Abstract
Thymoma is the commonest tumour of the anterior mediastinum in adults. Ectopic thymoma sometimes occurs, usually affecting the neck, mediastinal compartments, the lung and, very rarely, the pleura. We describe the case of a giant right-sided pleural thymoma (14 × 13 × 8 cm), preoperatively suspected to be a solitary fibrous tumour; a complete surgical resection was achieved and a postoperative diagnosis of type AB Masaoka stage II B tumour was attained.
Keywords: Thymoma, Intrathoracic tumour, Fine needle aspiration biopsy, Differential diagnosis, Surgery, Resection
INTRODUCTION
Epithelial thymic tumours (thymoma and thymic carcinoma) are rare neoplasms, but the most frequent mediastinal ones in adults. The incidence of thymomas is estimated to be 0.15 cases per 100 000 person/year in the USA, and they usually manifest in the antero-superior mediastinal space. Ectopic tumours have been described, accounting only for 4% of all thymomas [1]. Intrathoracic tumours with pleural origin are very unusual. We hereby report the case of an incidentally discovered giant pleural thymoma and we also discuss the differential diagnosis between thymomas and other large neoplasms originating from the pleura.
CASE PRESENTATION
A 74-year old, non-smoker, Caucasian woman was admitted in our department for a large right-sided thoracic lesion, with no other symptoms except dyspnoea and digital clubbing.
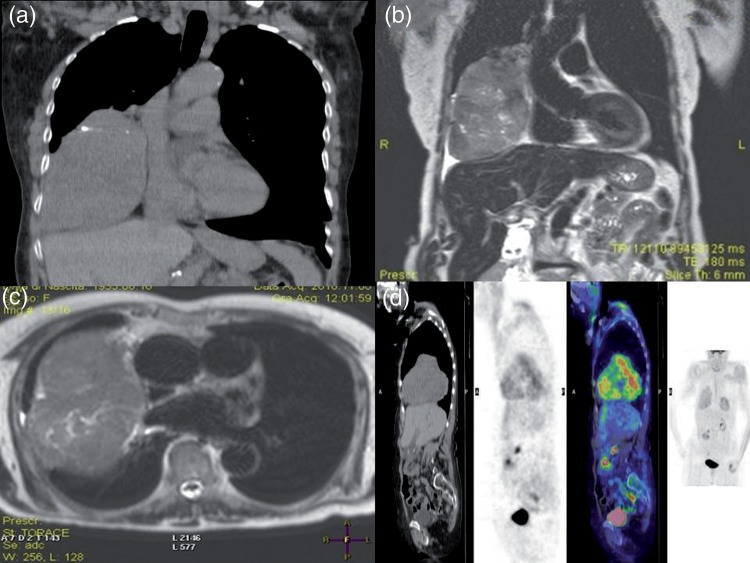
The thoracic computed tomography (CT) scan showed a right posterolateral tumour of 14 × 13 × 8 cm, with calcifications and necrotic areas (Fig. 1a); on the thoracic magnetic resonance imaging (MRI), the lesion had a low signal intensity on T1-weighted images, and an intermediate intensity on T2-weighted images (Fig. 1b and c). No signs of chest wall or diaphragmatic invasions were present. Positron emission tomography (PET) scan showed an elective uptake in correspondence with the lesion and the maximum standardized uptake value was 3.2 (Fig. 1d).
Figure 1:
Preoperative patient assessment. (a) Thoracic CT scan showing a large right-sided lesion, with possible necrotic areas. (b and c) Thoracic MRI excluding tumour invasion on the surrounding structures. (d) PET scan showing the elective uptake in correspondence of the lesion, only.
Due to its radiological and clinical characteristics (digital clubbing), the lesion was primarily suspected to be a solitary fibrous tumour of the pleura.
A transthoracic CT-guided tru-cut biopsy was performed, according to our protocol for resectable mediastinal neoplasms. Unfortunately, a definitive diagnosis was not achieved: the immunohistochemical tumour characteristics were not in fact, suggestive of a solitary fibrous tumour (negative antibodies anti CD-34, sinaptophysin, vimentin, Chromogranin A; positive antibodies anti CD99, CD15, Bcl-2 and calretin; tumour prolipherative index—MIBI-1: 20%). A slightly aggressive neoplasm (not a malignant mesothelioma) was thus suspected and, since it was deemed resectable, its resection was planned.
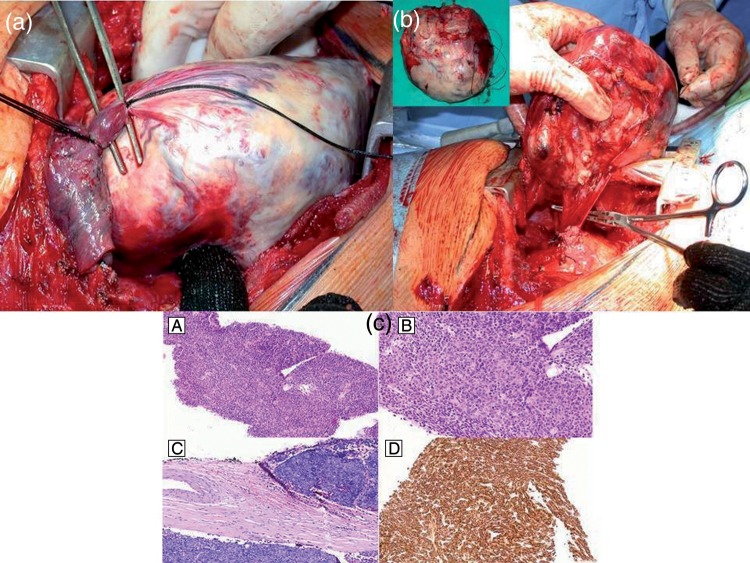
A right posterolateral thoracotomy was performed; a big and partially necrotic lesion, originating from the mediastinal pleura attached to the lung with a richly vascularized pedicle was detected (Fig. 2a and b). The tumour did not invade any surrounding structure, no continuity with the thymic gland and/or other mediastinal organs was observed and its complete resection was finally achieved.
Figure 2:
Intraoperative view of the large necrotic tumour attached to the lung with a richly vascularized pedicle (a); the tumour originated from the mediastinal pleura (intraoperative view) (b), without connections with thymic gland and/or other mediastinal organs. The completely resected tumour specimen is shown in the box ((b), in the top). (c) Type AB thymoma: histological and immunohistological appearances of the tumour. (A and B) Transthoracic needle biopsy showing monomorphic proliferation of spindle or oval-shaped tumour cells with pseudomesenchymal appearance and bland nuclei; Hassal corpuscles are absent (haematoxylin and eosin, (A): ×100, (B): ×200). (C) Postoperative histological specimen showing tumour focal invasion into fibrous capsule (Masaoka stage II2) (haematoxylin and eosin, ×100). (D) Immunohistochemical staining showing strongly cytokeratin AE1/3 immunoreactivity of neoplastic epithelial cells (×100).
The patient's postoperative course was uneventful and she was discharged from the hospital on the seventh day. Surprisingly, a definitive diagnosis of type AB stage II B thymoma (minimally invasive of the capsule) was made (Fig. 2c). This thymoma was consequently considered to be derived from the migration of ectopic thymic tissue.
We decided to not perform a subsequent transcervical thymectomy since the patient did not have a previous history of myasthenia gravis (MG), she was old and a complete thymoma resection was achieved; the patient is still alive and disease-free 14 months after surgery.
DISCUSSION
Not more than 4% of all thymomas present with an ectopic mass affecting the neck, the middle or posterior mediastinum or the lung. Thymomas originating from the pleura are extremely unusual, and very few are described in the literature [2, 3]. When an ectopic thymoma originates from the pleura (both visceral or mediastinal), its commonest radiological appearance is an anterior intrathoracic mass. It must be differentiated from other more common intrathoracic neoplasms, which may include solitary fibrous tumours of the pleura, sarcomas of the chest wall, malignant pleural mesotheliomas or other metastatic tumours.
In cases of large but potentially resectable intrathoracic lesions, we usually proceed to achieve a preoperative cyto/histological diagnosis through the least possible invasive procedure. Even if it is well known that the role of a non-surgical biopsy in the preoperative assessment of mediastinal lesions is still a matter of discussion, we reached the conclusion that transthoracic CT-guided tru-cut biopsy is effective in diagnosing thymomas, lymphomas and solitary fibrous tumours. In our experience, when an experienced pathologist evaluates the specimens, a tru-cut is preferred over a fine needle aspiration biopsy since, with the first procedure, the amount of pathological tissue obtained is usually sufficient for a correct diagnosis. Furthermore, even if in the literature, bleeding is described following mediastinal neoplasm biopsies [4], so far we have never experienced such a complication, and in the last 2 years, the number of surgical mediastinal biopsies performed in our division has dramatically reduced, with CT-guided tru-cut procedures being preferred instead. As is known, such a manoeuvre is not devoid of risks, but these are diminished if performed by experienced radiologists.
Unfortunately, in this case the tru-cut biopsy failed to obtain a conclusive diagnosis. The pathologist excluded an solitary fibrous tumour due to the immunohistochemical characteristics of the lesion (CD34, vimentin and BCL-2 negativity, and high MIBI-1 prolipheration index). At this point, we judged an anterior mediastinotomy to be unnecessary, due the following reasons: it would not change our therapeutic approach and the lesion was surgically resectable.
The definitive histological diagnosis of type AB thymoma was a real surprise.
Our patient was subjected neither to a subsequent transcervical thymectomy nor to an adjuvant therapy since firstly, we considered the risk of developing a secondary MG to be very low, and secondly, the thymoma, with a low Masaoka and histological staging, was radically resected. A strict clinical-radiological follow-up (thoracic CT scan every 6 months for 2 years, and later, every 12 months) was mandatory for this patient.
On the contrary, when a preoperative biopsy confirms the suspicion of an ectopic thymoma, the surgical approach should not differ from that of a typical sited one, which comprises the resection of both the tumour and the thymic gland, eventually followed by chemoradiotherapy, according to the tumour histological grade and stage.
In conclusion, ectopic thymoma, even if as a very rare occurrence, should always be included in the differential diagnosis whenever a large intrathoracic mass is observed.
Conflict of interest: none declared.
REFERENCES
- 1.Venuta F, Anile M, Diso D, Vitolo D, Rendina EA, de Giacomo T, et al. Thymoma and thymic carcinoma. Eur J Cardiothorac Surg. 2010;37:13–25. doi: 10.1016/j.ejcts.2009.05.038. doi:10.1016/j.ejcts.2009.05.038. [DOI] [PubMed] [Google Scholar]
- 2.Yamazaki K, Yoshino I, Oba T, Yohena T, Kameyama T, Tagawa T, et al. Ectopic pleural thymoma presenting as a giant mass in the thoracic cavity. Ann Thorac Surg. 2007;83:315–7. doi: 10.1016/j.athoracsur.2006.03.092. doi:10.1016/j.athoracsur.2006.03.092. [DOI] [PubMed] [Google Scholar]
- 3.Kitada M, Sato K, Matsuda Y, Hayashi S, Tokusashi Y, Miyokawa N, et al. Ectopic thymoma presenting as a giant intrathoracic tumor: a case report. World J Surg Oncol. 2011;9:66–9. doi: 10.1186/1477-7819-9-66. doi:10.1186/1477-7819-9-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Santoprete S, Ragusa M, Urbani M, Puma F. Shock induced by spontaneous rupture of a giant thymoma. Ann Thorac Surg. 2007;83:1526–8. doi: 10.1016/j.athoracsur.2006.10.016. doi:10.1016/j.athoracsur.2006.10.016. [DOI] [PubMed] [Google Scholar]