Abstract
Primary care is a major component of England's National Health Service (NHS), responsible for approximately 300 million consultations per year with GPs in England, which represents 70–90% of all patient contacts with the NHS. In addition to providing healthcare to the registered population, GPs are charged with coordination and gatekeeping of access to services provided by secondary care, tertiary care and other allied healthcare providers. As GPs will be assuming a key role in commissioning health services in England, there is a clear opportunity to re-model care delivery to maximize outcomes, cost efficiency and patient access by focusing on diseases that are most amenable to management in primary care. It is essential that there is evidence to inform what conditions are most sensitive to management in primary care – commonly referred to as primary care sensitive conditions or ambulatory care sensitive conditions. Such definitions would aid resource planning, drafting of local management protocols and simplification of the interface between primary and secondary care for a number of chronic conditions. Indeed, inappropriate utilization of secondary care resources is likely to represent a significant opportunity cost to healthcare providers and may be less desirable for patients.
Primary care is a major component of England's National Health Service (NHS), responsible for approximately 300 million consultations per year with general practitioners (GPs) in England,1 which represents 70–90% of all patient contacts with the NHS.2 In addition to providing healthcare to the registered population, GPs are charged with coordination and gatekeeping of access to services provided by secondary care, tertiary care and other allied healthcare providers.
While primary care has a role to play in the management of acute conditions, there are a number of alternative means by which individuals can directly access appropriate advice and care for acute problems via services such as NHS Direct, Walk-in Centres and Accident & Emergency Departments. In contrast, the management of chronic conditions generally lies within the remit of GPs, and patients are usually only able to obtain ongoing specialist care for their condition if referred to a specialist by their GP.
Primary care consultation rates in England are rising year-on-year,1 and the role of primary care in managing chronic conditions will increase, against a backdrop of a drive to contain costs, as a result of both an ageing population and changes in healthcare policy.3,4 In addition to the increasing demand for management of chronic conditions in primary care that an ageing population will place upon health services, the way in which services are designed and delivered also needs to change to ensure that primary healthcare is both accessible and appropriate to the needs of an increasingly ageing population with a rising burden of chronic disease.5 As GPs will be assuming a key role in commissioning health services in England, there is a clear opportunity to re-model care delivery to maximize outcomes, cost efficiency and patient access by focusing on diseases that are most amenable to management in primary care.6,7
It is essential that there is evidence to inform what conditions are most sensitive to management in primary care – commonly referred to as primary care sensitive conditions (PCSCs) or ambulatory care sensitive conditions (ACSCs). Such definitions would aid resource planning, drafting of local management protocols and simplification of the interface between primary and secondary care for a number of chronic conditions. Indeed, inappropriate utilization of secondary care resources is likely to represent a significant opportunity cost to healthcare providers and may be less desirable for patients.
Defining primary care sensitive conditions
PCSCs can be broadly defined as conditions for which good primary care – defined by the World Health Organization as ‘ … first-contact, accessible, continued, comprehensive and coordinated care’ – can potentially prevent the need for hospitalization, or for which early intervention can prevent complications or more severe disease.8 PCSCs commonly cited in academic literature include angina, asthma, chronic obstructive pulmonary disease, congestive heart failure, diabetes mellitus and hypertension among others.9–11
Definitions of PCSCs tend to reflect expert consensus on whether primary care can achieve the desired clinical endpoints with respect to these diagnoses in the context of the resources available to it. Indeed, the prevalence and severity of such diseases is likely to be a function of prevention, prompt diagnosis and continuity, and co-ordination of care – all of which are key and accepted functions of primary care.12 By means of example, there are a number of levers by which primary care can modulate the severity of asthma and reduce the risk of severe exacerbations requiring hospital treatment (see Box 1).
Box 1. Influences that primary care can exert on risk of acute asthma admissions.
Symptom and medication reviews:
Ensuring that the patient's symptoms are adequately controlled by their current medication and that therapy is adjusted according to local or national protocols; doing so should decrease the frequency and severity of major exacerbations, thereby reducing the need for emergency treatment in hospital;
The mode of delivery and type of inhaler should be closely aligned with what the patient feels confident in using. For example, some patients may find the required coordination to use ‘puffer’ inhalers difficult and may benefit from using dry powder inhalers or use of a spacer; tailoring how their medication is delivered to the needs of the patient will maximize the efficacy of drug delivery, hence reducing symptom severity and the risk of exacerbations.
Patient education:
Understanding the medication that they have been prescribed – particularly the difference between bronchodilators and steroid inhalers with respect to their roles as ‘relievers’ or ‘preventers’. Ensuring that the patient has this knowledge may allow for reductions in acute asthma exacerbations and may reduce the risk of hospital attendance or admission;
Providing knowledge on good inhaler technique, thereby ensuring maximal therapeutic effect from their medications;
Engendering confidence in self-management may help empower patients to be proactive in controlling their own symptoms without the need to consult community or hospital medical staff for minor exacerbations;
Educating the patient with regards to ‘triggers’ of asthma exacerbations, be they seasonal, activity-related or environmental, so that they can proactively adjust their medication accordingly or, where possible, avoid these ‘triggers’;
Provision of other health education interventions – such as smoking cessation – that may reduce frequency and severity of exacerbations.
Accessibility of primary care:
In order to establish an optimal therapeutic relationship, patients must be able to access care that is delivered in an appropriate and understandable manner when needed. Delivering care in this manner supports the therapeutic objectives of primary care, and may allow for early provision of treatment to prevent worsening symptoms deteriorating into a severe exacerbation of asthma.
While many chronic diseases may seem good potential candidates for being classed as a PCSC, there is considerable variation in which diseases are deemed primary care sensitive13 both within academic literature, among clinicians and between health systems (Table 1). This lack of agreement may relate to disagreement as to what it is reasonable to expect of primary care or, perhaps, what role primary care should assume within a health system. When considering whether a condition is truly primary care sensitive, one has to consider the functions of primary care which may reasonably alter the course of disease (Table 2).
Table 1.
Selected PCSC definitions
| Agency for Healthcare Research andQuality8 (USA) | Victorian Public HealthDivision14 (Australia) | National HealthService13,24 (UK) |
|---|---|---|
| Adult asthma | Angina | Angina (without procedure) |
| Angina (without procedure) | Appendicitis* | Asthma |
| Bacterial pneumonia | Asthma | Cellulitis |
| Chronic obstructive pulmonary disease | Cellulitis | Congestive heart failure |
| Congestive heart failure | Chronic obstructive pulmonary disease | Convulsions and epilepsy |
| Dehydration | Congestive heart failure | Chronic obstructive pulmonary disease |
| Diabetes – long-term complication | Convulsions and epilepsy | Dehydration and gastroenteritis |
| Diabetes – lower extremity amputation | Dehydration and gastroenteritis | Dental conditions |
| Diabetes – short-term complication | Dental conditions | Diabetes complications |
| Hypertension | Diabetes complications | Ear, nose and throat infections |
| Low birth weight* | Ear, nose and throat infections | Gangrene |
| Paediatric asthma | Gangrene | Hypertension |
| Paediatric gastroenteritis | Hypertension | Influenza and pneumonia |
| Perforated appendix* | Influenza and pneumonia | Iron deficiency anaemia |
| Uncontrolled diabetes | Iron deficiency anaemia | Nutritional deficiency |
| Urinary tract infection | Nutritional deficiencies | Other vaccine-preventable diseases |
| Other vaccine-preventable diseases | Pelvic inflammatory disease | |
| Pelvic inflammatory disease | Perforated/bleeding ulcer | |
| Perforated/bleeding ulcer | Pyelonephritis | |
| Pyelonephritis |
PCSC = Primary care sensitive condition
* = PCSC unique to this list
Table 2.
The role of primary care in adjusting disease course and risk of hospitalization in selected PCSCs (adapted from Caminal et al.17)
| Intervention | Infectious diseases | Non-infectious diseases |
|---|---|---|
| Primary prevention | Vaccine-preventable diseases | Chronic obstructive pulmonary disease |
| Hypertensive vascular disease | ||
| Early diagnosis and treatment | Acute pyelonephritis | Bleeding or perforated gastro-duodenal ulcer |
| Ongoing control and management | Appendicitis with complications | Chronic obstructive pulmonary disease |
| Pelvic inflammatory disease | Diabetes mellitus | |
| Peritonsillar abscess | Disorders of hydro-electrolyte metabolism | |
| Pneumonia | Heart failure | |
| Rheumatic fever | Hypertensive vascular disease | |
| Congenital syphilis | Iron deficiency anaemia | |
| Tuberculosis | Nutritional deficiencies | |
| Asthma | ||
| Bleeding or perforated gastro-duodenal ulcer | ||
| Diabetes mellitus | ||
| Heart failure | ||
| Hypertensive vascular disease |
PCSC, primary care sensitive condition
Although commonly cited as potential modulators of preventable and primary care sensitive hospital admissions, the notable omission of many common mental health disorders, such as depression and anxiety, from the more established and commonly cited lists of PCSCs8,13,14 may also indicate a potential bias against the consideration of mental health disorders as primary care sensitive. Indeed, in insurance-based health systems, the presence of a mental health disorder such as schizophrenia may impact the ability of an individual to maintain their health coverage, thereby imposing a barrier to accessing primary care services and obtaining timely healthcare in the early stages of evolving disorders – both mental health and non-mental health – that, in turn, may reduce the risk of hospitalization.15
The financial, political and sociodemographic environments in which any given primary care system exists should also be taken into account, as these external factors may modulate not only what is considered a healthcare priority, but also whether primary care would be able to discharge interventions in a timely and effective manner.
The ability of primary care practitioners to meaningfully impact the clinical course of many PCSCs depends not only on assigning the responsibility of care for these conditions to primary care but ensuring that sufficient and appropriate resources are available in order for primary care to discharge these duties effectively and in a timely manner. Differences in resourcing and allocative efficiency in resource distribution may, to some extent, explain the variations in outcomes; such as PCSC emergency admission rates across primary care providers. Furthermore, the ability to provide relevant care at the appropriate time may also depend on the suitability of a given health system to detect disease at an early stage, thereby enabling the delivery of interventions that may focus on secondary prevention.
Therefore, when considering whether a disease is truly a PCSC, the levers by which primary care may be reasonably expected to alter the course of disease – or prevent its occurrence through primary prevention – have to be considered. Such levers are well established for many common chronic diseases, but differing views on what constitutes the role and scope of primary care and the impact that it can reasonably expect to have on patient health behaviours may lead to variation in what is considered as primary care sensitive in practice.
While there may be legitimate differences in the structure, function and funding of primary care across health systems, the lack of an agreed, evidence-based list of conditions that can be universally accepted as PCSCs undermines efforts to meaningfully quantify and compare performance both within and between primary care health systems. Such an approach should ideally involve consensus between primary and secondary care and include a documented, valid method by which a shortlist of diseases was arrived at.
Hospital admissions for PCSCs have become an increasingly popular measure of primary care performance as, under the assumption that timely, appropriate, efficacious primary care interventions are available to and accessible by patients, the risk of unexpected and potentially preventable complications and deterioration in patients should be relatively low.9,13 The importance of primary care in the management of these conditions is highlighted by findings that support an inverse relationship between access to primary healthcare and the risk of hospitalization due to underlying PCSCs.16–18
As markers of primary care performance, hospital admissions for PCSCs may provide insight into potential shortcomings of either the structures or processes present in primary care, the effects of the socioeconomic environment in which they operate or to be used to draw inferences about the health of a given population. Many previous analyses examining PCSC admissions assume that primary care is operating in a closed system – such that it would be logical to assume that, given appropriate and timely treatment, hospital admissions for PCSCs would be largely preventable. But this assumes that the disease course – and patient behaviour – is wholly predictable and modifiable by primary care interventions. Furthermore, when considering the structural aspects of primary care, this approach also makes the assumption that there are no cultural, financial or social barriers to accessing services.
Primary care sensitive conditions and socioeconomic status
Socioeconomic factors play a crucial role in determining a given patient's level of health literacy, their ability to cope with illness and their willingness to engage with primary care – all of which have an association with increased rates of unscheduled hospitalization for certain conditions. Unsurprisingly, these disparities in PCSC admission rates are also present in healthcare systems that are not free at the point of access.11 It is of note, however, that while socioeconomic factors are associated with unscheduled hospitalization, the accessibility of primary healthcare services remains a key and independent predictor of preventable hospitalizations for a range of PCSCs.9
The delivery of healthcare and, ultimately healthcare outcomes, are dependent on a wide range of cultural, social, political and economic factors that are interlinked, with the individual patient at the centre of these interdependent layers of influence. Many of these factors – and the policy that pertains to them – are outside of what is traditionally considered the scope and sphere of the influence of medicine, yet profoundly affect an individual's health and their health outcomes. So, perhaps, it is not merely deciding what conditions may be amenable for management in primary care, but also what it is reasonable for primary care to be able to achieve in the prevailing health and non-health policy landscape in addition to the impact that population risk factors may have on the incidence and disease course of PCSCs.
Primary care sensitive conditions and policy response
Some healthcare purchasers in the USA recognize that variation in primary care performance may be a function of a provider's practice environment. They are demonstrating a willingness to increase payments for primary care providers because they believe that this delivery model could ultimately contribute to lower hospital admission rates for PCSCs and lower overall healthcare costs. Purchasers pursuing this approach support not only the availability of primary care providers to fulfil the role of care coordinators, but also an environment that makes this possible. This strategy is generally referred to as the primary care medical home.
Primary care medical home providers are expected to have access to electronic health records to support after-hours management, and for supporting communication with specialists, emergency departments and hospitals for patients who need and use these services. Furthermore, they are expected to manage patients’ acute care needs including those that arise after-hours and to employ staff who can perform a variety of services such as prescription renewals and follow-up on abnormal test results.
There is an increasing evidence base supporting the ability of medical homes to provide clinically sound and cost-effective treatment in comparison to the traditional specialist-dominant model of healthcare delivery in the USA. Cost-savings under such a primary care-focused system may be as high as 30%, largely as a result of fewer hospitalizations, reduced duplication of work and more appropriate use of technology.19
The structure of the NHS in England is largely centred on universal access to primary care, where is it is well established as the accepted and preferred point of initial contact with health services regardless of locality. This structure enables primary care facilities to act as gatekeepers to secondary and tertiary care services and thereby enable a degree of containment of the burden of care for many chronic diseases within the community. As a result, associations between primary care factors and PCSC admission rates in England have generally been weaker. However, primary care physician supply in England has been shown to be associated with under-diagnosis of PCSCs such as cardiovascular disease.20
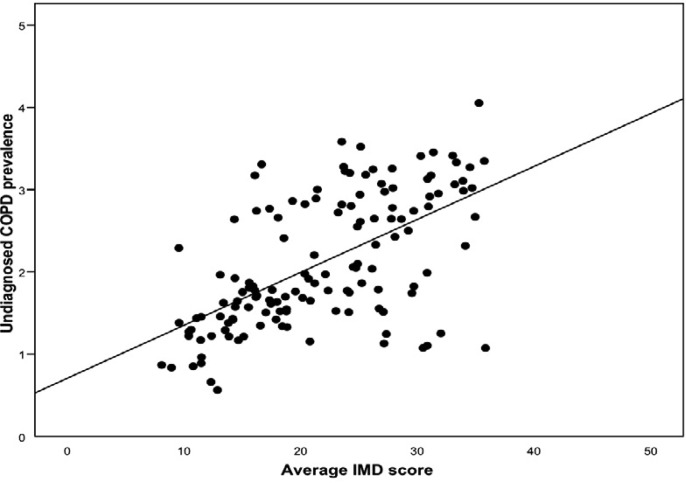
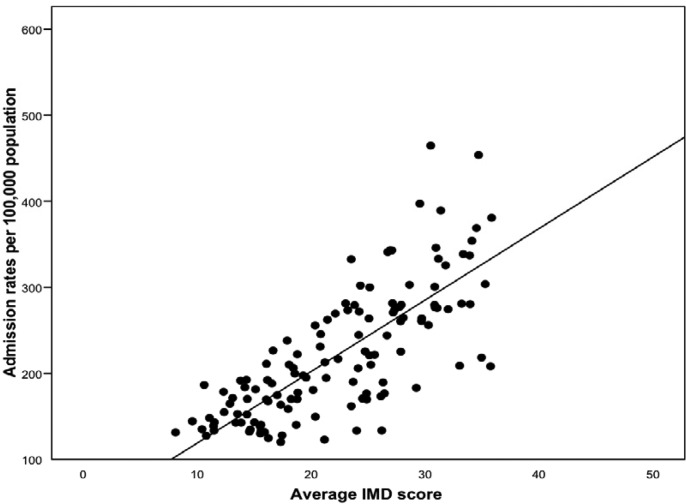
Despite the weak associations between primary care factors and PCSC admission rates, significant socioeconomic differences remain with respect to utilization of Accident & Emergency departments and admission rates for chronic diseases such as asthma.21 These differences may reflect differentials in the accessibility and appropriateness of the mode of primary care delivery according to socioeconomic status, which may modulate the ability of primary care to not only provide appropriate care at an appropriate time, but also alter the likelihood of detecting chronic PCSCs at an early stage where the risk of complications may be more amenable to secondary prevention activities. For example, both rates of undiagnosed disease and admission rates for chronic obstructive pulmonary disease are strongly associated with area socioeconomic deprivation (Figures 1 and 2).
Figure 1.
Relation between mean neighbourhood socioeconomic status (Index of Multiple Deprivation, IMD), and undiagnosed prevalence of COPD (n = 151). COPD, chronic obstructive pulmonary disease
Figure 2.
Relation between mean neighbourhood socioeconomic status (Index of Multiple Deprivation, IMD), and directly standardized COPD hospital admission rates (DSR) per 100,000 population (n = 151). COPD, chronic obstructive pulmonary disease
Primary care practitioners are also important actors in the interplay between patients and healthcare outcomes – and, while standardization of practice by protocols is commonplace – the variations in acceptance of risk between practitioners is highly likely to alter the likelihood of referral to secondary care for a given PCSC presentation to primary care.22
While healthcare practitioners in primary care have the potential to fulfil their duties of providing coordinated, comprehensive care close to home, it is essential that they be provided with the necessary resources to do so. For primary care – and the healthcare professionals who work within it – to effectively and efficiently manage an increasing burden of chronic disease, it must be provided with the necessary infrastructure and resources to enable delivery of care. As this necessary service reconfiguration takes place, care must be taken to ensure that the evidence underlying efficacious chronic disease management is appropriate for primary care. Simply applying models of care delivery, and the evidence that underpins them, from secondary care to primary care may not be appropriate; such an approach would neglect to take account of the varying population characteristics, resources and skills that impact delivery of primary care.23
Conclusions
As policy develops, identification of diseases that may be primary care sensitive and the development of a robust evidence-based list of which diseases qualify as PCSCs, in addition to modelling the expected impact of optimal primary care, will be essential for the management of resources and workload of healthcare systems, many of which stand to become increasingly reliant on primary care for the management of a range of chronic diseases. Furthermore, identification of endpoints that may represent failure of the processes of primary care - that take into account ascertainable variation in the impact of optimal preventive primary care – is also of key importance.
Measuring the rates of admission for PCSCs is potentially a useful indicator of primary care performance. However, for this measure to be truly representative of what it seeks to assess, not only does there need to be consensus on what diseases – or disease events – are PCSCs, but also agreement of what is within the power of primary care to change. It has to be borne in mind that while the markers of service quality – and many financial incentives that derive from such markers – in primary care focus on clinical outcomes or actions undertaken by physicians or other healthcare practitioners, a number of non-medical factors exert influence on the healthcare environment and, consequently, on the ability of primary care to effectively discharge its duties and affect change. As the burden of chronic care management increases over the coming decades, healthcare policy is likely to evolve in a manner that places increasing demands on primary care; however, it is essential that primary care is also appropriately resourced to ensure that it is operating in an environment commensurate with achieving the goals and targets that it is set.
Key questions for future research include assessment of what proportion of unplanned admissions for chronic conditions are potentially preventable through better patient education, improved health literacy, and higher quality management in primary care; what healthcare factors or interventions can reduce the risk of complications such as unplanned admissions; the effect of practice-level financial incentives on admission rates for PCSCs; and what proportion of these admissions are either unpredictable or outside the control of the health system.
DECLARATIONS
Competing interests
None declared
Funding
DCG is a Doctoral Research Fellow, funded by the NHS National Institute for Healthcare Research. The Department of Primary Care & Public Health at Imperial College London is grateful for support from the NW London NIHR Collaboration for Leadership in Applied Health Research & Care (CLAHRC), the Imperial NIHR Biomedical Research Centre and the Imperial Centre for Patient Safety and Service Quality (CPSSQ)
Ethical approval
Ethical approval was not required as this article is a discussion piece based on a secondary analysis of existing research findings
Guarantor
DCG
Contributorship
DCG prepared the first and subsequent drafts of the manuscript, AB provided information on the US Health System in addition to feedback on the manuscript, CM, MS and AM edited the manuscript
Acknowledgements
None
References
- 1.Hippisley-Cox J Final Report to the NHS Information Centre and Department of Health: Trends in Consultation Rates in General Practice 1995 to 2008: Analysis of the QResearch® Database. London: NHS Information Centre, 2009 [Google Scholar]
- 2.Majeed A Role of hospitals in NHS must not be undervalued. BMJ 1998;317:1653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.United Nations UN General Assembly – Prevention and Control of Non-Communicable Diseases: Report of the Secretary General. New York: United Nations, 2011 [Google Scholar]
- 4.Majeed A Primary care in Europe: Entering the age of austerity. J Ambul Care Manage 2012;35:162–6 [DOI] [PubMed] [Google Scholar]
- 5.World Health Organisation Active Ageing: Towards Age-Friendly Primary Care. Geneva: World Health Organisation, 2004 [Google Scholar]
- 6.Sibbald B, McDonald R, Roland M Shifting care from hospitals to the community: a review of the evidence on quality and efficiency. J Health Serv Res Policy 2007;12:110–7 [DOI] [PubMed] [Google Scholar]
- 7.Sibbald B, Pickard S, McLeod H, et al. Moving specialist care into the community: an initial evaluation. J Health Serv Res Policy 2008;13:233–9 [DOI] [PubMed] [Google Scholar]
- 8.Agency for Healthcare Research and Quality AHRQ Quality Indicators – Guide to Prevention Quality Indicators: Hospital Admission for Ambulatory Care Sensitive Conditions. Revision 3. Rockville, MD: Agency for Healthcare Research and Quality, 2004 [Google Scholar]
- 9.Bindman AB, Grumbach K, Osmond D, et al. Preventable hospitalizations and access to health care. JAMA 1995;274:305–11 [PubMed] [Google Scholar]
- 10.Bottle A, Aylin P, Majeed A Identifying patients at high risk of emergency hospital admissions: a logistic regression analysis. J R Soc Med 2006;99:406–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Agabiti N, Pirani M, Schifano P, et al. Income level and chronic ambulatory care sensitive conditions in adults: a multicity population-based study in Italy. BMC Public Health 2009;9:457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Starfield B Primary Care: Balancing Health Needs, Services and Technology. New York: Oxford University Press, 1998 [Google Scholar]
- 13.Purdy S, Griffin T, Salisbury C, Sharp D Ambulatory care sensitive conditions: terminology and disease coding need to be more specific to aid policy makers and clinicians. Public Health 2009;123:169–73 [DOI] [PubMed] [Google Scholar]
- 14.Ansari Z The Victorian Ambulatory Care Sensitive Conditions Study: Preliminary Analyses. Melbourne, Victoria: Department of Human Services, Public Health Division, 2001 [Google Scholar]
- 15.Harman JS, Manning WG, Lurie N, Christianson JB Association between interruptions in medicaid coverage and use of inpatient psychiatric services. Psychiatr Serv 2003;54:999–1005 [DOI] [PubMed] [Google Scholar]
- 16.Backus L, Moron M, Bacchetti P, Baker LC, Bindman AB Effect of managed care on preventable hospitalization rates in California. Med Care 2002;40:315–24 [DOI] [PubMed] [Google Scholar]
- 17.Caminal J, Starfield B, Sánchez E, Casanova C, Morales M The role of primary care in preventing ambulatory care sensitive conditions. Eur J Public Health 2004;14:246–51 [DOI] [PubMed] [Google Scholar]
- 18.Laditka JN, Laditka SB, Probst JC More may be better: evidence of a negative relationship between physician supply and hospitalization for ambulatory care sensitive conditions. Health Serv Res 2005;40:1148–66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rosenthal TC The medical home: growing evidence to support a new approach to primary care. J Am Board Fam Med 2008;21:427–40 [DOI] [PubMed] [Google Scholar]
- 20.Soljak M, Samarasundera E, Indulkar T, Walford H, Majeed A Variations in cardiovascular disease under-diagnosis in England: national cross-sectional spatial analysis. BMC Cardiovasc Disord 2011;11:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ormerod LP Adult Asian acute asthma admissions reassessed: Blackburn 1991–1992. Respir Med 1995;89:415–7 [DOI] [PubMed] [Google Scholar]
- 22.Ingram JC, Calnan MW, Greenwood RJ, Kemple T, Payne S, Rossdale M Risk taking in general practice: GP out-of-hours referrals to hospital. Br J Gen Pract 2009;59:e16–24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Graham RP, James PA, Cowan TM Are clinical practice guidelines valid for primary care? J Clin Epidemiol 2000;53:949–54 [DOI] [PubMed] [Google Scholar]
- 24.NHS Institute for Innovation and Improvement NHS Better Care, Better Value Indicators (Incorporating Opportunity Locator). See http://www.productivity.nhs.uk/Indicator/608/For/National/And/25th/Percentile (last accessed 10 March 2012)