Abstract
Objectives
To assess whether T cell activation independently predicts the extent of CD4+ T cell recovery and mortality in HIV-infected Ugandans initiating antiretroviral therapy (ART).
Design
Prospective cohort study
Methods
HIV-infected adults starting ART and achieving a plasma HIV RNA level (VL) <400 copies/ml by month 6 were sampled from the Uganda AIDS Rural Treatment Outcomes (UARTO) cohort in Mbarara, Uganda. CD4 count, VL, and the % activated (CD38+HLA-DR+) T cells were measured every 3 months.
Results
Of 451 HIV-infected Ugandans starting ART, most were women (70%) with median pre-ART values: age, 34 years; CD4 count, 135 cells/mm3; and VL, 5.1 log10 copies/ml. Of these, 93% achieved a VL<400 c/ml by month 6 and were followed for a median of 24 months, with 8% lost to follow up at 3 years. Higher pre-ART CD8+ T cell activation was associated with diminished CD4 recovery after year 1, after adjustment for pre-ART CD4 count, VL, and gender (P=0.017). Thirty-four participants died, 15 after month 6. Each 10 percentage-point increase in activated CD8+ T cells at month 6 of suppressive ART was associated with a 1.6-fold increased hazard of subsequent death after adjusting for pre-therapy CD4 count (P=0.048).
Conclusions
Higher pre-ART CD8+ T cell activation independently predicts slower CD4+ T cell recovery and higher persistent CD8+ T cell activation during ART-mediated viral suppression independently predicts increased mortality among HIV-infected Ugandans. Novel therapeutic strategies aimed at preventing or reversing immune activation during ART are needed in this setting.
Keywords: HIV, Uganda, Sub-Saharan Africa, T cell activation, Antiretroviral Therapy, Mortality
INTRODUCTION
Generalized immune activation is a hallmark of HIV infection and is established as an independent predictor of morbidity and mortality in the absence of antiretroviral therapy (ART) [1-6]. We and others have further demonstrated that while generalized T cell activation (assessed by the expression of CD38 and HLA-DR on CD8+ T cells) declines during suppressive ART, it persists at abnormal levels in the majority of HIV-infected individuals despite years of viral suppression and is associated with poor CD4+ T cell recovery [7-11]. Soluble markers of inflammation also remain abnormally elevated during suppressive ART [12, 13], and independently predict subsequent mortality and cardiovascular disease [14]. Thus, preventing the persistent inflammatory consequences of HIV infection during suppressive ART has emerged as a major challenge for the modern treatment era.
However, no study to date has linked cellular immune activation markers during treatment-mediated viral suppression to clinical outcomes. This is an important point since cellular markers of immune activation are increasingly being used as primary outcomes for pilot clinical trials of immune-based therapies in HIV infection given their better reproducibility and responsiveness than soluble inflammatory markers [15-18]. Furthermore, nearly all of the research evaluating the impact of immune activation on treatment-mediated immune recovery has been conducted in resource-rich settings and it remains unclear whether immune activation is a major determinant of CD4+ T cell recovery in resource-limited settings, where the vast majority of treated HIV-infected individuals now live. Conceivably, differences in host genetics, viral clade, and prevalent co-infections (i.e., tuberculosis, malaria, helminthes, etc) could alter the relationship between immune activation and clinical outcomes in this setting. To address these issues, we measured T cell activation levels in a cohort of HIV-infected Ugandans starting their first ART regimen both before and during the first year of treatment-mediated viral suppression and assessed its association with subsequent CD4+ T cell recovery and mortality in this setting.
METHODS
Participants
Ugandan participants were sampled from Uganda Antiretroviral Treatment Outcomes (UARTO), a cohort of 500 HIV-infected individuals starting their first non-nucleoside reverse transcriptase inhibitor (NNRTI)-based combination ART regimen at a University clinic in Mbarara with a mostly rural catchment area in western Uganda. Study visits are performed every three months, which include extensive interviews, CD4 counts and plasma HIV RNA levels, and biological specimen archiving. During the first year of therapy, T cell activation is measured on fresh specimens every 3 months.
Laboratory Measurements
Plasma HIV RNA levels were first assessed using the Roche Amplicor HIV Monitor 1.5 test (Roche, Branchburg, NJ, dynamic range: 400-750,000 copies/ml). In April, 2007, this assay was replaced by the Roche Cobas Taqman HIV-1 test v1.0 (Roche, Branchburg, NJ, dynamic range: 48-10,000,000 copies/ml).
T cell activation
Freshly isolated peripheral blood was analyzed for T cell activation using a Becton Dickinson FACSCalibur in the Cao laboratory at the Joint Clinical Research Center in Kampala. Whole blood was stained with fluorochrome-conjugated monoclonal antibodies: CD8-PerCP-Cy5.5, HLA-DR-FITC, CD38-PE and CD3-APC (BD Biosciences, San Jose). Analysis was performed with FlowJo software v6.3.3 (Treestar, Ashland, OR). T cell activation was assessed by the frequency of CD4+ and CD8+ T cells that co-expressed CD38 and HLA-DR. Preset gating was applied to all samples and was based on the expression of activation markers in HIV-seronegative Ugandans [19]. A median of 42,000 (IQR: 30,000-54,000) CD8+ T cell and 14,000 (9,000-20,000) CD4+ T cell events were acquired for all analyses.
Statistical Methods
For the cross-sectional comparisons, continuous variables were compared between groups with Wilcoxon ranksum tests. Dichotomous variables were compared between groups with chi-square and Fisher’s exact tests. Relationships between continuous variables were assessed with Spearman’s rank order correlation coefficients. Adjusted differences between groups were assessed with linear regression, calculating standard errors with heteroskedasticity-consistent covariance matrix estimators and log-transforming outcomes when necessary to satisfy model assumptions.
The rate and predictors of CD4+ T cell recovery among UARTO participants achieving a plasma HIV RNA level <400 copies/ml by month 6 of ART were assessed with linear mixed models (PROC MIXED in SAS) with square-root transformation of CD4+ T cell count to satisfy model assumptions. A three-piece segmented linear model (0-3 months, 3-12 months, and >12 months) was used to allow for changing slopes of CD4+ T cell recovery over time. Observations were censored at the time of a subsequent plasma HIV RNA level >1,000 copies/ml. Baseline predictors of the rate of CD4+ T cell recovery in each segment were assessed with time-by-interaction terms. Factors associated with the rate of early or late CD4+ T cell recovery in unadjusted analyses (P<0.10) were included as potential confounders in multivariable models. For interpretability, predicted values were back-transformed into the native scale for graphical interpretation [20]. Predictors of mortality were assessed with Kaplan-Meier methods and Cox proportional hazards models for adjusted analyses.
RESULTS
Characteristics of participants prior to initiating ART
Among the 451 treatment-naïve HIV-infected Ugandans contributing to these analyses, 70% were female, median age was 34 (IQR: 29 to 39) years, median pre-therapy CD4+ T cell count was 135 (IQR: 76-203) cells/mm3, and median plasma HIV RNA level was 5.1 (IQR: 4.5-5.5) log10 copies/ml (Table 1). Prior to starting ART, the median % activated (CD38+HLA-DR+) CD8+ T cells was 67% (IQR: 56% to 76%) and the median % activated CD4+ T cells was 32% (IQR: 22% to 45%). Higher pre-ART plasma HIV RNA levels were associated with both higher CD8+ T cell activation (rho: 0.12, P=0.011) and CD4+ T cell activation levels (rho: 0.29, P<0.001). While pre-ART CD4+ T cell activation levels were associated with lower CD4+ T cell counts (rho: −0.51, P<0.001), there was no evidence for an association between pre-ART CD8+ T cell activation levels and pre-ART CD4+ T cell counts (rho: −0.05, P=0.30).
Table 1.
Characteristics of Untreated HIV-infected Ugandans Initiating First ART Regimen
| Characteristic | Median (IQR) N=451 |
|---|---|
| Age, years | 34 (29 to 39) |
| Female gender, No. (%) | 316 (70) |
| CD4+ T cell count, cells/mm3 | 135 (76 to 203) |
| Plasma HIV RNA level, log10 copies/ml | 5.1 (4.5 to 5.5) |
| % CD38+ HLA-DR+ CD8+ T cells | 67 (56 to 76) |
| % CD38+ HLA-DR+ CD4+ T cells | 32 (22 to 45) |
Relationship between T cell activation and subsequent CD4+ T cell count recovery in ART-suppressed Ugandans
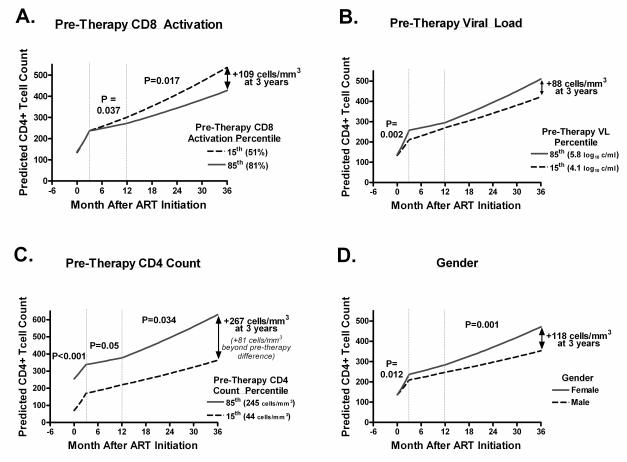
Of the 451 Ugandans initiating antiretroviral therapy, 93% (95% CI: 90%-95%) achieved a plasma HIV RNA level <400 copies/ml by month 6 of therapy and were included in the analyses of CD4+ T cell recovery, censoring observations for a plasma HIV RNA level >1,000 copies/ml. Median duration of follow up prior to censoring was 24 months (IQR: 14-33 months) and only 8% were lost to follow up at 3 years. Since the predictors of early (<3 months) and late (>12 months) CD4+ T cell recovery differ [21], we assessed predictors of CD4+ T cell recovery across 3 time segments using linear mixed models (0-3 months, 3-12 months, and >12 months). While there was no evidence for a relationship between pre-therapy CD4+ T cell activation or age and either early or late CD4+ T cell recovery in unadjusted analyses (P>0.51 for all), pre-therapy levels of CD8+ T cell activation, CD4+ T cell count, plasma HIV RNA level, and gender were all associated with the rate of either early or late CD4+ T cell recovery in unadjusted models (P<0.10, Table 2). After adjustment for gender, pre-treatment CD4+ T cell count, and plasma HIV RNA level, each 10 percentage-point increase in pre-therapy CD8+ T cell activation was associated with a mean 0.03 fewer square root-transformed CD4+ T cells/mm3 gained per month during months 3-12 (P=0.037) and a mean 0.02 fewer square root-transformed CD4+ T cells/mm3 gained per month after month 12 (P=0.017). The independent effect of pre-treatment CD8+ T cell activation on subsequent CD4+ T cell recovery can be visualized by plotting predicted CD4+ T cell count changes in two prototypic female participants, each with pre-treatment CD4+ T cell counts and plasma HIV RNA levels set to median values, but who have pre-treatment CD8+ T cell activation levels set to the 15th (51%) and 85th (81%) percentile values (Figure 1A). This adjusted difference in pre-treatment CD8+ T cell activation is associated with a difference of 109 CD4+ T cells/mm3 gained by year 3, and is comparable if not greater than the independent effect of pre-treatment plasma HIV RNA levels (Figure 1B), CD4+ T cell count (Figure 1C), and gender (Figure 1D) on subsequent CD4+ T cell recovery.
Table 2.
Predictors of CD4+ T Cell Recovery among HIV-infected Ugandans Receiving Suppressive ART
| Time Segment (months) |
Unadjusted | Adjusted | |||
|---|---|---|---|---|---|
| Characteristic | Mean Δ in square root CD4 Count (cells/mm3) |
P Value |
Mean Δ in square root CD4 Count (cells/mm3) |
P Value |
|
| Pre-therapy CD8+ T cell activation, | - | 0.09 | 0.82 | 0.06 | 0.57 |
| per 10 percentage-point increase | |||||
| Pre-therapy Plasma HIV RNA level, | - | −2.6 | 0.001 | 0.10 | 0.69 |
| per log10 copy/ml increase | |||||
| Pre-therapy CD4+ T cell count, | - | 5.4 | <0.001 | 4.0 | <0.001 |
| per 100 cell/mm3 increase | |||||
| Female Gender | - | 1.89 | 0.13 | 0.01 | 0.97 |
| Per Month | 0-3 | 1.02 | <0.001 | 0.96 | <0.001 |
| 3-12 | 0.15 | <0.001 | 0.14 | <0.001 | |
| 12 onward | 0.17 | <0.001 | 0.12 | <0.001 | |
| Pre-therapy CD8+ T cell activation × Month | 0-3 | −0.07 | 0.59 | −0.02 | 0.57 |
| 3-12 | −0.02 | 0.25 | −0.03 | 0.037 | |
| 12 onward | −0.01 | 0.09 | -0.02 | 0.017 | |
| Pre-therapy Plasma HIV RNA level × Month | 0-3 | 0.68 | 0.009 | 0.28 | 0.002 |
| 3-12 | −0.04 | 0.15 | −0.05 | 0.098 | |
| 12 onward | 0.09 | 0.58 | 0.03 | 0.10 | |
| Pre-therapy CD4+ T cell count × Month | 0-3 | −1.0 | <0.001 | −0.4 | <0.001 |
| 3-12 | −0.004 | 0.83 | −0.04 | 0.050 | |
| 12 onward | 0.008 | 0.46 | 0.03 | 0.034 | |
| Female Gender × Month | 0-3 | −0.38 | 0.38 | 0.32 | 0.012 |
| 3-12 | 0.07 | 0.12 | 0.02 | 0.64 | |
| 12 onward | 0.05 | 0.05 | 0.08 | 0.010 |
Figure 1. Independent Predictors of CD4+ T Cell Recovery in HIV-infected Ugandans Maintaining Treatment-mediated Viral Suppression.
Pre-therapy predictors of the rate of CD4+ T cell recovery were assessed in HIV-infected Ugandans with multivariable linear mixed models. CD4+ T cell recovery was modeled as a linear spline, allowing the rate of recovery to vary across three segments: baseline to month 3, month 3 to month 12, and month 12 onward. The plots depict the estimated mean CD4+ T cell changes for the 15th and 85th percentile values of each predictor in the multivariable model when setting all other significant predictors to median values. P values test whether the slope of CD4+ T cell recovery varies according to the predictor of interest within each spline segment and the mean adjusted difference in CD4+ T cell count at month 36 is reported for each predictor. For the prototypic female participant with a pre-therapy plasma HIV RNA level of 5.1 log10 copies/ml and a CD4+ T cell count of 135 cells/mm3, higher pre-therapy CD8+ T cell activation was associated with decreased rates of CD4+ T cell recovery after month 3 (A). Higher pre-treatment plasma HIV RNA levels predicted a more rapid rate of CD4+ T cell recovery in the first 3 months when adjusting for gender, pre-treatment CD4+ T cell count, and CD8+ T cell activation (B). Lower pre-treatment CD4+ T cell counts were associated with more rapid CD4+ T cell recovery in the first 12 months of antiretroviral therapy, but slower CD4+ T cell recovery thereafter, after adjustment for gender, pre-treatment plasma HIV RNA level, and CD8+ T cell activation (C). Women experienced a greater rate of CD4 recovery than men both during the first 3 months and after 12 months of antiretroviral therapy after adjusting for pre-treatment CD4+ T cell count, plasma HIV RNA level, and CD8+ T cell activation level (D).
We next assessed the relationship between T cell activation during treatment mediated viral suppression and subsequent CD4+ T cell recovery among participants with available T cell activation data at month 6 (n=267) and month 12 (n=216). After adjustment for pre-therapy plasma HIV RNA level, pre-therapy and month 6 CD4+ T cell count, and gender, there was no evidence for a relationship between the frequency of activated CD8+ T cells at month 6 of suppressive antiretroviral therapy and the rate of subsequent CD4+ T cell recovery (P=0.14). However, higher frequencies of activated CD8+ T cells at month 12 tended to predict a diminished rate of subsequent CD4+ T recovery after adjustment for pre-therapy plasma HIV RNA level, pre-therapy and month 12 CD4+ T cell count, and gender (P=0.075, Supplementary Table 1).
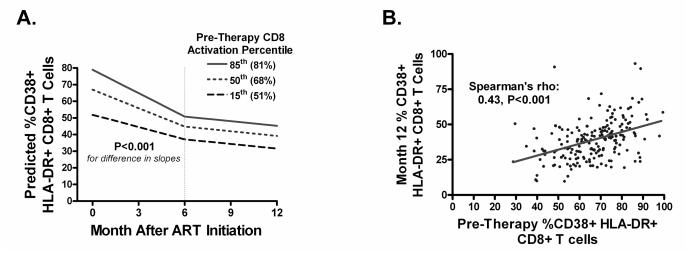
Changes in T cell activation during suppressive ART
Changes in the % activated CD8+ and CD4+ T cells were assessed every 12 weeks through week 48 among Ugandans achieving a plasma HIV RNA level <400 copies/ml by month 6, censoring observations for subsequent plasma HIV RNA levels >1000 copies/ml. CD8+ T cell activation declined more rapidly from baseline to month 6 (mean 3.8%/month, P<0.001) than from month 6 to 12 (mean 1.0%/month, P<0.001, P for interaction=0.001, Figure 2A). While the mean rate of decline in CD8+ T cell activation after month 6 was similar regardless of pre-therapy CD8+ T cell activation level (P for interaction = 0.68), the rate of decline in the first 6 months was more rapid for participants with higher pre-therapy CD8+ T cell activation levels (P for interaction=0.001). Despite early differences in the rate of decline in CD8+ T cell activation, those with higher pre-therapy CD8+ T cell activation levels continued to have higher CD8+ T cell activation levels at month 12 (rho: 0.43, P<0.001, Figure 2B). Higher month 12 CD8+ T cell activation was also associated with lower pre-treatment CD4+ T cell counts (rho: −0.25, P<0.001) and with higher pre-therapy plasma HIV RNA levels (rho: 0.16, P=0.020). In a multivariable model, higher month 12 T cell activation levels were predicted by both lower pre-treatment CD4+ T cell count (P=0.006) and higher pre-treatment CD8+ T cell activation (P<0.001), but no longer by pre-treatment plasma HIV RNA levels (P=0.67).
Figure 2. Changes in CD8+ T cell activation during ART-mediated viral suppression in HIV-infected Ugandans.
Changes in the frequency of activated (CD38+ HLA-DR+) CD8+ T cells was assessed over time with a linear mixed model among HIV-infected Ugandans achieving a plasma HIV RNA level <400 copies/ml by month 6 of ART, censoring observations for subsequent plasma HIV RNA levels >1000 copies/ml. Changes were modeled as a linear spline with a change point at month 6. Predicted changes in T cell activation from the linear mixed model are displayed when setting pre-therapy CD8+ T cell activation to 15th (51%), 50th (68%), and 85th (81%) percentile values, P values representing whether the average rate of decline was significantly different than zero (A). While the mean rate of decline in CD8+ T cell activation after month 6 (−1.0%/month, P<0.001) was similar regardless of pre-therapy CD8+ T cell activation level (P for interaction = 0.68), the rate of decline in the first 6 months was more rapid for participants with higher pre-therapy CD8+ T cell activation levels (−4.7%/mo for a participant with the 85th percentile value and −2.5%/month for a participant with the 15th percentile value, P for interaction=0.001) in the first 6 months of ART (P<0.001). Despite early differences in the rate of decline in CD8+ T cell activation, those with higher pre-therapy CD8+ T cell activation levels continued to have higher CD8+ T cell activation levels at month 12 (rho: 0.43, P<0.001, B).
Similar biphasic declines were observed in CD4+ T cell activation levels. Higher month 12 CD4+ T cell activation was also predicted by higher pre-therapy CD4+ T cell activation (rho: 0.57, P<0.001), higher pre-therapy plasma HIV RNA levels (rho: 0.21, P=0.002), and lower pre-therapy CD4+ T cell counts (rho: −0.44, P<0.001). In a multivariable model, while pre-treatment CD4+ T cell count and plasma HIV RNA level were no longer predictive (P>0.17 for both), higher pre-treatment CD4+ T cell activation continued to independently predict higher month 12 CD4+ T cell activation (P=0.001).
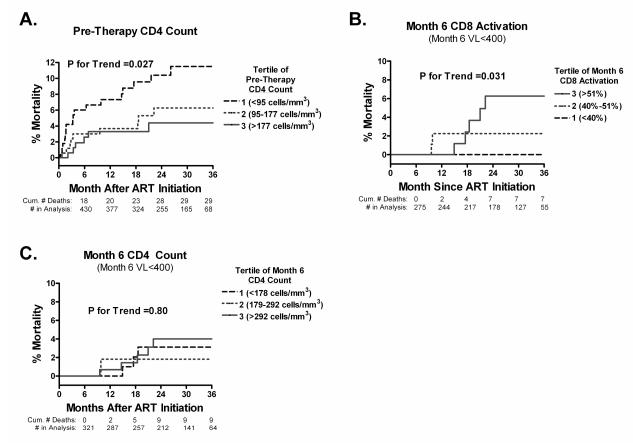
Predictors of mortality among HIV-infected Ugandans initiating ART
A total of 34 Ugandan participants died after initiating ART, with an overall mortality rate of 4% (95% CI: 2% to 6%) at 6 months, 5% (95% CI: 3% to 7%) at 12 months, and 7% (95% CI: 5% to 10%) at 24 months. Since most of these deaths occurred without autopsies or other antecedent diagnostic testing, the causes of death are unknown. Each 100 cell/mm3 increase in pre-therapy CD4+ T cell count was associated with a 51% (95% CI: 21%-69%) decreased hazard of death (P=0.003), largely driven by a high rate of death in the first 6 months of ART (Figure 3A). There was no evidence for a relationship between pre-therapy CD4+ or CD8+ T cell activation, plasma HIV RNA level, gender, or age and overall mortality during ART (P>0.12 for all). Fifteen participants died after month 6 of ART, 10 of whom had a confirmed plasma HIV RNA level <400 copies/ml at month 6 of therapy. These deaths occurred at a median of 18 months after treatment initiation (IQR: 15-21 months). Among participants with a plasma HIV RNA level <400 copies/ml at month 6 of ART, each 10% increase in month 6 CD8+ T cell activation was associated with a 1.65-fold increased hazard of subsequent death (P=0.029, Supplementary Table 2 and Figure 3B). Pre-therapy CD4+ T cell count was less significantly associated with mortality after month 6 of ART (HR: 0.43, P=0.081) and there was no evidence for a relationship between month 6 CD4+ T cell count and subsequent mortality (Figure 3C) among those with plasma HIV RNA levels <400 copies/ml. Each 10% increase in month 6 CD8+ T cell activation continued to be associated with a 1.6-fold increased hazard of death even after adjustment for pre-treatment CD4+ T cell count (P=0.048) or month 6 CD4 count (P=0.042).
Figure 3. Predictors of mortality during antiretroviral therapy among HIV-infected Ugandans.
Predictors of mortality were assessed using Kaplan-Meier methods among all HIV-infected Ugandans initiating ART as well as the subset achieving a plasma HIV RNA level <400 copies/ml by month 6 of ART. Predictors were assessed in tertiles. Lower pre-therapy CD4+ T cell counts predicted earlier death among all participants, largely driven by deaths occurring in the first 6 months of ART (P for trend=0.027, A). Among participants with plasma HIV RNA levels<400 copies/ml at month 6 of ART, higher CD8+ T cell activation predicted earlier subsequent mortality (P for trend=0.031, B). However, there was no evidence for a relationship between month 6 CD4+ T cell count and subsequent mortality among participants with plasma HIV RNA levels<400 copies/ml (P for trend=0.80, C).
DISCUSSION
Immune activation is associated with poor ART-mediated CD4+ T cell recovery among HIV-infected individuals in resource-rich settings, but little is known about its prognostic importance in resource-limited settings, where differences in host genetics, viral factors, and prevalent co-infections may modify these associations. Furthermore, no study has ever established a link between persistent T cell activation during suppressive ART and clinical morbidity or mortality. In the current study, we have established that higher pre-treatment CD8+ T cell activation (and a trend for month 12 T cell activation) independently predicts slower subsequent CD4+ T cell recovery. Lastly, we have established for the first time that higher persistent CD8+ T cell activation during early viral suppression independently predicts subsequent mortality in this setting, suggesting that immune activation is a major determinant of clinical outcomes in resource-limited settings and providing important clinical validation for these markers in the setting of viral suppression.
It has long been appreciated that HIV-uninfected individuals living in resource-limited settings in sub-Saharan Africa have higher frequencies of activated T cells than those living in resource-rich settings [22-27]. These differences have often been attributed to environmental factors (including prevalent helminthes infections [22, 25]), since Africans living in resource-rich countries for many years often have lower T cell activation levels than those living in Africa [24, 25], and Europeans living in sub-Saharan Africa often exhibit higher T cell activation levels than those living in Europe [24]. The mechanisms explaining the higher CD8+ T cell activation levels in Sub-Saharan Africans remains unclear, but may include prevalent co-infections (i.e., helminthes, subclinical malaria, etc.), or differences in host genetics or viral clade (though our group has not observed differences in T cell activation among HIV-infected Ugandans infected with clades A and D [28]).
Our finding that higher pre-therapy CD8+ T cell activation predicts slower CD4+ T cell recovery in HIV-infected Ugandans is consistent with several prior studies in North America and Africa linking T cell activation to poor CD4+ T cell recovery [7, 8, 10, 29]. However, only one of these prior studies established a temporal relationship between T cell activation and subsequent CD4+ T cell recovery [10]; thus, our current study adds important evidence supporting a causal role of immune activation in CD4+ T cell recovery. These data further suggest that the immune activation levels established prior to the initiation of therapy have a durable impact on the capacity for CD4+ T cell recovery long after viral suppression is achieved. The mechanisms explaining the durable impact of pre-treatment immune activation on CD4+ T cell recovery remain unclear, but could involve immune activation-induced lymphoid fibrosis, which fails to normalize during suppressive ART and has been shown to impair naïve and central memory CD4+ T cell homeostasis and CD4+ T cell recovery in this setting [30]. Alternatively, immune activation levels prior to ART may simply predict the extent of persistent immune activation during suppressive therapy. Our data provide less support for this model since the relationship between month 12 CD8+ T cell activation and subsequent CD4+ T cell recovery was not formally significant (P=0.075) and there was no evidence for a relationship between month 6 CD8+ T cell activation and subsequent CD4+ T cell recovery, though the much smaller number of participants contributing to these analyses resulted in comparatively lower statistical power and the beta coefficient for the pre-ART and month 12 CD8+ T cell activation-time interaction terms were identical (−0.2). Longitudinal data from larger cohorts of HIV-infected individuals maintaining treatment-mediated viral suppression will be necessary to resolve this issue. Lastly, it is possible that prevalent opportunistic infections at the time of ART initiation may have contributed to both higher levels of CD8+ T cell activation and poor CD4+ T cell recovery. However, given limited diagnostic testing available in the resource-constrained clinic from which the participants were sampled, we do not have comprehensive laboratory-confirmed opportunistic infection data available for this cohort. However, since pre-treatment CD8+ T cell activation primarily affected late CD4+ T cell recovery (after the first year of ART), it is unlikely that many opportunistic infections present at ART initiation would have remained untreated for over a year, affecting late CD4+ T cell recovery.
We also found that higher pre-treatment T cell activation and lower pre-treatment CD4+ T cell counts strongly predicted higher T cell activation during suppressive ART. This is an important observation as it may suggest an immunologic cost to delaying ART initiation in this setting. The fact that pre-treatment T cell activation strongly predicts T cell activation levels during suppressive ART also suggests that factors other than the extent of productive HIV replication are likely to contribute to T cell activation both in the presence and absence of suppressive ART. Studies in both resource-rich and resource-limited settings suggest that residual T cell activation during ART-mediated viral suppression may be at least partly explained by persistently abnormal levels of microbial translocation [31-33] and other chronic co-infections including CMV and/or other herpesviruses [16]. It is conceivable that the extent of immunodeficiency prior to ART initiation may be a major determinant of both microbial translocation and herpesvirus replication once ART-mediated viral suppression is achieved, but this has yet to be established in longitudinal studies. Prevalent co-infections in East Africa (i.e., helminthes, sub-clinical malaria, etc.) are also likely to contribute to immune activation in both the presence and absence of antiretroviral therapy. Host genetic factors may also modulate the inflammatory response to both productive HIV replication in the absence of ART and release of HIV from latently infected cells during suppressive ART. However, the host genetic determinants of immune activation have yet to be established in HIV infection.
Lastly, we observed for the first time that higher CD8+ T cell activation levels during early ART-mediated viral suppression independently predicts subsequent mortality. While low pre-therapy CD4+ T cell counts remains the strongest predictor of overall mortality in HIV-infected Ugandans, high persistent CD8+ T cell activation during suppressive ART is a more significant predictor of deaths occurring after the first 6 months of therapy. This association is unlikely to be mediated by incomplete viral suppression since this analysis was restricted to those with undetectable plasma HIV RNA levels at month 6 of ART. Furthermore, high persistent CD8+ T cell activation levels at month 6 are unlikely to be the immediate consequence of an undiagnosed fatal infection since the majority of deaths occurred at least 12 months after the T cell activation measurement. However, this observation is based on a relatively small number of deaths and we did not observe any evidence for a relationship between pre-ART CD8+ T cell activation and mortality (though the extent of pre-ART CD8+ T cell activation may have been in part driven by the degree of viremia, which was not associated with subsequent mortality in our study). While the relationship between month 6 CD8+ T cell activation and subsequent mortality will need to be confirmed in larger and/or longer studies, it suggests clinical relevance to the abnormally high T cell activation observed in treated HIV-infected Ugandans and suggests that additional interventions designed to decrease residual T cell activation may be required to fully restore health in this setting.
In summary, high pre-ART CD8+ T cell activation independently predicts a diminished rate of late CD4+ T cell recovery in HIV-infected Ugandans maintaining treatment-mediated viral suppression. Higher persistent CD8+ T cell activation during early treatment-mediated viral suppression also independently predicts earlier mortality. Thus, interventions designed to further reduce immune activation in this setting should be studied. Given the strong relationship between lower pre-treatment CD4+ T cell count and higher residual T cell activation, these observations also support the earlier initiation of ART in this setting.
Supplementary Material
ACKNOWLEDGEMENTS
This work was supported in part by the UCSF/Gladstone Center for AIDS Research (P30 AI27763, P30 MH59037), NIAID (AI055273, AI44595, AI065244, AI067854, and AI076981), the Center for AIDS Prevention Studies (P30 MH62246).
Footnotes
There is no conflict of interest for any of the investigations involved in this study.
REFERENCES
- 1.Giorgi JV, Lyles RH, Matud JL, Yamashita TE, Mellors JW, Hultin LE, et al. Predictive value of immunologic and virologic markers after long or short duration of HIV-1 infection. J Acquir Immune Defic Syndr. 2002;29:346–355. doi: 10.1097/00126334-200204010-00004. [DOI] [PubMed] [Google Scholar]
- 2.Giorgi JV, Hultin LE, McKeating JA, Johnson TD, Owens B, Jacobson LP, et al. Shorter survival in advanced human immunodeficiency virus type 1 infection is more closely associated with T lymphocyte activation than with plasma virus burden or virus chemokine coreceptor usage. J Infect Dis. 1999;179:859–870. doi: 10.1086/314660. [DOI] [PubMed] [Google Scholar]
- 3.Liu Z, Cumberland WG, Hultin LE, Kaplan AH, Detels R, Giorgi JV. CD8+ T-lymphocyte activation in HIV-1 disease reflects an aspect of pathogenesis distinct from viral burden and immunodeficiency. Journal of Acquired Immune Deficiency Syndromes and Human Retrovirology. 1998;18:332–340. doi: 10.1097/00042560-199808010-00004. [DOI] [PubMed] [Google Scholar]
- 4.Liu Z, Cumberland WG, Hultin LE, Prince HE, Detels R, Giorgi JV. Elevated CD38 antigen expression on CD8+ T cells is a stronger marker for the risk of chronic HIV disease progression to AIDS and death in the Multicenter AIDS Cohort Study than CD4+ cell count, soluble immune activation markers, or combinations of HLA-DR and CD38 expression. J Acquir Immune Defic Syndr Hum Retrovirol. 1997;16:83–92. doi: 10.1097/00042560-199710010-00003. [DOI] [PubMed] [Google Scholar]
- 5.Sousa AE, Carneiro J, Meier-Schellersheim M, Grossman Z, Victorino RM. CD4 T cell depletion is linked directly to immune activation in the pathogenesis of HIV-1 and HIV-2 but only indirectly to the viral load. J Immunol. 2002;169:3400–3406. doi: 10.4049/jimmunol.169.6.3400. [DOI] [PubMed] [Google Scholar]
- 6.Deeks SG, Kitchen CM, Liu L, Guo H, Gascon R, Narvaez AB, et al. Immune activation set point during early HIV infection predicts subsequent CD4+ T-cell changes independent of viral load. Blood. 2004;104:942–947. doi: 10.1182/blood-2003-09-3333. [DOI] [PubMed] [Google Scholar]
- 7.Hunt PW, Martin JN, Sinclair E, Bredt B, Hagos E, Lampiris H, et al. T Cell Activation Is Associated with Lower CD4+ T Cell Gains in Human Immunodeficiency Virus-Infected Patients with Sustained Viral Suppression during Antiretroviral Therapy. J Infect Dis. 2003;187:1534–1543. doi: 10.1086/374786. [DOI] [PubMed] [Google Scholar]
- 8.Gandhi RT, Spritzler J, Chan E, Asmuth DM, Rodriguez B, Merigan TC, et al. Effect of baseline- and treatment-related factors on immunologic recovery after initiation of antiretroviral therapy in HIV-1-positive subjects: results from ACTG 384. J Acquir Immune Defic Syndr. 2006;42:426–434. doi: 10.1097/01.qai.0000226789.51992.3f. [DOI] [PubMed] [Google Scholar]
- 9.Valdez H, Connick E, Smith KY, Lederman MM, Bosch RJ, Kim RS, et al. Limited immune restoration after 3 years’ suppression of HIV-1 replication in patients with moderately advanced disease. AIDS. 2002;16:1859–1866. doi: 10.1097/00002030-200209270-00002. [DOI] [PubMed] [Google Scholar]
- 10.Goicoechea M, Smith DM, Liu L, May S, Tenorio AR, Ignacio CC, et al. Determinants of CD4+ T cell recovery during suppressive antiretroviral therapy: association of immune activation, T cell maturation markers, and cellular HIV-1 DNA. J Infect Dis. 2006;194:29–37. doi: 10.1086/504718. [DOI] [PubMed] [Google Scholar]
- 11.Kaufmann GR, Zaunders JJ, Cunningham P, Cooper DA. Phenotypic analysis of CD8+ T lymphocytes in a cohort of HIV type 1-infected patients treated with saquinavir, ritonavir, and two nucleoside analogs for 1 year, and association with plasma HIV type 1 RNA. AIDS Research and Human Retroviruses. 1999;15:963–972. doi: 10.1089/088922299310476. [DOI] [PubMed] [Google Scholar]
- 12.French MA, King MS, Tschampa JM, da Silva BA, Landay AL. Serum immune activation markers are persistently increased in patients with HIV infection after 6 years of antiretroviral therapy despite suppression of viral replication and reconstitution of CD4+ T cells. J Infect Dis. 2009;200:1212–1215. doi: 10.1086/605890. [DOI] [PubMed] [Google Scholar]
- 13.Neuhaus J, Jacobs DR, Jr., Baker JV, Calmy A, Duprez D, La Rosa A, et al. Markers of inflammation, coagulation, and renal function are elevated in adults with HIV infection. J Infect Dis. 2010;201:1788–1795. doi: 10.1086/652749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kuller LH, Tracy R, Belloso W, De Wit S, Drummond F, Lane HC, et al. Inflammatory and coagulation biomarkers and mortality in patients with HIV infection. PLoS Med. 2008;5:e203. doi: 10.1371/journal.pmed.0050203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hatano H, Hayes TL, Dahl V, Sinclair E, Lee TH, Hoh R, et al. A Randomized, Controlled Trial of Raltegravir Intensification in Antiretroviral-treated, HIV-infected Patients with a Suboptimal CD4+ T Cell Response. J Infect Dis. 2011;203:960–968. doi: 10.1093/infdis/jiq138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hunt PW, Martin JN, Sinclair E, Epling L, Teague J, Jacobson MA, et al. Valganciclovir Reduces T Cell Activation in HIV-infected Individuals with Incomplete CD4+ T Cell Recovery on Antiretroviral Therapy. J Infect Dis. 2011 doi: 10.1093/infdis/jir060. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ganesan A, Crum-Cianflone N, Higgins J, Qin J, Rehm C, Metcalf J, et al. High Dose Atorvastatin Decreases Cellular Markers of Immune Activation Without Affecting HIV-1 RNA Levels: Results of a Double-blind Randomized Placebo Controlled Clinical Trial. J Infect Dis. 2011;203:756–764. doi: 10.1093/infdis/jiq115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Read SW, DeGrezia M, Ciccone EJ, DerSimonian R, Higgins J, Adelsberger JW, et al. The effect of leflunomide on cycling and activation of T-cells in HIV-1-infected participants. PLoS One. 2010;5:e11937. doi: 10.1371/journal.pone.0011937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Eggena MP, Barugahare B, Okello M, Mutyala S, Jones N, Ma Y, et al. T Cell Activation in HIV-Seropositive Ugandans: Differential Associations with Viral Load, CD4+ T Cell Depletion, and Coinfection. J Infect Dis. 2005;191:694–701. doi: 10.1086/427516. [DOI] [PubMed] [Google Scholar]
- 20.Gregoire TG, Lin QF, Boudreau J, Nelson R. Regression Estimation Following the Square-Root Transformation of the Response. For. Sci. 2008;54(6):597–606. [Google Scholar]
- 21.Hunt PW, Deeks SG, Rodriguez B, Valdez H, Shade SB, Abrams DI, et al. Continued CD4 cell count increases in HIV-infected adults experiencing 4 years of viral suppression on antiretroviral therapy. AIDS. 2003;17:1907–1915. doi: 10.1097/00002030-200309050-00009. [DOI] [PubMed] [Google Scholar]
- 22.Bentwich Z, Weisman Z, Moroz C, Bar-Yehuda S, Kalinkovich A. Immune dysregulation in Ethiopian immigrants in Israel: relevance to helminth infections? Clin Exp Immunol. 1996;103:239–243. doi: 10.1046/j.1365-2249.1996.d01-612.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kalinkovich A, Borkow G, Weisman Z, Tsimanis A, Stein M, Bentwich Z. Increased CCR5 and CXCR4 expression in Ethiopians living in Israel: environmental and constitutive factors. Clin Immunol. 2001;100:107–117. doi: 10.1006/clim.2001.5040. [DOI] [PubMed] [Google Scholar]
- 24.Clerici M, Butto S, Lukwiya M, Saresella M, Declich S, Trabattoni D, et al. Immune activation in africa is environmentally-driven and is associated with upregulation of CCR5. Italian-Ugandan AIDS Project. AIDS. 2000;14:2083–2092. doi: 10.1097/00002030-200009290-00003. [DOI] [PubMed] [Google Scholar]
- 25.Borkow G, Leng Q, Weisman Z, Stein M, Galai N, Kalinkovich A, et al. Chronic immune activation associated with intestinal helminth infections results in impaired signal transduction and anergy. J Clin Invest. 2000;106:1053–1060. doi: 10.1172/JCI10182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kassu A, Tsegaye A, Petros B, Wolday D, Hailu E, Tilahun T, et al. Distribution of lymphocyte subsets in healthy human immunodeficiency virus-negative adult Ethiopians from two geographic locales. Clin Diagn Lab Immunol. 2001;8:1171–1176. doi: 10.1128/CDLI.8.6.1171-1176.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Messele T, Abdulkadir M, Fontanet AL, Petros B, Hamann D, Koot M, et al. Reduced naive and increased activated CD4 and CD8 cells in healthy adult Ethiopians compared with their Dutch counterparts. Clin Exp Immunol. 1999;115:443–450. doi: 10.1046/j.1365-2249.1999.00815.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bousheri S, Burke C, Ssewanyana I, Harrigan R, Martin J, Hunt P, et al. Infection with different hiv subtypes is associated with CD4 activation-associated dysfunction and apoptosis. J Acquir Immune Defic Syndr. 2009;52:548–552. doi: 10.1097/QAI.0b013e3181c1d456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ruel T, Ssewanyana I, Achan J, Gasasira A, Kamya MR, Kekitiinwa A, et al. Dynamics of T cell activation accompanying CD4 recovery in antiretroviral treated HIV-infected Ugandan children. Clin Immunol. 2009;131:410–414. doi: 10.1016/j.clim.2009.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schacker TW, Nguyen PL, Beilman GJ, Wolinsky S, Larson M, Reilly C, et al. Collagen deposition in HIV-1 infected lymphatic tissues and T cell homeostasis. J Clin Invest. 2002;110:1133–1139. doi: 10.1172/JCI16413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cassol E, Malfeld S, Mahasha P, van der Merwe S, Cassol S, Seebregts C, et al. Persistent Microbial Translocation and Immune Activation in HIV-1-Infected South Africans Receiving Combination Antiretroviral Therapy. J Infect Dis. 2010;202:723–733. doi: 10.1086/655229. [DOI] [PubMed] [Google Scholar]
- 32.Jiang W, Lederman MM, Hunt P, Sieg SF, Haley K, Rodriguez B, et al. Plasma Levels of Bacterial DNA Correlate with Immune Activation and the Magnitude of Immune Restoration in Persons with Antiretroviral-Treated HIV Infection. J Infect Dis. 2009;199:1177–1185. doi: 10.1086/597476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Marchetti G, Bellistri GM, Borghi E, Tincati C, Ferramosca S, La Francesca M, et al. Microbial translocation is associated with sustained failure in CD4+ T-cell reconstitution in HIV-infected patients on long-term highly active antiretroviral therapy. Aids. 2008;22:2035–2038. doi: 10.1097/QAD.0b013e3283112d29. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.