Abstract
Objective
The purpose of this study is to assess the degenerative changes in the motion segments above a L5S1 spondylolytic spondylolisthesis and to view these in light of the retrolisthesis in the segment immediately above the slip.
Background summary
A spondylolytic spondylolisthesis causes an abnormal motion and predisposes to degenerative changes at the L5S1 disc. Degenerative changes in the adjacent segments would influence the symptomatology and natural history of the disease and the treatment options. The extent of degenerative changes in the levels immediately above a L5S1 spondylolytic spondylolisthesis is not well documented in the literature. We have noted retrolisthesis at this level, but this has not been previously reported or assessed.
Materials and methods
Thirty-eight patients with a symptomatic L5S1 spondylolytic spondylolisthesis with a mean age of 52.8 years (95% CI 47.2–58.4); 55.3% (n = 21) females and 44.7% (n = 17) males. We assessed the lumbar lordosis, slip angle, sacral slope, grade of the slip, facet angles at L34 and L45 on both sides, facet degenerative score (cartilage and sclerosis values), disc degenerative score (Pfirrmann) at L34, L45 and L5S1 and the presence of retrolisthesis at L45.
Results
We noted that 29% (11) had a retrolisthesis at L45. The degenerative scores reduced significantly from L5S1 through L45 and L34. Slip angle and L45 disc degenerative score were the only factors that occurred consistently in patients with a retrolisthesis.
Conclusions
There is a cascade of degenerative changes that involve both the disc and the facet joints at the levels above a spondylolytic spondylolisthesis. The degenerative changes at the L45 disc and a higher slip angle are consistent findings in patients with a retrolisthesis at the level above the slip.
Keywords: Spondylolytic spondylolisthesis, Retrolisthesis, Degeneration, Facet, Disc
Introduction
The posterior apophyseal joints play an important stabilising role in the lumbar spine. The load-sharing function between the disc and the paired facet joints is well documented. The extent of this load sharing is affected by factors such as posture, sacral and pelvic morphology, and degeneration. In situations of abnormal loading such as spondylolisthesis, facets are inevitably over-loaded. Although abnormal mobility and abnormal patterns have been reported at the spondylolisthetic segment, little is known about the segments cranial to the slip. Our study sets out to understand the role played by the local anatomic and geometric factors that might influence the natural history of abnormal structural changes in the motion segments cranial to the one with the spondylolytic slip.
Materials and methods
Cohort demographics
The subjects of our current study are 38 patients with spondylolytic spondylolisthesis that were referred to our unit between June 2005 and May 2008. The mean age of this cohort was 52.8 years (95% CI 47.2–58.4) and the sex distribution was 55.3% female (n = 21) and 44.7% male (n = 17). All the patients underwent a plain erect radiographs, AP and lateral of the lumbar spine, and an MRI scan of the lumbar spine as a part of routine assessment. All the patients had a low-grade L5S1 spondylolisthesis: 58% (22 patients), grade 1 slip and 42% (16 patients) a grade 2 slip.
Parameters assessed
Lumbar lordosis: This is measured on the erect lateral radiograph of the lumbo-sacral spine, as the angle between the superior end-plates of L1 and S1.
Sacral slope: This is measured on the erect lateral radiograph of the lumbo-sacral spine. The angle is formed by a horizontal reference line with the upper sacral end plate.
Slip angle: This is measured on the erect lateral radiograph of the lumbo-sacral spine. The angle is measured between the upper S1 endplate with the inferior end plate of the L5 vertebral body.
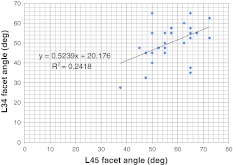
Facet geometry: The facet angle was measured as the angle subtended by a line along the long axis of the facet articulation with the midline [1]. This is measured on a T2-weighted axial scan on the MRI (Fig. 1) at L34 and L45 levels. The right and the left side angles are measured separately. The mean of the two values represents the mean facet angle. The difference of the right from the left side measures the facet tropism for that level. According to the method described by Vanharanta et al. [2] the tropism was mild if the difference was <5°, moderate if the difference was between 7 and 15°, and severe if >15°.
Fig. 1.
Facet angles are measured on both sides. The mean facet angle: (a + b)/2; facet tropism: a − b
Facet degenerative changes: The degree of articular cartilage degeneration and articular process sclerosis was scored by one experienced observer using conventional criteria on T2-weighted axial MRI scans [3]. This was measured at L34 and L45 levels. The cartilage changes within the facet joint were classified into four grades based on the shape and the amount of the articular cartilage covering the joint surface: grade 1 was characterised by a uniformly thick layer of articular cartilage covering both the articular surface completely; grade 2 by cartilage covering the entire sure surface with localised erosions; grade 3 as incomplete covering of the articular surface, with areas of exposed underlying bone and grade 4 by a complete absence of articular cartilage except for some traces. The degree of articular process sclerosis was classified into four grades: grade 1 is a uniform thin band of cortical bone; grade 2 is a thin band of cortical bone with focal thickening; grade 3 represents dense subchondral bone extending over less than half of the articular process; and grade 4 is defined by the presence of osteophytes or dense cortical bone that covers over half of the facet joint.
Disc degeneration (Pfirrmann’s classification): This was graded on T2-weighted mid-sagittal MRI cuts of the lumbar spine at L45 and L5S1 discs. The criteria involved are the disc homogeneity, nucleus-annular transition, signal intensity and the disc height. Five grades of disc degeneration are described: grade 1 is defined by a homogenous bright disc, a clear nuclear-annular transition, a hyperintense signal and a normal disc height; grade 2 as an inhomogenous disc, clear transition, hyper- or isointense signal and a normal height; grade 3 is represented by an inhomogenous grey disc, a loss of the nuclear-annular transition, intermediate intensity and a slight loss of disc height; grade 4 is defined by an inhomogenous grey-black disc, loss of nuclear transition, a hypointense signal and a reduced disc height; and a grade 5 is a black disc with a loss of transition, hypointense signal and a collapsed disc space.
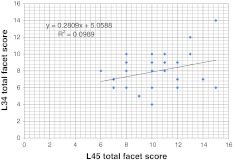
Retrolisthesis: Posterior slippage of one vertebra over the one below it. This was recorded on the lateral radiograph of the lower lumbar spine and was noted for the level above the spondylolisthesis as being present or absent. (Figs. 2, 3).
Fig. 2.
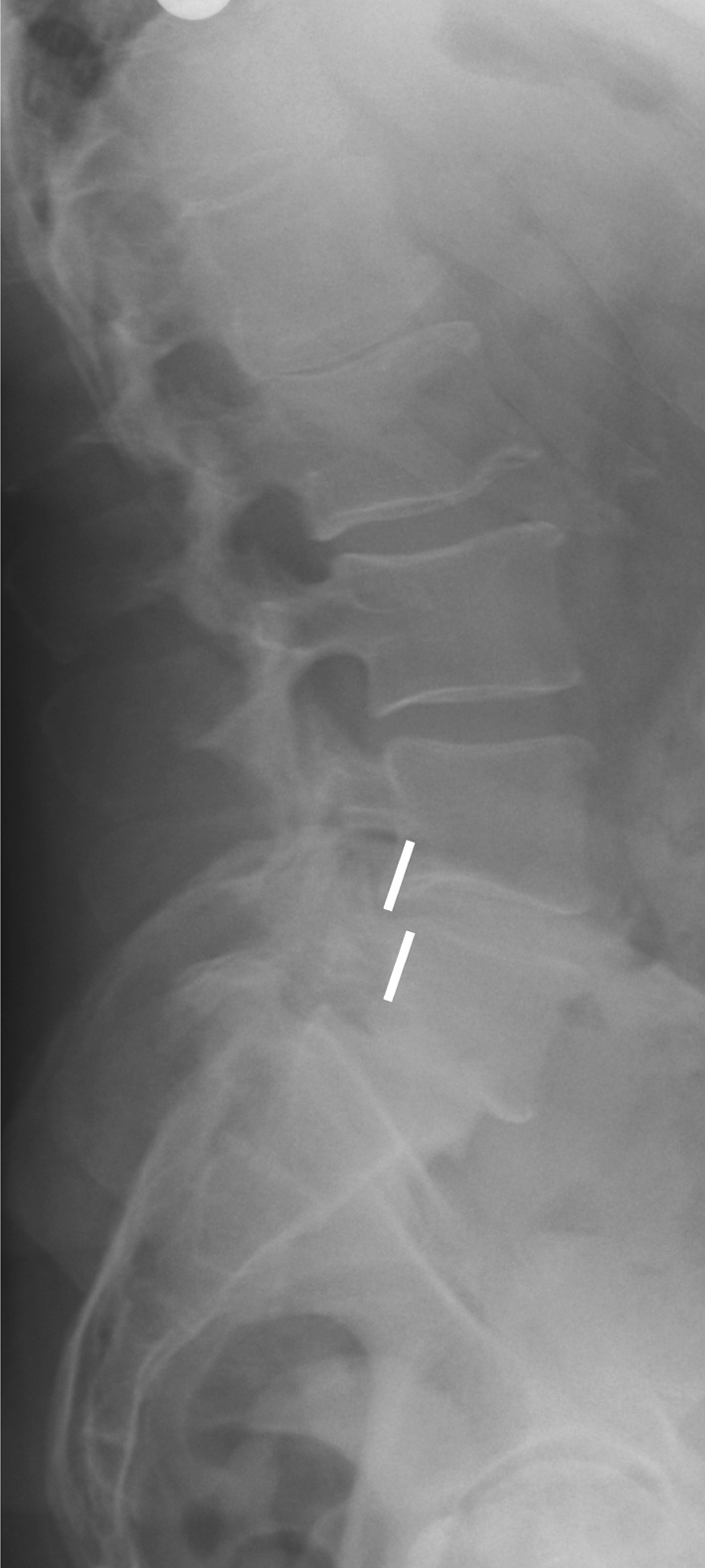
An example of retrolisthesis in a 47/F with a slip angle −16°, sacral slope 45°, lumbar lordosis −58°, L34 facet angle 44° and L45 facet angle 58° The solid white line represents the posterior vertebral border that is disrupted due to the retrolisthesis
Fig. 3.
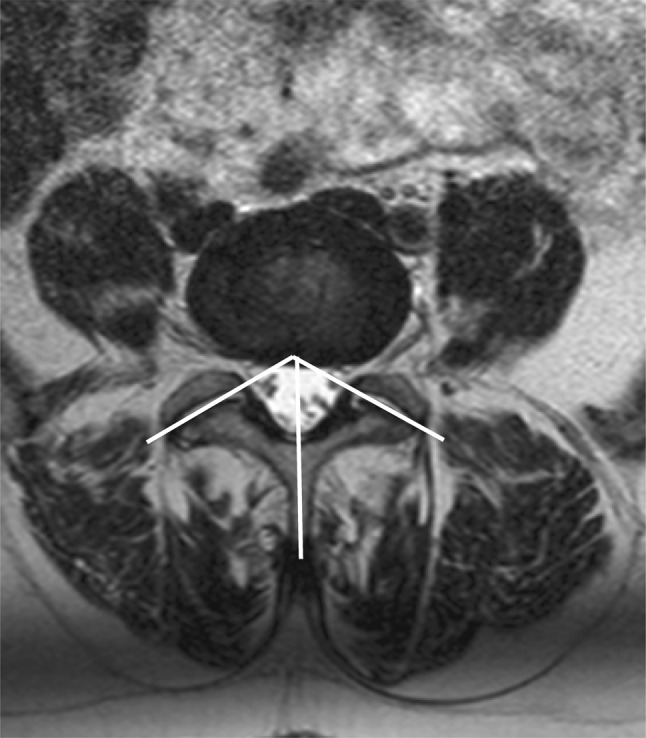
Linear regression of the facet angles at L34 and L45 levels
Statistical methods
The patients were dichotomised based on the presence of the retrolisthesis at the L45 level. The results are expressed by way of the mean ± standard deviations and the 95% confidence intervals for each of the sub-groups. The sub-groups are compared by way of comparing the means using an unpaired t test with a p values significant <0.05.
Results
Sagittal profile
Lumbar lordosis: The lordosis of the lumbar spine was a mean of −61.9° ± 10.4 (95% CI −65.5 to −58.4).
Slip angle: The mean slip angle was −17.4° ± 12.7 (95% CI −21.7 to −13.0).
Sacral slope: The mean sacral slope of the entire cohort was 46.7 ± 8.2° (95% CI 43.9–49.5).
Degenerative cascade (Table 1)
Table 1.
Degenerative cascade in the lower lumbar spine in the entire cohort
| Mean | Sd | p value | |
|---|---|---|---|
| L34 Pfirrmann | 1.88 | 0.94 | 0.0006 |
| L45 Pfirrmann | 2.75 | 1.14 | <0.0001 |
| L5S1 Pfirrmann | 4.44 | 0.62 | |
| L34 facet angle | 50.9 | 8.9 | 0.001 |
| L45 facet angle | 57.9 | 8.3 | |
| L34 facet score | 8 | 2.1 | 0.0001 |
| L45 facet score | 10.5 | 2.4 |
Disc degeneration: The mean Pfirrmann score at L34 was 1.88 ± 0.94, at L45 was 2.75 ± 1.14, while that at L5S1 had a mean of 4.44 ± 0.62. Comparing the L45 and L5S1 segments the changes at L5S1 were higher (p value of <0.0001) and between L34 and L45, the L45 segment was more degenerate (p = 0.0006).
Facet degeneration score: The mean facet score at L34 was 8 ± 2.1 and at L45 was 10.5 ± 2.4. The difference between the two was statistically significant with a value of 0.0001, the degeneration at L45 being higher than at L34.
Facet geometry
Mean facet angle: The mean facet angle at L34 was 50.9° ± 8.9 and L45 was 57.9° ± 8.3. An increase in the facet angle with a sagittal orientation caudally was statistically significant (p = 0.001).
Facet tropism (Table 2): When assessed at the L34 level the tropism was mild in 22, moderate in 14 and severe in two patients. At L45, the tropism was mild in 23, moderate in 13 and severe in two patients.
Table 2.
L34 facet tropism
| L34 | Retro | No retro | |
|---|---|---|---|
| Mild tropism | 8 | 14 | 22 |
| Moderate tropism | 5 | 9 | 14 |
| Severe tropism | 2 | 0 | 2 |
| 38 |
Retrolisthesis
Assessment of the erect lateral radiograph demonstrated 11 patients (29%) with a retrolisthesis at the level above the slip (L45). The remaining 27 patients (71%) had a normal sagittal alignment at this level.
Sagittal profile (Table 3): The lumbar lordosis in the retrolisthesis group was −62.5 ± 10.7° and in the non-retrolisthesis group was −61.7 ± 10.5° (p = 0.847). The sacral slope in the retrolisthesis group was 47 ± 10.7° compared to 46.5 ± 7.02° in the non-retrolisthesis group (p = 0.869). The slip angle in the retrolisthesis group was −9.3 ± 15.8° and in the non-retrolisthesis group was −21.1 ± 9.24° p = 0.009).
Table 3.
Sagittal profile: retro versus no retro
| Retro | No retro | p value | Significance | |||
|---|---|---|---|---|---|---|
| Lumbar lordosis | −62.5 | 10.7 | −61.7 | 10.5 | 0.847 | NS |
| Sacral slope | 47 | 10.7 | 46.5 | 7.02 | 0.869 | NS |
| Slip angle | −9.3 | 15.8 | −21.1 | 9.24 | 0.009 | *** |
*** indicate highly significant
Degenerative facet and disc scores (Table 4): The L34 facet score in the retrolisthesis group was 8.4 ± 2.5, while in the non-retrolisthesis group 7.8 ± 1.9 (p = 0.496). While the L45 facet score in the retrolisthesis group was 11.1 ± 2.8 compared with 10.1 ± 2.2 in the non-retrolisthesis group (p = 0.295). The disc score at L45 was 3.4 ± 1.1 in the retrolisthesis group and 2.4 ± 1.0 in the non-retrolisthesis group (p = 0.024). At the L5S1 level, the disc score was 4.6 ± 0.5 in the retrolisthesis group, and 4.4 ± 0.7 in the non-retrolisthesis group (p = 0.484). Table 5.
Table 4.
Degeneration scores: retro versus no retro
| Retro | No retro | p value | Significance | |||
|---|---|---|---|---|---|---|
| L45 facet degeneration score | 11.1 | 2.8 | 10.1 | 2.2 | 0.295 | NS |
| L34 facet degeneration score | 8.4 | 2.5 | 7.8 | 1.9 | 0.496 | NS |
| L5S1 Pfirrmann disc score | 4.6 | 0.5 | 4.4 | 0.7 | 0.484 | NS |
| L45 Pfirrmann disc score | 3.4 | 1.1 | 2.4 | 1 | 0.024 | ** |
| L34 Pfirrmann disc score | 1.7 | 0.8 | 2.0 | 1.1 | 0.46 | NS |
** indicate significant
Table 5.
L45 facet tropism
| L45 | Retro | No retro | |
|---|---|---|---|
| Mild tropism | 9 | 14 | 23 |
| Moderate tropism | 4 | 9 | 13 |
| Severe tropism | 1 | 1 | 2 |
| 38 |
Facet geometry: 8/22 patients with mild tropism at L34 also had a retrolisthesis, 5/14 had a moderate and the two patients with severe tropism were associated with a retrolisthesis. At the L45 level 9/23 had a mild tropism, 4/13 a moderate tropism and 1/2 a severe tropism.
Discussion
The patterns of degeneration in the lumbar motion segments have been extensively studied [4]. Some studies have demonstrated that the discs degenerate first [5–7]. An increase in the rotational forces leads to an over-loading of the facet joints [8–10]. This leads to a progressive degenerative changes in the facet joint occur with a lag of over two decades following the onset of disc degeneration [5]. Facet joint degeneration is relatively uncommon in persons under 40 years [11] and can steadily progress with the passage of time. By 60 years, moderate facet arthritic changes are usually seen in patients with disc degeneration [5]. The presence of a structural pathology, such as a spondylolytic spondylolisthesis, can provide a trigger for a more accelerated degeneration of the motion segment, particularly the facet joints [12]. However, more recent studies have suggested that factors such as the global spinal sagittal alignment and pelvic parameters account for variations in degenerative patterns, and facet and disc pathology [13].
The facet geometry, i.e. facet joint angulation and facet joint tropism [1, 14–20], may be additional factors that should be considered when assessing the degeneration of the motion segments. A more sagittal angulation of the facet joints allows for abnormal anterior translatory forces [8, 21]. In the presence of an L5S1 spondylolisthesis the effects on L34 and L45 can be conceived to be more profound than in the structurally normal lumbar spine. The mean facet angle in our series at L34 was 50.9° and at L45 57.9° (p = 0.001). These numbers imply higher translational forces at the L45 level than at the cranial levels. The facet angle by itself has little effect on the overall stability and may represent either an anatomic variation [22] or a secondary change based on re-modelling based on the lumbo-sacral pathology.
Facet tropism is considered more important than age, level or the facet angle in causing disc and facet degeneration [15]. Both the cases of severe facet tropism at L34 occured in association with retrolisthesis, while at L45 just one of the two cases of severe tropism occurred in conjunction with a retrolisthesis. We do not feel that could derive any meaningful associations between facet tropism and the presence of a retrolisthesis. However, the sagittal orientation of the facets along with an asymmetry may account for an accelerated degeneration in both the L45 disc and the L45 facet joints.
We noted a linear reduction in the degeneration scores cranially (Fig. 4). The facet degeneration scores reduced significantly from 10.1 at L45 to 8 at L34. The Pfirrmann scores for the disc degeneration reduced cranially from 4.4 at L5S1 to 2.75 at L45 and 1.88 at L34. When comparing these scores between the retrolisthesis group and the non-retrolisthesis group, the only factor that achieved statistical significance was the disc score at L45 (3.4 in the retrolisthesis group and 2.4 in the non-retrolisthesis group).
Fig. 4.
Linear regression of the facet degenerative scores at L34 and L45 levels
The sagittal profile assessments revealed that the lumbar lordosis of the cohort was in the high normal range, with a similar distribution between the retro and the non-retro groups. A similar pattern was seen with the sacral slope. Though the mean slip angle of the entire cohort was −17.4, there was a wide difference between the slip angles in the retrolisthesis and the non-retrolisthesis groups. The retrolisthesis group had a much lower slip angle (−9.3°) than the non-retrolisthesis group (−21.1°). The relative kyphotic disposition of the lumbo-sacral segment could be the trigger for a local compensatory mechanism i.e. a retrolisthesis at L45. Since the lordosis is similar in the two groups it is likely that the retrolisthesis is not global attempt at compensation at the L45, to shift the plumb-line further back due to the ‘kyphotic’ lumbo-sacral junction, but rather a local effort that is caused by the degenerate L45 disc with the facet geometry variation being an additional factor. Although other global factors such as pelvic incidence could contribute towards the overall lumbar lordosis, we have restricted our assessments in this study to local factors to maintain clarity. We feel that the retrolisthesis is a local effect produced by the degenerative changes and a higher slip angle.
Our findings support the hypothesis that the lumbar discs degenerate earlier than the facets in the same time frame, and that the degenerative changes representing a progressive transition with decreasing severity cranial-wards. Further, we have found that the degenerative scores at L45 disc and a low slip angle are the local factors that trigger a compensatory retrolisthesis at L45, the level above a low grade spondylolytic spondylolisthesis.
Conclusions
There is a cascade of degenerative change involving both the disc and the facet joints at the levels above a spondylolytic spondylolisthesis. The degenerative changes at the L45 disc and a higher slip angle predict a retrolisthesis at L45, the level above the slip.
Conflict of interest
None.
References
- 1.Noren R, Trafimow J, Andersson GB, Huckman MS. The role of facet joint tropism and facet angle in disc degeneration. Spine. 1991;16:530–532. doi: 10.1097/00007632-199105000-00008. [DOI] [PubMed] [Google Scholar]
- 2.Vanharanta H, Floyd T, Ohnmeiss DD, Hochschuler SH, Guyer RD. The relationship of facet tropism to degenerative disc disease. Spine. 1993;18:1000–1005. doi: 10.1097/00007632-199306150-00008. [DOI] [PubMed] [Google Scholar]
- 3.Pfirrmann CWMA, Zanettim, Hodler J, Boos N, et al. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine. 2001;26:1873–1878. doi: 10.1097/00007632-200109010-00011. [DOI] [PubMed] [Google Scholar]
- 4.Andersson GB. What are the age-related changes in the spine? Baillieres Clin Rheumatol. 1998;12:161–173. doi: 10.1016/S0950-3579(98)80010-1. [DOI] [PubMed] [Google Scholar]
- 5.Fujiwara A, Tamai K, Yamato M, An HS, Yoshida H, Saotome K, Kurihashi A. The relationship between facet joint osteoarthritis and disc degeneration of the lumbar spine: an MRI study. Eur Spine J. 1999;8:396–401. doi: 10.1007/s005860050193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Butler D, Trafimow JH, Andersson GB, McNeill TW, Huckman MS. Discs degenerate before facets. Spine. 1990;15:111–113. doi: 10.1097/00007632-199002000-00012. [DOI] [PubMed] [Google Scholar]
- 7.Eubanks JD, Lee MJ, Cassinelli E, Ahn NU. Does lumbar facet arthrosis precede disc degeneration? A postmortem study. Clin Orthop Relat Res. 2007;464:184–189. doi: 10.1097/BLO.0b013e3181583d4e. [DOI] [PubMed] [Google Scholar]
- 8.Fujiwara A, Tamai K, An HS, Kurihashi T, Lim TH, Yoshida H, Saotome K. The relationship between disc degeneration, facet joint osteoarthritis, and stability of the degenerative lumbar spine. J Spinal Disord. 2000;13:444–450. doi: 10.1097/00002517-200010000-00013. [DOI] [PubMed] [Google Scholar]
- 9.Fujiwara A, Lim TH, An HS, Tanaka N, Jeon CH, Andersson GB, Haughton VM. The effect of disc degeneration and facet joint osteoarthritis on the segmental flexibility of the lumbar spine. Spine. 2000;25:3036–3044. doi: 10.1097/00007632-200012010-00011. [DOI] [PubMed] [Google Scholar]
- 10.Haher TR, O’Brien M, Dryer JW, Nucci R, Zipnick R, Leone DJ. The role of the lumbar facet joints in spinal stability. Identification of alternative paths of loading. Spine. 1994;19:2667–2670. [PubMed] [Google Scholar]
- 11.Gries NCBU, Moore RJ, Vernon-Roberts B. Early histologic changes in lower lumbar discs and facet joints and their correlation. Eur Spine J. 2000;9:23–29. doi: 10.1007/s005860050004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Don AS, Robertson PA. Facet joint orientation in spondylolysis and isthmic spondylolisthesis. J Spinal Disord Tech. 2008;21:112–115. doi: 10.1097/BSD.0b013e3180600902. [DOI] [PubMed] [Google Scholar]
- 13.Roussouly PGS, Berthonnaud E, Dimnet J. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine. 2005;30:346–353. doi: 10.1097/01.brs.0000152379.54463.65. [DOI] [PubMed] [Google Scholar]
- 14.Wang J, Yang X. Age related changes in the orientation of lumbar facet joints. Spine. 2009;34:E596–E598. doi: 10.1097/BRS.0b013e3181abbf1e. [DOI] [PubMed] [Google Scholar]
- 15.Grogan J, Nowicki BH, Schmidt TA, Haughton VM. Lumbar facet joint tropism does not accelerate degeneration of the facet joints. AJNR Am J Neuroradiol. 1997;18:1325–1329. [PMC free article] [PubMed] [Google Scholar]
- 16.Murtagh FR, Paulsen RD, Rechtine GR. The role and incidence of facet tropism in lumbar spine degenerative disc disease. J Spinal Disord. 1991;4:86–89. [PubMed] [Google Scholar]
- 17.Cyron BM, Hutton WC. Articular tropism and stability of the lumbar spine. Spine. 1980;5:168–172. doi: 10.1097/00007632-198003000-00011. [DOI] [PubMed] [Google Scholar]
- 18.Kong MH, He W, Tsai YD, Chen NF, Keorochana G, Do DH, Wang JC. Relationship of facet tropism with degeneration and stability of functional spinal unit. Yonsei Med J. 2009;50:624–629. doi: 10.3349/ymj.2009.50.5.624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Van Schiak JP, Verbiest H, Van Schiak FD. The orientation of laminae and facet joints in the lower lumbar spine. Spine. 1985;10:59–63. doi: 10.1097/00007632-198501000-00009. [DOI] [PubMed] [Google Scholar]
- 20.Wang Z, Yu S, Haughton VM. Age-related changes in the lumbar facet joints. Clin Anat. 1989;2:55–62. doi: 10.1002/ca.980020202. [DOI] [Google Scholar]
- 21.Berlemann U, Jeszenszky DJ, Buhler DW, Harms J. The role of lumbar lordosis, vertebral end-plate inclination, disc height, and facet orientation in degenerative spondylolisthesis. J Spinal Disord. 1999;12:68–73. doi: 10.1097/00002517-199902000-00011. [DOI] [PubMed] [Google Scholar]
- 22.Boden SD, Riew KD, Yamaguchi K, Branch TP, Schellinger D, Wiesel SW. Orientation of the lumbar facet joints: association with degenerative disc disease. J Bone Joint Surg Am. 1996;78:403–411. doi: 10.2106/00004623-199603000-00012. [DOI] [PubMed] [Google Scholar]