Abstract

Introduction
Injuries of the occipital condyles are rare. While the majority of occipital condyle fractures can be treated conservatively, surgery is recommended in craniocervical misalignment and instability. Open reduction and temporary occipito-cervical stabilization might be an alternative to fusion or halo treatment.
Materials and methods
This Grand Round case presentation describes temporary C0–C3 stabilization in a 29-year-old man who was involved in a car accident. Radiological examination revealed a rotational burst fracture (type AO C3.1) of C7, and a slight displaced right occipital condyle fracture (Anderson/Montesano type III) with rotational misalignment of the C0–C2 complex.
Results
The C7 fracture was stabilized and fused from anterior and posterior. The occipital condyle fracture was reduced and temporarily stabilized from C0–C3 from posterior. Bony healing occurred after 6 months and consequently the internal fixator was removed to preserve upper cervical mobility.
Keywords: Occipital condyle fracture, Occipito-cervical stabilization, Temporary stabilization, Cervical spine
Case presentation
A 29-year-old man was found in the rear passenger compartment of his overturned car after a car accident. The initial Glascow Coma Scale was 13 despite signs of alcohol intoxication. On examination in the Emergency Department, he complained about neck pain and numbness of the right arm. Neurological examination revealed a right C7 radiculopathy with weakness of the elbow extension (grade II).
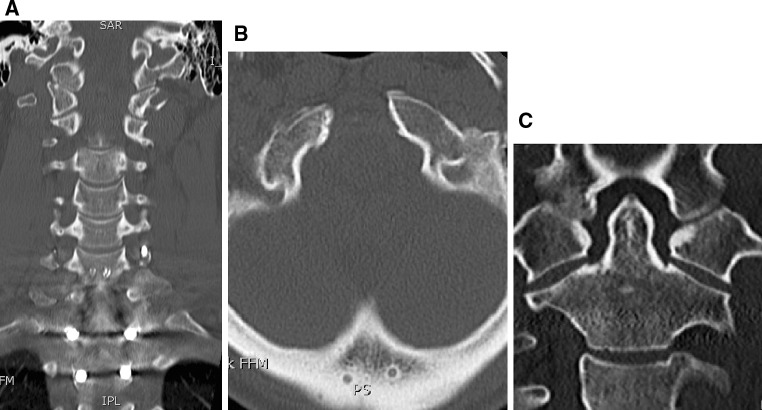
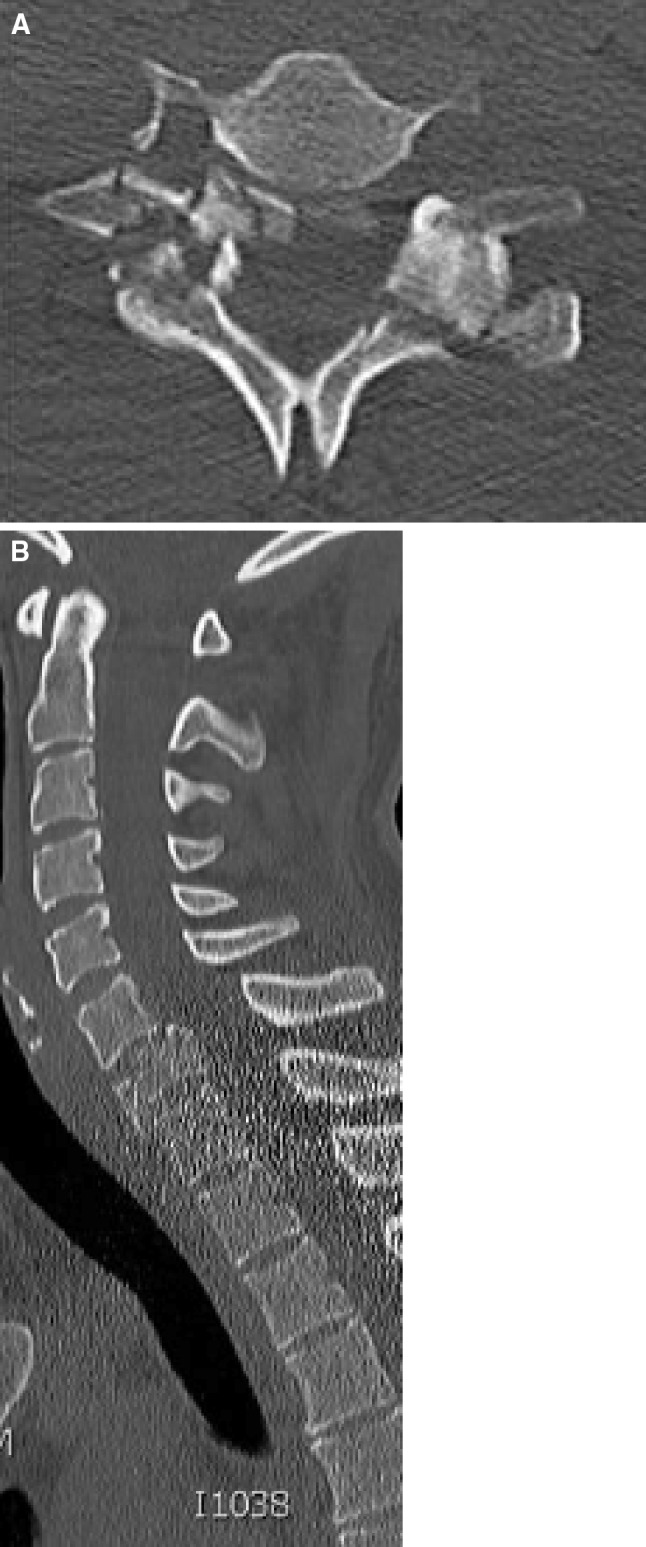
Plain radiographs of the cervical spine (antero-posterior and lateral) as well as a CT scan were performed and revealed a rotational burst fracture of C7 with partial occlusion of the right C7 foramen (Fig. 1). The fracture was classified as C3.1 according to Magerl and Reinhold [1, 2]. Furthermore, a slightly displaced occipital condyle fracture on the right side could be detected (Fig. 2). This fracture was classified as a type III according to Anderson and Montesano [3], and type 2A according to Tuli [4], respectively. In the axial view, a rotational misalignment of 22° to the left of C0/1 against C2 could be observed (Fig. 3).
Fig. 1.
Rotational burst fracture of C7 with right radicular C7 neuropathy due to bony fragment in the C7 foramen
Fig. 2.
Moderate dislocated right occipital condyle fracture
Fig. 3.

Left rotatory subluxation (CO/1–C2) of 22° due to bony avulsion fracture
Because of the neurological deficit, immediate surgery was performed with decompression of the right C7 foramen and posterior stabilization from C5 to Th2 and fusion from C6 to Th1. Postoperatively, patient regained complete neurological function. 4 days later, anterior corpectomy of C7 and fusion from C6 to T1 was performed using a plate-cage construct. After anterior surgery, patient was turned around and posterior reduction and stabilization of the occipital condyle fracture from C0 to C3 was performed.
Operative procedure
Patient was operated in a prone position with the head fixed in a Mayfield clamp. After midline incision and dissection of the neck muscles, bony elements from the occiput to C3 were exposed. Care was taken not to violate the facet joints and bone cortex. The following steps were performed under lateral image intensifier control: drilling and inserting of self-tapping lateral mass screws into C3 and short isthmus screws into C2 (Axon, Synthes, Oberdorf, Switzerland); drilling and inserting of self-tapping screws into the occiput to fixate the occiput rods (OCF, Synthes, Oberdorf, Switzerland). To reduce the rotational misalignment, the head (C0/1) was rotated approximately 20° to the right by adjusting the Mayfield clamp. Furthermore, the C2/3 complex was rotated to the left under visual control until the spine looked straight. The construct was fixed and a cross-link was mounted. Radiological images were taken in antero-posterior and lateral view to confirm anatomical reduction. No bone grafting was performed. No intra or postoperative complication was noted (Fig. 4).
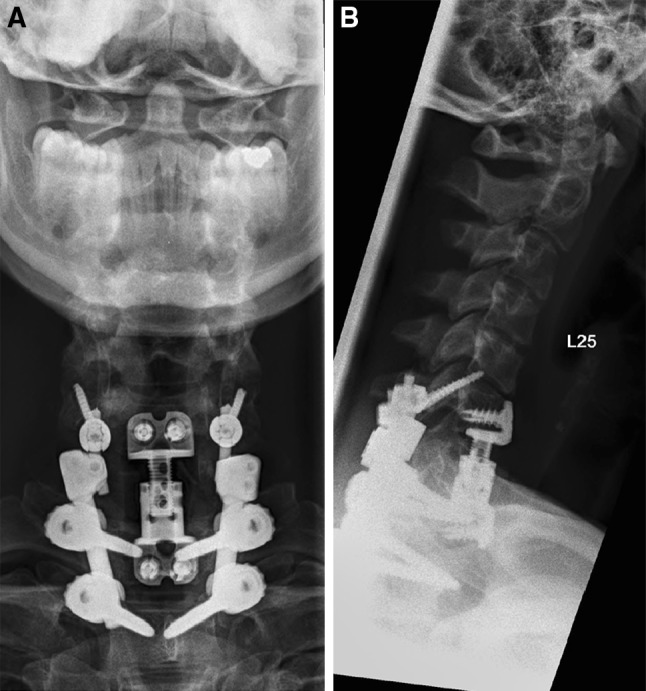
Fig. 4.
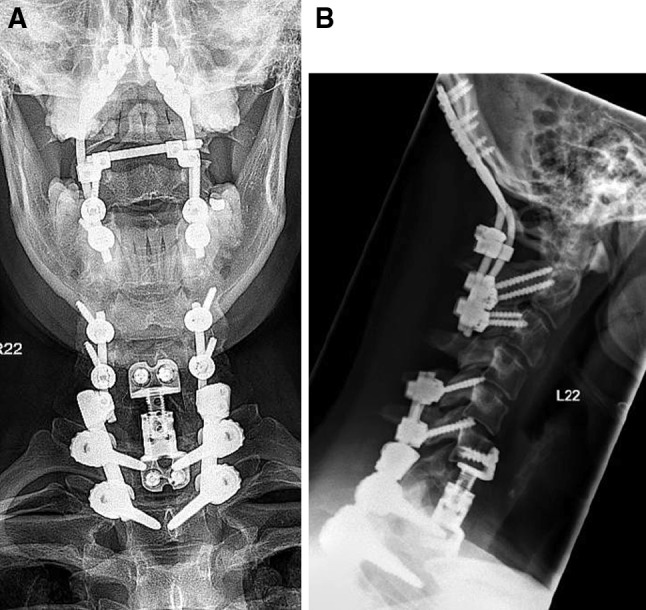
Postoperative X-rays after open, indirect reduction and temporary C0–3 stabilization and decompression and stabilization C5–T2 with fusion C6–T1
Postoperative course
Patient recovered quickly and could be discharged to a rehabilitation clinic. A CT scan showed anatomical reduction with 2° of remaining rotation between C0/1 and C2 (Fig. 5).
Fig. 5.
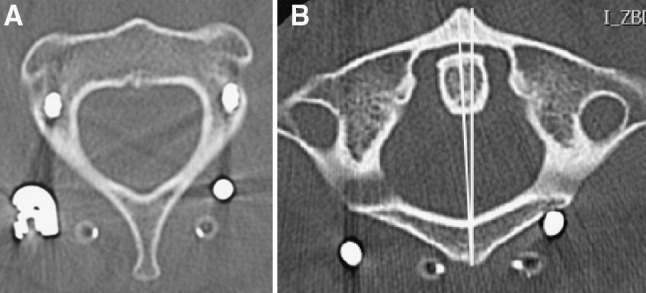
Postoperative CT scan shows residual C0–C2 rotation of 2°
Outcome
The later course was uneventful. 6 months postoperatively, a CT scan showed solid fusion of the fracture (Fig. 6). Hence, implant removal of the C0–C3 construct and of the C5 screws (shortening of the C5–T2 construct) was performed. Intraoperatively, no signs of fusion in the upper cervical spine could be detected and segments were still mobile. In the following months, patient underwent physiotherapy to regain as much as mobility of the cervical spine as possible. At the last follow-up, 12 months after implant removal, the patient was satisfied with the clinical result and did not complain about pain in the upper cervical spine. Due to the fusion from T6 to Th2, the overall cervical range of motion was somewhat restricted. On clinical examination, extension of the neck was still not possible and the cervical spine showed a kyphotic posture. The range of motion of the cervical spine was as follows: extension–flexion 0–0–30°, side-bending right–left 15–0–15°, rotation right–left 45–0–40°. A final CT scan showed stable radiological situation without loss of reduction or signs of pseudarthrosis. However, the cervical spine showed a global kyphotic alignment due to degeneration of the segments C2–C5. Adjacent segment degeneration was obvious at the segment C5/6 (Fig. 7).
Fig. 6.
CT scan before implant removal shows a consolidated fracture and centralized C2
Fig. 7.
X-ray control 12 months after implant removal
Rationale for treatment and review of the literature
Common indications for operative treatment of occipital condyle fractures are [4–11]:
pressure on brain stem and/or vertebral artery,
displacement of fracture with lower cranial nerve palsy,
craniocervical misalignment and instability [condyle-C1 interval >2 mm (Pang rule [12]), disruption of the C0–1 joint, bilateral injury, and additional ligamentous injuries].
Since these conditions are rare, the vast majority of patients receive conservative treatment with collar or halo. Despite the fact that conservative treatment leads to acceptable clinical outcome, the injury typically heals in the non-reduced, sometimes even displaced way [5, 13, 14].
If surgery is necessary, occipito-cervical fusion is recommended [4–11]. To the authors best knowledge, temporary stabilization for treatment of occipital condyle fractures has not been discussed in the literature so far.
The goal of the described operative technique was to reduce the rotational misalignment, to achieve solid healing of the fracture and to avoid external long-term immobilization of the cervical spine.
We are aware that each surgery carries the potential risk of complications and that the posterior approach to the upper cervical spine damages the local muscles. Therefore, muscle sparing techniques should be used and dissection of the muscle insertions at C2 should be avoided.
In order to gain as much stability as possible, we included C3 into the construct. This carries the risk of damaging the C2/3 facet joint. Retrospectively, a C0–C2 construct would have been stable enough and should therefore be recommended. Finally, the duration of the internal fixation might be crucial to achieve a clinical satisfactory result. The earlier the implants can be removed, the higher the possibility to maintain mobility of the joints. Looking from this point, we should have explanted the hardware earlier, probably after 3 months.
Conclusion
Open indirect reduction and temporary occipito-cervical stabilization might be an alternative to conservative treatment in selected cases of displaced occipital condyle fractures.
Conflict of interest
Frank Kandziora is consultant of Synthes GmbH, Switzerland.
References
- 1.Magerl F, Aebi M, Gertzbein SD, Harms J, Nazarian S. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J. 1994;3:184–201. doi: 10.1007/BF02221591. [DOI] [PubMed] [Google Scholar]
- 2.Reinhold M, Blauth M, Rosiek R, Knop C. Lower cervical spine trauma. Classification and operative treatment. Unfallchirurg. 2006;106:471–482. doi: 10.1007/s00113-006-1115-4. [DOI] [PubMed] [Google Scholar]
- 3.Anderson PA, Montesano PX. Morphology and treatment of occipital condyle fractures. Spine (Phila Pa 1976) 1988;13:721–736. doi: 10.1097/00007632-198807000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Tuli S, Tator CH, Fehlings MG, Mackay M. Occipital condyle fractures. Neurosurgery. 1997;41:368–377. doi: 10.1097/00006123-199708000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Mueller FJ, Fuechtmeier B, Kinner B, Rosskopf M, Neumann C, Nerlich M, Englert C. Occipital condyle fractures. Prospective follow-up of 31 cases within 5 years at a level 1 trauma centre. Eur Spine J. 2012;21:289–294. doi: 10.1007/s00586-011-1963-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maserati M, Stephens B, Zohny Z, Lee JY, Kanter AS, Spiro RM, Okonkwo DO. Occipital condyle fractures: clinical decision rule and surgical management. J Neurosurg Spine. 2009;11:388–395. doi: 10.3171/2009.5.SPINE08866. [DOI] [PubMed] [Google Scholar]
- 7.Caroli E, Rocchi G, Orlando ER, Delfini R. Occipital condyle fractures: report of five cases and literature review. Eur Spine J. 2005;14:487–492. doi: 10.1007/s00586-004-0832-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wassenberg J, Bartlett RJ. Occipital condyle fractures diagnosed by high-definition CT and coronal reconstructions. Neuroradiology. 1995;37:370–373. doi: 10.1007/BF00588014. [DOI] [PubMed] [Google Scholar]
- 9.Bozboga M, Unal F, Hepgul K, Izgi N, Turantan MI, Turker K. Fracture of the occipital condyle. Case report. Spine (Phila Pa 1976) 1992;17:1119–1121. doi: 10.1097/00007632-199209000-00019. [DOI] [PubMed] [Google Scholar]
- 10.Vaccaro AR, Lim MR, Lee JY. Indications for surgery and stabilization techniques of the occipito-cervical junction. Injury. 2005;36(Suppl 2):B44–B53. doi: 10.1016/j.injury.2005.06.014. [DOI] [PubMed] [Google Scholar]
- 11.Hanson JA, Deliganis AV, Baxter AB, Cohen WA, Linnau KF, Wilson AJ, Mann FA. Radiologic and clinical spectrum of occipital condyle fractures: retrospective review of 107 consecutive fractures in 95 patients. Am J Roentgenol. 2002;178(5):1261–1268. doi: 10.2214/ajr.178.5.1781261. [DOI] [PubMed] [Google Scholar]
- 12.Pang D, Nemzek WR, Zovickian J. Atlanto-occipital dislocation: part 1—normal occipital condyle-C1 interval in 89 children. Neurosurgery. 2007;61(3):514–521. doi: 10.1227/01.NEU.0000290897.77448.1F. [DOI] [PubMed] [Google Scholar]
- 13.Karam YR, Traynelis VC. Occipital condyle fractures. Neurosurgery. 2010;66:56–59. doi: 10.1227/01.NEU.0000365751.84075.66. [DOI] [PubMed] [Google Scholar]
- 14.Malham GM, Ackland HM, Jones R, Williamson OD, Varma DK. Occipital condyle fractures: incidence and clinical follow-up at a level 1 trauma centre. Emerg Radiol. 2009;16:291–297. doi: 10.1007/s10140-008-0789-z. [DOI] [PubMed] [Google Scholar]