Abstract
Fungi have emerged as important etiological agents for chronic sinusitis. Invasive aspergillosis has been reported in immunocompromised individuals or diabetics; however, it is uncommonly seen in immunocompetent patients. Definitive diagnosis of these lesions is based on histological examination and fungal culture. We report two cases of invasive maxillary lesions in immunocompetent patients, clinically suspected of malignancy; however, fine needle aspiration cytology showed fungal hyphae, morphologically suggestive of Aspergillus, which was later confirmed on histopathology. Aspiration cytology thus plays a crucial role in the early and definitive diagnosis of fungal sinusitis in cases clinico-radiologically suspected of malignancy. An early diagnosis will help the clinician for early and appropriate management and follow-up in order to decrease the high morbidity and mortality associated with it.
Keywords: Aspergillosis, cytology, fungal sinusitis, immunocompromised
Introduction
Aspergillus is the most common fungus affecting paranasal sinuses.[1] Primary infection involves eyes, ears, larynx, lungs, and sinuses, followed by liver, spleen, bone, and meninges.[2,3] Worldwide, Aspergillus fumigatus is the most common species, followed by Aspergillus niger and Aspergillus flavus, whereas A. flavus is the most common species in India.[2] Predisposing factors that promote fungal infections in the sinuses include polyps and stagnant secretions besides other factors like neutropenia, inappropriate use of antibiotics, immunosuppressive drugs, corticosteroids, uncontrolled diabetes mellitus (DM), human immunodeficiency virus (HIV) infection, trauma, burns, and radiation therapy.[4] In immunocompromised patients, Aspergillus leads to highly destructive lesions; however, literature search shows invasive aspergillosis in non-neutropenic patients also.[5] Clinico-radiological findings can be misleading as the lesions are locally destructive and mimic a neoplasm. Invasive fungal sinusitis (IFS) responds to conservative medical management and debridement; hence, an early diagnosis by fine needle aspiration cytology (FNAC) is mandatory to prevent undue surgery.
We report two patients presenting with swelling and pain in the maxillary region who were clinico-radiologically suspected of malignancy; however, FNAC in both the cases revealed fungal sinusitis (FS).
Case Reports
FNAC was performed in both cases using 22-gauge needle; aspirate was whitish fluid (Case 1) and blood mixed (Case 2). The aspirates were processed as air-dried Giemsa-stained smears; cytomorphological features were suggestive of aspergillosis. Periodic-acid-Schiff (PAS) and silver methanamine (SM) stains were performed on the aspirate smears for further typing of fungus. However, considering the clinico-radiological suspicion of neoplasm, a biopsy was advised that confirmed fungus in both the cases.
Case 1
A 45-year-old female presented to the Ear, Nose and Throat (ENT) Department with complaints of a painful swelling in the left maxillary region for 6 months. The swelling was insidious in onset with scant serous nasal discharge. There was no history suggestive of nasal obstruction, fever, recurrent infections or diabetes. Clinically, there was a tender swelling in the left maxillary region near the medial canthus. Computed tomography (CT) scan showed expansion of the maxillary sinus with bone erosion, suggestive of a malignancy.
Case 2
A 42-year-old male presented with complaints of headache, nasal discharge and swelling in right maxillary region for 8 months. There was no history indicative of immunodeficiency. A bony hard swelling measuring 8 × 8 cm was palpated in the right maxilla reaching up to the infraorbital region. Plain radiograph revealed a diffuse opacity in the maxillary sinus without any bone destruction. CT scan showed an enhancing soft tissue density in the right maxillary sinus, suggestive of a proliferative lesion.
Cytological findings
Microscopic examination of aspirate smears revealed predominantly hemorrhagic background with many multinucleated foreign body giant cells (GCs), and few inflammatory cells comprising eosinophils, plasma cells and lymphocytes. Interspersed amongst these and within the GCs, few septate fungal hyphae branching at acute angles were seen [Figure 1]. PAS stain highlighted its morphology. Based on the CT and cytological features, a diagnosis of IFS caused by aspergillus was suggested. A biopsy and fungal culture were further advised for species identification.
Figure 1.
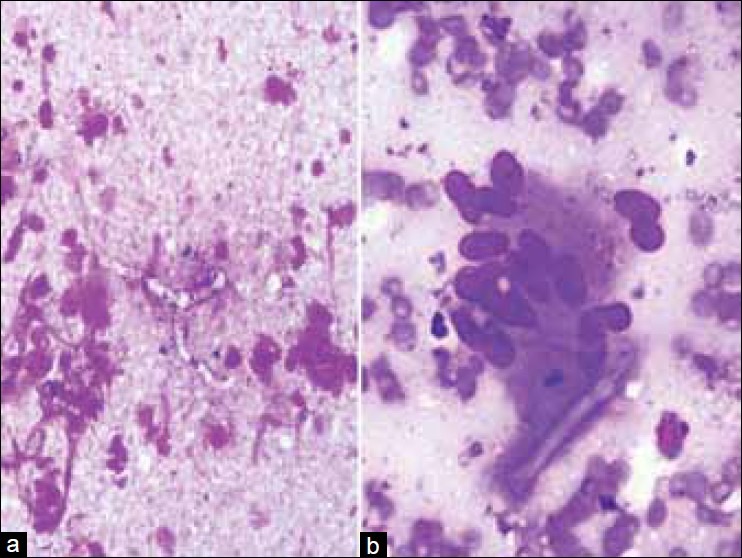
(a) Smear shows septate, fungal hyphae branching at acute angle in an acute inflammatory background (Giemsa, ×250) and (b) a hyphae within the giant cell (Giemsa, ×400)
Histopathological findings
Histopathological examination of biopsies from the maxillary sinus in both the cases showed abundant septate fungal hyphae, granulomatous inflammation, GCs and eosinophils; PAS and SM stains confirmed the type of fungus as Aspergillus [Figure 2]. Culture from the serous material from sinusitis showed greenish white cotton wool growth at 37°C on Sabouraud's dextrose agar (SDA), thus confirming the species as A. flavus.
Figure 2.
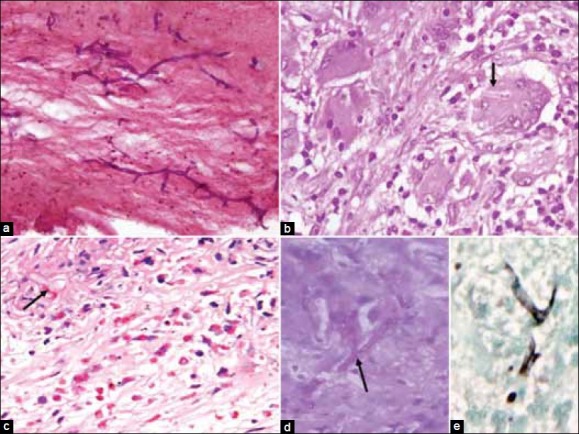
Sections show (a) Aspergillus in necrotic background (H and E, ×250), (b) fungal hyphae in giant cell (H and E, ×400), (c) many eosinophils and hyphae (H and E, ×250), special stains highlighting the fungal morphology (d; PAS, ×250) and (e; silver methanamine, ×250)
The former patient was treated initially with intravenous Amphotericin-B and endoscopic debridement, followed by oral itraconazole; further, she had to undergo partial maxillectomy in view of frequent recurrences and bone involvement. The latter patient was treated with oral itraconazole alone. Both the patients improved on treatment, and extensive surgery could be prevented.
Discussion
Fungal sinusitis constitutes 6–9% of all the rhinosinusitis.[6–8] Clinically, it presents as either an acute fulminant sinusitis or chronic invasive sinusitis. The former is largely attributed to Mucor and the latter is mainly due to Aspergillus. The acute form is a life-threatening condition, usually seen in immunocompromised patients with severe neutropenia or DM, and is associated with significant visual and neurological impairments in survivors, and sometimes mortality.[7] Clinically, these patients may present with rhinorrhea, headache, nasal obstruction, proptosis, facial and periorbital pain mimicking infections (Mucor, tuberculosis, osteomyelitis), inflammatory lesions (rhinoscleroma, Wegener's granulomatosis) and malignant tumors of the nose and paranasal sinuses. Radiologically, they show sinus opacification and bone erosion and may mimic a malignancy.[9] Non-invasive FS includes allergic and fungal ball and does not need extensive surgery, while most of the IFS patients are unresponsive to conservative management and require appropriate antifungals with local debridement. Early and definitive diagnosis of IFS is mandatory that will rule out other differential diagnoses, especially neoplasm, and will help clinicians for appropriate management and in the follow-up of patients.
Both magnetic resonance imaging (MRI) and CT can help establish a diagnosis of IFS. Bone involvement and erosion is more delineated on CT, while soft tissue extensions, vascular invasion and cavernous sinus involvement are more appreciated on MRI. Both the imaging techniques, however, are not definitive and often fail to differentiate an infectious process from a neoplastic one. Definite diagnosis of FS depends upon the demonstration of the fungus on aspirate smears or a biopsy. Fungal culture is complimentary to morphology and required for species identification; but samples submitted for culture may not be representative, and not all the fungi grow on culture media. Hence, morphology remains the mainstay of diagnosis in most cases. Sinonasal swellings when present are easily amenable to FNAC. Adequate and representative cytological material when obtained can reliably give a confident diagnosis. Aspergillus can be easily differentiated from Mucor on morphology, as the latter is characterised by broad, non-septate hyphae branching at right angle. In the present cases, both the patients were immunocompetent, middle aged and clinico-radiologically suspected of malignancy; however, they were diagnosed on FNAC as fungal sinusitis and prevented from undue surgery. Species identification is of importance in cases of Aspergillus sinusitis. A. flavus is the commonest type reported in India.[1] Species identification is not much relevant in patients’ management, but is of epidemiogical significance, since it depends upon various geographical locations, thus aiding diagnosis in difficult cases.
Conclusion
This report emphasizes on the early diagnosis of IFS, which can be managed conservatively preventing the morbidity and mortality in these patients. Cytology, being an easily available, minimally invasive and inexpensive procedure, can be used as initial diagnostic modality in cases of IFS.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Kumar Behera S, Patro M, Mishra D, Bal A, Behera B, Sahoo S. Fine needle aspiration in aspergilloma of frontal sinus: a case report. Acta Cytol. 2008;52:500–4. doi: 10.1159/000325562. [DOI] [PubMed] [Google Scholar]
- 2.Agarwal S, Kanga A, Sharma V, Sharma DR, Sharma ML. Invasive aspergillosis involving multiple paranasal sinuses--a case report. Indian J Med Microbiol. 2005;23:195–7. doi: 10.4103/0255-0857.16595. [DOI] [PubMed] [Google Scholar]
- 3.Garcia-Reija MF, Crespo-Pinilla JI, Labayru-Echeverria C, Espeso-Ferrero A, Verrier-Hernandez A. Invasive maxillary aspergillosis: report of a case and review of the literature. Med Oral. 2002;7:200–5. [PubMed] [Google Scholar]
- 4.Singh N, Siddaraju N, Kumar S, Muniraj F, Bakshi S, Gopalakrishnan S. Fine-needle aspiration biopsy as an initial diagnostic modality in a clinically unsuspected case of invasive maxillary fungal sinusitis: A case report. Diagn Cytopathol. 2010;38:290–3. doi: 10.1002/dc.21216. [DOI] [PubMed] [Google Scholar]
- 5.Nakahira M, Saito H, Miyagi T. Left vocal cord paralysis as a primary manifestation of invasive pulmonary aspergillosis in a nonimmunocompromised host. Arch Otolaryngol Head Neck Surg. 1999;125:691–3. doi: 10.1001/archotol.125.6.691. [DOI] [PubMed] [Google Scholar]
- 6.Schubert MS. Allergic fungal sinusitis: pathophysiology, diagnosis and management. Med Mycol. 2009;47(Suppl):S324–30. doi: 10.1080/13693780802314809. [DOI] [PubMed] [Google Scholar]
- 7.Parikh SL, Venkatraman G, DelGaudio JM. Invasive fungal sinusitis: a 15-year review from a single institution. Am J Rhinol. 2004;18:75–81. [PubMed] [Google Scholar]
- 8.Busaba NY, Colden DG, Faquin WC, Salman SD. Chronic invasive fungal sinusitis: a report of two atypical cases. Ear, Nose and Throat J. 2002;81:462–6. [PubMed] [Google Scholar]
- 9.Taxy JB. Paranasal fungal sinusitis: contributions of histopathology to diagnosis: A report of 60 cases and literature review. Am J Surg Pathol. 2006;30:713–20. doi: 10.1097/00000478-200606000-00006. [DOI] [PubMed] [Google Scholar]


