Abstract
We present the interesting case of a 15-year old boy with a monophasic synovial sarcoma (MSS) of the mediastinum, which was infiltrating the right heart chambers and the inferior vena cava (IVC). A radical excision was performed, with extensive reconstruction of the heart, under deep hypothermic circulatory arrest. Radical surgical excision is considered to be the treatment of choice for these lesions, as chemotherapy and radiotherapy have little effect. Unfortunately, the patient and his parents refused any further consultation with an oncologist and, although there was no recurrence at 12 months following the procedure, at 24 months we were informed of his death due to the tumour appearing on the left cardiac chambers with subsequent multi-organ failure.
Keywords: Monophasic synovial sarcoma, Radical surgical excision
INTRODUCTION
We present the case of a 15-year old boy with no previous medical history, who was referred to our unit with a large mediastinal mass invading the right heart chambers and inferior vena cava (IVC), which proved to be a monophasic monosynovial sarcoma. Current treatment options mainly involve radical surgical excision, due to the questionable benefit of chemotherapy or radiotherapy.
CASE REPORT
The patient was investigated following repeated episodes of shortness of breath, which became progressively worse. A chest X-ray was performed, followed by a computed tomography (CT) scan. These identified a large mass, originating from the anterior mediastinum, in contact with the right heart chambers, indicating infiltration and compression, and also encircling the IVC. The mass also filled the space between the right hemidiaphragm and the lower segments of the right lower lobe. A magnetic resonance imaging (MRI) scan was carried out confirming the CT, but the most troublesome finding was infiltration of the IVC. Finally an echocardiogram (ECHO) was performed, to complete the diagnosis.
The patient was transferred to a thoracic department and, as far as we are aware, there was no multidiscipline meeting, the decision to operate resting solely on the thoracic surgeon. A right thoracotomy was performed, which was subsequently stopped, as the lesion was considered inoperable in the absence of extracorporeal circulatory support, which was not available. The patient had an uneventful postoperative period.
He was transferred to our hospital on the 17th postoperative day. After discussing the treatment options with his parents, he was prepared for surgery. A median sternotomy was performed. The mass appeared to be in contact with the right heart chambers, with extension and infiltration of the structures, particularly the right atrium. The mass was infiltrating the pulmonary veins, the pericardium and the IVC and it appeared to extend to the space between the right hemidiaphragm—which appeared to be affected—and the right lower lobe of the lung. There were no signs of the lesion infiltrating the left heart chambers. Finally, the right phrenic nerve was also affected (Fig. 1). For the complete and radical resection of the tumour (Fig. 2a), we used deep hypothermic circulatory arrest under cardiopulmonary bypass. The aorta was cannulated in the usual manner and the superior vena cava (SVC) was cannulated with the cannula facing the right atrium (RA). Cardiopulmonary bypass (CPB) was initiated, and after decompression of the heart, we placed a second cannula to the RA and redirected the SVC cannula in a cephalad position. The heart was arrested, and a left ventricular (LV) vent was installed, followed by cooling the patient to 18°C. We then proceeded with the tumour excision. The excised mass was 14 × 8, 5 × 6 cm (Fig. 2b) and included three-quarters of the right atrium, the atrial septum with a small part of the left atrium, the supradiaphragmatic portion of the IVC, and the adjacent pericardium. Reconstruction followed, using autologous pericardium to rebuild the right hemidiaphragm, the left atrium and the atrial septum; a Peri-Guard® patch (Synovis Surgical Innovations, St. Paul MN, USA) was used to repair the IVC. We then redirected the IVC cannula and re-instituted CPB. Finally, we used the rest of the Peri-Guard® patch to reconstruct the right atrium (Fig. 2c).
Figure 1:
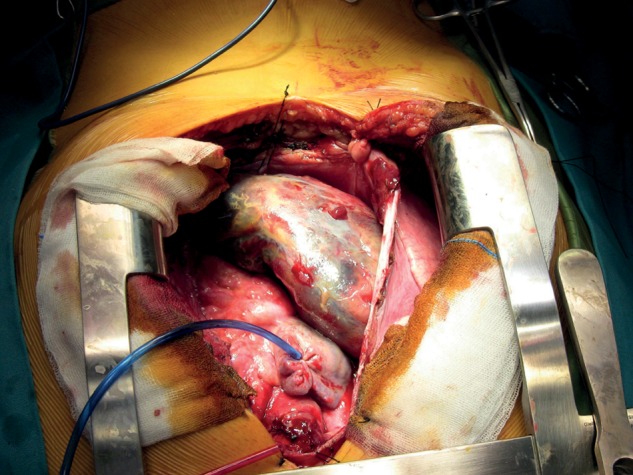
There were no signs of the lesion infiltrating the left heart chambers and, finally, the right phrenic nerve was also affected.
Figure 2:
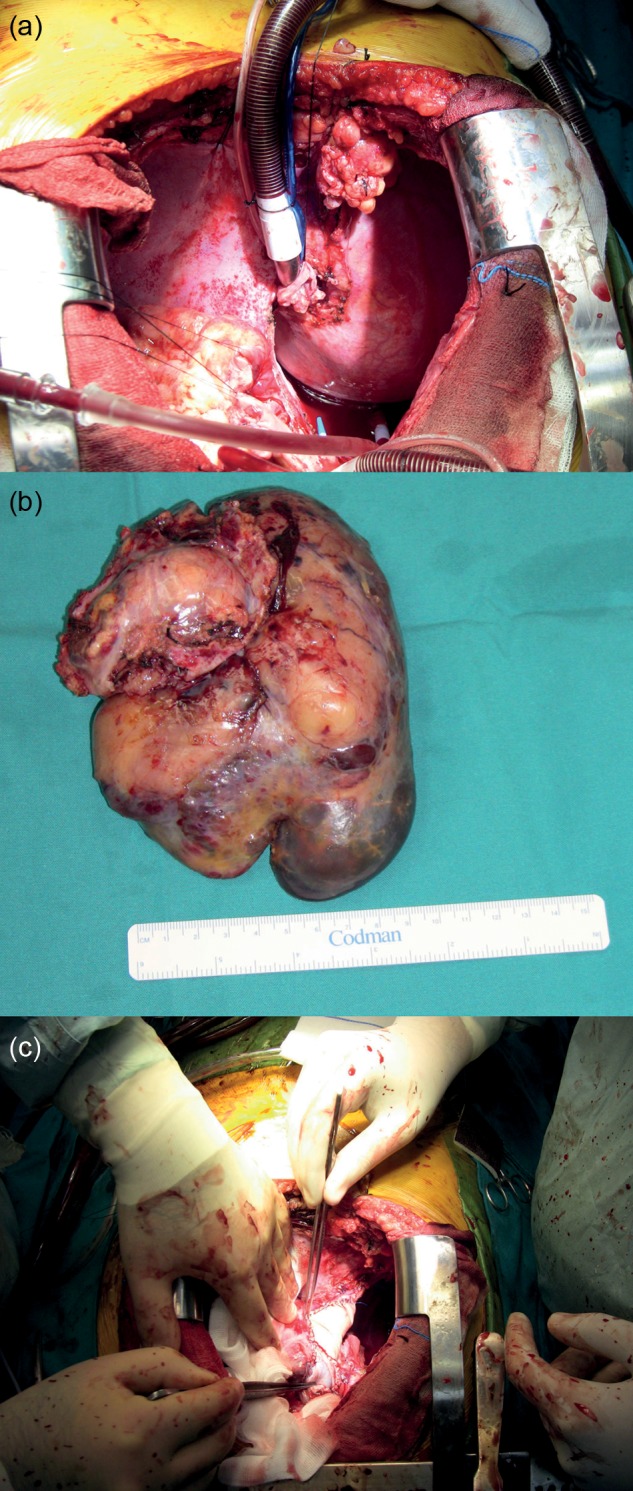
(a) For the complete and radical resection of the tumour. (b) The excised mass was 14 × 8, 5 × 6 cm. (c) We finally used the rest of the Peri-Guard® patch to reconstruct the right atrium.
The CPB and cross-clamp times were 202 min and 128 min, respectively. The tumour histology examination revealed areas of haemorrhage and necrosis, with a pale-white appearance. The immunochemistry tests revealed: positive to actine, focally positive to CD99, positive to CD31, CD34 of the endothelial cells of vessels. There was a review of the specimen and it resembled a fascicular spindle-cell sarcoma, with delicate bundles of wiry, stromal collagen and plump, overlapping nuclei. Immunostatins showed multifocal positivity for epithelial membrane antigen, as well as diffuse nuclear positivity for transducin like encancer of split 1, while keratin was negative. The specimen was also examined abroad and confirmed the lesion as monophasic synovial sarcoma.
The PICU stay was two days and the patient was then transferred to the normal ward. He had a long postoperative period that was complicated by deep vein thrombosis (DVT) and the presence of thrombus in the IVC, iliacs and hepatic veins, confirmed by ultrasound, even though the patient was started on low molecular weight heparin (LMWH) on the third postoperative day. A CT was requested, which revealed pulmonary embolism on both lungs, thrombus formation on the IVC, hepatic veins, left renal artery, bilateral iliacs and large ascites, and pleural effusion, but there were no findings from the internal organs of the thorax and abdomen, in terms of possible metastatic lesions. An ECHO also confirmed no visible cardiac involvement. The patient also had a bone scan that produced no findings. After appropriate treatment, the rest of his hospital stay was uneventful and he was discharged on the 33rd postoperative day with an urgent referral to an oncologist.
Unfortunately the patient and parents refused further consultation with the oncologist and—although there was no recurrence at 12 months following the procedure—at 24 months we were informed of his death, due to a tumour appearing this time on the left cardiac chambers, with subsequent multi-organ failure.
DISCUSSION
Synovial sarcoma constitutes 8–10% of all sarcomas, commonly affecting adults in the third to fifth decades of life. Males are more often affected than females, with no particular race known to be predisposed to the disease. More than 90% of patients have a t(X; 18) translocation mutation, which is not associated with other sarcomas [1]. Cytogenetic analysis has also proven that certain molecular genetics features are related to the course of the disease [2]. This malignancy usually involves the extremities—especially the lower extremities. Less common sites of involvement include the retroperitoneum, thoracic cavity, head and neck regions.
Regarding the thoracic cavity [3, 4], lesions can be presented as anterior mediastinal masses with chest pain, shortness of breath, pleural effusion, tamponade and, in some cases, they were situated in a paravertebral location, presented with neck or back pain. The tumours vary in size, usually exhibiting a tan white, soft-to-rubbery cut surface with areas of haemorrhage and necrosis and foci of gelatinous material, or even presenting with areas of cystic degeneration. The tumours can be well circumscribed, and may invade the pleura, pericardium, heart, great vessels, chest wall, ribs, and vertebrae. Diagnosis using CT, MRI and fine needle aspiration (FNA) with the aid of CT can be challenging.
Most of the patients were treated by complete surgical excision and others by partial excision, followed by radiation therapy. There has been a case where the tumours were inoperable and treated with radiation therapy only. Nevertheless, radical surgical excision is the treatment of choice [4]. Monophasic synovial sarcoma is a rare condition and, ideally, should be dealt with in centres with cardiothoracic cover, oncology, cardiology and respiratory departments before any action regarding diagnosis or treatment is undertaken. Finally, from our perspective, a paediatrician and support services for both parents and patient should be involved in the planning of treatment.
PROGNOSIS
Follow-up can reveal local recurrence, metastases to the lung, lymph nodes and epidural space from 1 to 3 years and, in some instances, liver metastasis and death as early as 6 months, as well as paraneoplastic symptoms. The prognosis for MSS has been poor. According to recent large studies, using chemotherapy and radiation is advantageous, particularly in high-risk patients [3, 5]. The 5-year overall survival and the 5-year metastasis-free survival rate in patients with non-metastatic, surgically resected disease are 71% and 51%, respectively.
FUNDING
The project was completed without any financial support and small expenses were covered by the authors.
Conflict of interest: none declared.
REFERENCES
- 1.Hazelbag HM, Szuhai K, Tanke HJ, Rosenberg C, Hogendoorn PC. Primary synovial sarcoma of the heart: a cytogenetic and molecular genetic analysis combining RT-PCR and COBRA-FISH of a case with a complex karyotype. Mod Pathol. 2004;17:1434–9. doi: 10.1038/modpathol.3800200. doi:10.1038/modpathol.3800200. [DOI] [PubMed] [Google Scholar]
- 2.Siegel HJ, Sessions W, Casillas MA, Jr, Said-Al-Naief N, Lander PH, Lopez-Ben R. Synovial Sarcoma: clinicopathologic features, treatment and prognosis. Orthopedics. 2007;30:1020–25. doi: 10.3928/01477447-20071201-15. [DOI] [PubMed] [Google Scholar]
- 3.Deshmukh R, Mankin HJ, Singer S. Synovial sarcoma: the importance of size and location for survival. Clin Orthop Relat Res. 2004;419:155–61. doi:10.1097/00003086-200402000-00025. [PubMed] [Google Scholar]
- 4.de Zwaan C, Bekkers SC, van Garsse LA, Jansen RL, van Suylen RJ. Primary monophasic mediastinal, cardiac and pericardial synovial sarcoma: a young man in distress. Neth Heart J. 2007;15:226. doi: 10.1007/BF03085986. doi:10.1007/BF03085986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ferrari A, Gronchi A, Casanova M, Meazza C, Gandola L, Collini P, et al. Synovial sarcoma: a retrospective analysis of 271 patients of all ages at a single institution. Cancer. 2004;101:627–34. doi: 10.1002/cncr.20386. doi:10.1002/cncr.20386. [DOI] [PubMed] [Google Scholar]


