Abstract
Background & Aims
We aimed to characterize offers of organs to candidates awaiting liver transplantation (LT).
Methods
We analyzed data from the United Network for Organ Sharing registry on all US LT candidates with non-fulminant disease who were offered livers from February 1 2005 to January 31, 2010 and ultimately received transplants. We excluded candidates with a final model for end-stage liver disease (MELD) scores <15. Livers were classified as high quality if they were from donors 18–50 years of age who were ≥170 cm tall, of non-black race, suffered brain death secondary to trauma, hepatitis C antibody-negative, not categorized as high risk by the Centers for Disease Control, and locally or regionally located.
Results
Of 33,389 candidates for LT, 20% died or were removed from the list and 64% were received LT; the median (interquartile range) number of liver offers for all candidates was 5 (range, 2–12). Of those who died or were removed from the list, 84% received ≥1 liver offer (s). Overall, 55% those who died or were removed from the list, and 57% of those who received LT, received ≥1 offer of a high-quality liver, when they had MELD scores ≥15 (P=.005). However, the proportion of last liver offers of high-quality to patients that underwent LT was twice that of patients that died or were removed from the list (28 vs 14%; P<0.001). Most liver offers (68%) were refused for reasons related to donor quality.
Conclusions
Most candidates for LT who died or were removed from the list received ≥1 offer of a liver beforehand, and 55% received ≥1 offer of a high-quality liver. These findings indicate that a substantial proportion of wait-list mortality results in part from declined, rather than lack of opportunity, for transplantation. Understanding the real-time factors involved in the complex decision to accept a liver offer is vital to reducing wait-list mortality for LT candidates.
Keywords: graft, availability, database analysis, surgery
Introduction
Under the current liver allocation system, patients are prioritized by their risk of wait-list mortality, as determined by their Model for End-Stage Liver Disease (MELD) score. Once a liver graft becomes available, it is offered to the candidate who is first on the wait-list. Depending upon the quality of the donor liver relative to the perceived need of the candidate, this liver offer may be accepted for transplantation. Alternatively, at the discretion of the center to which the graft was offered, this liver offer may be declined, in which case, it will be offered to the candidate who is next on the wait-list, and similarly down the wait-list, until it is finally accepted for transplantation. This donor offer process has been incompletely described. Therefore, we aimed to characterize liver offers from the perspective of the liver transplant wait-list candidate.
Methods
Study Population
We evaluated liver offers to all liver transplant candidates ≥18 years of age who were wait-listed for indications other than fulminant hepatic failure in the United States from February 1, 2005 through January 31, 2010 (n=53,659). We included only offers of livers that were ultimately transplanted. The study period was selected to correspond to the implementation of the “Share 15” policy, in which livers are first allocated locally and then regionally to wait-list candidates with Model for End-Stage Liver Disease (MELD) scores ≥15 before they are offered locally to candidates with MELD scores <15 (1). As a prior study has shown that patients with a MELD <15 may not derive survival benefit from liver transplantation versus continued waiting on the wait-list (2), only candidates with a MELD ≥15 at the time of their final wait-list event (e.g., death, removal, transplant) were included in the study. We excluded candidates listed with MELD exception points for reasons other than hepatocellular carcinoma as these patients fit into a heterogeneous group whose MELD score may not directly reflect their need for transplantation. Data on match-runs were obtained from the United Network for Organ Sharing/Organ Procurement Transplantation Network (UNOS/OPTN) as of June 30, 2010. Data on wait-list candidates and their donors were obtained from the Standard Transplant Analysis and Research files as of the same date.
Characteristics Evaluated
Wait-List Candidates
Demographic data on wait-list candidates included gender, race, age, and height at the time of listing. Etiologies of liver disease were grouped into the following categories: hepatitis C (HCV), hepatitis B (HBV), alcoholic liver disease, non-alcoholic fatty liver disease (NAFLD, including cryptogenic and non-alcoholic steatohepatitis), autoimmune (including autoimmune hepatitis, primary biliary cirrhosis, and primary sclerosing cholangitis), and other (including alpha-1-antitrypsin deficiency, Budd-Chiari, hemochromatosis, and others). Candidates listed with HCV in addition to other diagnoses were categorized as HCV. Only candidates listed as having “moderate” or “severe” ascites or encephalopathy in the UNOS/OPTN registry were classified as having ascites or encephalopathy in our study.
Donors
Donors were characterized by factors included in the donor risk index (3) including gender, race, age, height, HCV antibody status, Centers for Disease Control high risk for disease transmission status (CDC high risk), cause of death (e.g., trauma, anoxia, stroke, other), and donation after cardiac death (DCD). Split liver status was not considered, as this data was only available in the UNOS/OPTN registry for the transplanted liver (e.g., last offer) but not necessarily for the donor liver offers prior to the final acceptance.
Characteristics of each donor liver were available only at transplant. Therefore, we obtained characteristics of the donor offer by matching the donor identification number of the offer with the transplant donor identification number. Cutoffs for selected variables that were considered implausible for an adult recipient were as follows: recipient height <120 cm or > 240 cm, recipient weight <30 kg or >180 kg, donor height <100cm or >240 cm, donor weight <20kg or >180kg, cold ischemia time <1 hour or >24 hours, and warm ischemia time <10 minutes or >120 minutes. Observations including these implausible values were set to missing.
Liver offers were classified as “high-quality” if they were from donors between the ages of 18 and 50 years old, ≥170 cm in height, of non-black race, suffered brain death secondary to trauma, HCV-antibody negative, not CDC high risk, and locally or regionally located. A sensitivity analysis was performed to evaluate whether livers that were classified as “high-quality” behaved as expected with respect to graft failure rates.
Reasons for Refusal of Liver Offers
Refusal codes of liver offers were obtained from the UNOS/OPTN database. We categorized these refusal codes into six broad categories: 1) “Donor age or quality” (this was a single refusal code in the UNOS database), 2) “Donor size/weight”, 3) Other donor factors (e.g., “ABO”, “social history”, “positive serologic tests”, “organ preservation”, “organ anatomical damage or defect”, “organ-specific donor issue”), 4) Recipient readiness (e.g., “Patient’s condition improved”, “Patient ill, unavailable, refused, or temporarily unsuitable”, “Multiple organ transplant or different laterality is required”), 5) Programmatic (e.g., “heavy workload”, “operational at transplant center”, “exceeded one hour response time”, “surgeon unavailable”, “distance to travel or ship”), 6) Other (e.g., “multi-organ placement”, “directed donation”, etc.).
Statistical Analysis
Among candidates who received ≥1 liver offer(s), we compared dead/delisted with transplanted candidates using chi-square, Wilcoxon, and Kruskal-Wallis tests for categorical and continuous variables as appropriate. Parameter estimates were made using list-wise deletion under the assumption that missing data was missing completely at random. A sensitivity analysis to confirm that our classification of high quality livers behaved as expected was conducted using a Cox proportional hazards model for graft failure adjusted for MELD score, recipient age at transplant, and UNOS region. Analyses were performed using Stata®11.0 statistical software (College Station, Texas).
The institutional review board at the University of California-San Francisco approved the use of UNOS/OPTN registry data for this study.
Results
Of the 33,389 candidates included in our study, 6,737 (20%) died or became too sick for transplant (“dead/delisted”), 21,258 (64%) underwent deceased donor liver transplantation (“transplanted”), 2,030 (6%) were removed for other reasons, and 3,364 (10%) were still awaiting liver transplantation at the end of the study period. Of the dead/delisted, 5,680 (84%) received ≥1 liver offer(s) prior to death/delisting from the wait-list.
Characteristics of Wait-List Candidates
The characteristics of the dead/delisted with ≥1 offer(s) versus transplanted candidates, categorized by HCC exception point status, are shown in Table 1.
Table 1.
Characteristics of candidates awaiting liver transplantation, by wait-list outcome (dead/delisted versus transplanted) and by HCC exception point status
| Characteristics* | All Wait-List Candidates | Dead/Delisted with ≥1 offer(s) n=5,680 | Transplanted n=21,258 | ||
|---|---|---|---|---|---|
| n=33,389 | Without HCC n=4,916 | With HCC n=764 | Without HCC n=14,982 | With HCC n=6,276 | |
| Demographics | |||||
| Female gender | 32% | 40% | 23% | 33% | 22% |
| Age at listing in years | 54 (49–60) | 55 (49–60) | 56 (52–61) | 53 (48–59) | 56 (52–61) |
| African-American race | 9% | 8% | 10% | 10% | 9% |
| Etiology of liver disease | |||||
| Hepatitis C | 44% | 41% | 53% | 41% | 58% |
| Alcoholic | 16% | 16% | 11% | 19% | 8% |
| Non-alcoholic fatty liver | 7% | 7% | 3% | 9% | 4% |
| Cholestatic | 10% | 10% | 3% | 13% | 3% |
| Other | 23% | 26% | 30% | 18% | 27% |
| Disease Severity | |||||
| Ascites | 37% | 51% | 28% | 47% | 16% |
| Encephalopathy | 17% | 36% | 16% | 18% | 6% |
| MELD at listing | 16 (12–22) | 17 (13–23) | 13 (10–16) | 20 (15–26) | 11 (8–14) |
| MELD at first liver offer | 18 (15–25) | 17 (14–24) | 22 (14–22) | 20 (16–27) | 22 (18–22) |
| MELD at last liver offer | 22 (18–28) | 21 (16–32) | 22 (22–25) | 24 (19–32) | 22 (22–25) |
| MELD at wait-list event | 23 (19–29) | 27(19–38) | 24 (22–28) | 24 (19–31) | 22 (22–25) |
| Wait-list time, days | 130 (28–449) | 230 (56–733) | 233 (102–634) | 60 (13–244) | 110 (38–260) |
| Offers | |||||
| Offers per candidate | 5 (2–12) | 6 (2–14) | 6 (3–15) | 4 (2–9) | 6 (2–13) |
| Time from first offer to last offer, days | 65 (6–260) | 92 (9–383) | 96 (25–258) | 29 (1–159) | 71 (14–190) |
| Time from last offer to wait- list event, days | -- | 17 (4–57) | 24 (7–75) | -- | -- |
n (%) or median(interquartile range)
Without HCC
MELD score at listing, first offer, last offer, and final wait-list event was 17, 17, 21, and 27 for candidates who died/were delisted compared to 20, 20, 24, and 24 for candidates who were transplanted (p<0.001 between groups). Wait-list time was significantly longer (230 vs. 60 days) for the dead/delisted versus transplanted candidates (p<0.001 for both). While on the wait-list, the dead/delisted candidate group received a median of six liver offers compared to four offers for the transplanted group (p<0.001); the median time from first to last offer was 92 vs. 29 days for the dead/delisted versus transplanted candidates, respectively (p<0.001) [Table 1].
With HCC
MELD score at listing was 13 for the dead/delisted candidates and 11 for transplanted candidates (p<0.001). MELD score at the final wait-list event was higher for those who died/were delisted than for those who were transplanted (24 vs. 22; p<0.001). Both groups received a median of 6 liver offers (p=0.002) with a median of 96 vs. 71 days for dead/delisted and transplanted candidates, respectively (p<0.001) [Table 1].
Donor Characteristics of the Liver Offers
Donors of livers that were offered to dead/delisted versus transplanted candidates were clinically comparable but statistically different (p<0.001 for all) [Table 2]. Donors of the last liver offer to those who died/were delisted with ≥1 offer(s) compared to those who were transplanted were older (49 vs. 43 years), more likely to be African-American (16 vs. 13%), die from stroke (45 vs. 43%), DCD (12 vs. 6%), be nationally offered (25 vs. 12%), be HCV antibody positive (6 vs. 3%), or be categorized as CDC high risk (12 vs. 9%) [p<0.001; Table 2].
Table 2.
Characteristics of all liver offers versus last liver offer to candidates who died/were delisted compared to those who were transplanted.*
| Characteristics† | Among dead/delisted candidates with ≥1 offer(s) n=64,742 | Among transplanted candidates n=184,576 | ||
|---|---|---|---|---|
| All offers | Last offer | All offers | Last offer | |
| Donor age | 51 (36–65) | 49 (32–62) | 50 (35–64) | 43 (26–55) |
| Donor African-American race | 14% | 16% | 16% | 13% |
| Donor height | 170 (163–179) | 172 (163–179) | 173 (163–180) | 173 (165–180) |
| Cause of death | ||||
| Anoxia | 23% | 24% | 22% | 18% |
| Trauma | 24% | 27% | 26% | 37% |
| Stroke | 49% | 45% | 48% | 43% |
| Other | 4% | 4% | 4% | 3% |
| Donation after cardiac death | 13% | 12% | 12% | 6% |
| Nationally offered | 22% | 25% | 21% | 12% |
| Donor HCV antibody positive | 8% | 6% | 7% | 3% |
| CDC high risk | 12% | 12% | 11% | 9% |
| “High-quality”‡ | 11% | 14% | 13% | 28% |
Comparisons between the two groups (dead/delisted versus DDLT) were significant at p<0.001.
n (%) or median(interquartile range)
Livers were defined as high quality if they were from donors between the ages of 18 and 50 years old, ≥170 cm in height, of non-black race, suffered brain death secondary to trauma, HCV-antibody negative, not CDC high risk, and locally or regionally located.
It is of interest to examine the acceptance of organs that may be considered “high-quality”. As a point of reference, only 28% of transplanted livers were considered high-quality by these criteria. Among livers classified as high quality, 56% were accepted on the first offer compared to 39% of lower quality livers (p<0.001). As expected, adjusted risk of graft failure was significantly lower for high quality livers compared to the other livers (HR, 0.76; 95% CI, 0.71–0.81; p<0.001). In a subgroup analysis restricted to only the high-quality livers, adjusted graft failure for recipients who received a high quality liver that was refused at least once was similar to graft failure for recipients who received a high quality liver that was accepted on the first offer (HR, 0.95; 95% CI, 0.83–1.07; p=0.38).
Overall, 55% of dead/delisted and 57% of transplanted candidates received ≥1 high-quality liver offer(s) at a MELD ≥15 (p=0.005). Among all liver offers, high quality livers accounted for 11% of livers offered to died/delisted and 13% to transplanted candidates (p<0.001) [Table 2]. The proportion of last liver offers that were of high-quality to those who were transplanted (i.e., the accepted liver) was twice as high as the proportion to those who died/were delisted (28 vs. 14%) [p<0.001; Table 2].
Reasons for Liver Offer Refusal
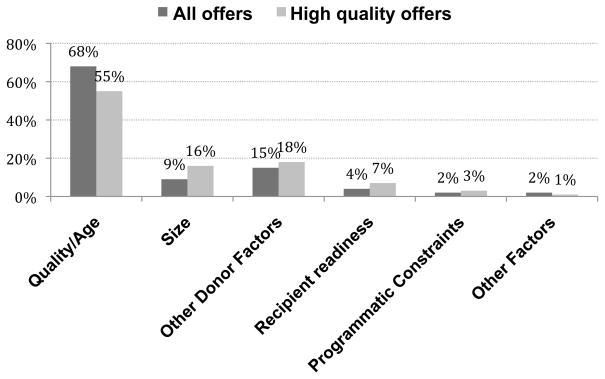
The majority (68%) of liver offer refusals for organs that were subsequently transplanted were reported under a single UNOS refusal code for “donor quality/age”. An additional 9% were refused for “size”, 15% for “other donor factors”, 4% for “recipient readiness”, and 4% for “programmatic” or “other” reasons. Compared to all liver offers, a greater proportion of the high quality offers (as previously defined) were refused for reasons related to size (16%) and recipient readiness (7%). Nevertheless, the majority of high quality liver offers were refused for reasons related to donor quality/age or other donor-related factors (73%) [Figure].
Figure.
Reasons for refusal of all versus high quality liver offers. Livers were defined as high quality if they were from donors between the ages of 18 and 50 years old, ≥170 cm in height, of non-black race, suffered brain death secondary to trauma, HCV-antibody negative, not CDC high risk, and locally or regionally located.
Among all livers refused at least once, 92% were transplanted into patients with the same or a lower MELD score than the first candidate to whom it was offered (e.g., 8% of livers were transplanted into patients with a higher MELD score than the first candidate).
Discussion
Integrating data regarding liver offers with donor and candidate characteristics, we found that the vast majority (84%) of wait-listed candidates who died or were delisted at a MELD ≥15 had received liver offers that were ultimately transplanted into lower priority candidates. More surprisingly, these candidates received not just one or two but a median of six liver offers during their time on the wait-list. These findings suggest that wait-list mortality is not simply a result of not having the opportunity for transplantation, as many of us assume. Rather, wait-list mortality appears to result from opportunities for transplantation that were declined.
Although each declination is associated with a specific refusal code, the dominant use of a single code “donor quality or age” – even when the liver appears to be of high quality – strongly suggests that the UNOS/OPTN data does not accurately or fully capture the true refusal reason. However, we found no difference in the risk of graft failure among high quality livers that were accepted on the first offer compared to high quality livers that were turned down at least once, suggesting that there were no systematic differences inherent to the fact that they were refused, despite the fact that the most common refusal code registered in UNOS was “donor age/quality. There are undoubtedly reasons in addition to a single unfavorable donor factor, such as recipient-donor interactions or the transplant centers’ philosophy about the utility of transplantation given certain donor and recipient characteristics, that drive the real-time decisions to decline a liver offer. The nuances of these refusals cannot be determined in the absence of more granular, center-level data.
Nevertheless, in considering the rhythm and patterns of daily clinical practice, we suggest that there are three major categories of factors that influence this complex and dynamic decision:
Candidate factors
For most patients with cirrhosis, the progression of liver disease is a nonlinear process characterized by sudden deteriorations related to events such as variceal hemorrhage, spontaneous bacterial peritonitis, or hepatorenal syndrome. During the course of these events, candidates may be perceived to have excess peri-operative and short-term post-transplant risk (e.g., sepsis) rendering the candidate temporarily or permanently unsuitable for transplantation necessitating refusal of liver offers. Second, a candidate may be actively listed but still completing the pre-transplant evaluation and therefore, are essentially not ready for transplantation. It is also a possibility that transplant clinicians perceive candidates to be “well enough” to wait for a better graft, especially when faced with an offer of lower quality. Finally, candidates, themselves, can refuse a transplant opportunity presented to them by their transplant physician secondary to logistical constraints, concerns regarding donor quality, or non-medical limitations.
Donor factors
The quality of donor livers has been decreasing over time (4), with only 29% of livers transplanted during our five-year study period meeting the definition of high quality. We have increasingly sophisticated knowledge of interactions between donor characteristics and recipient outcome, as seen with HCV-infected recipients receiving older donor livers (5) and possibly with DCD livers (6, 7). Finally, there is a strong mandate that any and all aspects of a donor that pose increased risk must be fully disclosed to and discussed with a potential recipient. This heightened awareness of all dimensions of donor risk likely discourages acceptance of non-ideal transplant opportunities.
Center factors
The current regulatory environment focused on transplant center performance and outcomes may, consciously or subconsciously, influence offer acceptance versus declination decisions. This may be especially relevant for low volume transplant centers for whom even a small number of poor outcomes associated with grafts that have been declined by other centers (most often for low quality) may make a relatively large difference in the center’s perceived performance (8). Moreover, the financial implications of transplant decisions are substantial, particularly if the candidate has high disease severity and/or the donor liver is of suboptimal quality (9). Finally, factors such as competition with other centers and availability of surgeons and operating room space may also play a role in the decision to accept offers at certain times.
Understanding the real-time factors involved in these decisions is vital to improving the wait-list process for liver transplant candidates. While some of the factors are beyond control, others can be managed. For example, centers should encourage wait-list candidates to complete their liver transplant work-up (e.g., cardiac testing, age-appropriate cancer screening, tuberculosis testing) as expeditiously as possible to avoid having liver offers turned down simply because they are not ready. Patients with a MELD ≥ 15 should be thoroughly educated about the unpredictability of death on the wait-list and their survival benefit of transplantation with any graft relative to continued waiting on the list (10) in order to reduce patient refusal of otherwise suitable organs. This education effort might include a prospective assessment of the individual candidate’s willingness to accept increased donor risk in exchange for more expeditious transplantation (thereby reducing wait-list mortality), as has been proposed by Volk et al (11). Given the increasing risk profile of deceased liver donors, efforts should be made in the transplant community to reduce the stigma associated with non-ideal livers and set realistic expectations for wait-listed candidates. Perhaps, liver offer acceptance practices should be taken into consideration in assessing center performance, as a means of encouraging centers to accept more livers for their candidates.
In conclusion, our data demonstrate that the current liver allocation system has provided one or more transplant opportunities to nearly all candidates prior to death/delisting. Therefore, simply increasing the availability of deceased donor livers or the number of offers may not substantially reduce wait-list mortality. It is worth noting that all centers/physicians are provided with the same information about the donors, so differential decisions regarding declining or accepting a liver offer cannot solely be based on donor factors. Efforts must be directed at reducing offer declination rates through identification of modifiable barriers that may exist at multiple levels – candidate, physician, center, as well as donor – to proceeding with timely transplantation to avoid death or delisting as the terminal wait-list event.
Acknowledgments
Grant support: This project was supported by the National Institute of Diabetes and Digestive and Kidney Diseases (T32 DK060414 JCL) and the University of California San Francisco Liver Center (P30 DK026743 SF, JPR).
Abbreviations
- CDC
Centers for Disease Control
- DCD
donation after cardiac death
- DSA
donation service area
- IQR
interquartile range
- MELD
model for end-stage liver disease
- UNOS/OPTN
United Network for Organ Sharing/Organ Procurement and Transplantation Network
Footnotes
Disclosures: The authors of this manuscript have no conflicts of interest to disclose as described by Gastroenterology.
Transcript Profiling: Not applicable
Writing Assistance: None
Author Contributions:
- Jennifer Lai – study concept and design, acquisition of data, analysis and interpretation of data, drafting of the manuscript, critical revision of the manuscript for important intellectual content, statistical analysis. Dr. Lai had full access to all of the data and takes full responsibility for the veracity of the data and statistical analysis.
- Sandy Feng – study concept and design, interpretation of data, drafting of the manuscript, critical revision of the manuscript for important intellectual content, study supervision
- John Roberts – study concept and design, analysis and interpretation of data, drafting of the manuscript, critical revision of the manuscript for important intellectual content, study supervision
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Organ Procurement and Transplantation Network. [Accessed July 8, 2011];Policy 3.6: Allocation of Livers. http://optntransplanthrsagov/PoliciesandBylaws2/policies/pdfs/policy_8pdf.
- 2.Schaubel DE, Guidinger MK, Biggins SW, Kalbfleisch JD, Pomfret EA, Sharma P, et al. Survival benefit-based deceased-donor liver allocation. Am J Transplant. 2009 Apr;9(4 Pt 2):970–81. doi: 10.1111/j.1600-6143.2009.02571.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Feng S, Goodrich NP, Bragg-Gresham JL, Dykstra DM, Punch JD, DebRoy MA, et al. Characteristics associated with liver graft failure: the concept of a donor risk index. Am J Transplant. 2006 Apr;6(4):783–90. doi: 10.1111/j.1600-6143.2006.01242.x. [DOI] [PubMed] [Google Scholar]
- 4.Thuluvath PJ, Guidinger MK, Fung JJ, Johnson LB, Rayhill SC, Pelletier SJ. Liver transplantation in the United States, 1999–2008. Am J Transplant. 2010 Apr;10(4 Pt 2):1003–19. doi: 10.1111/j.1600-6143.2010.03037.x. [DOI] [PubMed] [Google Scholar]
- 5.Berenguer M, Prieto M, San Juan F, Rayon JM, Martinez F, Carrasco D, et al. Contribution of donor age to the recent decrease in patient survival among HCV-infected liver transplant recipients. Hepatology. 2002 Jul;36(1):202–10. doi: 10.1053/jhep.2002.33993. [DOI] [PubMed] [Google Scholar]
- 6.Hernandez-Alejandro R, Croome KP, Quan D, Mawardi M, Chandok N, Dale C, et al. Increased risk of severe recurrence of hepatitis C virus in liver transplant recipients of donation after cardiac death allografts. Transplantation. 2011 Sep 27;92(6):686–9. doi: 10.1097/TP.0b013e31822a79d2. [DOI] [PubMed] [Google Scholar]
- 7.Mathur AK, Heimbach J, Steffick DE, Sonnenday CJ, Goodrich NP, Merion RM. Donation after cardiac death liver transplantation: predictors of outcome. Am J Transplant. 2010 Nov;10(11):2512–9. doi: 10.1111/j.1600-6143.2010.03293.x. [DOI] [PubMed] [Google Scholar]
- 8.Halldorson JB, Paarsch H, Segre A, Roberts JP. The Influence of Inter-Center Competition on Liver Transplant Outcomes (abstract) Hepatology. 2011;54:360A–1455A. [Google Scholar]
- 9.Salvalaggio PR, Dzebisashvili N, MacLeod KE, Lentine KL, Gheorghian A, Schnitzler MA, et al. The interaction among donor characteristics, severity of liver disease, and the cost of liver transplantation. Liver Transpl. 2011 Mar;17(3):233–42. doi: 10.1002/lt.22230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Merion RM, Schaubel DE, Dykstra DM, Freeman RB, Port FK, Wolfe RA. The survival benefit of liver transplantation. Am J Transplant. 2005 Feb;5(2):307–13. doi: 10.1111/j.1600-6143.2004.00703.x. [DOI] [PubMed] [Google Scholar]
- 11.Volk ML, Tocco RS, Pelletier SJ, Zikmund-Fisher BJ, Lok AS. Patient decision making about organ quality in liver transplantation. Liver Transpl. 2011 Dec;17(12):1387–93. doi: 10.1002/lt.22437. [DOI] [PMC free article] [PubMed] [Google Scholar]