Abstract
Purpose
‘Low back pain’ (LBP) is a prevalent condition with a majority showing no specific organic pathology. Distinguishing ‘secondary gain motives (SGM)’ from organic causes is imperative in clinical practice. We describe here, three new tests—resistive straight leg raise test (rSLRT), resistive forward bend test (rFBT) and heel compression test (HCT) to help differentiate patients with ‘SGM’ from those without. We conducted a prospective study to validate the above tests in predicting non-organic causes as a reason for LBP.
Methods
200 patients presenting with low back pain at the senior author’s outpatient orthopaedic clinic from Jan 2009 to Nov 2010 were studied. Patients were separated into two groups—‘SGM group’ (n = 100) and ‘non-SGM group’ (n = 100). ‘SGM group’ patients had a history of work-related accidents, road traffic accidents or assault, with a background of ongoing litigation issues or compensation benefits. rSLRT, rFBT, HCT, Schober’s test and Waddell’s five signs were performed on them. Statistical analysis was done to identify correlations between test results, MRI findings and ‘SGM’ status.
Results
Statistically significant differences were observed between the SGM and non-SGM group (p < 0.0005) for all tests studied. In predicting SGM status, rSLRT showed highest specificity (0.94) and highest positive predictive value (0.925) while HCT showed the highest negative predictive value (0.859). Positive rSLRT was found to be strongly correlated with ≥3 positive Waddell’s signs. SGM patients with positive rSLRT tended to show resistance ≤45°.
Conclusions
rSLRT, rFBT and HCT (NK triad) are highly practical tests which strongly predict SGM status in patients.
Keywords: Low back pain, Secondary gain motives, Resistive straight leg raise test (rSLRT), Resistive forward bend test (rFBT), Heel compression test (HCT)
Introduction
Approximately 70 % of the adult population experiences low back pain (LBP) at least once during their lifetime [1, 2]. Worldwide, 37 % of LBP was deemed attributable to occupational risk factors [3]. Work-related LBP was estimated to cause 818,000 disability-adjusted life years loss annually [3], with significant costs to industry [4]. However, up to 85 % of patients with LBP show no identifiable specific organic pathology [1, 2].
Non-organic causes of LBP include stress, personality issues and various ‘secondary gain motives’ (SGM) which could range from a desire to obtain exemption from work duties to seeking financial reimbursement through the legal system, e.g., those undergoing litigation, seeking compensation or involved in medico-legal cases [5–9]. Distinguishing SGM from organic disease is imperative in improving clinical practice and pertinent in the modern medico-legal climate [5–9]. However, it is often difficult to [10] distinguish patients who have a genuine organic component to their LBP from those who do not [6, 8, 9].
It is desirable to have clinical tests, which are efficient and predictable in identifying patients with SGM. In 1979, Waddell in his classic paper[11] defined 5 categories of non-organic physical signs—tenderness, simulation, distraction, regional and overreaction—which have been found to be strong predictors of SGM [12]. Correlations were also found between his signs and indications of general psychopathology on the Minnesota Multi-phasic Personality Inventory [11, 13]. However, Waddell’s signs are time-consuming to elicit and are sometimes equivocal [14]. This led various authors to describe novel tests for non-organic causes of LBP, with varied results [15]. Examples include the heel-tap test [14], production of LBP by active cervical motion of the erect individual [16] and limitation of motion in one or both shoulders distinctly accompanied by LBP [16].
Recently, Moradi et al. [17] have used three physical performance tests (Villiger test, Oesch test, Biering–Sorensen test) to differentiate between patients with somatic parameters of LBP and control group. They found these tests to display good discriminative ability and high reliability, but could not predict treatment outcome. However, these novel tests described above have to be conducted separately from standard clinical examination for the lumbar spine. Here, we describe three simple clinical tests, which can be incorporated into the routine spinal examination, which have demonstrated different results in patients with SGM. The differences observed were a ‘Straight Leg Raise Test’ (SLRT) with a downward resistive force in the first 30° of elevation; resistance to ‘Forward Bend Test’ (FBT); and exacerbation of back pain while conducting a ‘Heel compression test’ (HCT).
We performed a study to evaluate whether the above-mentioned tests were effective in identifying patients with secondary gain objectives.
Materials and methods
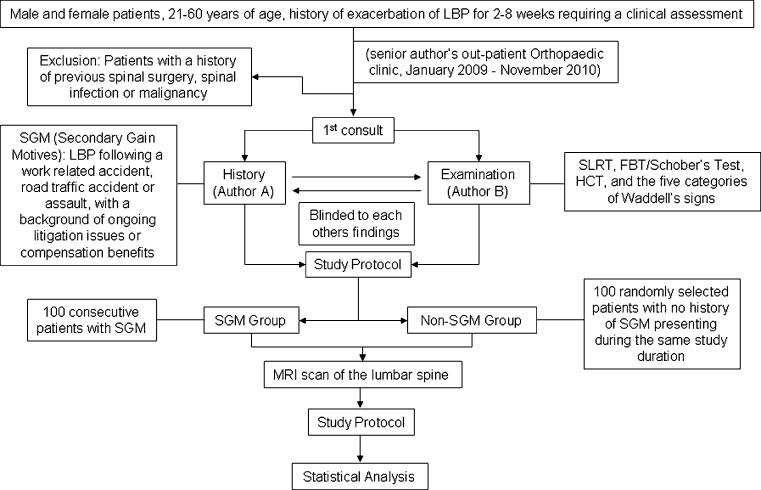
This prospective study consists of patients who presented with LBP to the senior author’s outpatient Orthopaedic clinic from January 2009 till November 2010. A study protocol was followed for clinical assessment, patient follow-up and data collection. Please refer to the methodology flow chart (Fig. 1) for details of the study design.
Fig. 1.
Illustration of methodology
The history taking and physical examination of a selected patient were carried out on the first day of clinic assessment. These two processes were not performed by the same author. One author documented the history and the presence of any possible SGM while the physical examination was carried out by another author who was not informed of the history. SLRT, FBT/Schober’s test, HCT, and the five categories of Waddell’s signs were performed on these patients. The authors documented their findings on the study protocol separately and independently.
The patients were then divided into two groups—patients with SGM, i.e., LBP following a work-related accident, road traffic accident or assault, with a background of ongoing litigation issues or compensation benefits (SGM group) and those without (non-SGM group). All the selected patients were then followed up with an MRI scan of the lumbar spine.
The resistive SLRT (rSLRT), resistive FBT (rFBT) and HCT are described in detail below.
Resistive straight leg raise test (rSLRT)
Historically, the SLRT was described by Lasègue’s pupil Forst in 1881 [18] and subsequently reported in further detail by Lazarevic [19]. The SLRT is traditionally performed with the patient in the supine position. The examiner flexes the patient’s hip while maintaining the knee in extension. With lumbar-spine pathology, this may lead to pain radiating down the leg in the appropriate nerve root distribution. This is classified as a ‘positive SLRT’. If no pain is reproduced by 90°, it is considered a ‘negative SLRT’ [20].
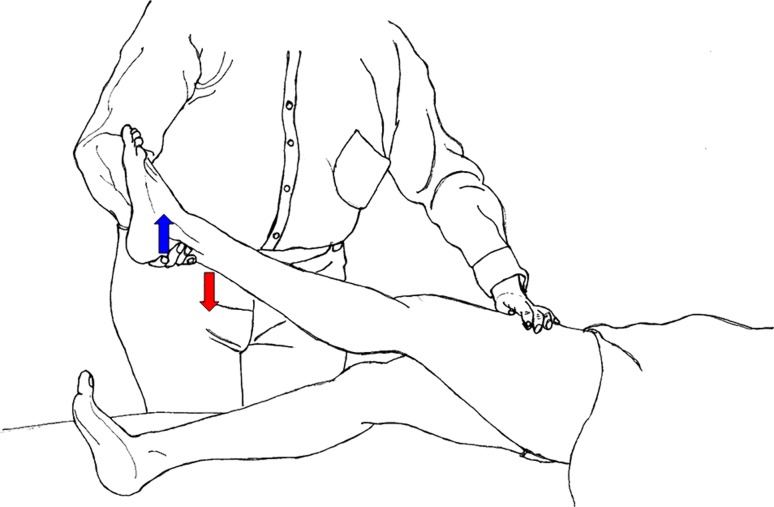
We performed the SLRT in a similar manner in our patients. If a patient actively exerts a downward resistive force on the examiner’s hand when the examiner tries to lift the leg (Fig. 2), the test would be classed as a ‘positive resistive SLRT (rSLRT)’. A non-SGM patient would be expected to allow the examiner to raise his leg without a downward resistive force until 90º or until the angle at which pain elicited is reached, assuming an organic pathology.
Fig. 2.
Demonstration of resistive straight leg raise test (rSLRT)
Resistive forward bend test (rFBT)
The standard Schober’s test (ST) is conducted by placing one mark approximately 5 cm below the posterior superior iliac spine (PSIS) and another mark about 10 cm above the PSIS. The patient is then asked to touch his/her toes. This maneuver increases the distance between the two marks, the amount of increment is measured and documented. Normal increment is 5 cm or more and there is no difficulty in bending [21].
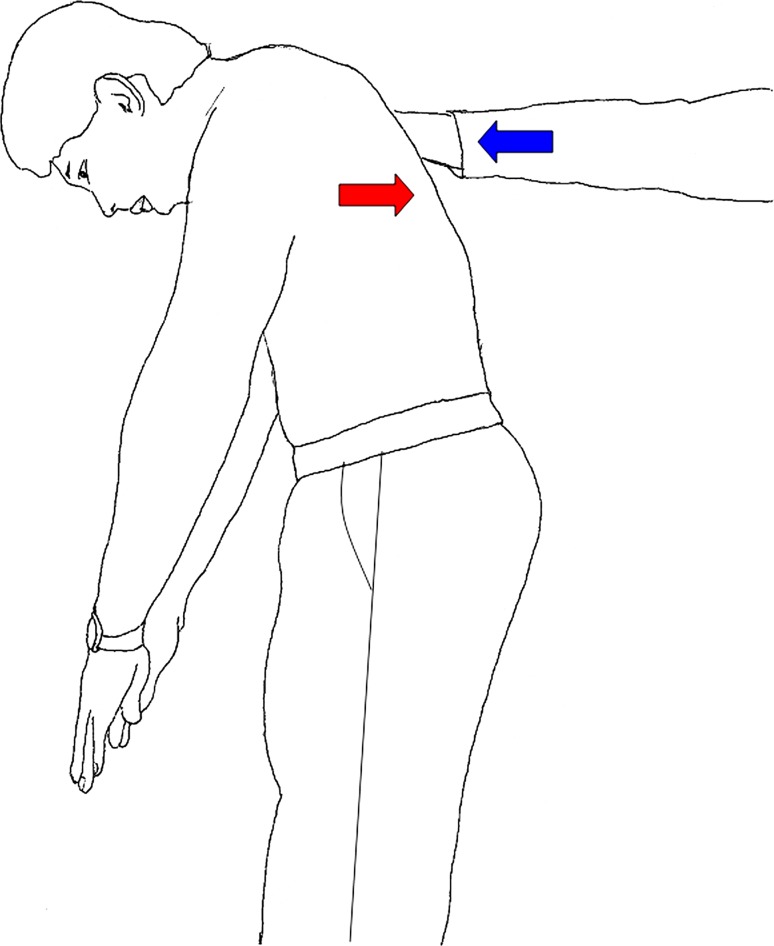
A ‘positive resistive forward bend test (rFBT)’ occurs if a patient expresses complete inability or great difficulty in bending on his or her own due to pain during the bending phase of the Schober’s test. They actively exert a resistive force on the examiner’s hand when guided to bend forwards (Fig. 3). A patient with an underlying organic pathology would be able to bend with minimal resistive force until the angle at which pain prevents him/her from bending further.
Fig. 3.
Demonstration of resistive forward bend test (rFBT)
Heel compression test (HCT)
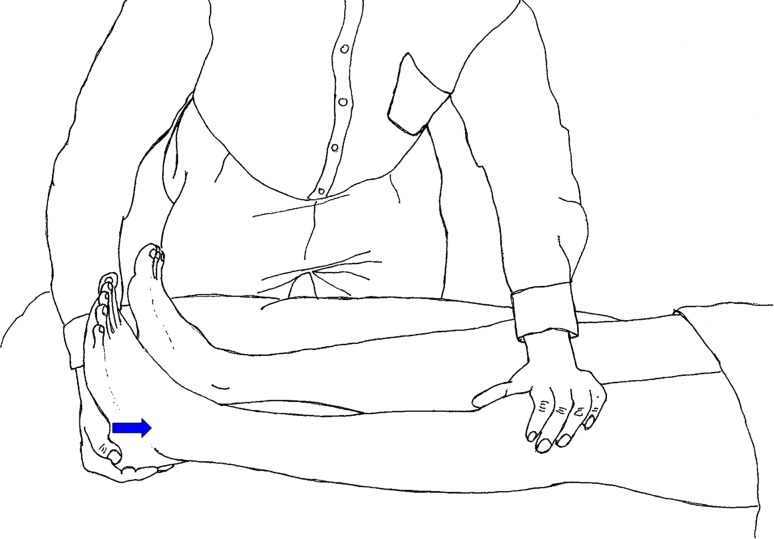
The HCT is a novel test described by the principal author. The patient lies supine on the examination couch. After suggesting that the test may or may not cause or exacerbate LBP, the examiner applies a force on the patient’s heel along the axis of the lower limb, with hip and knee in complete extension (Fig. 4). This action will not result in any movement of the spinal column and hence should not cause any LBP or leg pain. If the patient complains of onset or exacerbation of LBP, the test is considered a ‘positive heel compression test’. A patient with an underlying organic pathology would not complain of onset or exacerbation of LBP.
Fig. 4.
Demonstration of heel compression test (HCT)
Statistical methods
Patients’ demographic data and baseline clinical data were analyzed descriptively. The comparison of clinical assessments and findings in the MRI scans between the SGM and non-SGM groups was performed by using either a Chi-square test or Fisher’s exact test, where applicable. Analyses were carried out using Statistical Package for the Social Sciences (SPSS) version 18.0.
Results
A total of 200 patients were studied, of which the majority were males (n = 145). Mean age of the population was 41.91 years (range 21–60). Mean age and standard deviation in the SGM group was 41.06 (±11.705) and in the non-SGM group it was 42.76 (±13.689). In the SGM group there was slight male preponderance (males = 79 %, females = 21 %) as compared to the non-SGM group (males = 66 %, females = 34 %) (p = 0.04). Results of the rSLRT, rFBT, HCT, ST and the five categories of the Waddell’s signs showed statistically significant differences between the SGM and non-SGM groups (p < 0.0005 for each test) (Table 1).
Table 1.
Comparative analysis of rSLRT, rFBT, HCT, Waddell’s signs and Schober’s test between the SGM and non-SGM groups
| Test and results | SGM group | Non-SGM group | Pearson Chi-square value | |
|---|---|---|---|---|
| rSLRT | Positive | 74 | 6 | 96.333 (p < 0.0005) |
| Negative | 26 | 94 | ||
| rFBT | Positive | 82 | 39 | 38.686 (p < 0.0005) |
| Negative | 18 | 61 | ||
| HCT | Positive | 87 | 21 | 87.681 (p < 0.0005) |
| Negative | 13 | 79 | ||
| Tenderness | Positive | 83 | 17 | 87.120 (p < 0.0005) |
| Negative | 17 | 83 | ||
| Simulation | Positive | 52 | 6 | 51.384 (p < 0.0005) |
| Negative | 48 | 94 | ||
| Distraction 90° | Positive | 92 | 67 | 19.175 (p < 0.0005) |
| Negative | 8 | 33 | ||
| Regional | Positive | 53 | 10 | 42.846 (p < 0.0005) |
| Negative | 47 | 90 | ||
| Overreaction | Positive | 82 | 9 | 107.450 (p < 0.0005) |
| Negative | 18 | 91 | ||
| Schober’s test <5 cm | Positive | 88 | 43 | 44.806 (p < 0.0005) |
| Negative | 12 | 57 | ||
The most common finding in the MRI scans of the patients was degenerative disc disease at L4–L5, L5–S1 or both levels (27.5 % of all patients). A statistically significant number of abnormal MRI scans were observed in the non-SGM group compared to the SGM group (p < 0.0001) (Table 2). There was no statistically significant difference in the MRI scan findings between the patients who had positive or negative rSLRT within the SGM group (p = 0.6440) (Table 2).
Table 2.
Comparative analysis of MRI findings between the SGM and non-SGM groups
| SGM/Non-SGM | Normal MRI | Abnormal MRI | p value | |
|---|---|---|---|---|
| SGM | Positive rSLRT | (45) 60.8 % | (29) 39.2 % | p = 0.6440 |
| Negative rSLRT | (14) 53.9 % | (12) 46.1 % | ||
| Total | (59) 59 % | (41) 41 % | p < 0.0001 | |
| Non-SGM | Total | (11) 11 % | (89) 89 % | |
Positive rSLRT was observed in 74 % of SGM group patients. In these patients, downward resistance was first felt at a mean of 37.5° (±20.6). However, in non-SGM group patients, positive rSLRT was observed in only 6 % and downward resistance was first felt in these patients at a mean of 69.5° (±16.2). In patients with positive rSLRT, resistance felt at an angle ≤45° was highly predictive of SGM (p < 0.0001). In the SGM group, the ST showed a mean of 2.73 cm (±1.34) but in the non-SGM group the mean was 5.18 cm (±1.40). In patients with positive rFBT, resistance felt at a length ≤4 cm during the ST was highly predictive of SGM (p < 0.0001). Out of 74 patients with a positive rSLRT in the SGM group, 70 patients (94.6 %) had ≥3 positive Waddell’s signs. In the same SGM group, patients with a negative rSLRT (n = 26) only 15 patients (57.7 %) had ≥3 positive Waddell’s signs; this was statistically significant (p < 0.0001).
Table 3 shows the correlation of rFBT, HCT, Waddell’s signs and Schober’s test with rSLRT results in patients in the SGM group. Sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of the studied variables in predicting SGM are mentioned in Table 4. For individual tests, rSLRT and simulation showed the highest specificity (0.94) while distraction showed the highest sensitivity (0.92) followed by ST (0.88) and HCT (0.87). If any two tests out of rSLRT, rFBT and HCT were positive, then the sensitivity was 0.91 and NPV was 0.898. The highest specificity (0.97) and PPV (0.951) were seen when all three tests (rSLRT, rFBT and HCT) were positive.
Table 3.
Comparative analysis of Waddell’s signs, rFBT, HCT and Schober’s test with rSLRT in patients in the SGM group
| Test and results | Negative rSLRT | Positive rSLRT | Pearson Chi-square value | |
|---|---|---|---|---|
| Tenderness | Negative | 10 (58.8 %) | 7 (41.2 %) | 11.469 (p = 0.001) |
| Positive | 16 (19.3 %) | 67 (80.7 %) | ||
| Simulation | Negative | 19 (39.6 %) | 29 (60.4 %) | 8.852 (p = 0.003) |
| Positive | 7 (13.5 %) | 45 (86.5 %) | ||
| Distraction (90°) | Negative | 4 (50 %) | 4 (50 %) | 2.603 (p = 0.107) |
| Positive | 22 (23.9 %) | 70 (76.1 %) | ||
| Regional | Negative | 16 (34 %) | 31 (66 %) | 2.981 (p = 0.084) |
| Positive | 10 (18.9 %) | 43 (81.1 %) | ||
| Overreaction | Negative | 10 (55.6 %) | 8 (44.4 %) | 9.966 (p = 0.002) |
| Positive | 16 (19.5 %) | 66 (80.5 %) | ||
| rFBT | Negative | 8 (44.4 %) | 10 (55.6 %) | 3.881 (p = 0.049) |
| Positive | 18 (22.0 %) | 64 (78.0 %) | ||
| HCT | Negative | 5 (38.5 %) | 8 (61.5 %) | 1.206 (p = 0.272) |
| Positive | 21 (24.1 %) | 66 (75.9 %) | ||
| Schober’s test (≤4 cm) | Negative | 9 (56.3 %) | 7 (43.8 %) | 9.059 (p = 0.003) |
| Positive | 17 (20.2 %) | 74 (74.0 %) | ||
Table 4.
Sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of rSLRT, rFBT, HCT, Waddell’s signs and Schober’s test in predicting secondary gain motives
| Test and results | Sensitivity | Specificity | PPV | NPV |
|---|---|---|---|---|
| rSLRT | 0.74 | 0.94 | 0.925 | 0.783 |
| rFBT | 0.82 | 0.61 | 0.678 | 0.772 |
| HCT | 0.87 | 0.79 | 0.806 | 0.859 |
| Tenderness | 0.83 | 0.83 | 0.83 | 0.83 |
| Simulation | 0.52 | 0.94 | 0.897 | 0.662 |
| Distraction 90º | 0.92 | 0.33 | 0.579 | 0.805 |
| Regional | 0.53 | 0.9 | 0.841 | 0.657 |
| Overreaction | 0.82 | 0.91 | 0.901 | 0.835 |
| Schober’s test <5 cm | 0.88 | 0.57 | 0.672 | 0.826 |
| rSLRT/rFBT/HCT (at least two positive) | 0.91 | 0.79 | 0.812 | 0.898 |
| rSLRT/rFBT/HCT (all three positive) | 0.57 | 0.97 | 0.951 | 0.693 |
Discussion
The concept of ‘secondary gain motives’ (SGM) in patients seeking medical treatment is not new and has been described in detail since the early twentieth century [22]. As patients’ self-reporting forms a significant portion of clinical assessment, clinicians have always been particularly vulnerable to patients who feign, magnify or minimize problems due to ulterior motives. In a bid to aid the clinician in this aspect, Waddell in 1979 [11] created physical tests to identify non-organic causes of LBP and various authors have shown his tests to be reliable [10, 13, 23]. New ‘non-organic tests’ have been developed since [14, 16], but these have not been assessed in terms of sensitivity and specificity. Hence, such tests would be less valuable in clinical practice in exploring non-organic causes for LBP. Despite the reliability of Waddell’s signs, we have found them to be more useful for research purposes, with debatable practical functionality in a real clinic setting.
Our present study, which aims to describe and evaluate three new tests for possible non-organic causes of LBP, was done with intimate knowledge of the various pressures and heavy burdens that clinicians face in the modern medico-legal climate. Making the correct clinical decision in medico-legal cases and in treating patients with SGM often involves a fine balance of clinical acumen, empathy towards the patient and dire need for equality to all parties involved.
The three tests described in this study—rFBT, rSLRT and HCT (NK triad)—stand out from other previously described tests in terms of convenience and ease of performance. This is illustrated in two ways. Firstly, the nature of the tests themselves—FBT and SLRT are amongst the most frequently used ‘physical impairment tests’ [24] and hence will be familiar to many clinicians who already use them in their practice regularly. Secondly, the smooth transitions in which the tests can be performed—we recommend starting with rFBT (done standing up), followed by rSLRT and then HCT (patient supine). It can be seen that the order described above minimizes unnecessary patient movement and flows seamlessly from one test to another. We hope that these tests and the order described above will aid the time-pressed clinician in making difficult medico-legal decisions in a busy clinical setting.
Our results show that rFBT, rSLRT and HCT are strong individual and combined predictors of the presence of SGM in patients (Table 4). In addition, positive rSLRT in SGM group patients was found to be strongly correlating with 3 or more positive Waddell’s signs. The single best predictor of the SGM status was overreaction followed by rSLRT and HCT, respectively. However, we feel that overreaction (e.g., facial expressions, disproportionate verbalizations) is highly subjective and can vary greatly between observers but the three new tests described are more objective tests, which will show greater reproducibility between observers compared to overreaction. In addition, we have provided quantifiable values for rSLRT (≤45°) and rFBT (≤4 cm) to further enhance the objectivity of the tests to predict SGM.
Our results support the use of the three new tests—rFBT, rSLRT and HCT (NK triad)—in a clinical setting to aid clinicians in identifying the presence of SGM in patients. However, we would caution against over-interpretation of the results of this study. The resistance to forward bending or straight leg raising may arise from fear of avoidance of pain or further injury [25]. This is pertinent in patients with chronic LBP—persistent pain may have led to the development of specific ‘fear-mediated responses’, i.e., avoidance of certain movements or activities [25] which could affect their physical examination findings. The ‘SGM’ status does not exclude the presence of a genuine medical condition causing LBP. Despite the higher percentage (89 %) of abnormal MRIs in the non-SGM group, 41 % of patients in the SGM group still had abnormal MRIs.
We would like to alert the reader that the assessment of behavioral signs is not a complete psychological assessment and that the signs may be used to decide type of treatment and not used as a tool to offer or not to offer treatment [25]. All patients in our study, regardless of whether they produced positive test findings, were offered appropriate investigational modalities and treatment options for their conditions. SGM group patients with positive findings were not simply dismissed as malingerers. Studies involving psychological and psychometric testing would be useful in assessing the effectiveness of these tests (NK triad) in predicting psychological components to LBP, particularly when SGM may be involved. The tests, therefore, should only serve to alert clinicians to possible SGM in their patients, so as to act with due caution.
Acknowledgments
Dr Deepti Nayak (University Spine Centre, National University Hospital, Singapore) is thanked for illustrations.
Conflict of interest
None.
References
- 1.Deville WL, Windt DA, Dzaferagic A, Bezemer PD, Bouter LM. The test of Lasegue: systematic review of the accuracy in diagnosing herniated discs. Spine (Phila Pa 1976) 2000;25:1140–1147. doi: 10.1097/00007632-200005010-00016. [DOI] [PubMed] [Google Scholar]
- 2.Deyo RA, Tsui-Wu YJ. Descriptive epidemiology of low-back pain and its related medical care in the United States. Spine (Phila Pa 1976) 1987;12:264–268. doi: 10.1097/00007632-198704000-00013. [DOI] [PubMed] [Google Scholar]
- 3.Punnett L, Pruss-Utun A, Nelson DI, Fingerhut MA, Leigh J, Tak S, Phillips S. Estimating the global burden of low back pain attributable to combined occupational exposures. Am J Ind Med. 2005;48:459–469. doi: 10.1002/ajim.20232. [DOI] [PubMed] [Google Scholar]
- 4.Spengler DM, Bigos SJ, Martin NA, Zeh J, Fisher L, Nachemson A (1986) Back injuries in industry: a retrospective study. I. Overview and cost analysis. Spine (Phila Pa 1976) 11:241–245 [DOI] [PubMed]
- 5.Atlas SJ, Chang Y, Kammann E, Keller RB, Deyo RA, Singer DE. Long-term disability and return to work among patients who have a herniated lumbar disc: the effect of disability compensation. J Bone Joint Surg Am. 2000;82:4–15. doi: 10.2106/00004623-200001000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Janowski K, Steuden S, Kurylowicz J. Factors accounting for psychosocial functioning in patients with low back pain. Eur Spine J. 2010;19:613–623. doi: 10.1007/s00586-009-1151-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lancourt J, Kettelhut M (1992) Predicting return to work for lower back pain patients receiving worker’s compensation. Spine (Phila Pa 1976) 17:629–640 [DOI] [PubMed]
- 8.Rohling ML, Binder LM, Langhinrichsen-Rohling J. Money matters: a meta-analytic review of the association between financial compensation and the experience and treatment of chronic pain. Health Psychol. 1995;14:537–547. doi: 10.1037/0278-6133.14.6.537. [DOI] [PubMed] [Google Scholar]
- 9.Wand BM, Chiffelle LA, O’Connell NE, McAuley JH, Desouza LH. Self-reported assessment of disability and performance-based assessment of disability are influenced by different patient characteristics in acute low back pain. Eur Spine J. 2010;19:633–640. doi: 10.1007/s00586-009-1180-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Apeldoorn AT, Bosselaar H, Blom-Luberti T, Twisk JW, Lankhorst GJ. The reliability of nonorganic sign-testing and the Waddell score in patients with chronic low back pain. Spine (Phila Pa 1976) 2008;33:821–826. doi: 10.1097/BRS.0b013e318169502a. [DOI] [PubMed] [Google Scholar]
- 11.Waddell G, McCulloch JA, Kummel E, Venner RM. Nonorganic physical signs in low-back pain. Spine (Phila Pa 1976) 1980;5:117–125. doi: 10.1097/00007632-198003000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Gaines WG,, Jr, Hegmann KT. Effectiveness of Waddell’s nonorganic signs in predicting a delayed return to regular work in patients experiencing acute occupational low back pain. Spine (Phila Pa 1976) 1999;24:396–400. doi: 10.1097/00007632-199902150-00021. [DOI] [PubMed] [Google Scholar]
- 13.Maruta T, Goldman S, Chan CW, Ilstrup DM, Kunselman AR, Colligan RC. Waddell’s nonorganic signs and Minnesota Multiphasic Personality Inventory profiles in patients with chronic low back pain. Spine (Phila Pa 1976) 1997;22:72–75. doi: 10.1097/00007632-199701010-00012. [DOI] [PubMed] [Google Scholar]
- 14.Blom A, Taylor A, Whitehouse S, Orr B, Smith E. A new sign of inappropriate lower back pain. Ann R Coll Surg Engl. 2002;84:342–343. doi: 10.1308/003588402760452682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Greer S, Chambliss L, Mackler L, Huber T. Clinical inquiries. What physical exam techniques are useful to detect malingering? J Fam Pract. 2005;54:719–722. [PubMed] [Google Scholar]
- 16.Kummel BM (1996) Nonorganic signs of significance in low back pain. Spine (Phila Pa 1976) 21:1077–1081 [DOI] [PubMed]
- 17.Moradi B, Benedetti J, Zahlten-Hinguranage A, Schiltenwolf M, Neubauer E. The value of physical performance tests for predicting therapy outcome in patients with subacute low back pain: a prospective cohort study. Eur Spine J. 2009;18:1041–1049. doi: 10.1007/s00586-009-0965-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Forst JJ (1881) Contribution à l’étude clinique de la sciatique. Facultè de Mèdecine, Université de Paris Thèse, No 33
- 19.Lazarevic LK. Ischias postica Cotunnii: ein beitrag zu deren differential diagnose. Allg Wein Med Zeitung. 1884;29:425–426. [Google Scholar]
- 20.Rabin A, Gerszten PC, Karausky P, Bunker CH, Potter DM, Welch WC. The sensitivity of the seated straight-leg raise test compared with the supine straight-leg raise test in patients presenting with magnetic resonance imaging evidence of lumbar nerve root compression. Arch Phys Med Rehabil. 2007;88:840–843. doi: 10.1016/j.apmr.2007.04.016. [DOI] [PubMed] [Google Scholar]
- 21.Schober P. Lendenwirbelsäule und Kreuzschmerzen. Much Med Wochenschr. 1937;84:336–339. [Google Scholar]
- 22.Collie J. Malingering and feigned sickness. New York: Paul B. Boeber; 1913. [Google Scholar]
- 23.Hirsch G, Beach G, Cooke C, Menard M, Locke S (1991) Relationship between performance on lumbar dynamometry and Waddell score in a population with low-back pain. Spine (Phila Pa 1976) 16:1039–1043 [DOI] [PubMed]
- 24.Ekedahl KH, Jonsson B, Frobell RB. Validity of the fingertip-to-floor test and straight leg raising test in patients with acute and subacute low back pain: a comparison by sex and radicular pain. Arch Phys Med Rehabil. 2010;91:1243–1247. doi: 10.1016/j.apmr.2010.05.002. [DOI] [PubMed] [Google Scholar]
- 25.Main CJ, Waddell G (1998) Behavioral responses to examination. A reappraisal of the interpretation of “nonorganic signs”. Spine (Phila Pa 1976) 23:2367–2371 [DOI] [PubMed]