Our study highlights the association of lumbosacral transitional vertebrae (LSTV) and types II and IV with lower back and buttock pain; therefore, LSTV should be considered part of the differential diagnosis of back pain, especially in cases of pain refractory to conventional management.
Abstract
Purpose:
To assess the prevalence and degree of lumbosacral transitional vertebrae (LSTV) in the Osteoarthritis Initiative (OAI) cohort, to assess whether LSTV correlates with low back pain (LBP) and buttock pain, and to assess the reproducibility of grading LSTV.
Materials & Methods:
Institutional review board approval was obtained, and informed consent documentation was approved for the study protocol. Standard standing pelvic radiographs that included the transverse processes of L5 were graded according to Castellvi classification of LSTV in 4636 participants (1992 men and 2804 women; aged 45–80 years) from the OAI cohort. These data were correlated with prevalence and severity of LBP and buttock pain.
Results:
Prevalence of LSTV was 18.1% (841 of 4636), with a higher rate in men than in women (28.1% vs 11.1%, respectively; P < .001). Of the 841 individuals with LSTV, 41.72% were type I (dysplastic enlarged transverse process), 41.4% were type II (pseudoarticulation), 11.5% were type III (fusion), and 5.2% were type IV (one transverse process fused and one with pseudoarticulation). Of the participants without LSTV, 53.9% reported LBP, while the prevalence of LBP for types I, II, III, and IV was 46%, 73%, 40%, and 66%, respectively (P < .05, χ2 test). Types II and IV had higher prevalence and severity of LBP and buttock pain (P < .001).
Conclusion:
LSTV types II and IV positively correlate with prevalence and severity of LBP and buttock pain.
© RSNA, 2012
Introduction
Back pain causes a substantial loss of productivity (4), and it is one of the leading reasons for patients to seek health care in the United States (1–3). In many patients, the exact cause of their pain is unclear (5). The present study was focused on lumbosacral transitional vertebrae (LSTV), which have been previously identified as a potential cause of back pain (6–9). The prevalence of LSTV, its subtypes, and their associations with back pain are not well understood. An LSTV is an anomalous vertebra with intermediate morphologic characteristics between the sacral and the lumbar vertebrae (10,11); its transverse processes are enlarged and can articulate with the sacrum or the ilium (12). LSTV with articulation of some degree—whether partial (pseudoarthrosis) or complete fusion—is defined as either sacralization of the lowest lumbar segment or lumbarization of the most superior sacral segment of the spine (10). LSTV is a common finding in the general population, and has a reported prevalence of 5%–30% (13,14). Mario Bertolotti first described the morphologic characteristics of LTSV and its association with low back pain (LBP) in 1917, and this association has therefore been termed Bertolotti syndrome (12). The relationship between LSTV and LBP has been described in several studies but remains uncertain. Although Tini et al (11) suggested that LSTV was not associated with LBP (6,11), the findings of other studies indicated an association of LBP with LSTV (7,12,15,16).
The goals of this study were to describe the overall prevalence of the subtypes of LSTV in the 4796 patients of the Osteoarthritis Initiative (OAI) cohort, to determine the association of the different subtypes of LSTV with LBP and buttock pain, and to assess the reproducibility of the assessment and classification of LSTV.
Materials and Methods
The study protocol and informed consent documentation were approved by the local institutional review boards. Details on OAI enrollment and baseline datasets used for this study are available at http://www.oai.ucsf.edu/.
Population
OAI included 4796 participants who were recruited on the basis of their risk factors for knee osteoarthritis (OA) or mild to moderate knee OA. Of these participants, 4636 (97%) patients with diagnostic baseline pelvic radiographs were studied. The study population consisted of 1919 men (41%) between the ages of 45 and 79 years (mean age, 61 years ± 9 [standard deviation]) and 2717 women (58.5%) between the ages of 45 and 79 years (mean age, 61 years ± 9). Patient characteristics, including age, sex, race, and body mass index are shown in Table 1. The study’s participants represented a sample selected by OAI for the study of knee OA and were not recruited on the basis of whether they experienced back pain. Sixty-two percent (860 of 1390) of the participants who had knee OA and were in the progression subcohort of OAI had back pain, and 58% (1900 of 3289) of the participants in the incidence subcohort (patients who did not have knee OA but who were at risk for developing it) had back pain. However, this difference was not statistically significant (P = .08).
Table 1.
Characteristics of 4636 Patients with and without LSTV
Note.—Unless otherwise stated, data are numbers of patients, with percentages in parentheses.
χ2 for categorical variables and analysis of variance for continuous variables.
BMI = body mass index
Imaging Technique
Standardized standing pelvic radiographs were performed by using a dedicated foot-positioning mat with the toes internally rotated at a 5° angle, and the x-ray beam was positioned approximately 7 cm above the pubic symphysis. The images were obtained at five institutions: Ohio State University (Columbus, Ohio), University of Maryland School of Medicine (Baltimore, Md), Johns Hopkins University School of Medicine (Baltimore, Md), University of Pittsburgh School of Medicine (Pittsburgh, Pa), and Memorial Hospital of Rhode Island (Pawtucket, RI). Representative radiographs are shown in the Figure.
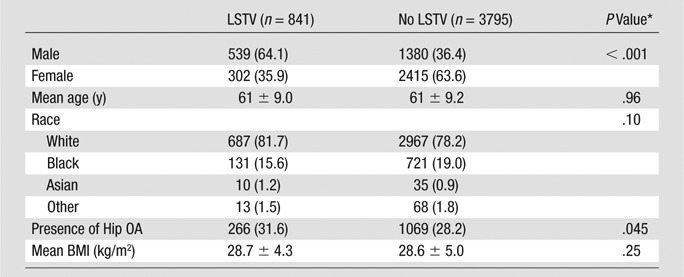
Figure a:
Radiographs demonstrate the Castellvi classification of LSTV: (a) Type I: dysplastic enlarged transverse process (arrow); (b) Type II: pseudoarticulation of the transverse process with the sacrum with increased sclerosis (arrows); (c) Type III: fusion with the sacrum (arrows); (d) Type IV: unilateral LSTV type II (long arrow) with type III on the contralateral side (short arrow).
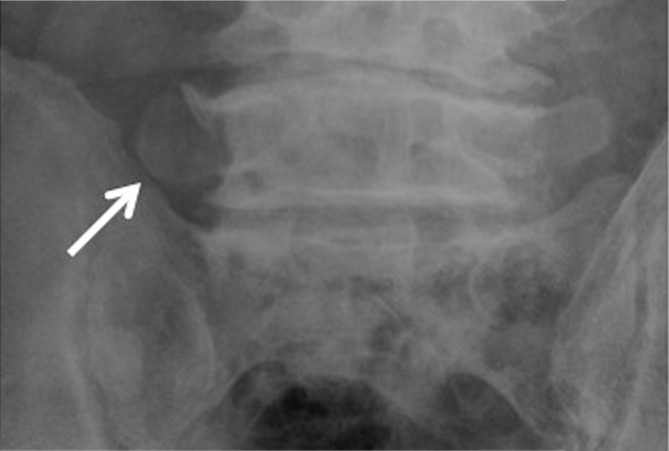
Figure b:
Radiographs demonstrate the Castellvi classification of LSTV: (a) Type I: dysplastic enlarged transverse process (arrow); (b) Type II: pseudoarticulation of the transverse process with the sacrum with increased sclerosis (arrows); (c) Type III: fusion with the sacrum (arrows); (d) Type IV: unilateral LSTV type II (long arrow) with type III on the contralateral side (short arrow).
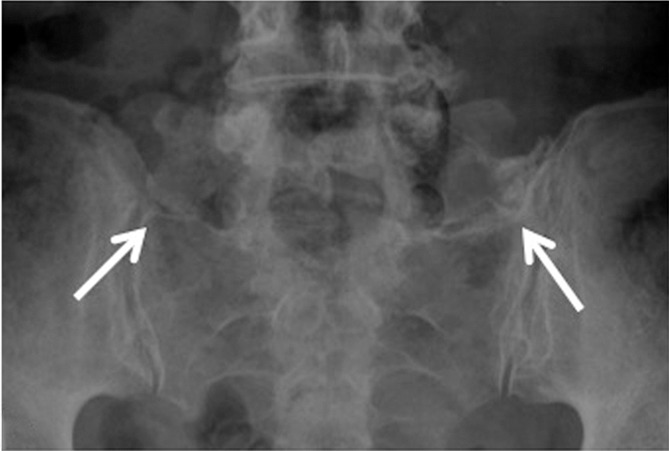
Figure c:
Radiographs demonstrate the Castellvi classification of LSTV: (a) Type I: dysplastic enlarged transverse process (arrow); (b) Type II: pseudoarticulation of the transverse process with the sacrum with increased sclerosis (arrows); (c) Type III: fusion with the sacrum (arrows); (d) Type IV: unilateral LSTV type II (long arrow) with type III on the contralateral side (short arrow).
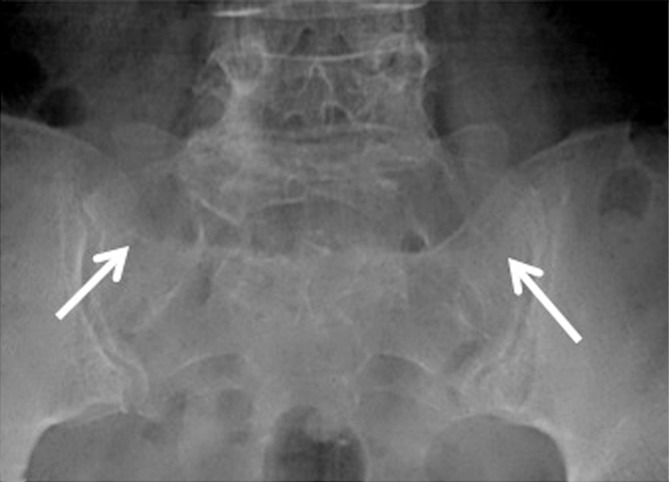
Figure d:
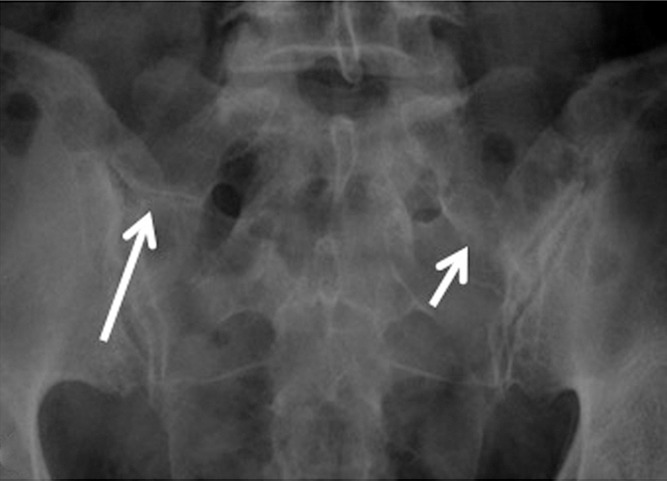
Radiographs demonstrate the Castellvi classification of LSTV: (a) Type I: dysplastic enlarged transverse process (arrow); (b) Type II: pseudoarticulation of the transverse process with the sacrum with increased sclerosis (arrows); (c) Type III: fusion with the sacrum (arrows); (d) Type IV: unilateral LSTV type II (long arrow) with type III on the contralateral side (short arrow).
Image Analysis
All images were reviewed on picture archiving and communication system workstations (Agfa, Ridgefield Park, NJ). All of the 4796 pelvic anteroposterior radiographs were independently read by two radiologists (L.N., 5 years of experience; W.V., 8 years of experience). Initially, the pelvic radiographs were independently screened by these radiologists for image quality (ie, the ability to assess the relationship between the sacral ala and the lumbar transverse process), postsurgical changes obscuring transitional anatomy, and presence of LSTV. Out of 4796 radiographs, 160 were considered to be of poor quality and were excluded from the study.
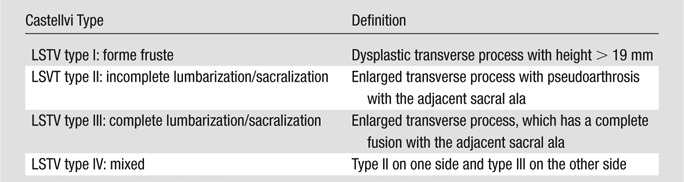
Radiographs with adequate image quality were classified according to the presence of LSTV. The presence of an LSTV was determined manually by evaluating the craniocaudal width of the transverse process, with a threshold of greater than 19 mm as measured by using the digital caliper on a picture archiving and communication system, or by the presence of articulation or complete fusion of the transverse process with the sacrum. All discrepancies were settled by a third radiologist (T.M.L., 25 years of experience). LSTV cases were graded according to a radiographic classification system modified from that of Castellvi et al (9), hereafter, the Castellvi classification (Figure). Table 2 outlines the main characteristics of the Castellvi classification. To minimize the number of categories, we classified the cases independently from the bilateral or unilateral findings into four basic types (11,14). The hip joints were also assessed for OA according to the Osteoarthritis Research Society International classification (18). All of the hip images had been independently read 1 year earlier by both a radiologist (L.N.) and a rheumatologist (N.E.L., 30 years of experience). In cases where there was disagreement among the readers, a radiologist (T.M.L.) was also consulted.
Table 2.
LSTV according to Castellvi Classification
Clinical Data
The OAI back pain and function questionnaire provided information about frequency, severity, and location of pain. Patients were asked about the frequency of their back pain during the past 30 days and graded it as never, rarely, some of the time, most of the time, or all of the time. Patients were also asked to evaluate the average severity of their back pain during the past 30 days and to classify it as none, mild, moderate, or severe. The location of the pain was assessed with four questions that varied according to the presence of upper back pain, middle back pain, LBP, or buttock pain within the past 30 days. A five-part variable was created for location of back pain. The categories were mutually exclusive and included LBP, buttock pain (without LBP), pain located in the middle or upper back (without LBP or buttock pain), and no back pain at any location.
Information was also provided regarding limitation of physical activity due to back pain and physical activity level by using the Physical Activity Scale for the Elderly (PASE) (19–22).
Reproducibility Analysis
Interobserver reproducibility was calculated from all studies by using the initial readings by the two radiologists. Intraobserver reproducibility was obtained by using 500 randomly selected studies that were independently analyzed by two radiologists on two separate occasions. Cohen κ values were calculated to assess intraobserver and interobserver agreement of the radiographic classification according to Castellvi classification.
Statistical Analysis
Statistical analysis was performed by using SAS 9.2 (SAS Institute, Cary, NC). Descriptive statistics for baseline demographic data were calculated for LSTV and non-LSTV groups, as well as for each LSTV subtype compared with non-LSTV. Continuous variables are presented as mean ± standard deviation and categorical variables as frequency (percentages). For bivariate comparisons, continuous variables were compared by using analysis of variance or ranked analysis of variance as required, and categorical variables were compared by using a χ2 test.
Multivariable models were used to assess the relationship between back pain and LSTV, adjusted for age, sex, race, body mass index, and radiographic hip OA. Age, race, hip OA, and body mass index were included in the models because these are known risk factors for back pain. Back pain variables, measured as presence or absence of upper back pain, middle back pain, LBP, or buttock pain, were modeled by using a multinomial model. Odds ratios (ORs), 95% confidence intervals (CIs), and P values were reported for comparison of LSTV to non-LSTV, with each back pain location category (lower back, buttocks, and middle or upper back) versus no back pain. The LSTV subtypes were treated as a categorical variable, and separate ORs were obtained for each value. Back pain variables measured with ordinal scales used proportional odds models, reported as the OR, and were in a higher category on the ordered scale compared with the next lower category. The statistical significance of all calculations was defined as P < .05.
Results
Patient Characteristics
LSTV was found in 18.1% (841 of 4636) of participants (Table 1)—28.1% (539 of 1919) of men and 11.1% (302 of 2717) of women (P < .001). No significant difference in the prevalence of LSTV was observed by race. The 841 patients with LSTV were placed into four modified Castellvi classification (9) subgroups; of these, 351 patients (41.7%) had LSTV type I, 349 (41.4%) had LSTV type II, 97 (11.5%) had LSTV type III, and 44 (5.2%) had LSTV type IV (Table 2).
LSTV and LBP
Overall, patients with LSTV were more likely to have reported LBP in the past 30 days than were participants without LSTV (OR: 1.42 [95% CI: 1.21, 1.68], P < .001) (Table 3). Four hundred eighty-four patients (10.4%) were diagnosed with Bertolotti syndrome (ie, LSTV with LBP). The subgroup analysis (Table 4) demonstrated that types II and IV were strongly associated with LBP. Compared to the non-LSTV group, types II and IV had respective ORs of 3.48 (95% CI: 2.62, 4.64) and 3.94 (95% CI: 1.63, 9.54). Types I and III had respective ORs of 0.78 (95% CI: 0.62, 0.99) and 0.69 (95% CI: 0.45, 1.07).
Table 3.
ORs of Buttock Pain, LBP, and Middle/Upper Back Pain Compared within LSTV Patients and Subtypes Compared with Non-LSTV Patients
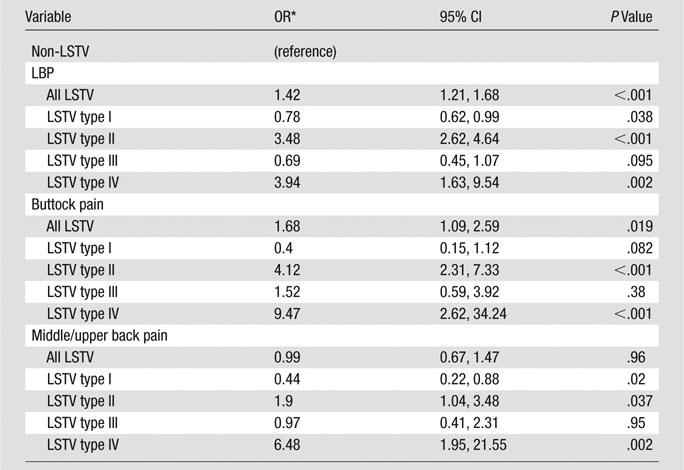
Note.—Results from a multinomial model.
OR, 95% CI, and P value from multinomial model. LBP, buttock pain, or middle/upper back pain compared to no back pain.
Table 4.
Severity of Pain, Pain Frequency, and Limitation of Activity in LSTV Patients
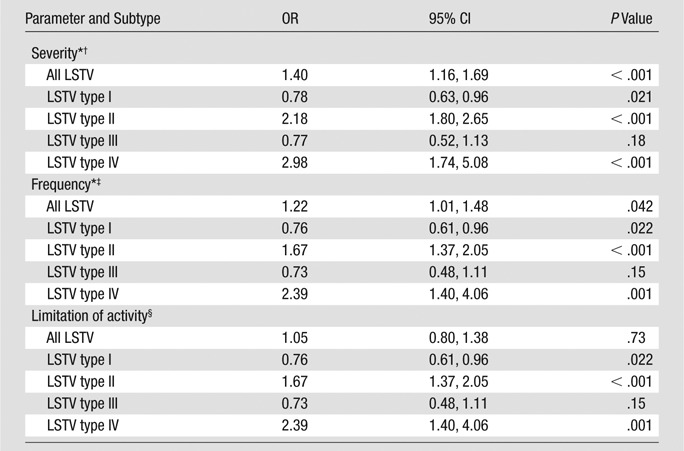
Note.—Reference standard was patients without LSTV.
Proportional odds regression model adjusted for age, sex, race, body mass index, and hip OA was used.
Severity scale: 0 = no pain, 1 = mild pain, 2 = moderate pain, 3 = severe pain.
Frequency scale: 0 = rarely bothered by pain, 1 = bothered by pain some of the time, 2 = bothered by pain most of the time, 3 = bothered by pain all of the time.
Past 30 days activity limited by back pain (yes or no). Logistic regression model adjusted for age, sex, race, body mass index, and hip OA was used.
LSTV and Buttock Pain
Individuals with LSTV were more likely to report buttock pain than were participants without LSTV (OR: 1.68 [95% CI: 1.09, 2.59], P = .019) (Table 3). Compared to the non-LSTV group, Types II and IV were associated with buttock pain, with respective ORs of 4.12 (95% CI: 2.31, 7.33) and 9.47 (95% CI: 2.62, 34.24) (Table 3). Types I and III were not associated with buttock pain.
LSTV and Middle and Upper Back Pain
Pain in the middle or upper back was not associated with the presence or absence of LSTV (P = .96) (Table 4). The relationships of LSTV subtypes with middle or upper back pain, however, were similar to those of LBP and buttock pain, with pain in type II (OR: 1.9 [95% CI: 1.04, 3.48], P = .037) and type IV (OR: 6.48 [95% CI: 1.95, 21.55], P = .002), and less pain in type I (OR: 0.44 [95% CI: 0.22, 0.88], P < .001).
Comparison between Back Pain and Other Variables
As presented in Table 4, back pain frequency (OR: 1.22 [95% CI: 1.01, 1.48], P = .042) and severity (OR: 1.40 [95% CI: 1.16, 1.69], P < .001) at any location were higher in the LSTV group; types I, II, and IV had a significant association with frequency and severity of back pain, but type III did not. Types II and IV were more likely to report higher severity or frequency, while type I was less likely to report higher severity or frequency of back pain. No significant differences in physical activity were observed between the LSTV and non-LSTV groups. However, the subgroup analysis demonstrated via PASE that types II and IV were associated with lower physical activity levels. Compared to the non-LSTV group, type II and IV had respective ORs of 1.67 (95% CI: 1.37, 2.05) and 2.39 (95% CI: 1.40, 4.06). Type I and III had no statistically significant associations with PASE.
No significant differences were found between LSTV and non-LSTV hip OA cohorts. No differences in presence, absence, or severity of hip OA were found among LSTV subgroups.
Reproducibility Analysis
The Cohen κ value for interobserver agreement on the presence or absence of LSTV in the entire cohort was 0.75, and intraobserver agreements for the two radiologists in a set of 500 randomly selected radiographs were 0.78 and 0.79. The Cohen κ value for interobserver agreement using the categorical Castellvi classification was 0.65, and the values for intraobserver agreement were 0.72 and 0.68. These values were classified as good reader agreement (23).
Discussion
Our study demonstrated that LSTV was associated with LBP and buttock pain; types II and IV had the strongest correlation, probably due to the pseudoarticulation of the transverse process of L5 with the sacrum. Increased severity and frequency of LBP were also associated with types II and IV. Within the OAI population, LSTV was nearly three times as prevalent for men as it was for women. The findings of our study demonstrate the importance of correctly diagnosing LSTV due to the association of LSTV with back pain.
The reported prevalence of LSTV ranges from 4% to 37% (14,24–27). This variability may be caused by a difference in diagnostic criteria for the definition of LSTV. The prevalence of LSTV was higher in studies that selected patients for LBP, while lower prevalence was seen in community-based studies (4%–24%) (14). We did not use back pain as an inclusion criterion, and the prevalence of LSTV in our study was similar to that of community-based studies. However, our study population had a higher incidence of knee OA than that found in the general population. Our study also confirms the results presented in the literature (13,28) regarding higher prevalence of LSTV in men.
LSTV’s relationship to back pain has been debated since it was first described in 1917 (6,7,29,30). In terms of the number of patients and the clinical parameters analyzed (such as low back pain), a study by Tini et al (11) included 4000 patients and did not demonstrate any difference regarding LBP in patients with LSTV or patients without LSTV (11). Other studies, however, support our results: Oyinloye et al (30) described the association of LBP and LSTV in a cohort of 561 patients (2009); Quinlan et al (12) also concluded that LSTV should be considered a possible cause of LBP.
Interestingly, the association between LBP and LSTV subgroups demonstrates that LSTV types II and IV are affiliated with presence of pain, as well as pain severity and frequency. Our results differ from those of Tini et al (11), which did not demonstrate any evidence of an association of LSTV with LBP when using a subtype-specific analysis. However, most of the studies (8–10,14,31,32) that support the association of LSTV with LBP implicate types II and IV.
Although literature connecting pain severity to physical activity with LSTV is limited, Taskaynatan et al (7) studied 881 young men and demonstrated an association between LSTV and severity of pain. This association is clinically relevant because patients with severe pain are more likely to seek health care, including physician visits, medication, and surgical treatment.
Pain was less frequent in type I, which suggested that type I may be a protective factor for both LBP and buttock pain. This may result from an alteration of the spine movement where a large transverse process may prevent bending. Castellvi et al (9) stated that type I was not clinically relevant and was just a forme fruste of LSTV.
The pathophysiologic mechanism of pain associated with LSVT (6,9,16,31) remains unclear. Some of the proposed mechanisms include the association of extraforaminal stenosis (8), disk prolapses, and spinal stenosis (10) with LSTV. Connolly et al (33) used skeletal scintigraphy in young patients with LSTV to demonstrate that mechanical stress at the transverse process–sacral articulation with repeated flexion and extension of the spine may contribute to pain.
Buttock pain that is associated with LSTV in types II and IV may result from nerve compression (34,35). A mechanical irritation of the nerve root may result in pain with radicular characteristics. Some studies have demonstrated an association of LSTV with extraforaminal stenosis secondary to the dysplastic transverse process (16,36), and Taskaynatan et al (7) reported an increased prevalence of nerve root symptoms in patients with LSTV. Studies concerning the correlation of buttock pain to LSTV subtypes are limited.
Our study had a number of limitations. A major limitation was that cross-sectional imaging for assessment of disk-related causes of back pain was unavailable. Another limitation was that identification of LSTV was occasionally difficult, even with objective criteria, due to poor image quality or overprojection of bowel structures; most of these poor-quality images were excluded after the initial screening. We did not make a distinction between unilateral and bilateral pseudoarthrosis and fusion in terms of back pain. Using this additional information would make the model complicated, increasing the four-level outcome to an eight-level outcome and resulting in very small numbers of individuals in some of these groups. Analysis of the raw data did not reveal a difference between unilateral and bilateral pseudoarthrosis and fusion in terms of back pain. Finally, the patient population was selected by OAI for a study of knee OA; the main differences between the OAI cohort and the general population are that the OAI cohort had higher levels of obesity, lower levels of physical activity, and presence of knee OA, and was at risk for knee OA. Of these differences, only obesity (and perhaps low levels of physical activity) is likely associated with back pain; there is no established association between knee OA and back pain (17).
In conclusion, our study highlights the association of LSTV and types II and IV with lumbar back and buttock pain; therefore, LSTV should be considered part of the differential diagnosis of back pain, especially in cases of pain refractory to conventional management.
Advances in Knowledge.
• The prevalence of lumbosacral transitional vertebrae (LSTV) with knee osteoarthritis or risk factors for knee osteoarthritis was 18.1% in a middle-aged and elderly population, with more men affected than women.
• According to Castellvi classification, patients with LSTV that was pseudoarticulated to the sacrum (such as types II and IV) were prone to back and buttock pain (P < .001 and P = .001 for types II and IV, respectively).
• Low back pain is more severe in patients with LSTV types II and IV (P < .001) and is associated with lower physical activity levels (P < .001 and P = .001 for types II and IV, respectively).
Implication for Patient Care.
• LSTV types II and IV are associated with back pain, which may affect patient care.
Disclosures of Conflicts of Interest: L.N. Financial activities related to the present article: none to disclose. Financial activities not related to the present article: none to disclose. Other relationships: none to disclose. H.A. Financial activities related to the present article: none to disclose. Financial activities not related to the present article: none to disclose. Other relationships: none to disclose. W.V. Financial activities related to the present article: none to disclose. Financial activities not related to the present article: none to disclose. Other relationships: none to disclose. F.L. Financial activities related to the present article: none to disclose. Financial activities not related to the present article: none to disclose. Other relationships: none to disclose. A.H. Financial activities related to the present article: none to disclose. Financial activities not related to the present article: none to disclose. Other relationships: none to disclose. J.A.L. Financial activities related to the present article: none to disclose. Financial activities not related to the present article: none to disclose. Other relationships: none to disclose. M.C.N. Financial activities related to the present article: none to disclose. Financial activities not related to the present article: none to disclose. Other relationships: none to disclose. C.E.M. Financial activities related to the present article: none to disclose. Financial activities not related to the present article: none to disclose. Other relationships: none to disclose. N.E.L. Financial activities related to the present article: none to disclose. Financial activities not related to the present article: none to disclose. Other relationships: none to disclose. T.M.L. Financial activities related to the present article: none to disclose. Financial activities not related to the present article: institution and individual receives consultancy fees from GE; institution receives general grant from GE. Other relationships: none to disclose.
Received January 6, 2012; revision requested February 20; revision received April 23; accepted May 3; final version accepted May 8.
Current address: Department of Radiology, University of Texas Health Science Center at San Antonio, San Antonio, Tex.
Current address: Department of Radiology, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand.
Supported by NIH U01 AR055079 and P50 AR060752, as well as through the Osteoarthritis Initiative, which is a public-private partnership composed of five contracts (N01-AR-2-2258; N01-AR-2-2259; N01-AR-2-2260; N01-AR-2-2261; N01-AR-2-2262) funded by the National Institutes of Health, a branch of the Department of Health and Human Services, and conducted by the Osteoarthritis Initiative Study Investigators. Private funding partners include Merck Research Laboratories; Novartis Pharmaceuticals, GlaxoSmithKline; and Pfizer. Private sector funding for the OAI is managed by the Foundation for the National Institutes of Health, and NIH grant K24-AR048841 to N.E.L.
Funding: This research was supported by the National Institutes of Health (grants NIH U01 AR055079, P50 AR060752, N01-AR-2-2258, N01-AR-2-225, N01-AR-2-2260, N01-AR-2-2261, N01-AR-2-2262, and K24-AR048841).
Abbreviations:
- CI
- confidence interval
- LBP
- low back pain
- LSTV
- lumbosacral transitional vertebrae
- OA
- osteoarthritis
- OAI
- Osteoarthritis Initiative
- OR
- odds ratio
- PASE
- Physical Activity Scale for the Elderly
References
- 1.Becker A, Held H, Redaelli M, et al. Low back pain in primary care: costs of care and prediction of future health care utilization. Spine 2010;35(18):1714–1720 [DOI] [PubMed] [Google Scholar]
- 2.Luo X, Pietrobon R, Sun SX, Liu GG, Hey L. Estimates and patterns of direct health care expenditures among individuals with back pain in the United States. Spine 2004;29(1):79–86 [DOI] [PubMed] [Google Scholar]
- 3.Frymoyer JW, Cats-Baril WL. An overview of the incidences and costs of low back pain. Orthop Clin North Am 1991;22(2):263–271 [PubMed] [Google Scholar]
- 4.Stewart WF, Ricci JA, Chee E, Morganstein D, Lipton R. Lost productive time and cost due to common pain conditions in the US workforce. JAMA 2003;290(18):2443–2454 [DOI] [PubMed] [Google Scholar]
- 5.Deyo RA, Weinstein JN. Low back pain. N Engl J Med 2001;344(5):363–370 [DOI] [PubMed] [Google Scholar]
- 6.Luoma K, Vehmas T, Raininko R, Luukkonen R, Riihimäki H. Lumbosacral transitional vertebra: relation to disc degeneration and low back pain. Spine 2004;29(2):200–205 [DOI] [PubMed] [Google Scholar]
- 7.Taskaynatan MA, Izci Y, Ozgul A, Hazneci B, Dursun H, Kalyon TA. Clinical significance of congenital lumbosacral malformations in young male population with prolonged low back pain. Spine 2005;30(8):E210–E213 [DOI] [PubMed] [Google Scholar]
- 8.Konin GP, Walz DM. Lumbosacral transitional vertebrae: classification, imaging findings, and clinical relevance. AJNR Am J Neuroradiol 2010;31(10):1778–1786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Castellvi AE, Goldstein LA, Chan DP. Lumbosacral transitional vertebrae and their relationship with lumbar extradural defects. Spine 1984;9(5):493–495 [DOI] [PubMed] [Google Scholar]
- 10.Hughes RJ, Saifuddin A. Imaging of lumbosacral transitional vertebrae. Clin Radiol 2004;59(11):984–991 [DOI] [PubMed] [Google Scholar]
- 11.Tini PG, Wieser C, Zinn WM. The transitional vertebra of the lumbosacral spine: its radiological classification, incidence, prevalence, and clinical significance. Rheumatol Rehabil 1977;16(3):180–185 [DOI] [PubMed] [Google Scholar]
- 12.Quinlan JF, Duke D, Eustace S. Bertolotti’s syndrome. A cause of back pain in young people. J Bone Joint Surg Br 2006;88(9):1183–1186 [DOI] [PubMed] [Google Scholar]
- 13.Eyo MU, Olofin A, Noronha C, Okanlawon A. Incidence of lumbosacral transitional vertebrae in low back pain patients. West Afr J Radiol 2001;8(1):1–6 [Google Scholar]
- 14.Delport EG, Cucuzzella TR, Kim N, Marley J, Pruitt C, Delport AG. Lumbosacral transitional vertebrae: incidence in a consecutive patient series. Pain Physician 2006;9(1):53–56 [PubMed] [Google Scholar]
- 15.Dai L. Lumbosacral transitional vertebrae and low back pain. Bull Hosp Jt Dis 1999;58(4):191–193 [PubMed] [Google Scholar]
- 16.Otani K, Konno S, Kikuchi S. Lumbosacral transitional vertebrae and nerve-root symptoms. J Bone Joint Surg Br 2001;83(8):1137–1140 [DOI] [PubMed] [Google Scholar]
- 17.Rubin DI. Epidemiology and risk factors for spine pain. Neurol Clin 2007;25(2):353–371 [DOI] [PubMed] [Google Scholar]
- 18.Altman RD, Gold GE. Atlas of individual radiographic features in osteoarthritis, revised. Osteoarthritis Cartilage 2007;15(Suppl A):A1–A56 [DOI] [PubMed] [Google Scholar]
- 19.Husni ME, Meyer KH, Cohen DS, Mody E, Qureshi AA. The PASE questionnaire: pilot-testing a psoriatic arthritis screening and evaluation tool. J Am Acad Dermatol 2007;57(4):581–587 [DOI] [PubMed] [Google Scholar]
- 20.Washburn RA, Ficker JL. Physical Activity Scale for the Elderly (PASE): the relationship with activity measured by a portable accelerometer. J Sports Med Phys Fitness 1999;39(4):336–340 [PubMed] [Google Scholar]
- 21.Martin KA, Rejeski WJ, Miller ME, James MK, Ettinger WH, Jr, Messier SP. Validation of the PASE in older adults with knee pain and physical disability. Med Sci Sports Exerc 1999;31(5):627–633 [DOI] [PubMed] [Google Scholar]
- 22.Washburn RA, Smith KW, Jette AM, Janney CA. The Physical Activity Scale for the Elderly (PASE): development and evaluation. J Clin Epidemiol 1993;46(2):153–162 [DOI] [PubMed] [Google Scholar]
- 23.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33(1):159–174 [PubMed] [Google Scholar]
- 24.Schultz VA, Watson AG. Lumbosacral transitional vertebra and thoracic limb malformations in a Chihuahua puppy. J Am Anim Hosp Assoc 1995;31(2):101–106 [DOI] [PubMed] [Google Scholar]
- 25.Brault JS, Smith J, Currier BL. Partial lumbosacral transitional vertebra resection for contralateral facetogenic pain. Spine 2001;26(2):226–229 [DOI] [PubMed] [Google Scholar]
- 26.Connolly LP, d’Hemecourt PA, Connolly SA, Drubach LA, Micheli LJ, Treves ST. Skeletal scintigraphy of young patients with low-back pain and a lumbosacral transitional vertebra. J Nucl Med 2003;44(6):909–914 [PubMed] [Google Scholar]
- 27.Hinterdorfer P, Parsaei B, Stieglbauer K, Sonnberger M, Fischer J, Wurm G. Segmental innervation in lumbosacral transitional vertebrae (LSTV): a comparative clinical and intraoperative EMG study. J Neurol Neurosurg Psychiatry 2010;81(7):734–741 [DOI] [PubMed] [Google Scholar]
- 28.Leboeuf C, Kimber D, White K. Prevalence of spondylolisthesis, transitional anomalies and low intercrestal line in a chiropractic patient population. J Manipulative Physiol Ther 1989;12(3):200–204 [PubMed] [Google Scholar]
- 29.Marks RC, Thulbourne T. Infiltration of anomalous lumbosacral articulations. Steroid and anesthetic injections in 10 back-pain patients. Acta Orthop Scand 1991;62(2):139–141 [DOI] [PubMed] [Google Scholar]
- 30.Oyinloye OI, Abdulkadir AY, Babalola OM. Incidence and patterns of lumbosacral transitional vertebrae, in patients with low backpain in a Nigerian hospital. Nig Q J Hosp Med 2009;19(2):95–99 [PubMed] [Google Scholar]
- 31.Chang HS, Nakagawa H. Altered function of lumbar nerve roots in patients with transitional lumbosacral vertebrae. Spine 2004;29(15):1632–1635; discussion 1635 [DOI] [PubMed] [Google Scholar]
- 32.Paraskevas G, Tzaveas A, Koutras G, Natsis K. Lumbosacral transitional vertebra causing Bertolotti’s syndrome: a case report and review of the literature. Cases J 2009;2:8320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Connolly LP, Drubach LA, Connolly SA, Treves ST. Young athletes with low back pain: skeletal scintigraphy of conditions other than pars interarticularis stress. Clin Nucl Med 2004;29(11):689–693 [DOI] [PubMed] [Google Scholar]
- 34.Miyoshi Y, Yasuhara T, Date I. Posterior decompression of far-out foraminal stenosis caused by a lumbosacral transitional vertebra—case report. Neurol Med Chir (Tokyo) 2011;51(2):153–156 [DOI] [PubMed] [Google Scholar]
- 35.Hashimoto M, Watanabe O, Hirano H. Extraforaminal stenosis in the lumbosacral spine. Efficacy of MR imaging in the coronal plane. Acta Radiol 1996;37(5):610–613 [DOI] [PubMed] [Google Scholar]
- 36.Peh WC, Siu TH, Chan JH. Determining the lumbar vertebral segments on magnetic resonance imaging. Spine 1999;24(17):1852–1855 [DOI] [PubMed] [Google Scholar]


