The authors describe 2 steps useful to avoid iatrogenic injury during introduction of laparoscopic ancillary trocars.
Keywords: Laparoscopic entry, Ancillary trocars, Second port trocars, First access, Complications, Vessel injury, Vascular trauma, Epigastric artery, Iatrogenic injury, Minimally invasive surgery, Laparoscopy, Trocar associated injuries
Abstract
The problem of laparoscopic entry is currently still unsolved, and despite the various techniques adopted by the surgical community, it has not yet been determined which is the correct access in all patients. Add to this the problem of safe ancillary port introduction; all surgeons must avoid vascular and visceral damage. The 2 most common problems with second port trocars are inferior and superior epigastric artery damage, and bowel loops and adhesions. Over the years, we have developed 2 steps that are very useful to avoid iatrogenic injuries to vessels and viscera. In this brief report, we explain the following 2 simple steps, called by the authors “yellow island” port entry and second trocar “tip entry guided” by a suction cannula. In our practice of more than 3400 conventional laparoscopies, with data from patients with different characteristics, surgeons who have introduced laparoscopic surgery into their daily practice might teach these steps to young fellows and trainees.
BRIEF COMMUNICATION
Operative Technique/Laparoendoscopic Education
For several years in our daily surgical practice, we have tried to find useful, simple solutions to apply in many patients. The idea of developing a new entry technique into the abdomen has arisen during discussions among laparoscopists, trainers of young surgeons: we noted that each laparoscopic operation begins with an unknown: laparoscopic entry.1 The ability to operate in laparoscopy is subjective, while laparoscopic access is objectively common to all surgeons. Although laparoscopy is usually safe, a small minority of patients worldwide experience life-threatening complications, which include injuries to blood vessels and to the bowel. Laparoscopic injuries frequently occur during the insertion of needles, trocars, and cannulae through the abdominal wall, and hence, the period of greatest risk is from the start of the procedure, until visualization within the peritoneal cavity has been established.2 The problem of laparoscopic entry is currently still unsolved, and despite various techniques adopted by the surgical community, it has not yet been determined which is the correct access for all patients.3
So we have developed a novel laparoscopic access technique by Direct Optical Access,2,4–7 to use in gynecological, surgical, and urological patients.
But the problems do not end there; the second obstacle to overcome in the laparoscopic environment is the safe introduction of ancillary or second port trocars8–11 that are used for most traditional laparoscopies.
In fact, one of the most dangerous complications in laparoscopy is injury to the inferior epigastric artery (IEA), a collateral branch of the external iliac artery. This artery has received much attention in the literature, because of its relation to laparoscopic injuries10 and femoral hernia. When the IEA originates beneath the inguinal ligament, it passes medial to the inguinal ring. The IEA may arise from the external iliac at a higher point than usual: it has been found 6.2cm above the inguinal ligament.9 The IEA may also arise from the femoral artery below the inguinal ligament or from the profunda femoral artery, or as a common trunk with the circumflex iliac artery and it may be doubled.11 The inferior epigastric may arise from, or conversely, give rise to the obturator artery: this variation is due to the anastomosis of the epigastric and obturator through their pubic branches.10 It is of considerable importance to the surgeon, since the obturator artery when derived from the inferior epigastric may run either lateral or medial to the femoral ring to reach the obturator foramen; this origin of the obturator artery from the epigastric occurs in about 20% of individuals.9 The IEA occasionally provides vascularization of the clitoris/penis, circumflex iliac, superficial epigastric, and medial femoral circumflex arteries.10 The superior or superficial epigastric artery is occasionally not seen on the dorsal surface of the rectus muscle, being either absent or buried in the muscle tissue. When present, it is usually a single stem that enters the medial portion of the muscle after a short course on the surface.8,9 The superficial epigastric artery arises from the front of the femoral artery about 1cm below the inguinal ligament, and passing through the femoral sheath and the fascia cribrosa, turns upward in front of the inguinal ligament, and ascends between the 2 layers of the superficial fascia of the abdominal wall nearly as far as the umbilicus.11 It anastomoses with branches of the inferior epigastric on the surface of the rectus muscle and with its twin on the opposite side. When muscle fibers were dissected away from the arteries, only 40% of the superior and inferior epigastric arteries were found to have any gross anastomoses. To avoid IEA damage, it is mandatory to detect the artery's anatomical course under laparoscopic view when possible.8 It should be remembered that IEA begins immediately medially at the origin of the round ligament, and it is always detectable even in obese patients. Generally, during ancillary trocar introduction, after identifying the epigastric vessels by transillumination and intraperitoneal observation, 1 to 3 secondary trocars are placed, depending on the procedure and the number of trocars required for the laparoscopy. Since 1998, we have selected and identified a laparoscopic macroscopic yellow structure, called the “yellow island” (YI): it is an accumulation of adipose subperitoneal tissue (Figure 1), which is at the lateral third of a line between the anterior superior iliac spine and the umbilicus (Figure 2). The IEA and other major blood vessels are never present in the YI; moreover, YI is more evident in obese patients, in whom it is much more difficult to see the IEA during ancillary port entry. The YI is poorly represented in thin patients, but the artery is clear and easily visualized. On the contrary, IEA is less evident in obese women, but the large representation of YI, which is very yellow, allows surgeons to safely introduce the trocar (Figure 3). Because obesity is a major problem in developed countries where traditional laparoscopy is common in every hospital, each surgeon must avoid damage to the IEA in obese women during ancillary trocar introduction. Transillumination of the abdominal wall, unfortunately, is still indicated by some schools as a maneuver likely to avoid IEA injury (Figure 4), but we have demonstrated that it is ineffective in overweight and obese women. Transillumination shows only the superficial epigastric artery, injury of which causes no problem, but injury can occur to the IEA, because vision is obscured by the lateral margin of the rectus muscles of the abdomen.10,11
Figure 1.
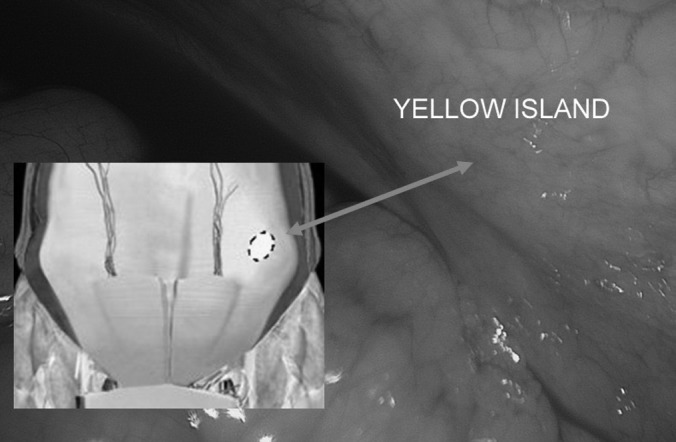
The red rings indicate the yellow island on the right lateral side of the abdominal wall.
Figure 2.
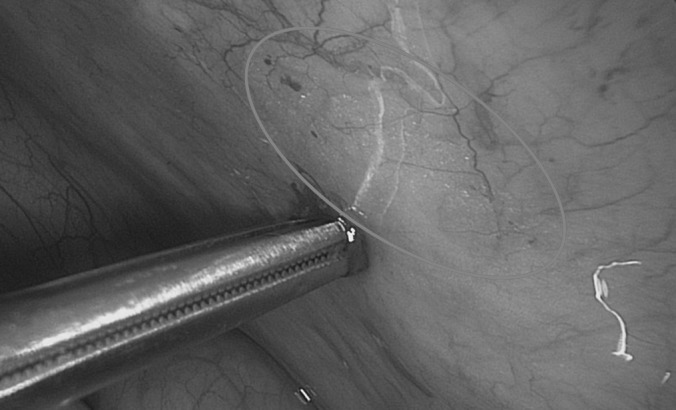
Image shows the yellow island on the right, as an accumulation of adipose subperitoneal round tissue, at the lateral third of the line between the anterior superior iliac spine and umbilicus; on the left, a corresponding computerized anatomical internal abdominal wall is reproduced.
Figure 3.
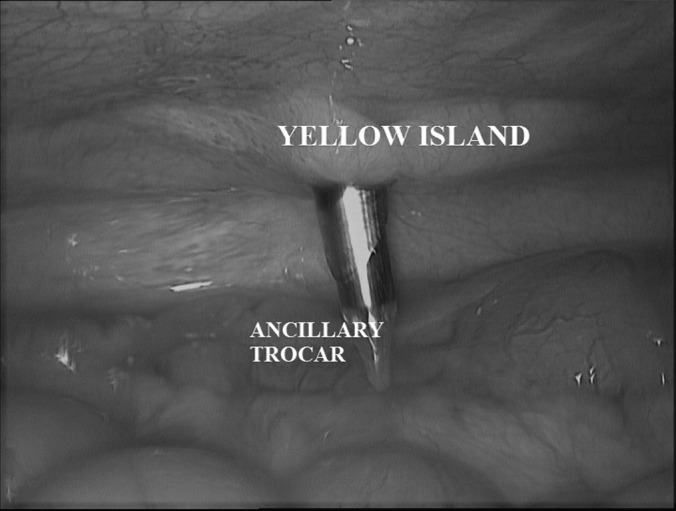
Surgeon safely introduced the first ancillary trocar though the yellow island.
Figure 4.
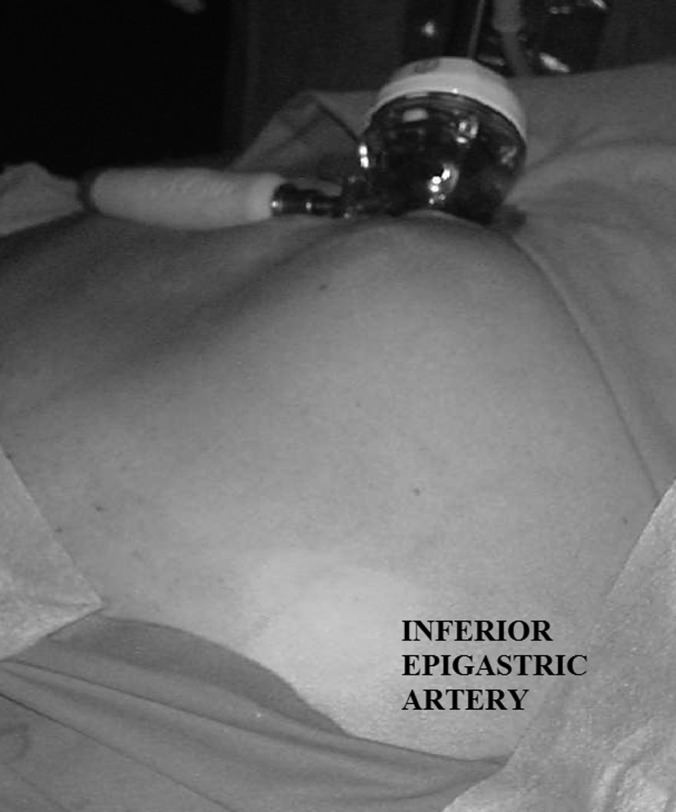
Transillumination of the abdominal wall is still indicated by some schools as a maneuver likely to avoid IEA injury, but it is clearly detectable only in thin and white-skinned women.
We have used the YI for introduction of ancillary trocars in more than 3400 laparoscopies, in women between 16 and 83 years of age (average age=49; BMI=26±4.9). The operations included ovarian cyst enucleations, myomectomies, endometriosis removal, ovariectomies, salpingectomies, hysterectomies, appendectomies, adhesiolysis, and extrauterine pregnancies. We have not experienced damage to the IEA or other blood vessels.
The second step for safe ancillary trocar introduction is a lateral maneuver performed by the first operator to help the second operator. This maneuver is of help for fellows or trainees just beginning to learn laparoscopy. The sequence that illustrates the operation is as follows: after introduction of the first ancillary trocar, often on the left side of the patient, we place a suction cannula introduced into the first lateral trocar directed to the point of introduction of the second trocar by the assistant. The surgeon must lead out of the tip of the trocar position, so that the tip of the trocar should be completely inside the suction cannula, ie, a “tip entry guided” by suction cannula (Figure 5).
Figure 5.

First operator must leak out of the tip position of the trocar, so that the tip of the second ancillary trocar is completely in the suction cannula, ie, safe “tip entry guide” by suction cannula.
The authors use this maneuver when intestinal loops or adhesions occupy the site of entry of secondary trocars. We have not had a major injury, organ damage, or vessel damage below the entry point during this safe second-step. It is recommended that the second trocar be introduced while visible by the surgeon. The function of the cannula is only for protection: it prevents the trocar tip while free in the abdominal cavity from accidentally injuring pelvic vessels and bowel loops. The tip of the trocar does not enter into the abdominal cavity, because it goes directly into the cannula.
CONCLUSION
Even if transillumination successfully visualizes most of the inferior or superficial epigastric vessels, it is less effective in those with increased weight and in dark-skinned women.12–14 In these cases you need to keep in mind the 2 techniques discussed above, the yellow island and tip entry guided by suction cannula, which can solve many problems and prevent damage to organs and viscera. The possibility of YI and the tip entry guided third trocar as safe entry sites, as recommended by the authors, could represent an important role in safe trocar entry.
Contributor Information
Andrea Tinelli, Department of Obstetrics & Gynecology, Vito Fazzi Hospital, Lecce, Italy..
Nicola Gasbarro, Unit of Obstetrics & Gynecology, Santa Maria delle Grazie Hospital, Pozzuoli (Na), Italy..
Pietro Lupo, Unit of Obstetrics & Gynecology, Santa Maria delle Grazie Hospital, Pozzuoli (Na), Italy..
Antonio Malvasi, Department of Obstetrics & Gynecology, Santa Maria Hospital, Bari, Italy..
Daniel A. Tsin, The Mount Sinai Hospital of Queens, Long Island City, New York, USA..
Fausto Davila, Universidad Autonoma de Mexico, Facultad de Estudios Superiores. Iztacala, Mexico..
Guillermo Dominguez, Fundación Hospitalaria. Buenos Aires, Argentina..
Liselotte Mettler, Professor Emeritus, Kiel School of Gynaecological Endoscopy, Department of Obstetrics and Gynaecology, University Hospitals Schleswig-Holstein, Kiel, Germany..
Paul Alan Wetter, Professor Emeritus, University of Miami School of Medicine, FL, USA and; Chairman, Society of Laparoendoscopic Surgeons (SLS)..
References:
- 1. Deguara C, Davis C. Laparoscopic entry techniques. Curr Opin Obstet Gynecol. 2011;23(4):268–272 [DOI] [PubMed] [Google Scholar]
- 2. Deffieux X, Ballester M, Collinet P, Fauconnier A, Pierre F. Risks associated with laparoscopic entry: guidelines for clinical practice from the French College of Gynaecologists and Obstetricians. Eur J Obstet Gynecol Reprod Biol. 2011;158:159–166 [DOI] [PubMed] [Google Scholar]
- 3. Ahmad G, Duffy JM, Phillips K, Watson A. Laparoscopic entry techniques. Cochrane Database Syst Rev. 2008;(2):CD006583. [DOI] [PubMed] [Google Scholar]
- 4. Tinelli A, Malvasi A, Istre O, Keckstein J, Stark M, Mettler L. Abdominal access in gynaecological laparoscopy: a comparison between direct optical and blind closed access by Veress needle. Eur J Obstet Gynecol Reprod Biol. 2010;148(2):191–194 [DOI] [PubMed] [Google Scholar]
- 5. Tinelli A, Malvasi A, Hudelist G, Istre O, Keckstein J. Abdominal access in gynaecologic laparoscopy: a comparison between direct optical and open access. J Laparoendosc Adv Surg Tech A. 2009;19(4):529–533 [DOI] [PubMed] [Google Scholar]
- 6. Tinelli A, Malvasi A, Guido M, Istre O, Keckstein J, Mettler L. Initial laparoscopic access in postmenopausal women: a preliminary prospective study. Menopause. 2009;16(5):966–70 [DOI] [PubMed] [Google Scholar]
- 7. Tinelli A, Malvasi A, Guido M, et al. Laparoscopy entry in patients with previous abdominal and pelvic surgery. Surg Innov. 2011;18:201–205 [DOI] [PubMed] [Google Scholar]
- 8. Hurd WW, Amesse LS, Gruber JS, Horowitz GM, Cha GM, Hurteau JA. Visualization of the epigastric vessels and bladder before laparoscopic trocar placement. Fertil Steril. 2003;80(1):209–212 [DOI] [PubMed] [Google Scholar]
- 9. Saber AA, Meslemani AM, Davis R, Pimentel R. Safety zones for anterior abdominal wall entry during laparoscopy: a CT scan mapping of epigastric vessels. Ann Surg. 2004;239(2):182–185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Epstein J, Arora A, Ellis H. Surface anatomy of the inferior epigastric artery in relation to laparoscopic injury. Clin Anat. 2004;17(5):400–408 [DOI] [PubMed] [Google Scholar]
- 11. Bhatti AF, Iqbal S, Lee TC. Variation in surface marking of superior epigastric vessels. A guide to safe laparoscopic port insertion. Surgeon. 2008;6(1):50–52 [DOI] [PubMed] [Google Scholar]
- 12. Pickett SD, Rodewald KJ, Billow MR, Giannios NM, Hurd WW. Avoiding major vessel injury during laparoscopic instrument insertion. Obstet Gynecol Clin North Am. 2010;37(3):387–397 [DOI] [PubMed] [Google Scholar]
- 13. Sandadi S, Johannigman JA, Wong VL, Blebea J, Altose MD, Hurd WW. Recognition and management of major vessel injury during laparoscopy. J Minim Invasive Gynecol. 2010;17(6):692–702 [DOI] [PubMed] [Google Scholar]
- 14. Vilos GA, Ternamian A, Dempster J, Laberge PY, The Society of Obstetricians and Gynaecologists of Canada Laparoscopic entry: a review of techniques, technologies, and complications. J Obstet Gynaecol Can. 2007;29(5):433–465 [DOI] [PubMed] [Google Scholar]


