Abstract
Purpose
Clinical observations suggest that endplate shape and size are related to complications of disc arthroplasty surgery. Yet, the morphology of the vertebral endplate has not been well defined. This study was conducted to characterize the morphology of lumbar vertebral endplates and to quantify their morphometrics using radiographic, visual and digital measures.
Methods
A total of 591 vertebral endplates from 76 lumbosacral spines of men were studied (mean age 51.3 years). The shape of the vertebral endplates was classified as concave, flat and irregular, and was evaluated from both radiographs and cadaveric samples. Each endplate was further digitized using a laser scanner to quantify diameters, surface area and concavity for the whole endplate and its components (central endplate and epiphyseal rim). The morphological characteristics and morphometrics of the vertebral endplates were depicted.
Results
In both radiographic and visual assessments, more cranial endplates (relative to the disc) were concave and more caudal endplates were flat at all disc levels (p < 0.001). On average, the mean concavity depth was 1.5 mm for the cranial endplate and 0.7 mm for the caudal endplate. From L1/2 down to L5/S1 discs, the vertebral endplate gradually changed into a more oval shape. The central endplate was approximately 70 % of the diameter of the whole endplate and the width of the epiphyseal rim varied from 3 to 7 mm.
Conclusions
There is marked morphological asymmetry between the two adjacent endplates of a lumbar intervertebral disc: the cranial endplate is more concave than the caudal endplate. The size and shape of the vertebral endplate also vary considerably between the upper and lower lumbar regions.
Keywords: Lumbar spine, Endplate, Morphology, Disc arthroplasty, Artificial disc
Introduction
The interface between the vertebral trabeculae and intervertebral disc is the endplate, which comprises the cartilaginous endplate and osseous endplate [1]. The osseous endplate virtually is the shell of the vertebral body and, thus, is also called the vertebral endplate. A vertebral endplate consists of the epiphyseal rim, which is a ring of smooth bone at the peripheral margin of the endplate, and the central endplate, which is the central portion of the endplate. The epiphyseal rim is relatively solid and strong, as compared to the thin and porous central endplate [2].
The endplate is important in maintaining the integrity and functions of the intervertebral disc [3], and its morphology, which is less well known, could have practical relevance, such as for disc arthroplasty. It has been suggested that endplate morphometrics, especially the degree of concavity and concordance between the two endplates adjacent to a disc, may be important to artificial disc design [4–6]. Furthermore, endplate shape has been linked to clinical outcomes of disc arthroplasty [7]. Yet, in vivo standard radiological approaches may not be able to fully depict endplate morphology. While literature on the size of the endplate and its components is sparse [8], detailed reference data of vertebral endplate morphometrics by spinal level could be of important clinical significance in improving the technical success and longevity of disc arthroplasty.
The purposes of this study were to describe the morphological characteristics of the lumbar vertebral endplates from radiographs and cadaveric vertebral bones, and to determine the geometry of the endplate and its components using digital measures.
Materials and methods
Samples
We had access to a lumbar spine archive comprising 149 Caucasian cadavers of men who had passed away in the hospital wards [9]. The inclusion criteria for this archive were men below the age of 64 years, who had been employed before death and whose history of illness was short. Exclusion criteria were chronic illness or long hospitalization and death from cancer or infectious diseases. After a routine autopsy examination of the lumbar spines, anterior–posterior (AP) and lateral radiographs were taken with spines in situ. Then, the lumbosacral vertebrae were dissected and soft tissues around the vertebrae were removed. The vertebral bones were dried spontaneously under a well-ventilated fume hood at room temperature. Together with radiography films, the dried vertebrae were archived for later visual and digital assessments [9].
In designing a series of studies of which this study was a part, a primary interest was to explore associations between endplate morphometrics and disc degeneration and back pain. Thus, we selected lumbar spines from the archive based solely on the availability of low back pain history data and disc degeneration data. All the spines with data of both back pain history and disc degeneration were included in the current study, irrespective of the presence or absence of low back pain or disc degeneration. Low back pain data were acquired for only 84 of the subjects, as contact of a family member was required, and 8 were excluded due to missing disc degeneration data, which left a sample of 76 lumbosacral spines included in the current study. Some of the vertebrae in the selected spines were lost in preservation, leaving 266 cadaveric lumbar vertebrae (L1–L5) and 69 sacral vertebrae (S1) in the current sample. In the radiographic and visual endplate assessment, there were 600 endplates (264 cranial endplates and 336 caudal endplates) studied. In digital measurements, 9 endplates were excluded because of poorly scanned images, leaving a total number of 591 vertebral endplates (264 cranial endplates and 327 caudal endplates). The mean age of the sample was 51.3 years (range 21–64 years). In the current study, we specify the vertebral endplates as cranial or caudal, with respect to the intervertebral disc. The study was approved by the health research ethics board of the author’s institute.
Radiographic assessments
Both radiographic and visual assessments were performed by an orthopedic surgeon (Y.W). Using the lateral radiograph of the lumbar spine, the endplate shape was classified as: concave if the lateral endplate image demonstrated a smooth concave curvature; flat if the endplate appeared as approximately a straight line and no apparent curvature was seen; or irregular if the endplate appeared convex, jagged or rough due to intensive calcification. In addition, a special endplate curvature on the AP radiograph, the Cupid’s bow contour (Fig. 1), was evaluated as present or absent. This Cupid’s bow contour is a parasagittal concave curvature similar to a bow and is thought to be a normal endplate curvature variation [10].
Fig. 1.

The AP radiograph of a lumbar spine shows the Cupid’s bow contour at the cranial endplates of L4/5 and L5/S1 intervertebral discs
Visual assessments
In line with radiological assessments, the endplates were also visually classified into three basic shapes: concave if the central endplate was lower as compared to the epiphyseal rim, typically with an apparent curvature; flat if the central endplate and the epiphyseal rim were almost in the same plane without apparent curvature; or irregular if the central endplate was higher or convex as compared to the epiphyseal rim, or the endplate surface was rough or irregular. If an endplate was evaluated as concave, the curvature apex was further classified as: single apex if there was only one apex, which usually crosses the mid-sagittal axis of the endplate; double apex if there were two para-sagittal apexes, with a protruded ridge between. Correspondingly, no apex was given to a flat or irregular endplate.
For the radiographic and visual assessments, a random sample of 124 endplates was re-evaluated 1 week later. Kappa statistics were used to examine the intra-rater reliability.
Digital measurements
Laser scanning and image processing
Each vertebral endplate was scanned using a Konica Minolta non-contact three-dimension (3D) digitizer (VIVID 910, Konica Minolta Sensing Americas, Inc., Ramsey, NJ, USA) to acquire surface geometric parameters. This 3D line triangulation scanner is a high-speed, highly accurate laser scanning system to digitize the surface geometry of a targeted object.
Using the telescopic lens and the high accuracy mode (precision 8 μm, 640 × 480 pixels, input time 2.5 s), all scans were performed under the following standard conditions: the camera positioned horizontally on a table with a height of 1.5 m; the vertebra placed vertically in an adjustable holder at a stand-off distance of 0.6 m, with the endplate facing the camera lens and ambient room lighting used. According to the pre-scan images, the position of the vertebra was adjusted to obtain the best image for the endplate. Both endplates of a lumbar vertebra were scanned. The scanner was operated via a computer using the affiliated program Polygon Editing Tool (PET, version 2.21). Unneeded vertebral components in the acquired 3D virtual images, such as the posterior elements and osteophytes, were deleted using the PET program, leaving only the vertebral endplate. In brief, the vertebral endplate was scanned into a total number of 30,000–50,000 digital points, each with a 3D coordinate. Based on the digital data, a 3D image was generated for each endplate to measure its surface geometry.
Measurement of endplate geometry
AP and transverse diameters (mm) and circularity
For both the whole endplate and the central endplate, the AP diameter was measured from the mid-sagittal plane. The transverse diameter was defined as the maximal distance in the coronal plane (Fig. 2). For the epiphyseal rim, the anterior and posterior widths were measured from the mid-sagittal plane and the lateral width was acquired from the right side in the coronal plane (Fig. 2). The endplate circularity was defined as the ratio of the AP diameter to the transverse diameter. It reflects the axial shape of the endplate, without taking the concavity into account. The circularity of a circle is 1.
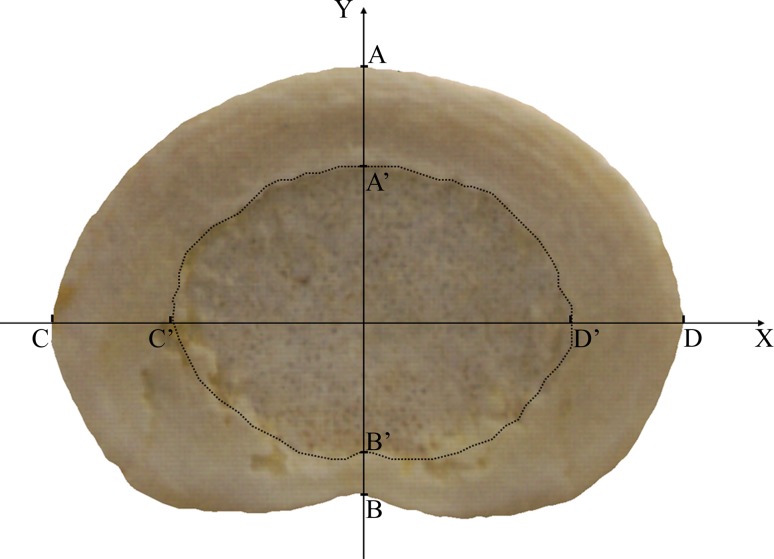
Fig. 2.
A typical scanned 3D image of vertebral endplate (cranial endplate of L3/4 disc). The vertebral endplate consists of a ring of solid epiphyseal rim outside and a porous central endplate inside. Diameter measurements were acquired from X axis (the mid-coronal plane) and Y axis (the mid-sagittal plane). Line AB and CD were measured as AP and transverse diameters of the endplate, respectively. Correspondingly, line A′B′ and C′D′ were measured as the AP and transverse diameters of the central endplate. For the epiphyseal rim, line AA′ and BB’ were measured as the anterior and posterior widths and line CC′ was measured as the lateral width. Three points from the epiphyseal rim, one each from line AA′, CC′ and DD′, were used to define an axial reference plane for measuring the concavity of the endplate. The central endplate and the epiphyseal rim were later radiologically separated (dash line) to measure their surface areas
Surface area (cm2)
The measurement of surface area was provided by the PET program directly. With the aim of acquiring specific area measurements for endplate components, the 3D image of each endplate was further partitioned into the central endplate and the epiphyseal rim by manually segmenting the regions of interest along the boundary between them (Fig. 2). The corresponding images were saved separately and the surface areas were acquired for the whole endplate, the central endplate and the epiphyseal rim.
Concavity (mean depth, mm)
A 3D graph software Dplot (version 2.2.6.3; HydeSoft Computing LLC., Vicksburg, MS, USA) was further used to measure the concavity of the endplate. After reconstructing the 3D endplate plots, an axial reference plane was defined using three points from the epiphyseal rim (one anterior point from the mid-sagittal plane, two lateral points from the coronal plane, Fig. 2). Between the axial reference plane and the endplate surface was the concavity space. The Dplot program provided a series of concavity measurements such as volume, mean depth and depth variations. In the current study, only the mean depth was used to indicate the magnitude of endplate concavity. If an endplate was evaluated as flat or irregular in visual assessment, the concavity depth was defined as zero.
The reliability, validity and precision of laser scanning for recording surface geometry are well established [11, 12]. In addition, a random sample of 30 endplates was measured twice to examine the intra-rater reliability, using intra-class correlation coefficients (ICC).
Statistical analysis
Descriptive statistics were used to depict the geometry of the endplate and its components. χ2 test was used to compare the prevalence of endplate shapes resulting from categorical radiographic and visual assessments. Pearson correlation coefficient was used to indicate the criterion validity of radiographic endplate shape evaluation, referring to visual assessments. Multiple comparisons were tested using ANOVA and Bonferroni test. To describe the changes of endplate morphometrics in relation to disc level, a trend analysis using a variance-weighted least squares model [13, 14] was used and cranial and caudal endplates were examined together. Shapiro–Wilk test was used to examine the normality of data distribution over subgroups. T tests were used to examine differences for normally distributed data. If data were not normally distributed, nonparametric tests, such as Sign tests, were used. As the endplate shapes were reportedly different in the upper (L1/2, L2/3 and L3/4 discs) and lower lumbar regions (L4/5 and L5/S1 discs) [5], we further grouped cranial and caudal endplates into upper and lower lumbar regions and compared the degree of endplate concavity. In addition, the difference in concavity of cranial and caudal endplates adjacent to the same disc was further examined using paired t tests or Wilcoxon signed-rank tests by disc level. Statistical analyses were performed using STATA (Version 9.2, StataCorp LP, USA).
Results
Reliability of the measures
The intra-rater reliabilities of the radiographic and visual measures of endplate shape were “good” or “excellent” (Kappa = 0.66–0.83, Table 1), according to Landis and Koch [15]. All the digital measurements were highly reliable (ICC = 0.85–0.98, Table 1).
Table 1.
Intra-rater reliability of the endplate measurements
| Measurements | Kappa | 95 % CI |
|---|---|---|
| Radiographic assessments | ||
| Shape | 0.66 | (0.53, 0.78) |
| Cupid’s bow contour | 0.83 | (0.66, 0.99) |
| Visual assessments | ||
| Shape | 0.78 | (0.68, 0.87) |
| Apex | 0.82 | (0.74, 0.90) |
| Digital measurements | ICC | |
| AP diameter | 0.96 | (0.92, 0.98) |
| Transverse diameter | 0.98 | (0.96, 0.99) |
| Circularity | 0.95 | (0.90, 0.98) |
| Surface area | 0.97 | (0.94, 0.99) |
| Central endplate area | 0.95 | (0.89, 0.97) |
| Epiphyseal ring area | 0.90 | (0.79, 0.95) |
| Concavity (mean depth) | 0.85 | (0.69, 0.93) |
95 % CI 95 % confidence interval, ICC intra-class correlation coefficient
Radiographic and visual assessments
Based on visual assessments, 58.2 % of endplates were evaluated as concave, 33.3 % as flat and the remaining 8.5 % as irregular. The apex of the concavity, if present, was usually located in the posterior portion of the endplate. Overall, 39.8 % of endplates had one concavity apex and 18.5 % had two apexes (Table 2).
Table 2.
Radiographic and visual assessments of the shape of lumbar vertebral endplates
| Cranial endplate (N = 264) | Caudal endplate (N = 336) | Total (N = 600) | |
|---|---|---|---|
| Radiographic assessmenta | |||
| Concave | 199 (75.4 %) | 74 (22.0 %) | 273 (45.5 %) |
| Flat | 50 (18.9 %) | 235 (69.9 %) | 285 (47.5 %) |
| Irregular | 15 (5.7 %) | 27 (8.0 %) | 42 (7.0 %) |
| Visual assessmenta | |||
| Concave | 225 (85.2 %) | 124 (36.9 %) | 349 (58.2 %) |
| Flat | 22 (8.3 %) | 178 (53.0 %) | 200 (33.3 %) |
| Irregular | 17 (6.4 %) | 34 (10.1 %) | 51 (8.5 %) |
| Concavity apex | |||
| No | 39 (14.8 %) | 212 (63.1 %) | 251 (41.8 %) |
| Single | 148 (56.1 %) | 90 (26.8 %) | 238 (39.8 %) |
| Double | 77 (29.2 %) | 34 (10.1 %) | 111 (18.5 %) |
χ2 test was used to compare the cranial and caudal endplates
ap < 0.001, more cranial endplates were concave and more caudal endplates were flat
The radiographic assessments of endplate shape were moderately correlated to the visual measurements (r = 0.53). A substantial percent (29.8 %) of concave endplates, as judged visually, were evaluated as flat in the radiographic assessment. The Cupid’s bow contour was observed in 15.7 % (93) of endplates. The bow contour was more common in cranial endplates (87.4 %), and most of them (93.2 %) were at L3/4, L4/5 and L5/S1 discs. Fifty-three (57.1 %) endplates with the bow contour apparent on radiographs had two para-sagittal apexes in the visual assessment.
Digital measurements
The whole endplate
Overall, the mean size was 35.6 × 51.4 × 1.5 mm (AP diameter × transverse diameter × mean depth) for the cranial endplate and 35.2 × 50.0 × 0.7 mm for the caudal endplate. The average surface area was 15.7 cm2 for the cranial endplate and 15.3 cm2 for the caudal endplate. The measurements for cranial and caudal endplates from different disc levels are presented in Table 3.
Table 3.
Digital geometric measurements of lumbar vertebral endplates
| Disc | Endplate | Endplate | Central endplate | Epiphyseal rim | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | APD | TD | Depth | Area | APD | TD | Area | Anterior width | Lateral width | Posterior width | ||
| T12/L1 | Cranial | NA | NA | NA | ||||||||
| Caudal | 36 | 34.8 ± 3.2 | 45.3 ± 3.7 | 0.3 ± 0.7 | 12.5 ± 2.1 | 23.3 ± 2.5 | 34.7 ± 3.0 | 7.3 ± 1.3 | 4.9 ± 1.5 | 4.9 ± 1.4 | 2.9 ± 1.0 | |
| L1/2 | Cranial | 39 | 35.5 ± 2.9 | 47.6 ± 4.0 | 1.0 ± 0.7 | 14.1 ± 2.2 | 24.1 ± 2.4 | 34.9 ± 2.6 | 7.4 ± 1.0 | 5.7 ± 1.5 | 6.5 ± 1.6 | 2.9 ± 1.0 |
| Caudal | 61 | 35.7 ± 2.3 | 47.0 ± 3.5 | 0.5 ± 0.9 | 14.4 ± 2.1 | 24.6 ± 2.7 | 36.0 ± 2.8 | 7.9 ± 1.3 | 5.2 ± 1.4 | 5.7 ± 1.3 | 3.0 ± 0.9 | |
| L2/3 | Cranial | 61 | 36.2 ± 2.8 | 50.3 ± 3.6 | 1.2 ± 0.6 | 15.4 ± 2.3 | 24.9 ± 2.6 | 34.7 ± 3.4 | 7.5 ± 1.4 | 6.2 ± 1.8 | 8.0 ± 2.1 | 2.8 ± 0.8 |
| Caudal | 19 | 35.7 ± 3.1 | 48.0 ± 3.1 | 0.8 ± 0.9 | 14.9 ± 2.4 | 24.3 ± 2.0 | 35.7 ± 3.2 | 7.8 ± 1.7 | 5.3 ± 1.8 | 6.5 ± 1.6 | 3.5 ± 1.1 | |
| L3/4 | Cranial | 19 | 35.6 ± 2.8 | 51.5 ± 3.4 | 1.5 ± 0.7 | 15.6 ± 2.1 | 24.0 ± 2.8 | 34.2 ± 3.8 | 6.7 ± 1.5 | 6.4 ± 2.1 | 8.7 ± 2.3 | 3.2 ± 1.1 |
| Caudal | 73 | 35.8 ± 2.8 | 51.3 ± 3.7 | 0.7 ± 0.9 | 15.8 ± 2.4 | 25.2 ± 2.6 | 37.5 ± 3.3 | 8.2 ± 1.4 | 5.7 ± 1.8 | 6.9 ± 2.1 | 3.2 ± 0.9 | |
| L4/5 | Cranial | 73 | 36.1 ± 2.8 | 53.6 ± 3.7 | 1.9 ± 0.8 | 16.7 ± 2.4 | 25.6 ± 3.3 | 35.3 ± 4.9 | 7.9 ± 1.9 | 6.2 ± 2.0 | 9.4 ± 2.7 | 3.4 ± 1.2 |
| Caudal | 69 | 35.5 ± 2.9 | 53.0 ± 4.1 | 0.5 ± 0.7 | 16.1 ± 2.5 | 25.2 ± 3.1 | 37.4 ± 3.8 | 8.2 ± 1.8 | 5.4 ± 2.1 | 7.8 ± 2.6 | 3.8 ± 1.3 | |
| L5/S1 | Cranial | 72 | 34.7 ± 3.2 | 52.3 ± 4.7 | 1.5 ± 0.9 | 15.8 ± 3.0 | 23.8 ± 3.7 | 37.7 ± 5.3 | 8.3 ± 2.2 | 5.9 ± 2.1 | 7.7 ± 2.3 | 3.6 ± 1.6 |
| Caudal | 69 | 33.8 ± 3.5 | 51.2 ± 5.3 | 1.0 ± 1.1 | 15.1 ± 2.8 | 24.6 ± 2.9 | 38.0 ± 5.7 | 8.2 ± 1.8 | 4.7 ± 1.9 | 6.8 ± 2.4 | 3.5 ± 1.3 | |
| Overall | Cranial | 264 | 35.6 ± 3.0 | 51.4 ± 4.5 | 1.5 ± 0.8 | 15.7 ± 2.6 | 24.8 ± 3.1 | 35.7 ± 4.5 | 7.8 ± 1.8 | 6.1 ± 1.9 | 8.1 ± 2.5 | 3.2 ± 1.3 |
| Caudal | 327 | 35.2 ± 3.1 | 50.0 ± 4.9 | 0.7 ± 0.9 | 15.3 ± 2.5 | 24.7 ± 2.8 | 36.9 ± 4.0 | 8.0 ± 1.7 | 5.2 ± 1.8 | 6.6 ± 2.3 | 3.3 ± 1.1 | |
| Range | Cranial | 264 | 26–44.2 | 38–69.7 | 0–3.7 | 9.7–27.7 | 16.5–35.5 | 24–53.9 | 3.7–17 | 2.3–13 | 3.4–17.4 | 1.0–9.2 |
| Caudal | 327 | 23–44.9 | 36–69.3 | 0–3.9 | 10.2–23.9 | 17–35.5 | 26–56.0 | 3.8–17.3 | 1.3–16 | 2.3–18.0 | 1.2–7.2 | |
Data were mean ± standard deviation
APD anterior–posterior diameter (mm), TD transverse diameter (mm), depth mean depth of concavity (mm), area surface area (cm2)
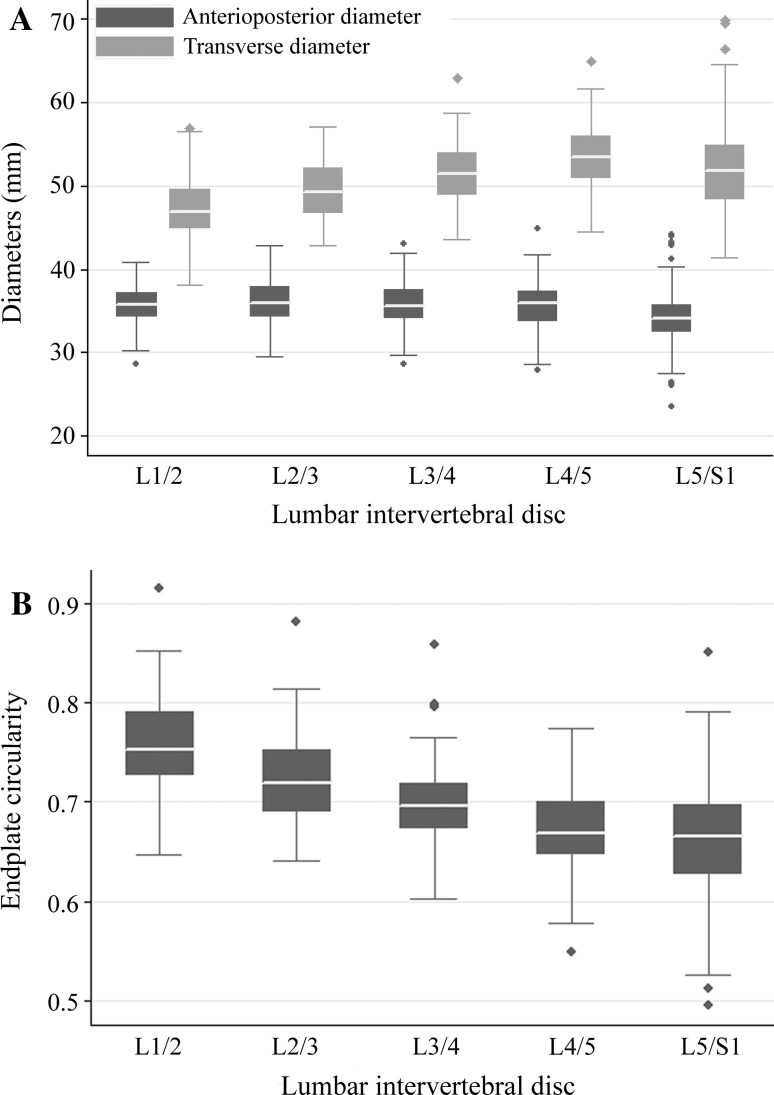
When the cranial and caudal endplates were analyzed together, the AP diameters were relatively constant from L1/2 disc to L4/L5 disc (trend analysis, p > 0.05). However, the transverse diameter increased gradually from L1/2 down to L5/S1 disc (trend analysis, p < 0.001, Fig. 3a). Therefore, the circularity of the endplate decreased gradually from the upper to the lower lumbar disc, such that the endplates became more elliptical (trend analysis, p < 0.001, Fig. 3b).
Fig. 3.
The geometries of the cranial endplate by disc level. a diameters and b circularity
For the cranial endplates, the mean depth of concavity was significantly greater at the lower lumbar discs, compared with those at upper lumbar regions (t test, p < 0.001). For the caudal endplates, there was no statistically significant difference in concavity depths between the upper and lower lumbar regions (t test, p = 0.11). The endplates with Cupid’s bow contour in radiographs had greater mean depth of concavity than those without (t test, p < 0.001). The endplate concavity was independent of age and weight (p > 0.05 for both).
The central endplate and the epiphyseal rim
For the central endplate, the AP diameter was 24.7 ± 2.9 mm and the transverse diameter was 36.3 ± 4.3 mm, which were 70 % and 72 % of the whole endplate diameter, respectively. On average, the central endplate contributed 58 % of the endplate area (Table 3).
The width of the epiphyseal rim varied considerably at different sub-regions. The rim in the lateral region (7.3 ± 0.1 mm, overall measurement) was wider than that in the anterior region (5.6 ± 0.1 mm, Bonferroni test after one-way ANOVA, p < 0.001). The narrowest rim was in the posterior region (3.3 ± 0.1 mm), which was statistically significantly less than that in the anterior region (Bonferroni test after one-way ANOVA, p < 0.001, Table 3).
Difference between cranial and caudal endplates
In both radiographic and visual assessments, more cranial endplates were concave and more caudal endplates were flat (χ2 test, p < 0.001, Table 2). Among these concave endplates, the apex pattern was not significantly different between the cranial and caudal endplates (p = 0.19).
Overall, the endplates cranial to the disc had greater mean depth of concavity than the caudal endplates (t test, p < 0.001). We further compared concavity depth between cranial and caudal endplates adjacent to the same lumbar disc level by level. As data were not normally distributed over subgroups, we used Wilcoxon signed-rank tests, which is an equivalent of a paired t test. For lumbar intervertebral discs from L1/2 to L5/S1, the mean concavity depth of cranial endplate was greater than that of the corresponding caudal endplate (p < 0.05 for all discs, with the exception of L2/3).
Discussion
The morphology and geometry of lumbar vertebral endplates were described in detail using a large cadaveric sample of men with radiographic, visual and digital measures. There was marked morphological asymmetry between the two vertebral endplates adjacent to the same lumbar intervertebral disc: the cranial endplate was more concave than the corresponding caudal endplate. Moreover, the cranial endplates of lower lumbar discs (L4/5, L5/S1) were more concave than those in upper lumbar discs. From L1/2 down to the L5/S1 disc, the vertebral endplate gradually changed into a more oval shape. The central endplate was about 70 % of the diameter of the whole endplate and the width of the epiphyseal rim varied from 3 to 7 mm. Conventional radiography alone was not adequate to evaluate the shape of the vertebral endplate.
Previously, the morphological parameters of vertebral endplates have been described for selected lumbar vertebrae [16, 17] or in relatively small samples of cadavers [18–20] Others measured the shape of the endplate in vivo by sampling one or more sections with CT or MRI [21, 22]. Different from previous morphological studies of the endplate, introducing an accurate laser surface digital technique to measure the endplates allowed not only the quantification of concavity, but also separate measurements of the central endplate and the epiphyseal rim.
In accordance with van der Houwen’s observation [6], our study confirmed a morphological asymmetry between the two vertebral endplates bordering the same lumbar disc. In both radiographic and visual assessments, the endplate cranial to the disc was usually concave and the caudal endplate was flat. Specifically, the mean concavity depth of the cranial endplate was on average 0.8 mm greater than that of the caudal endplate and this asymmetry was consistent at all discs. The mechanism underlying the asymmetry, however, remains unexplained. As the cranial endplate is thicker and has greater bone mineral density than the corresponding caudal endplate [23], mechanical effects alone may not be adequate to explain why the structurally stronger cranial endplate is more concave than the caudal endplate. Moreover, the cranial or caudal endplates from different levels of the same spine were similar to each other, suggesting common determinants of endplate morphology, such as genetics.
Our findings on endplate morphology may have practical implications such as disc arthroplasty. Currently, complications related to fixation of the prosthesis, such as device migration and subsidence, are more commonly reported [24–26]. It is evident that an ideal artificial disc should mirror the shape of both endplates adjacent to a disc in all three dimensions to obtain a maximal contact area of the prosthesis–endplate interface [27]. Therefore, the incorporation of the endplate morphological characteristics, such as the cranial endplate being more concave than its caudal endplate, into the design of disc prostheses may improve prosthesis stability to prevent loosening and migration. On the other hand, it has been realized that undersized prostheses, which lack the support from the stronger peripheral endplate epiphyseal rim, are the main cause of prosthesis subsidence [25–27]. The finding that the diameters of the central endplate were about 70 % of that of the whole endplate may provide a reference for artificial disc sizing to obtain support from the epiphyseal rim of the endplate.
The evaluation of the endplate shape using radiographs was only moderately correlated to the “gold standard” of visual assessments (r = 0.53). Therefore, despite reasonable reliability (Kappa = 0.78), it may not be valid enough to assess the curvature of the endplate. An endplate is typically concave, more or less. The difference lies in the extent, as was confirmed by our digital measurements. Originally, we speculated that the Cupid’s bow contour is the specific radiographic feature of double-apex endplates. However, only approximately half of endplates with Cupid’s bow contour on radiographs were identified as double apexes on visual evaluation. As evaluation of the endplate shape using radiography is limited by its two-dimensional nature, more advanced approaches, such as high resolution 3D reconstructed CT or MR imaging, are needed for a better understanding of endplate contour and its association with clinical outcomes of disc arthroplasty.
One of the study limitations is that all subjects were men. Although the endplate size may be smaller in women than in men, reportedly there is no difference of endplate concavity between men and women [6]. While samples were selected from the spine archive based on the availability of back pain and disc degeneration data, it is not clear whether the selection introduced bias for the endplate measurements. Another concern is that the visual and digital measurements were obtained from dried specimens, which may be different from those acquired from fresh samples or in vivo. In addition, the endplate concavity was indicated by mean depth. Spatial analyses of the endplate surface may better depict endplate morphology. With respect to study strengths, the sample size was large and the digital measurements were precise. Along with the detailed geometrics of the endplate and its components measured, the finding of the asymmetry between the two adjacent endplates of lumbar intervertebral discs may provide a reference for future disc prosthesis design and disc arthroplasty.
Acknowledgments
We thank Darrell Goertzen, Jesse Huard and Kevin Ye for assisting with the acquisition of the quantitative morphometric measurements. Y.W. was supported by Alberta Innovates-Health Solutions (AIHS) and the China Scholarship Council (CSC). M.C.B. was supported by the Canada Research Chairs Program.
Conflict of interest
None.
References
- 1.Taylor JR. Growth of human intervertebral discs and vertebral bodies. J Anat. 1975;120:49–68. [PMC free article] [PubMed] [Google Scholar]
- 2.Moore K, Dalley A. Clinically oriented anatomy. Baltimore: Lippincott Williams and Wilkins; 2006. pp. 478–519. [Google Scholar]
- 3.Moore RJ. The vertebral endplate: disc degeneration, disc regeneration. Eur Spine J. 2006;15:S333–S337. doi: 10.1007/s00586-006-0170-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Eijkelkamp M (2002) Development of an artificial intervertebral disc. PhD thesis, University of Groningen
- 5.Lakshmanan P, Dvorak V, Schratt W, Thambiraj S, Collins I, Boszczyk B. Is there a difference in shape of the endplates in sagittal plane? A morphometric study of the lumbosacral spine (Abstract) Spine J. 2010;10:46s. doi: 10.1016/j.spinee.2010.07.127. [DOI] [Google Scholar]
- 6.Houwen EB, Baron P, Veldhuizen AG, Burgerhof JG, Ooijen PM, Verkerke GJ. Geometry of the intervertebral volume and vertebral endplates of the human spine. Ann Biomed Eng. 2010;38:33–40. doi: 10.1007/s10439-009-9827-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guyer RD, Auer PB, Zigler JE, Blumenthal S, Ohnmeiss DD (2009) P1. Relationship between endplate morphology and clinical outcome of single-level lumbar disc arthroplasty. Spine J 9:114S
- 8.Dar G, Masharawi Y, Peleg S, Steinberg N, May H, Medlej B, et al. The epiphyseal ring: a long forgotten anatomical structure with significant physiological function. Spine (Phila Pa 1976) 2011;36:850–856. doi: 10.1097/BRS.0b013e3181e9b19d. [DOI] [PubMed] [Google Scholar]
- 9.Videman T, Nurminen M, Troup JD. 1990 Volvo Award in clinical sciences. Lumbar spinal pathology in cadaveric material in relation to history of back pain, occupation, and physical loading. Spine. 1990;15:728–740. [PubMed] [Google Scholar]
- 10.Chan KK, Sartoris DJ, Haghighi P, Sledge P, Barrett-Connor E, Trudell DT, et al. Cupid’s bow contour of the vertebral body: evaluation of pathogenesis with bone densitometry and imaging–histopathologic correlation. Radiology. 1997;202:253–256. doi: 10.1148/radiology.202.1.8988219. [DOI] [PubMed] [Google Scholar]
- 11.Keating AP, Knox J, Bibb R, Zhurov AI. A comparison of plaster, digital and reconstructed study model accuracy. J Orthod. 2008;35:191–201. doi: 10.1179/146531207225022626. [DOI] [PubMed] [Google Scholar]
- 12.Spalding SJ, Kwoh CK, Boudreau R, Enama J, Lunich J, Huber D, et al. Three-dimensional and thermal surface imaging produces reliable measures of joint shape and temperature: a potential tool for quantifying arthritis. Arthritis Res Ther. 2008;10:R10. doi: 10.1186/ar2360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Portney LG, Watkins MP (2007) Multiple comparison tests. In: Foundations of clinical research, applications to practice, Pearson Education Inc., New Jersey, pp 479–501
- 14.Sribney B, StataCorp (1996) A comparison of different tests for trend. http://www.stata.com/support/faqs/stat/trendhtml
- 15.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. doi: 10.2307/2529310. [DOI] [PubMed] [Google Scholar]
- 16.Hall LT, Esses SI, Noble PC, Kamaric E. Morphology of the lumbar vertebral endplates. Spine (Phila Pa 1976) 1998;23:1517–1522. doi: 10.1097/00007632-199807150-00002. [DOI] [PubMed] [Google Scholar]
- 17.Langrana NA, Kale SP, Edwards WT, Lee CK, Kopacz KJ. Measurement and analyses of the effects of adjacent end plate curvatures on vertebral stresses. Spine J. 2006;6:267–278. doi: 10.1016/j.spinee.2005.09.008. [DOI] [PubMed] [Google Scholar]
- 18.Aharinejad S, Bertagnoli R, Wicke K, Firbas W, Schneider B. Morphometric analysis of vertebrae and intervertebral discs as a basis of disc replacement. Am J Anat. 1990;189:69–76. doi: 10.1002/aja.1001890109. [DOI] [PubMed] [Google Scholar]
- 19.Berry JL, Moran JM, Berg WS, Steffee AD. A morphometric study of human lumbar and selected thoracic vertebrae. Spine (Phila Pa 1976) 1987;12:362–367. doi: 10.1097/00007632-198705000-00010. [DOI] [PubMed] [Google Scholar]
- 20.Panjabi MM, Goel V, Oxland T, Takata K, Duranceau J, Krag M, et al. Human lumbar vertebrae. Quantitative three-dimensional anatomy. Spine (Phila Pa 1976) 1992;17:299–306. doi: 10.1097/00007632-199203000-00010. [DOI] [PubMed] [Google Scholar]
- 21.Harrington J, Jr, Sungarian A, Rogg J, Makker VJ, Epstein MH. The relation between vertebral endplate shape and lumbar disc herniations. Spine (Phila Pa 1976) 2001;26:2133–2138. doi: 10.1097/00007632-200110010-00018. [DOI] [PubMed] [Google Scholar]
- 22.Pappou IP, Cammisa FP, Jr, Girardi FP. Correlation of end plate shape on MRI and disc degeneration in surgically treated patients with degenerative disc disease and herniated nucleus pulposus. Spine J. 2007;7:32–38. doi: 10.1016/j.spinee.2006.02.029. [DOI] [PubMed] [Google Scholar]
- 23.Wang Y, Battie MC, Boyd SK, Videman T. The osseous endplates in lumbar vertebrae: thickness, bone mineral density and their associations with age and disk degeneration. Bone. 2011;48:804–809. doi: 10.1016/j.bone.2010.12.005. [DOI] [PubMed] [Google Scholar]
- 24.Murtagh RD, Quencer RM, Cohen DS, Yue JJ, Sklar EL. Normal and abnormal imaging findings in lumbar total disk replacement: devices and complications. Radiographics. 2009;29:105–118. doi: 10.1148/rg.291075740. [DOI] [PubMed] [Google Scholar]
- 25.Punt IM, Visser VM, Rhijn LW, Kurtz SM, Antonis J, Schurink GW, et al. Complications and reoperations of the SB Charite lumbar disc prosthesis: experience in 75 patients. Eur Spine J. 2008;17:36–43. doi: 10.1007/s00586-007-0506-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ooij A, Oner FC, Verbout AJ. Complications of artificial disc replacement: a report of 27 patients with the SB Charite disc. J Spinal Disord Tech. 2003;16:369–383. doi: 10.1097/00024720-200308000-00009. [DOI] [PubMed] [Google Scholar]
- 27.Auerbach JD, Ballester CM, Hammond F, Carine ET, Balderston RA, Elliott DM. The effect of implant size and device keel on vertebral compression properties in lumbar total disc replacement. Spine J. 2010;10:333–340. doi: 10.1016/j.spinee.2010.01.008. [DOI] [PubMed] [Google Scholar]