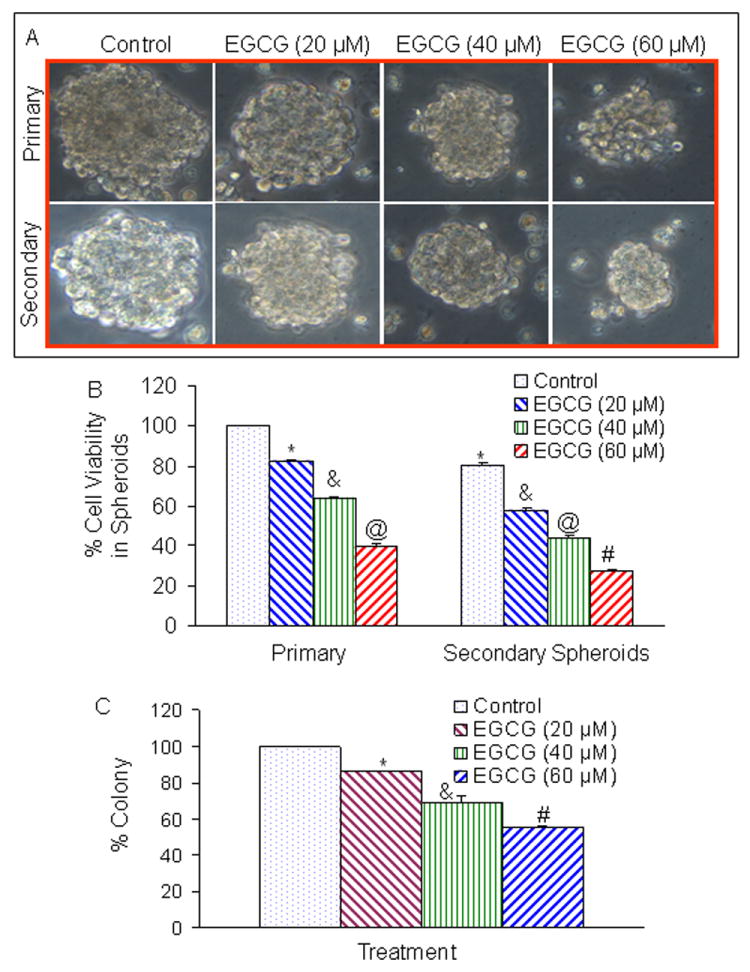
Effects of EGCG on tumor spheroids and cell viability of pancreatic cancer stem cells (CSCs). (A), Pancreatic CSCs were seeded in suspension and treated with EGCG (0-60 μM) for 7 days. Pictures of spheroids formed in suspension were taken by a microscope. (B), Pancreatic CSCs were seeded in suspension and treated with EGCG (0-60 μM) for 7 days. At the end of incubation period, sheroids were collected, and dissociated with Accutase (Innovative Cell Technologies, Inc.). For secondary spheroids, cells were reseeded and treated with EGCG (0-60 μM) for 7 days. Cell viability was measured by trypan blue assay. Data represent mean ± SD. *, &, @, or # = significantly different from respective controls, P < 0.05. (C), EGCG inhibits colony formation by CSCs. Pancreatic CSCs were seeded in soft agar and treated with various doses of EGCG and incubated at 4°C for 21 days. At the end of incubation period, colonies were counted. Data represent mean ± SD. *, & or # = significantly different from respective controls, P < 0.05.
Since EGCG inhibited the growth of tumor spheroid and cell viability of CSCs, we sought to examine the effects of EGCG on colony formation (Fig. 1C). Pancreatic CSCs were grown in agar, and treated with various doses of EGCG for 3 weeks. At the end of incubation period, numbers of colonies were counted. EGCG inhibited the growth of colonies in a dose-dependent manner. These data suggest that EGCG can be effective in inhibiting the self-renewal capacity of pancreatic CSCs.
EGCG induces caspase-3/7 activity and apoptosis, and inhibits the expression of Bcl-2, survivin and XIAP in human pancreatic CSCs
Since members of the IAP and Bcl-2 play important roles in cell survival and apoptosis27, we sought to examine the effects of EGCG on caspase-3/7 activity and apoptosis, and on the expression of Bcl-2, survivin and XIAP in pancreatic CSCs (Fig. 2). EGCG induced caspase-3/7 activity and apoptosis in pancreatic CSCs in a dose-dependent manner (Fig. 2A and B). Furthermore, EGCG inhibited the expression of Bcl-2, survivin and XIAP in pancreatic CSCs (Fig. 2C). These data suggest that EGCG can induce apoptosis in CSCs by engaging cell-intrinsic pathway of apoptosis.
Fig. 2.
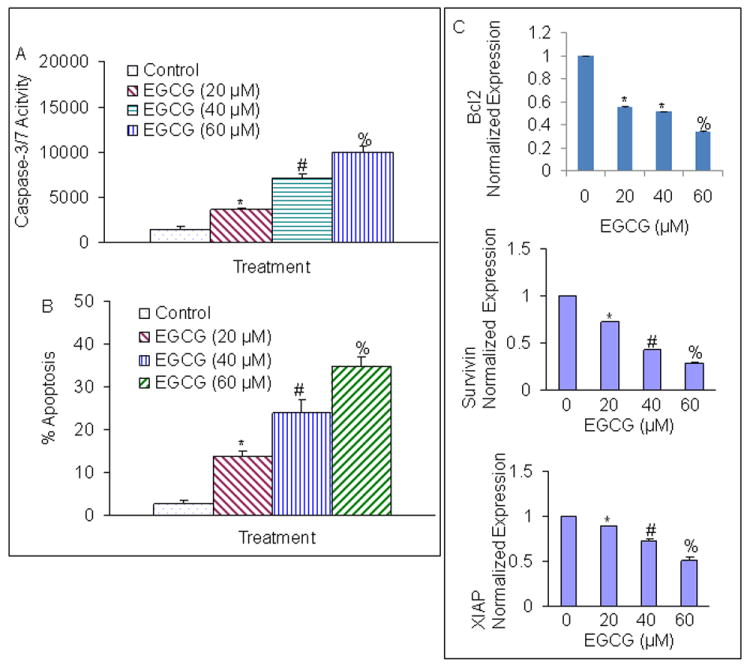
Regulation of caspase-3/7 activity, apoptosis and apoptosis-related proteins by EGCG on CSCs derived from human primary pancreatic tumors. (A), Regulation of caspase-3/7 activity by EGCG. CSCs were treated with EGCG (0-60 μM) for 24 h, and caspase-3/7 activity was measured as per manufacturer’s instructions. Data represent mean ± SD. *, # or % = significantly different from control, P < 0.05. (B), Regulation of apoptosis by EGCG. CSCs were treated with EGCG (0-60 μM) for 48 h, and apoptosis was measured by TUNEL assay. Data represent mean ± SD. *, # or % = significantly different from control, P < 0.05. (C), Regulation of apoptosis-related proteins. Pancreatic CSCs were treated with EGCG (0-60 μM) for 36 h. Real time PCR (q-RT-PCR) was performed to examine the expression of Bcl-2, survivin, XIAP, and GAPDH. Data represent mean ± SD. *, # or % = significantly different from control, P < 0.05.
EGCG inhibits the expression of pluripotency maintaining transcription factors, and inhibition of Nanog enhances the inhibitory effects of EGCG on pancreatic CSC’s self-renewal
Since Nanog, Sox-2, c-Myc and Oct-4 are required for maintaining pluripotency in stem cells28, 29, we sought to examine the effects of EGCG on the expression of these factors. As shown in Fig. 3A, EGCG inhibited the expression of Nanog, c-Myc and Oct-4 in pancreatic CSCs. However, EGCG has no effect on the expression of Sox-2.
Fig. 3.
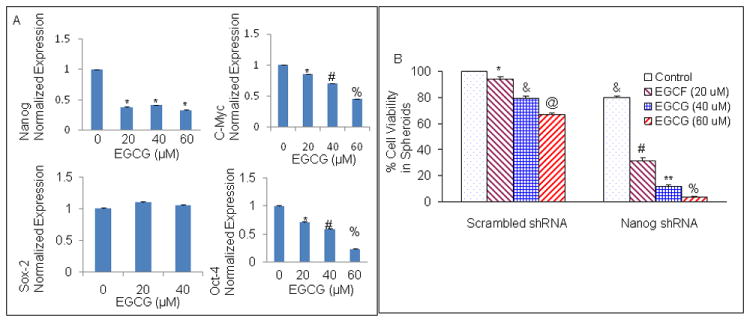
Regulation of pluripotency maintaining transcription factors by EGCG in pancreatic cancer stem cells. (A) Pancreatic CSCs were treated with EGCG (0-60 μM) for 36 h. At the end of incubation period, cells were harvested and the expression of Nanog, Sox-2, c-Myc and Oct-4 was measured by the q-RT-PCR. Data represent mean ± SD. *, #, or % = significantly different from respective controls, P < 0.05. (B), Nanog shRNA enhances the inhibitory effects of EGCG on CSC’s spheroid viability. Pancreatic CSCs were transduced with either scrambled shRNA or Nanog shRNA expressing lentiviral vector (pLKO.1), and cell lysates were collected and western blot analysis was performed using anti-Nanog antibody (data not shown). CSC/scrambled and CSC/Nanog shRNA were seeded as described above and treated with EGCG (0-60 μM). After 7 days, spheroids were collected and cell suspensions were prepared and viable cells were counted by trypan blue assay. Data represent mean ± SD. *, &, @, #, ** or % = significantly different from control, P < 0.05.
A high level of Nanog is a key regulator of embryonic stem cell (ESC) self-renewal and puripotency30. Nanog-deficient ES cells and embryos lose their pluripotency 31. Since Nanog is highly expressed in CSCs compared to normal cells32, we therefore examined whether inhibition of Nanog by shRNA can enhance the inhibitory effects of EGCG on cell viability in spheroids. Lentiviral mediated transduction of Nanog shRNA inhibited Nanog protein expression (data not shown). EGCG inhibited CSC’s viability in spheroids transduced with Nanog-scrambled shRNA in a dose-dependent manner (Fig. 3B). The inhibition of Nanog by shRNA further enhanced the antiproliferative effects of EGCG on CSCs. These data suggest that inhibition of Nanog may be an attractive target for regulation of self-renewal capacity of CSCs, and EGCG inhibits the factors required for maintaining pluripotency in CSCs.
EGCG inhibits Shh signaling pathway
We first sought to examine the effects of EGCG on Shh pathway by measuring the expression of Shh receptors (Patched-1, Patched-2 and Smothened) and effectors (Gli1 and Gli2) by qRT-PCR (Fig. 4). EGCG inhibited the expression of smoothened (SMO), Patched-1, and Patched-2 (Fig. 4A). Similarly, EGCG inhibited the expression of transcription factor Gli1 and Gli2 (Fig. 4B). Since Gli mediates the effects of Shh which play important roles in maintaining stemness and tumorigenesis11, we measured the Gli transcriptional activity by luciferase assay. As shown in Fig. 4B, EGCG inhibited Gli transcriptional activity in a dose-dependent manner. EGCG inhibited the expression of Ptch 1 and Ptch 2 because they are downstream targets of Gli.
Fig. 4.
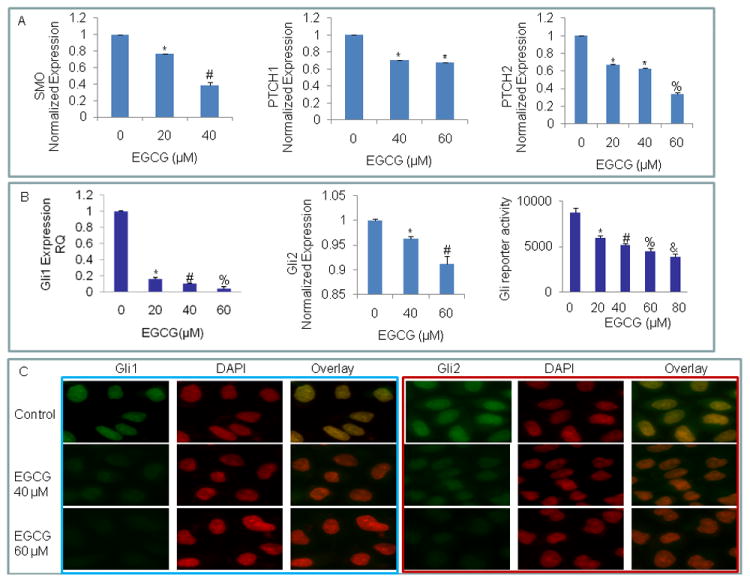
Inhibition of components of sonic hedgehog pathway, Gli transcription and nuclear translocation by EGCG. (A) Inhibition of components of sonic hedgehog pathway and Gli transcription. Pancreatic CSCs were treated with EGCG (0-60 μM) for 36 h. The expression of Smothened (Smo), patched 1 (PTCH1), patched 2 (PTCH2), was measured by q-RT-PCR. Data represent mean ± SD. *, #, or % = significantly different from respective controls, P < 0.05. (B), Inhibition of Gli1 and Gli2 expression and Gli transcription. Pancreatic CSCs were treated with EGCG (0-60 μM) for 36 h. The expression of Gli1 and Gli2 was measured by q-RT-PCR. Gli reporter activity. CSCs were transduced with Gli-responsive GFP/firefly luciferase viral particles (pGreen Fire1-Gli with EF1, System Biosciences). After transduction, culture medium was replaced and CSCs were treated with EGCG (0-60 μM) for 24 h. Gli-responsive reporter activity was measured by luciferase assay (Promega Corporation). Data represent mean ± SD. *, #, % or & = significantly different from respective controls, P < 0.05. (C), EGCG inhibits nuclear translocation of Gli1 and Gli2. Pancreatic CSCs were treated with or without EGCG (40 or 60 μM) for 24 h. At the end of incubation period, CSCs were fixed with paraformaldehyde, permeabilized with titron X100, and blocked with 5% normal goat serum. Cells were then treated with either anti-Gli1 or anti-Gli2 antibody, followed by secondary antibody plus DAPI. Stained cells were mounted and visualized under a fluorescence microscope. Blue fluorescence of DAPI was changed to red color for a better contrast.
We next examined the effects of EGCG on nuclear expression of Gli1 and Gli2 by immunohistochemistry (Fig 4C). EGCG inhibited the nuclear expression of Gli1 and Gli2 proteins. These data suggest that EGCG can inhibit pancreatic CSC characteristics by inhibiting Shh pathway which has been shown to play an important role in maintaining stemness and metastasis.
EGCG inhibits the expression of epithelial-mesenchymal transition (EMT) markers, migration, invation and TCF/LEF activity
During cancer metastasis, the mobility and invasiveness of cancer cells increase. To detach from neighboring cells and invade adjacent cell layers, carcinoma cells must lose cell-cell adhesion and acquire motility. The highly conserved EMT program has been implicated in dissemination of carcinoma cells from primary epithelial tumors33. Tumor progression is frequently associated with the downregulation of E-cadherin33, and upregulation of vimentin and several transcription factors including Snail, ZEB1 and Slug34. Cancer stem cells undergoing metastasis usually express EMT markers. We therefore examined the regulation of EMT markers by EGCG. As expected, EGCG inhibited the expression of Snail, ZEB1 and Slug as measured by q-RT-PCR (Fig. 5A).
Fig. 5.
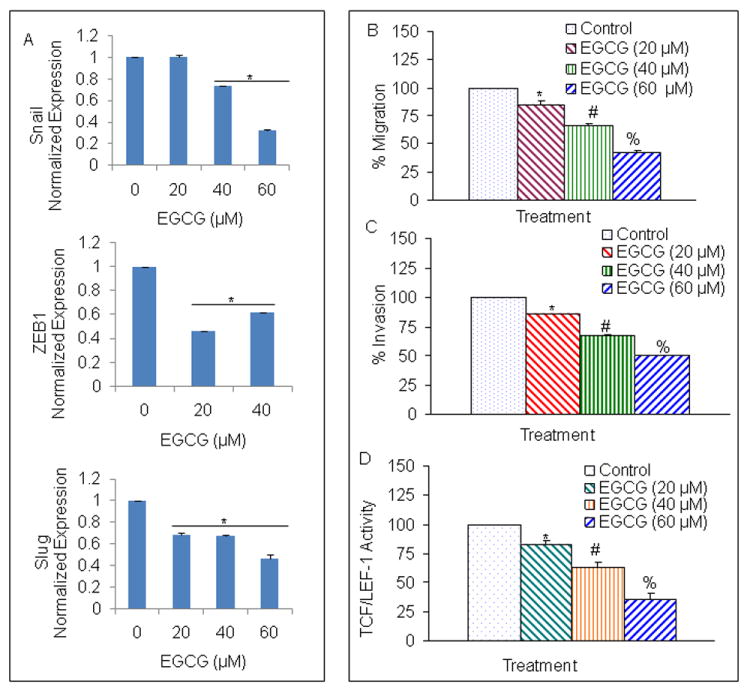
Regulation of epithelial mesenchymal transition factors, migration, invasion and TCF/LEF activity by EGCG in pancreatic CSCs. (A), Pancreatic CSCs were treated with EGCG (0-60 μM) for 48 h. At the end of incubation period, the expression of Snail, ZEB1 and Slug was measured by q-RT-PCR. Data represent mean ± SD. * = significantly different from respective controls, P < 0.05. (B), Transwell migration assay. Pancreatic CSCs were plated in the top chamber of the transwell and treated with EGCG (0-60 μM) for 24 h. Cells migrated to the lower chambered were fixed with methanol, stained with crystal violet and counted. Data represent mean ± SD. * # or % = significantly different from respective controls, P < 0.05. (C) Matrigel invasion assay. CSCs were plated onto the Matrigel-coated membrane in the top chamber of the transwell and treated with EGCG (0-60 μM) for 48 h. Cells invaded to the lower chambered were fixed with methanol, stained with crystal violet and counted. Data represent mean ± SD. *, # or % = significantly different from respective controls, P < 0.05. (D), Effects of EGCG on TCF-1/LEF activity. Pancreatic CSCs were transduced with TCF/LEF responsive GFP/firefly luciferase viral particles (pGreen Fire1-Gli with EF1, System Biosciences). Transduced CSCs were treated with EGCG (0-60) for 48 h and the GFP fluorescence was measured. Data represent mean ± SD. *, # or ** = significantly different from control, P < 0.05.
Since CSCs appear to play a significant role in early metastasis35, we sought to measure the effects of EGCG on migration and invasion of CSCs (Fig. 4B and C). EGCG inhibited cell migration and invasion of CSCs. These data suggest that EGCG can inhibit early metastasis of pancreatic CSCs.
Wnt/β-catenin signaling involves target gene activation by a complex of β-catenin with a T-cell factor (TCF) family member. Increased expression of β-catenin has been associated with enhanced transcriptional activation of TCF/LEF, invasion and migration by CSCs. We therefore examined the effects of EGCG on TCF/LEF transcriptional activity by luciferase assay (Fig. 5D). As expected, EGCG inhibited TCF/LEF activity in pancreatic CSCs. These data suggest that inhibition of EMT markers by EGCG could inhibit early metastasis of CSCs.
Quercetin enhances the effects of EGCG on spheroid and colony formation, apoptosis, invasion, migration, and the transcriptional activities of TCF/LEF and Gli in pancreatic CSCs
We have recently demonstrated that quercetin can enhance the inhibitory effects of sulforaphane on CSC’s characteristics25, 26. We therefore examined whether quercetin enhances the inhibitory effects of EGCG on self-renewal, migration and invasion of pancreatic CSCs (Fig. 6). EGCG inhibited cell viability in spheroids, colony formation, migration and invasion by CSCs in a dose-dependent manner (Fig. 6A and B). Quercetin, although effective alone, further enhanced the inhibitory effects of EGCG on cell viability, colony formation, migration and invasion. Furthermore, EGCG and quercetin alone induced apoptosis (Fig. 6C). Interestingly, EGCG synergizes with quercetin to induce apoptosis in pancreatic CSCs. These data suggest that EGCG can be used with quercetin to inhibit pancreatic CSC characteristics.
Fig. 6.
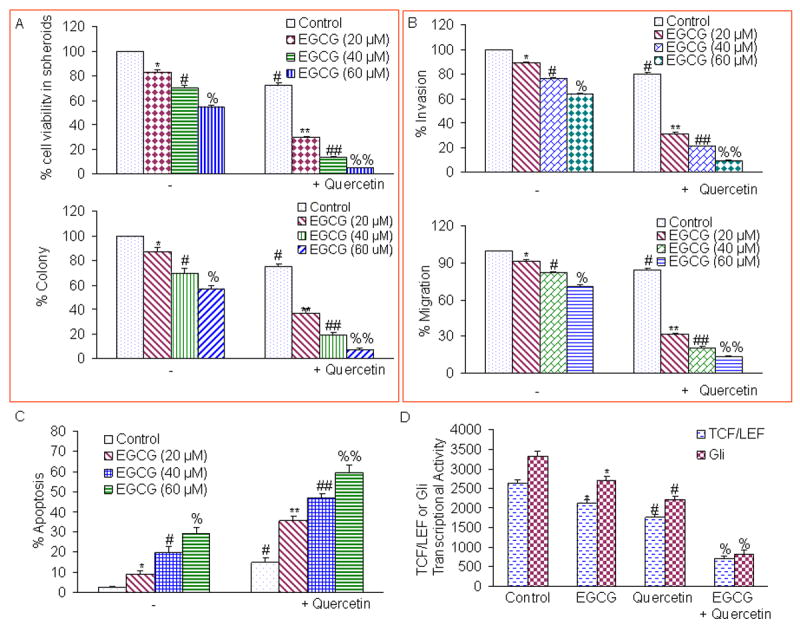
Quercetin synergizes with EGCG to inhibit self-renewal capacity, invasion, migration, and TCF/LEF and Gli transcriptional activities in pancreatic CSCs. (A), Effects of EGCG and quercetin on spheroid and colony formation. Upper Panel, Quercetin synergizes with EGCG to inhibit spheroid’s cell viability. CSCs were seeded in suspension and treated with EGCG (0-60 μM) with or without quercetin (20 μM) for 7 days. At the end of incubation period, all the spheroids were collected and resuspended. Cell viability was measured by trypan blue assay. Data represent mean ± SD. *, #, %, **, ##, or %% = significantly different from control, P < 0.05. Lower panel, Quercetin synergizes with EGCG to inhibit colony formation. Pancreatic CSCs were seeded in soft agar and treated with various doses of EGCG (0-60 μM) with or without quercetin (20 μM) and incubated at 4°C for 21 days. At the end of incubation period, colonies were counted. Data represent mean ± SD. *, #, %, **, ##, or %% = significantly different from control, P < 0.05. (B), Effects of EGCG and quercetin on invasion and migration. Upper panel, Matrigel invasion assay. CSCs were plated onto the Matrigel-coated membrane in the top chamber of the transwell and treated with EGCG (0-60 μM) with or without quercetin (20 μM) for 48 hrs. Cells invaded to the lower chambered were fixed with methanol, stained with crystal violet and counted. Data represent mean ± SD. *, #, %, **, ##, or %% = significantly different from control, P < 0.05. Lower panel, Transwell migration assay. Pancreatic CSCs were plated in the top chamber of the transwell and treated with EGCG (0-60 μM) with or without quercetin (20 μM) for 48 hrs. Cells migrated to the lower chambered were fixed with methanol, stained with crystal violet and counted. Data represent mean ± SD. *, #, %, **, ##, or %% = significantly different from respective controls, P < 0.05. (C), Quercetin synergizes with EGCG to induce apoptosis. CSCs were seeded in suspension and treated with EGCG (0-60 μM) with or without quercetin (20 μM) for 7 days. At the end of incubation period, all the spheroids were collected. Apoptosis was measured by TUNEL assay. Data represent mean ± SD. *, #, %, **, ##, or %% = significantly different from control, P < 0.05. (D), Effects of EGCG and quercetin on TCF/LEF and Gli transcriptional activities. Pancreatic CSCs were transduced with either lentivirus encoding TCF/LEF responsive GFP and luciferase genes or Gli-responsive GFP and luciferase genes. Transduced CSCs were treated with EGCG (40 μM) with or without quercetin (20 μM) for 48 hrs and the luciferase activity was measured. Data represent mean ± SD. *, #, or % = significantly different from respective control, P < 0.05.
Since enhanced levels of TCF/LEF and Gli transcriptional activities have been associated with CSC characteristics, we sought to measure the expression of TCF/LEF and Gli activities in pancreatic CSCs (Fig. 6D). EGCG inhibited both TCF/LEF and Gli transcriptional activities in pancreatic CSCs. These data suggest that EGCG synergizes with quercetin to inhibit self-renewal capacity of pancreatic CSCs by inhibiting TCF/LEF and Gli transcription factors.
Discussion
Our study demonstrates, for the first time, that cancer preventive agents EGCG and quercetin regulate self-renewal capacity and early metastasis (invasion and migration) of human pancreatic CSCs. Specifically, EGCG inhibits the self-renewal capacity of pancreatic CSCs by inhibiting the expression of pluripotency maintaining transcription factors (Nanog and Oct-4), EMT markers (twist-1, and Zeb-1), and the components of Shh pathway, and induces apoptosis by inhibiting Bcl-2 and XIAP and activating caspase-3. Furthermore, EGCG synergizes with quercetin to inhibit CSC’s characteristics by attenuating transcriptional activation of Gli and TCF/LEF. In addition, we have convincingly demonstrated that inhibition of Nanog may be an attractive target to enhance the anticancer activity of EGCG. Our data strongly suggest that EGCG alone or in combination with quercetin can be used for the management of pancreatic cancer by targeting CSCs.
Pancreatic adenocarcinoma arises from precursor lesions, pancreatic intraepithelial neoplasia (PanIN) that progress from PanIN 1 to 336. PanIN-1 lesions demonstrate K-ras mutations and Her2 overexpression. In PanIN-2, p16 mutations occur37. In PanIN-3, DPC4, P53 and BRCA2 mutations predominate. Shh expression is both a feature of PanIN and pancreatic adenocarcinoma implicating hedgehog as an early and late mediator of pancreatic cancer tumorigenesis. Shh protein expression correlated with TNM stages and distant metastasis. Moreover, the expression levels of Shh mRNA were higher in pancreatic adenocarcinoma tissues than that of the matched adjacent nontumorous tissues 38. The combined blockade of Shh and mTOR signaling together with standard chemotherapy was able to eliminate pancreatic CSCs. In a recent microarray study, nineteen altered genes of Hh pathway were identified and 100% of tumors had alterations in at least one of the Hh pathway genes39. Altered genes of the Hh pathway included GLI1, GLI3, BOC, SOX3, LRP2, TBX 5, BMPR2, and CREBBP. Other pathways involved in apoptosis, DNA damage control, regulation in G1/S phase transition, homophilic cell adhesion, integrin signaling, cJun N-terminal kinase signaling, K-ras signaling, regulation of invasion, small GTPase dependent signaling, TGFβ signaling and Wnt/Notch signaling were also altered39. In the present study, EGCG inhibited the components of Shh pathway and Gli transcription. Inhibition of Gli transcription can inhibit CSC’s self-renewal, invasion and migration. Further preclinical investigation of this promising approach may lead to the development of a novel therapeutic strategy to improve the devastating prognosis of patients with pancreatic cancer40.
EGCG inhibits the factors required for maintaining the pluripotency in CSCs. Nanog, Oct-4 and Sox-2 co-occupy and regulate their own promoters together with other developmental genes with diverse functions and collaborate to form an extensive regulatory circuitry including autoregulatory and feed-forward loops41. A high level of Nanog is a key regulator of embryonic stem cell (ESC) self-renewal and pluripotency. Nanog-deficient ES cells and embryos lose their pluripotency31. Nanog overexpression leads to the clonal expansion of ES cells through circumvention of the LIF-dependent Stat-3 pathway and sustained Oct-4 expression levels42. Genome-wide gene expression profiling shows that Nanog is expressed at high levels in testicular carcinoma in situ and germ cell tumors 43. In the present study, the inhibition of Nanog attenuated the self-renewal capacity of pancreatic CSCs, and enhanced the antiproliferative effects of EGCG. These data suggest that inhibition of Nanog expression could be a novel strategy to target CSCs.
β-Catenin is a cadherin-binding protein involved in cell-cell adhesion, which also functions as a transcriptional activator when complexed in the nucleus with members of the T-cell factor (TCF)/lymphoid enhancer factor (LEF) family of proteins. It has been reported that β-catenin protein expression was diminished by EGCG in several cellular compartments, but there was an accumulation of β-catenin in lysosomes, without a concomitant increase in transcriptional activity44. These results suggest that EGCG activated a pathway of β-catenin trafficking into lysosomes, thereby sequestering β-catenin and limiting the nuclear transport and further activation β-catenin/TCF target genes. Similarly in the present study, EGCG inhibited TCF/LEF activity in pancreatic CSCs. Inhibition of TCF/LEF activity by EGCG may regulate the ability of CSCs to self-renew and metastasize.
Epithelial-to-mesenchymal transition (EMT) is an embryonic program in which epithelial cells lose their characteristics and gain mesenchymal features. Accumulating evidence suggests that EMT plays an important role during malignant tumor progression. Furthermore, transformed epithelial cells can activate embryonic programs of epithelial plasticity and switch from a sessile, epithelial phenotype to a motile, mesenchymal phenotype. Induction of EMT can, therefore, lead to invasion of surrounding stroma, intravasation, dissemination and colonization of distant sites. It is believed that sustained metastatic growth requires the dissemination of a CSC from the primary tumor followed by its reestablishment in a secondary site. Thus, EMT can confer metastatic ability on carcinomas. In the present study, EGCG inhibited the expression of transcription factors (ZEB1, Snail and Slug) required for inducing EMT in pancreatic CSCs, suggesting a potential role of EGCG in early metastasis.
The combinations of chemopreventive agents have been shown to exert synergistic inhibitory effects on CSC characteristics25, 26. In the present study, EGCG synergizes with quercetin to inhibit the self-renewal capacity of pancreatic CSCs by attenuating transcriptional activities of Gli and TCF/LEF. Inhibition of Gli and TCF/LEF is expected to inhibit stem cell self-renewal, migration and invasion. Similarly, we have recently demonstrated that EGCG synergizes with quercetin to inhibit prostate CSC characteristics, invasion, migration and EMT26. In another study, quercetin inhibited growth of cancer stem cell-enriched xenografts associated with reduced proliferation, angiogenesis, cancer stem cell-marker expression and induction of apoptosis45.
Conclusions
We have demonstrated that EGCG inhibited self-renewal capacity of pancreatic CSCs, and these properties of EGCG can be enhanced with quercetin. EGCG inhibited the expression of transcription factors (Nanog and Oct-4) which are required for maintaining stem-cell pluripotency. Inhibition of Nanog could be considered as a novel strategy to enhance the biological effects of anticancer and chemopreventive agents or sensitize those cells which are resistant to chemotherapy and irradiation. Moreover, EGCG inhibited expression of proteins involved in the EMT, suggesting the blockade of signaling involved in early metastasis. Furthermore, combination of EGCG with quercetin had synergistic inhibitory effects on self-renewal capacity of pancreatic CSCs which correlated with Gli and TCF/LEF transcriptional activities. These data suggest that EGCG either alone or in combination with quercetin can be used for the prevention and/or treatment of pancreatic cancer.
Acknowledgments
We thank our lab members for critical reading of the manuscript. This work was supported in part by the grants from the National Institutes of Health (R01CA125262, RO1CA114469 and RO1CA125262-02S1).
Footnotes
Author Contributions
S-N.T., J.F., D.N., M.R: conception and design, collection and assembly of data, data analysis and integration, manuscript writing, and final approval of the manuscript; S.S., R.K.S.: conception and design, financial support, collection and assembly of data, data analysis and integration, manuscript writing, and final approval of the manuscript.
Disclosure of Potential Conflicts of Interest
The authors indicate no potential conflicts of interest.
References
- 1.Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010;60:277–300. doi: 10.3322/caac.20073. [DOI] [PubMed] [Google Scholar]
- 2.Pliarchopoulou K, Pectasides D. Pancreatic cancer: current and future treatment strategies. Cancer Treat Rev. 2009;35:431–6. doi: 10.1016/j.ctrv.2009.02.005. [DOI] [PubMed] [Google Scholar]
- 3.Magee CJ, Ghaneh P, Neoptolemos JP. Surgical and medical therapy for pancreatic carcinoma. Best Pract Res Clin Gastroenterol. 2002;16:435–55. doi: 10.1053/bega.2002.0317. [DOI] [PubMed] [Google Scholar]
- 4.Yeo TP, Hruban RH, Leach SD, Wilentz RE, Sohn TA, Kern SE, Iacobuzio-Donahue CA, Maitra A, Goggins M, Canto MI, Abrams RA, Laheru D, et al. Pancreatic cancer. Curr Probl Cancer. 2002;26:176–275. doi: 10.1067/mcn.2002.129579. [DOI] [PubMed] [Google Scholar]
- 5.Warshaw AL, Fernandez-del Castillo C. Pancreatic carcinoma. N Engl J Med. 1992;326:455–65. doi: 10.1056/NEJM199202133260706. [DOI] [PubMed] [Google Scholar]
- 6.Jones RJ, Matsui WH, Smith BD. Cancer stem cells: are we missing the target? J Natl Cancer Inst. 2004;96:583–5. doi: 10.1093/jnci/djh095. [DOI] [PubMed] [Google Scholar]
- 7.Reya T, Morrison SJ, Clarke MF, Weissman IL. Stem cells, cancer, and cancer stem cells. Nature. 2001;414:105–11. doi: 10.1038/35102167. [DOI] [PubMed] [Google Scholar]
- 8.Ischenko I, Seeliger H, Kleespies A, Angele MK, Eichhorn ME, Jauch KW, Bruns CJ. Pancreatic cancer stem cells: new understanding of tumorigenesis, clinical implications. Langenbecks Arch Surg. 2010;395:1–10. doi: 10.1007/s00423-009-0502-z. [DOI] [PubMed] [Google Scholar]
- 9.Shankar S, Nall D, Tang SN, Meeker D, Passarini J, Sharma J, Srivastava RK. Resveratrol inhibits pancreatic cancer stem cell characteristics in human and KrasG12D transgenic mice by inhibiting pluripotency maintaining factors and epithelial-mesenchymal transition. PLoS One. 2011;6:e16530. doi: 10.1371/journal.pone.0016530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jones RJ. Cancer stem cells-clinical relevance. J Mol Med. 2009;87:1105–10. doi: 10.1007/s00109-009-0534-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Varjosalo M, Taipale J. Hedgehog: functions and mechanisms. Genes Dev. 2008;22:2454–72. doi: 10.1101/gad.1693608. [DOI] [PubMed] [Google Scholar]
- 12.Beachy PA, Karhadkar SS, Berman DM. Tissue repair and stem cell renewal in carcinogenesis. Nature. 2004;432:324–31. doi: 10.1038/nature03100. [DOI] [PubMed] [Google Scholar]
- 13.Rohatgi R, Scott MP. Patching the gaps in Hedgehog signalling. Nat Cell Biol. 2007;9:1005–9. doi: 10.1038/ncb435. [DOI] [PubMed] [Google Scholar]
- 14.Osterlund T, Kogerman P. Hedgehog signalling: how to get from Smo to Ci and Gli. Trends Cell Biol. 2006;16:176–80. doi: 10.1016/j.tcb.2006.02.004. [DOI] [PubMed] [Google Scholar]
- 15.Olive KP, Jacobetz MA, Davidson CJ, Gopinathan A, McIntyre D, Honess D, Madhu B, Goldgraben MA, Caldwell ME, Allard D, Frese KK, Denicola G, et al. Inhibition of Hedgehog signaling enhances delivery of chemotherapy in a mouse model of pancreatic cancer. Science. 2009;324:1457–61. doi: 10.1126/science.1171362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Feldmann G, Habbe N, Dhara S, Bisht S, Alvarez H, Fendrich V, Beaty R, Mullendore M, Karikari C, Bardeesy N, Ouellette MM, Yu W, et al. Hedgehog inhibition prolongs survival in a genetically engineered mouse model of pancreatic cancer. Gut. 2008;57:1420–30. doi: 10.1136/gut.2007.148189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee CJ, Dosch J, Simeone DM. Pancreatic cancer stem cells. J Clin Oncol. 2008;26:2806–12. doi: 10.1200/JCO.2008.16.6702. [DOI] [PubMed] [Google Scholar]
- 18.Ishizawa K, Izawa-Ishizawa Y, Ohnishi S, Motobayashi Y, Kawazoe K, Hamano S, Tsuchiya K, Tomita S, Minakuchi K, Tamaki T. Quercetin glucuronide inhibits cell migration and proliferation by platelet-derived growth factor in vascular smooth muscle cells. J Pharmacol Sci. 2009;109:257–64. doi: 10.1254/jphs.08236fp. [DOI] [PubMed] [Google Scholar]
- 19.Nair HB, Sung B, Yadav VR, Kannappan R, Chaturvedi MM, Aggarwal BB. Delivery of anti-inflammatory nutraceuticals by nanoparticles for the prevention and treatment of cancer. Biochem Pharmacol. 2010 doi: 10.1016/j.bcp.2010.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Psahoulia FH, Drosopoulos KG, Doubravska L, Andera L, Pintzas A. Quercetin enhances TRAIL-mediated apoptosis in colon cancer cells by inducing the accumulation of death receptors in lipid rafts. Mol Cancer Ther. 2007;6:2591–9. doi: 10.1158/1535-7163.MCT-07-0001. [DOI] [PubMed] [Google Scholar]
- 21.Zhang L, Angst E, Park JL, Moro A, Dawson DW, Reber HA, Eibl G, Hines OJ, Go VL, Lu QY. Quercetin aglycone is bioavailable in murine pancreas and pancreatic xenografts. J Agric Food Chem. 2010;58:7252–7. doi: 10.1021/jf101192k. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Duraj J, Zazrivcova K, Bodo J, Sulikova M, Sedlak J. Flavonoid quercetin, but not apigenin or luteolin, induced apoptosis in human myeloid leukemia cells and their resistant variants. Neoplasma. 2005;52:273–9. [PubMed] [Google Scholar]
- 23.Knekt P, Jarvinen R, Seppanen R, Hellovaara M, Teppo L, Pukkala E, Aromaa A. Dietary flavonoids and the risk of lung cancer and other malignant neoplasms. Am J Epidemiol. 1997;146:223–30. doi: 10.1093/oxfordjournals.aje.a009257. [DOI] [PubMed] [Google Scholar]
- 24.Mi Y, Zhang C, Li C, Taneda S, Watanabe G, Suzuki AK, Taya K. Quercetin attenuates oxidative damage induced by treatment of embryonic chicken spermatogonial cells with 4-nitro-3-phenylphenol in diesel exhaust particles. Biosci Biotechnol Biochem. 2010;74:934–8. doi: 10.1271/bbb.90740. [DOI] [PubMed] [Google Scholar]
- 25.Srivastava RK, Tang SN, Zhu W, Meeker D, Shankar S. Sulforaphane synergizes with quercetin to inhibit self-renewal capacity of pancreatic cancer stem cells. Front Biosci (Elite Ed) 2011;3:515–28. doi: 10.2741/e266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tang SN, Singh C, Nall D, Meeker D, Shankar S, Srivastava RK. The dietary bioflavonoid quercetin synergizes with epigallocathechin gallate (EGCG) to inhibit prostate cancer stem cell characteristics, invasion, migration and epithelial-mesenchymal transition. J Mol Signal. 2010;5:14. doi: 10.1186/1750-2187-5-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Srivastava RK. TRAIL/Apo-2L: mechanisms and clinical applications in cancer. Neoplasia. 2001;3:535–46. doi: 10.1038/sj.neo.7900203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cavaleri F, Scholer HR. Nanog: a new recruit to the embryonic stem cell orchestra. Cell. 2003;113:551–2. doi: 10.1016/s0092-8674(03)00394-5. [DOI] [PubMed] [Google Scholar]
- 29.Kashyap V, Rezende NC, Scotland KB, Shaffer SM, Persson JL, Gudas LJ, Mongan NP. Regulation of stem cell pluripotency and differentiation involves a mutual regulatory circuit of the NANOG, OCT4, and SOX2 pluripotency transcription factors with polycomb repressive complexes and stem cell microRNAs. Stem Cells Dev. 2009;18:1093–108. doi: 10.1089/scd.2009.0113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jeter CR, Badeaux M, Choy G, Chandra D, Patrawala L, Liu C, Calhoun-Davis T, Zaehres H, Daley GQ, Tang DG. Functional evidence that the self-renewal gene NANOG regulates human tumor development. Stem Cells. 2009;27:993–1005. doi: 10.1002/stem.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mitsui K, Tokuzawa Y, Itoh H, Segawa K, Murakami M, Takahashi K, Maruyama M, Maeda M, Yamanaka S. The homeoprotein Nanog is required for maintenance of pluripotency in mouse epiblast and ES cells. Cell. 2003;113:631–42. doi: 10.1016/s0092-8674(03)00393-3. [DOI] [PubMed] [Google Scholar]
- 32.Bae KM, Su Z, Frye C, McClellan S, Allan RW, Andrejewski JT, Kelley V, Jorgensen M, Steindler DA, Vieweg J, Siemann DW. Expression of pluripotent stem cell reprogramming factors by prostate tumor initiating cells. J Urol. 2010;183:2045–53. doi: 10.1016/j.juro.2009.12.092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Thiery JP, Acloque H, Huang RY, Nieto MA. Epithelial-mesenchymal transitions in development and disease. Cell. 2009;139:871–90. doi: 10.1016/j.cell.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 34.Iwatsuki M, Mimori K, Yokobori T, Ishi H, Beppu T, Nakamori S, Baba H, Mori M. Epithelial-mesenchymal transition in cancer development and its clinical significance. Cancer Sci. 2010;101:293–9. doi: 10.1111/j.1349-7006.2009.01419.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mueller MT, Hermann PC, Heeschen C. Cancer stem cells as new therapeutic target to prevent tumour progression and metastasis. Front Biosci (Elite Ed) 2010;2:602–13. doi: 10.2741/e117. [DOI] [PubMed] [Google Scholar]
- 36.Wang Z, Li Y, Ahmad A, Banerjee S, Azmi AS, Kong D, Sarkar FH. Pancreatic cancer: understanding and overcoming chemoresistance. Nat Rev Gastroenterol Hepatol. 2011;8:27–33. doi: 10.1038/nrgastro.2010.188. [DOI] [PubMed] [Google Scholar]
- 37.Maitra A, Hruban RH. Pancreatic cancer. Annu Rev Pathol. 2008;3:157–88. doi: 10.1146/annurev.pathmechdis.3.121806.154305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dai J, Ai K, Du Y, Chen G. Sonic hedgehog expression correlates with distant metastasis in pancreatic adenocarcinoma. Pancreas. 2011;40:233–6. doi: 10.1097/MPA.0b013e3181f7e09f. [DOI] [PubMed] [Google Scholar]
- 39.Jones S, Zhang X, Parsons DW, Lin JC, Leary RJ, Angenendt P, Mankoo P, Carter H, Kamiyama H, Jimeno A, Hong SM, Fu B, et al. Core signaling pathways in human pancreatic cancers revealed by global genomic analyses. Science. 2008;321:1801–6. doi: 10.1126/science.1164368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mueller MT, Hermann PC, Witthauer J, Rubio-Viqueira B, Leicht SF, Huber S, Ellwart JW, Mustafa M, Bartenstein P, D’Haese JG, Schoenberg MH, Berger F, et al. Combined targeted treatment to eliminate tumorigenic cancer stem cells in human pancreatic cancer. Gastroenterology. 2009;137:1102–13. doi: 10.1053/j.gastro.2009.05.053. [DOI] [PubMed] [Google Scholar]
- 41.Rodda DJ, Chew JL, Lim LH, Loh YH, Wang B, Ng HH, Robson P. Transcriptional regulation of nanog by OCT4 and SOX2. J Biol Chem. 2005;280:24731–7. doi: 10.1074/jbc.M502573200. [DOI] [PubMed] [Google Scholar]
- 42.Chambers I, Colby D, Robertson M, Nichols J, Lee S, Tweedie S, Smith A. Functional expression cloning of Nanog, a pluripotency sustaining factor in embryonic stem cells. Cell. 2003;113:643–55. doi: 10.1016/s0092-8674(03)00392-1. [DOI] [PubMed] [Google Scholar]
- 43.Hoei-Hansen CE, Nielsen JE, Almstrup K, Sonne SB, Graem N, Skakkebaek NE, Leffers H, Rajpert-De Meyts E. Transcription factor AP-2gamma is a developmentally regulated marker of testicular carcinoma in situ and germ cell tumors. Clin Cancer Res. 2004;10:8521–30. doi: 10.1158/1078-0432.CCR-04-1285. [DOI] [PubMed] [Google Scholar]
- 44.Dashwood WM, Carter O, Al-Fageeh M, Li Q, Dashwood RH. Lysosomal trafficking of beta-catenin induced by the tea polyphenol epigallocatechin-3-gallate. Mutat Res. 2005;591:161–72. doi: 10.1016/j.mrfmmm.2005.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wong MY, Chiu GN. Simultaneous liposomal delivery of quercetin and vincristine for enhanced estrogen-receptor-negative breast cancer treatment. Anticancer Drugs. 2010;21:401–10. doi: 10.1097/CAD.0b013e328336e940. [DOI] [PubMed] [Google Scholar]


