Abstract
Introduction
To date, few studies have focused on spinopelvic sagittal alignment as a predisposing factor for the development of degenerative spondylolisthesis (DS). The objectives of this study were to compare differences in spinopelvic sagittal alignment between patients with or without DS and to elucidate factors related to spinopelvic sagittal alignment.
Materials and methods
A total of 100 patients with or without DS who underwent surgery for lumbar spinal canal stenosis were assessed in this study. Fifty patients with DS (DS group) and 50 age- and gender-matched patients without DS (non-DS group) were enrolled. Spinopelvic parameters including pelvic incidence (PI), sacral slope (SS), pelvic tilt (PT), L4 slope, L5 slope, thoracic kyphosis (TK), lumbar lordosis (LL) and sagittal balance were compared between the two groups. In the DS group, the percentage of vertebral slip (% slip) was also measured.
Results
Several spinopelvic parameters, PI, SS, L4 slope, L5 slope, TK and LL, in the DS group were significantly greater than those in the non-DS group, and PI had positive correlation with % slip (r = 0.35, p < 0.05). Degrees of correlations among spinopelvic parameters differed between the two groups. In the DS group, PI was more strongly correlated with SS (r = 0.82, p < 0.001) than with PT (r = 0.41, p < 0.01). In the non-DS group, PI was more strongly correlated with PT (r = 0.73, p < 0.001) than with SS (r = 0.38, p < 0.01).
Conclusions
Greater PI may lead to the development and the progression of vertebral slip. Different compensatory mechanisms may contribute to the maintenance of spinopelvic sagittal alignment in DS and non-DS patients.
Keywords: Spinopelvic sagittal alignment, Pelvic incidence, Lumbar spinal canal stenosis, Degenerative spondylolisthesis, Percentage of vertebral slip
Introduction
The whole spinal sagittal alignment is affected by various factors including aging, posture, disorders of the spine and those of the pelvis and lower extremities. In recent years, evaluations of spinal sagittal alignment are becoming increasingly important for investigating pathomechanisms and treating degenerative spinal diseases. To date, several studies regarding spinal sagittal alignment in normal populations and patients with low back pain have been reported [8, 11, 23]. Sacral slope and sacral inclination were evaluated in some studies; these parameters are greatly influenced by the position of the pelvis and may not be precise indicators of the spinopelvic alignment [8, 23]. Duval-Beaupère et al. [6] described an index, naming pelvic incidence (PI) as an invariable morphologic angle, which is not affected by aging, posture or tilting of the pelvis. PI would be a useful tool for investigating the pathomechanisms of spinal diseases. Mac-Thiong et al. [15] reported a study that used PI to compare the spinopelvic sagittal alignment in children and adolescents with developmental lumbosacral spondylolisthesis and asymptomatic subjects. PI is also a predicting factor for spinal correction surgeries using osteotomies. Rose et al. [17] demonstrated that PI and thoracic kyphosis can predict lumbar lordosis required for obtaining correct sagittal balance in patients undergoing pedicle subtraction osteotomy.
Several factors influencing the pathologies and the development of degenerative spondylolisthesis (DS) have been reported. Imada et al. [10] reported that an oophorectomy was a predisposing factor for the development of DS among women. Sanderson et al. [20] and Matsunaga et al. [16], respectively, reported that pregnancy and joint laxity were contributing factors to DS. Sato et al. [21] demonstrated that the configuration of the laminas and sagittal facet joints were predisposing factors for DS. Despite these studies, few studies have focused on the spinopelvic sagittal alignment, especially PI, as a factor that would be related to DS. To the best of our knowledge, the relationship between PI and DS has not yet been evaluated in detail, with adjustments for confounding factors such as age and gender.
The objectives of the present study were to use PI to clarify the difference in spinopelvic sagittal alignment between patients with or without DS who underwent surgery for lumbar spinal canal stenosis, and to elucidate factors related to spinopelvic sagittal alignment.
Materials and methods
The approval of the institutional review boards of the participating institutions was obtained prior to the present study. A total of 268 patients with lumbar spinal canal stenosis, 89 patients with DS and 179 patients without DS, underwent surgery at our hospital between 2003 and 2006. DS was defined as an anterior slip of the L4 vertebra of 5 % or more. Patients with other spinal diseases such as trauma, tumor, scoliosis, isthmic lysis with or without spondylolisthesis, severe osteoarthritis in the lower limbs and a history of spine surgery were excluded from the study. To compare the characteristics between patients with DS (DS group) and those without DS (non-DS group) or to investigate differences in spinopelvic sagittal alignment according to gender, one of the authors who was not involved in the radiograph measurements randomly selected the medical charts of 50 patients (male 25, female 25) in the DS group and 50 patients (male 25, female 25) in the non-DS group. The average age was 66.1 ± 9.5 years in the DS group and 69.7 ± 7.8 years in the non-DS group.
Before surgery, standing lateral radiographs of the whole spine were taken with the arms in the fists-on-clavicles position, elbows fully flexed with fists resting on the clavicles, and knees and hips fully extended [7]. All the radiographs were taken using vertical 35.4 × 83.7 cm film and a digital radiography system (Fuji IP Longview cassette, Fuji Photo Film, Co., Japan). The patients for whom lateral radiographs were unavailable, such as those with a low visibility of bilateral femoral heads, were excluded.
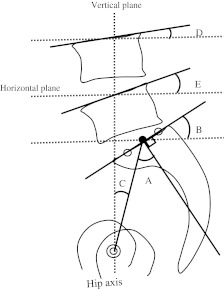
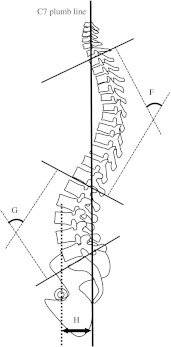
The spinopelvic parameters, including PI, sacral slope (SS) and pelvic tilt (PT), were measured as reported by Duval et al. [6]. Briefly, PI was regarded as the angle between the line connecting the hip axis (HA) and the midpoint of the superior endplate of S1 and the line perpendicular to it. SS was regarded as the angle between the superior endplate of S1 and the horizontal plane. PT was regarded as the angle between the line connecting the midpoint of the superior endplate of S1 and the HA, and the vertical plane. L4 slope was regarded as the angle between the superior endplate of L4 and the horizontal plane. L5 slope was regarded as the angle between the superior endplate of L5 and the horizontal plane (Fig. 1). The spinal parameters were investigated as follows, according to Jackson’s procedure [11]. The angle of thoracic kyphosis (TK) was measured from the superior endplate of T1 to the inferior endplate of T12, and that of lumbar lordosis (LL) was measured from the inferior endplate of T12 to the superior endplate of S1 using the Cobb’s method. To evaluate global balance, the horizontal distance between HA and the C7 plumbline (HAC7PL) was also measured (Fig. 2).
Fig. 1.
Spinopelvic parameters. Standing lateral radiographs of the whole spine were taken in the fists-on-clavicles position. The pelvic parameters were measured as follows. Pelvic incidence (PI) was regarded as the angle between the line connecting the hip axis (HA) and the midpoint of the superior endplate of S1, and the line perpendicular to it (A). Sacral slope (SS) was regarded as the angle between the superior endplate of S1 and the horizontal plane (B). Pelvic tilt (PT) was regarded as the angle between the line connecting the midpoint of the superior endplate of S1 and the HA, and the vertical plane (C). L4 slope was regarded as the angle between the superior endplate of L4 and the horizontal plane (D). L5 slope was regarded as the angle between the superior endplate of L5 and the horizontal plane (E)
Fig. 2.
Spinopelvic parameters The spinal parameters were measured as follows. The angle of thoracic kyphosis (TK) was measured from the superior endplate of T1 to the inferior endplate of T12 (F). The angle of lumbar lordosis (LL) was measured from the inferior endplate of T12 to the superior endplate of S1 (G). The horizontal distance between HA and the C7 plumbline (HAC7PL) was also measured (H)
Spinopelvic sagittal alignments in both groups were classified into four types defined by Roussouly et al. [19]. Type 1 was defined as SS less than 35°, usually associated with a low PI. The apex of the lumbar lordosis was located at the center of the L5 vertebral body. Type 2 was defined as SS less than 35°. The apex of the lumbar lordosis was located at the base of the L4 vertebral body. Type 3 was defined as SS between 35° and 45°. The apex of lumbar lordosis was at the center of the L4 vertebral body. Type 4 was defined as SS greater than 45°, associated with a high PI. The apex of lumbar lordosis was located at the base of L3 vertebral body or higher.
Additionally, in the DS group, % slip was measured according to Taillard’s method.
All data were expressed as the mean ± standard deviation. Student’s t-test was used to compare each parameter between the DS and non-DS group. Correlations among the spinopelvic parameters and between PI and % slip were determined using Pearson correlation coefficient and the differences in the coefficients between the two groups were tested using rank test. A p value less than 0.05 was considered to be statistically significant.
Results
Table 1a shows the differences in the spinopelvic parameters between the DS and non-DS groups. In the DS group, PI, SS, L4 slope, L5 slope, TK and LL were significantly greater than those in the non-DS group. In contrast, PT and HAC7PL were not different between the two groups. The spinopelvic parameters stratified according to gender were also compared between the two groups (Table 1b, c). In the DS group, PI, SS, L4 slope, L5 slope, TK and LL were also significantly greater than those in the non-DS group, both in males and females. The mean L5 slope was 17.8 ± 7.3°, and the mean L4 slope was 7.8 ± 5.5° in the DS group. The mean L5 slope was 9.4 ± 5.6° and the mean L4 slope was 2.7 ± 5.3° in the non-DS group. L5 slope was significantly larger than L4 slope in both DS and non-DS groups (p < 0.001).
Table 1.
Comparison of the spinopelvic parameters
| DS total (n = 50) | Non-DS total (n = 50) | p value | |
|---|---|---|---|
| (a) Comparison of the spinopelvic parameters between the DS and non-DS group in all the subjects | |||
| PI | 57.5 ± 10.7° | 48.8 ± 9.7° | <0.001 |
| SS | 34.0 ± 9.9° | 26.6 ± 7.0° | <0.001 |
| PT | 23.5 ± 6.2° | 22.2 ± 9.5° | 0.427 |
| TK | 37.2 ± 11.2° | 30.5 ± 9.7° | 0.002 |
| LL | 47.4 ± 16.5° | 35.5 ± 8.9° | <0.001 |
| HAC7PL | 15.3 ± 32.9 mm | 15.3 ± 29.2 mm | 0.995 |
| L5 slope | 17.8 ± 7.3° | 9.4 ± 5.6° | <0.001 |
| L4 slope | 7.8 ± 5.5° | 2.7 ± 5.3° | <0.001 |
| DS male (n = 25) | Non-DS male (n = 25) | p value | |
|---|---|---|---|
| (b) Comparison of the spinopelvic parameters between the DS and non-DS group in males | |||
| PI | 57.8 ± 11.7° | 48.0 ± 8.6° | 0.002 |
| SS | 34.9 ± 9.8° | 28.6 ± 7.6° | 0.015 |
| PT | 22.9 ± 6.5° | 19.4 ± 8.2° | 0.1 |
| TK | 38.7 ± 8.9° | 32.6 ± 9.3° | 0.022 |
| LL | 48.1 ± 15.6° | 38.0 ± 8.2° | 0.006 |
| HAC7PL | 11.0 ± 29.6 mm | 9.7 ± 26.9 mm | 0.866 |
| L5 slope | 17.8 ± 7.3° | 9.4 ± 5.6° | <0.001 |
| L4 slope | 7.6 ± 6.0° | 2.4 ± 4.9° | 0.002 |
| DS female (n = 25) | Non-DS female (n = 25) | p value | |
|---|---|---|---|
| (c) Comparison of the spinopelvic parameters between the DS and non-DS group in females | |||
| PI | 57.2 ± 9.8° | 49.5 ± 10.7° | 0.011 |
| SS | 33.1 ± 10.0° | 24.5 ± 5.7° | 0.001 |
| PT | 24.0 ± 6.0° | 25.0 ± 10.0° | 0.683 |
| TK | 35.6 ± 13.2° | 28.3 ± 9.9° | 0.03 |
| LL | 46.7 ± 17.6° | 33.0 ± 9.1° | 0.001 |
| HAC7PL | 19.5 ± 36.0 mm | 21.0 ± 30.8 mm | 0.88 |
| L5 slope | 18.7 ± 8.3° | 9.2 ± 5.6° | <0.001 |
| L4 slope | 8.0 ± 5.0° | 3.0 ± 5.7° | 0.002 |
mean ± standard deviation
Significant positive correlations were also observed between several spinopelvic parameters in both groups (Table 2). However, the degrees of correlations among the spinopelvic parameters differed between DS and non-DS groups. In the DS group, PI was more strongly correlated with SS (r = 0.82, p < 0.001) and LL (r = 0.58, p < 0.001) than with PT (r = 0.41, p < 0.01). In contrast, in the non-DS group, PI was more strongly correlated with PT (r = 0.73, p < 0.001) than with SS (r = 0.38, p < 0.01).
Table 2.
Correlation coefficients among the spinopelvic parameters in the DS and non-DS group
| DS (n = 50) | p value | Non-DS (n = 50) | p value | |
|---|---|---|---|---|
| PI-SS | 0.82 | <0.001 | 0.38 | 0.006 |
| PI-PT | 0.41 | 0.003 | 0.73 | <0.001 |
| PI-TK | 0.22 | 0.129 | −0.14 | 0.344 |
| PI-LL | 0.58 | <0.001 | 0.29 | 0.039 |
| PI-HAC7PL | −0.03 | 0.827 | 0.12 | 0.389 |
| SS-PT | −0.18 | 0.208 | −0.35 | 0.014 |
| SS-TK | 0.25 | 0.084 | 0.21 | 0.138 |
| SS-LL | 0.84 | <0.001 | 0.76 | <0.001 |
| SS-HAC7PL | 0.14 | 0.319 | −0.18 | 0.219 |
| PT-TK | −0.02 | 0.895 | −0.3 | 0.037 |
| PT-LL | −0.34 | 0.017 | −0.26 | 0.071 |
| PT-HAC7PL | −0.28 | 0.046 | 0.26 | 0.072 |
| TK-LL | 0.53 | <0.001 | 0.6 | <0.001 |
| TK-HAC7PL | 0.09 | 0.554 | −0.08 | 0.595 |
| LL-HAC7PL | 0.43 | 0.002 | 0.08 | 0.588 |
The Roussouly types of spinopelvic saggital alignments in the DS male group were Type1, 0; Type2, 10; Type3, 10; Type4, 5 patients. Those in the DS female group were Type1, 0; Type2, 14; Type3, 4; Type4, 7 patients. Those in the non-DS male group were Type1, 10; Type2, 12; Type3, 3; Type4, 0 patients. Those in the non-DS female group were Type1, 9; Type2, 15; Type3, 1; Type4, 0 patients.
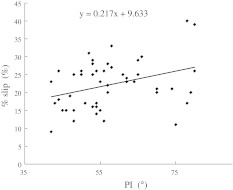
The mean % slip was 22.16 ± 6.73 % (9–40 %) in the DS group. Interestingly, PI had a weak but positive correlation with % slip (r = 0.35, p < 0.05) (Fig. 3).
Fig. 3.
Correlation coefficients between PI and % slip. The mean % slip in the DS group was 22.16 ± 6.73 % (9–40 %). PI had a weak but positive correlation with % slip in the DS group (r = 0.35, p < 0.05)
Discussion
PI is an invariable morphologic parameter in an individual person [6]. It is well established that PI determines the pelvic shape and is strongly correlated with SS and PT in normal and scoliotic adult subjects as demonstrated by Legaye et al. [14]. These authors also reported that SS was closely correlated with spinal parameter, especially LL, suggesting that the pelvic shape has a great impact on thoracolumbar spinal curvatures. Our results also demonstrated that spinopelvic parameters, including PI, SS, PT, LL and TK, had significant positive correlation with each other.
Several factors have been reported to affect the etiology and development of DS, such as gender [16, 18], hormones [10, 18], pregnancy [20], ligamentous hyperlaxity [16], facet tropism, orientation of the lumber facet joints [4, 5, 9] and configuration of the lamina [21]. Although many studies have suggested the predisposing factors for the development of DS, few studies have been reported regarding the influence of spinopelvic sagittal alignment, especially PI, on the development of DS. Legaye et al. [14] reported that a large PI indicated a steep SS and large sagittal curves. Barrey et al. reported that patients with DS demonstrated significantly greater PI (60°) than the normal population (52°) and they also suggested that the shape of the pelvis was the major predisposing factor for DS [2, 3]. Schuller et al. [22] also reported a significant increase in PI (66.2° vs. 54.2°) and SS (42.3° vs. 33.4°) in the DS group than in the reference group (low back pain due to moderate degenerative disc disease). They suggested the anatomic orientation of the pelvis with a high PI and SS seems to represent a predisposing factor for DS. In the present study, we also demonstrated that PI (57.5° vs. 48.8°) and SS (34.0° vs. 26.6°) in DS patients were significantly larger than in non-DS patients.
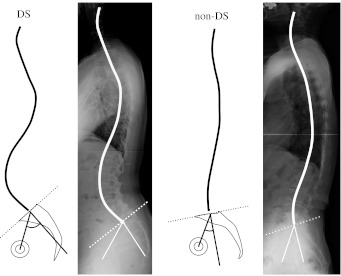
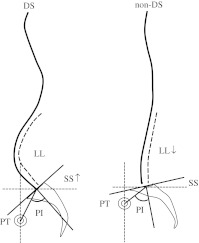
DS is approximately four times or more common in women [16, 18]. However, our analyses of the spinopelvic sagittal alignment, stratified according to gender in the present sex-matched study, demonstrated that PI in the DS group were significantly greater than those in the non-DS group both in males and females. Therefore, large PI in conjunction with steep SS might be a common predisposing factor for DS in both genders. To compensate for the increase in SS and to maintain global balance, lumbar lordosis and thoracic kyphosis would be maintained, thereby showing characteristic spinopelvic alignments with greater spinal curvatures in the DS group (Fig. 4).
Fig. 4.
Typical spinopelvic sagittal alignments in the non-DS and DS patients. Greater PI may lead to an increase in SS. In order to compensate for the increase in SS and to maintain the global balance, lumbar lordosis and thoracic kyphosis may increase, thereby showing characteristic spinopelvic alignments with greater spinal curvatures in DS patients compared with non-DS patients
Roussouly et al. [19] classified four types of spinopelvic sagittal alignment using lateral radiographs in 160 normal volunteers. They had noted that patients with symptomatic disc herniations were most commonly classified as Type 1 or 2, patients with spinal stenosis as Type 4, and they rarely saw patients with significant complaints who were classified as Type 3. In the present study, non-DS patients were mostly classified into Type 1 or 2 (low sacral slope), and patients with DS tended to be classified into Type 3 or 4 (high sacral slope), indicating positive correlation between the spinopelvic alignments of the DS group and the Roussouly types of 3 or 4. Therefore, the translational force leading to the development of vertebral slip might be greater in DS than in non-DS patients. Furthermore, in the DS group, patients keep the lordosis without compensating for a retroverted pelvis, and the mechanical stress might be focused on the facet joints resulting in arthritis, loosening and finally vertebral slip. In the present study, L5 slope was significantly larger than L4 slope, thus the stress on the facet joints of L4/5 may be larger than that of L3/4. In contrast, there is an anatomical difference between L4/5 and L5/S1. Ligamentous structures including the iliolumbar ligament between L5 and the sacrum is stronger than that between L4 and 5. Therefore, it was suggested that vertebral slip generally developed in L4.
Our results also demonstrated that PI had weak but positive correlation with % slip. Recently, Aono et al. [1] also reported the relationship of PI and the development of DS in a long-term prospective observation of 142 female subjects without spondylolisthesis on baseline radiographs. It is suggested that greater PI may lead not only to the development, but also to the progression of vertebral slip.
Global balance was well maintained in both groups in the present study. Our results showed that there was no significant difference in PT (23.5° vs. 22.2°) between the DS and non-DS patients. Schuller et al. [22] reported a significant increase in PT (25.6° vs. 21.0°) in the DS group than in the reference group. They suggested the posterior tilt of the pelvis was a compensation mechanism in patients with high PI. However, our analyses demonstrated that the degree of correlations among the spinopelvic parameters differed between the DS and non-DS groups. In the DS group, PI was more strongly correlated with SS than with PT, suggesting that an increase in the sacral slope was the major factor compensating for a greater PI. In contrast, in the non-DS group, PI was more strongly correlated with PT than with SS, suggesting that a backward pelvic tilt was the major factor compensating for a greater PI (Fig. 5). In previous studies, lumbar lordosis varied depending on the position during imaging, measured lumbar spinal level and age of subjects. Kalichman et al. [12] reported that the mean lumbar lordosis was 46 0.2° for males and 47.6° for females. In other studies, mean lumbar lordotic angles were reported to be 46.5° in 100 young French volunteers [24]. Kanemura et al. [13] reported that the mean lumbar lordosis was 54.0° in 160 Japanese normal volunteers. In the present study, the mean LL in non-DS patients was 35.5° which was a relatively low lordosis. Thus, in the non-DS group, a loss of lordosis possibly related to advanced disc degeneration induced the compensatory increase in PT. In this mechanism, the higher the PI, the more is the compensatory increase in PT. Therefore, different mechanisms may contribute to the maintenance of spinopelvic sagittal alignment in DS and non-DS patients.
Fig. 5.
Schematic drawing depicting the different mechanisms responsible for the maintenance of spinopelvic sagittal alignment in non-DS and DS groups. In the DS group, PI was more strongly correlated with SS and LL than with PT, suggesting that an increase in the sacral slope and lumbar lordosis was the major factor compensating for a greater PI. In the non-DS group, PI was more strongly correlated with PT than with SS, suggesting that a backward pelvic tilt was the major factor compensating for a greater PI
The present study had several limitations including a small sample size, lack of a normal population, and a retrospective and cross-sectional design, rather than a longitudinal study design. However, to the best of our knowledge, this is the first report to demonstrate the importance of spinopelvic sagittal alignment, especially about PI, for the different pathomechanisms between the patients with lumbar spinal canal stenosis with or without DS regardless of the gender bias. The information obtained in this study may shed light on the pathomechanisms responsible for the onset and progression of DS.
Conclusions
PI in the DS group was significantly greater than that in the non-DS group, and PI had positive correlation with % slip. Greater PI may lead to the development and the progression of vertebral slip. The degree of the correlations among the spinopelvic parameters differed between the DS and non-DS groups; different compensatory mechanisms may contribute to the maintenance of the spinopelvic sagittal alignment in the DS and non-DS patients.
Conflict of interest
None.
References
- 1.Aono K, Kobayashi T, Jimbo S, Atsuta Y, Matsuno T. Radiographic analysis of newly developed degenerative spondylolisthesis in a mean twelve-year prospective study. Spine. 2010;35:887–891. doi: 10.1097/BRS.0b013e3181cdd1aa. [DOI] [PubMed] [Google Scholar]
- 2.Barry C, Jund J, Noseda O, et al. Sagittal balance of the pelvis-spine complex and lumbar degenerative diseases. A comparative study about 85 cases. Eur Spine J. 2007;16:1459–1467. doi: 10.1007/s00586-006-0294-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barry C, Jund J, Perrin G, et al. Spinopelvic alignment of patients with degenerative spondylolisthesis. Neurosurg. 2007;61:981–986. doi: 10.1227/01.neu.0000303194.02921.30. [DOI] [PubMed] [Google Scholar]
- 4.Cinotti G, Postacchini F, Fassari F, et al. Predisposing factors in degenerative spondylolisthesis: A radiographic and CT study. Intern Orthop. 1997;21:337–342. doi: 10.1007/s002640050180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dai LY. Orientation and tropism of lumbar facet joints in degenerative spondylolisthesis. Intern Orthop (SICOT) 2001;25:40–42. doi: 10.1007/s002640000201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Duval-Beaupère G, Schmidt C, Cosson P. A barycentremetric study of the sagittal shape of spine and pelvis: the conditions required for an economic standing position. Ann Biomed Eng. 1992;20:451–462. doi: 10.1007/BF02368136. [DOI] [PubMed] [Google Scholar]
- 7.Faro FD, Marks MC, Pawelek J, et al. Evaluation of a functional position for lateral radiograph acquisition in adolescent idiopathic scoliosis. Spine. 2004;15:2284–2289. doi: 10.1097/01.brs.0000142224.46796.a7. [DOI] [PubMed] [Google Scholar]
- 8.Gelb DE, Lenke LG, Bridwell KH, et al. An analysis of sagittal spinal alignment in 100 asymptomatic middle and older aged volunteers. Spine. 1995;20:1351–1358. [PubMed] [Google Scholar]
- 9.Grobler LJ, Robertson PA, Novotny JE, et al. Etiology of spondylolisthesis: assessment of the role played by lumbar facet joint morphology. Spine. 1993;18:80–91. doi: 10.1097/00007632-199301000-00013. [DOI] [PubMed] [Google Scholar]
- 10.Imada K, Matsui H, Tsuji H (1995) Oophorectomy predisposes to degenerative spondylolisthesis. J Bone Joint Surg [Br] 77-B: 126–130 [PubMed]
- 11.Jackson RP, Peterson MD, McManus AC, et al. Compensatory spinopelvic balance over the hip axis and better reliability in measuring lordosis to the pelvic radius on standing lateral radiographs of adult volunteers and patients. Spine. 1998;16(23):1750–1767. doi: 10.1097/00007632-199808150-00008. [DOI] [PubMed] [Google Scholar]
- 12.Kalichman L, Li L, Hunter DJ, Been E. Association between computed tomography-evaluated lumbar lordosis and features of spinal degeneration, evaluated in supine position. Spine J. 2011;11:308–315. doi: 10.1016/j.spinee.2011.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kanemura T, Kawakami N, Matsubara Y, Katayama Y, Imagama S, Matsuyama Y, Gotou M. Sagittal spinopelvic alignment in adult Japanese. J Japanese Scoliosis Soc (Spinal Deformity) 2003;18:150–155. [Google Scholar]
- 14.Legaye J, Duval-Beaupère G, Hecquet J, et al. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J. 1998;7:99–103. doi: 10.1007/s005860050038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mac-Thiong J-M, Wang Z, Guise JA, et al. Postural model of sagittal spino-pelvic alignment and its relevance for lumbosacral developmental spondylolisthesis. Spine. 2008;33:2316–2325. doi: 10.1097/BRS.0b013e318186b236. [DOI] [PubMed] [Google Scholar]
- 16.Matsunaga S, Sakou T, Morizono Y, et al. Natural history of degenerative spondylolisthesis: pathogenesis and natural course of the slippage. Spine. 1990;15:1204–1210. doi: 10.1097/00007632-199011010-00021. [DOI] [PubMed] [Google Scholar]
- 17.Rose PS, Bridwell KH, Lenke LG, et al. Role of pelvic incidence, thoracic kyphosis, and patient factors on sagittal plane correction following pedicle subtraction osteotomy. Spine. 2009;34:785–791. doi: 10.1097/BRS.0b013e31819d0c86. [DOI] [PubMed] [Google Scholar]
- 18.Rosenberg NJ (1975) Degenerative spondylolisthesis: predisposing factors. J Bone Joint Surg [Am] 57-A :467–474 [PubMed]
- 19.Roussouly P, Gollogly S, Berthonnaud E, Dimnet J. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine. 2005;30:346–353. doi: 10.1097/01.brs.0000152379.54463.65. [DOI] [PubMed] [Google Scholar]
- 20.Sanderson PL, Fraser RD (1996) The influence of pregnancy on the development of degenerative spondylolisthesis. J Bone Joint Surg [Br] 78-B: 951–954 [DOI] [PubMed]
- 21.Sato K, Wakamatsu E, Yoshizumi A, et al. The configuration of the laminas and facet joints in degenerative spondylolisthesis. Spine. 1989;14:1265–1271. doi: 10.1097/00007632-198911000-00022. [DOI] [PubMed] [Google Scholar]
- 22.Schuller S, Charles YP, Steib JP. Sagittal spinopelvic alignment and body mass index in patients with degenerative spondylolisthesis. Eur Spine J. 2011;20:713–719. doi: 10.1007/s00586-010-1640-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stagnara P, Mauroy JC, Dran G, et al. Reciprocal angulation of vertebral bodies in a sagittal plane. Approach to references for the evaluation of kyphosis and lordosis. Spine. 1982;7:335–342. doi: 10.1097/00007632-198207000-00003. [DOI] [PubMed] [Google Scholar]
- 24.Vaz G, Roussouly P, Berthonnaud E, Dimnet J. Sagittal morphology and equilibrium of pelvis and spine. Eur Spine J. 2002;11:80–87. doi: 10.1007/s005860000224. [DOI] [PMC free article] [PubMed] [Google Scholar]