Abstract
Purpose
Early-life stress (ELS) has a long-lasting effect on affective function and may entail an increased risk for major depressive disorder (MDD). However, resilience can play a protective role against developing psychopathology. In this study, we investigated the relationships of depressive symptoms with ELS and resilience in MDD.
Materials and Methods
Twenty-six patients with MDD as well as age- and gender-matched healthy controls were included in this study. Each subject was assessed concerning ELS, resilience, and depressive symptom severity with self-report questionnaires. Independent samples t-test and Mann-Whitney test were performed to compare ELS and resilience between the patient and control groups. Spearman correlation analyses and linear regression analysis were conducted to investigate significant ELS and resilience factors associated with depressive symptoms.
Results
In the MDD patient group, subjects reported greater exposure to inter-parental violence, and five factor scores on the resilience scale were significantly lower in comparison to the control group. In linear regression analysis, in regards to resilience, depressive symptom score was significantly associated with self-confidence and self-control factors; however, ELS demonstrated no significant association with depressive symptoms.
Conclusion
Among resilience factors, self-confidence and self-control may ameliorate depressive symptoms in MDD. ELS, including inter-parental violence, physical abuse and emotional abuse, might be a risk factor for developing depression. Assessment of early-life stress and intervention programs for increasing resilience capacity would be helpful in treating MDD.
Keywords: Resilience, self-confidence, self-control, inter-parental violence, depressive disorder
INTRODUCTION
Early-life stress (ELS) including abuse, neglect, and exposure to inter-parental violence may cast a long-lasting shadow on one's life and can lead to lifetime psychiatric morbidities. Numerous studies have shown that ELS exerts considerable enduring effects on affective and cognitive function,1 and is associated with a significantly increased risk of developing depression.2 In the seminal study by McCauley, et al.3 the authors demonstrated that women with a history of childhood, but not adulthood, abuse showed increases in depression and anxiety symptoms. Subsequent epidemiological studies demonstrated a strong dose-response relationship between stressful events in early-life and mental health problems in adulthood,4 as well as a 2- to 5- fold increased risk of attempted suicide.5
Resilience is used to describe the personal characteristics that enable one to adapt to environmental challenges and to overcome adversities or stressors.6 It comprises the ability to cope with stress, as well as other important protective factors, and has been shown to protect against the development of psychopathology.7 Moreover, depressive disorder has been linked with low resilience to stress, a relationship that has been studied both biologically and psychologically.8
Simultaneous investigation of ELS and resilience in a single patient group with major depressive disorder (MDD) is warranted since these psychological characteristics may have an interactive effect on depressive symptom severity in such patients. Accordingly, in this study, ELS and resilience in patients with MDD were assessed to investigate the relationship between these psychological factors and depressive symptom severity. We hypothesized that patients with MDD might report greater ELS and decreased resilience capacity compared to controls. In addition, we attempted to uncover specific ELS and resilience factors associated with depressive symptom severity in MDD patients.
MATERIALS AND METHODS
Participants
Twenty-six patients with MDD (7 males and 19 females; mean age of 31.9±1.8 years) were recruited by hospital staff psychiatrists. Diagnosis of MDD was confirmed using the Korean version of the Structured Clinical Interview for DSM-IV.9 Exclusion criteria included a current diagnosis of an Axis I disorder other than MDD requiring psychiatric treatment, a DSM-IV Axis II diagnosis, and current or past serious medical or neurological illness. All of the MDD patients were receiving antidepressant treatment.
An age- and gender-matched healthy control group (mean age of 32.3±1.7 years) was recruited from community and hospital advertisements. All subjects were interviewed for current or past medical or psychiatric illness by a psychiatrist prior to participating in the study. They were ascertained to have no current Axis I or Axis II disorders, or current serious medical or neurological illness. This study was approved by the Institutional Review Board of the ethical committee of the Hallym University Sacred Heart Hospital. All subjects provided written informed consent after receiving a thorough description of the study.
Assessment of psychosocial characteristics
ELS profiles of the subjects were assessed using the Korean Early-Life Abuse Experience Questionnaire. This questionnaire was organized by Oh10 and comprises 44 items that inquire about exposure to five categories of ELS, including emotional abuse (5 items), physical abuse (9 items), neglect (10 items), and inter-parental violence (10 items), on the Parent-Child Conflict Tactics Scale,11 in addition to 10 items concerning sexual abuse on another scale developed by Korean researchers.12 This questionnaire was developed to investigate exposure frequencies to ELS during childhood and adolescence, and demonstrated considerable reliability in the original study (Cronbach's alpha: 0.79 for emotional abuse, 0.81 for physical abuse, 0.88 for neglect, 0.80 for sexual abuse, and 0.95 for inter-parental violence).
Resilience was measured using a brief self-reporting tool of 27 items developed by Connor and Davidson.13 Recently, the Korean-version of this scale was translated and standardized, demonstrating sound psychometric properties and a five-factor structure similar to the original version with significant internal consistency (Cronbach's alpha=0.93).14
Depressive symptom severity was assessed using the Korean version of the Beck Depression Inventory.15 Other psychosocial variables that may affect depressive symptom severity, including education level, marital status, and economic status were also assessed.
Statistical analysis
Demographic variables including education, marital status, and total family income level were compared between the patient and control groups using independent samples t-test and Fisher's exact test. ELS factor scores and depressive symptom severity were not normally distributed and these variables were compared using the Mann-Whitney test. ELS factor scores were transformed with the natural log function for correlation and regression analysis. Resilience factor scores were compared between the two groups using independent samples t-test. Spearman correlation analyses and linear regression analysis were conducted to assess significant relationships for depressive symptom severity with ELS and resilience factors in each group.
RESULTS
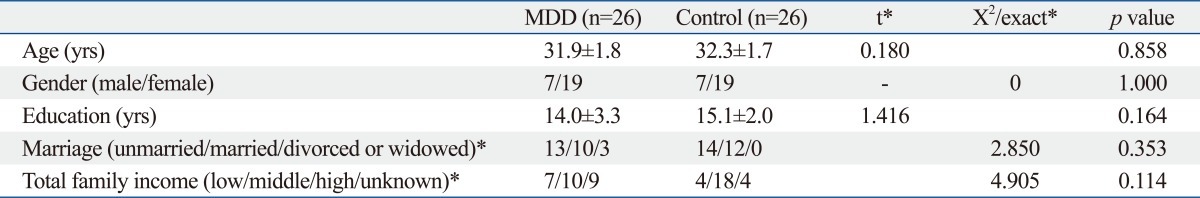
There were no significant differences in age, gender distribution, education level, marital status, or economic status between the patient and control groups (Table 1).
Table 1.
Comparisons of Demographic Characteristics between the Major Depressive Disorder and Control Groups
MDD, major depressive disorder patient group.
Values are presented as mean±standard error.
*Fisher's exact test was performed for distribution analysis of marriage and family income status.
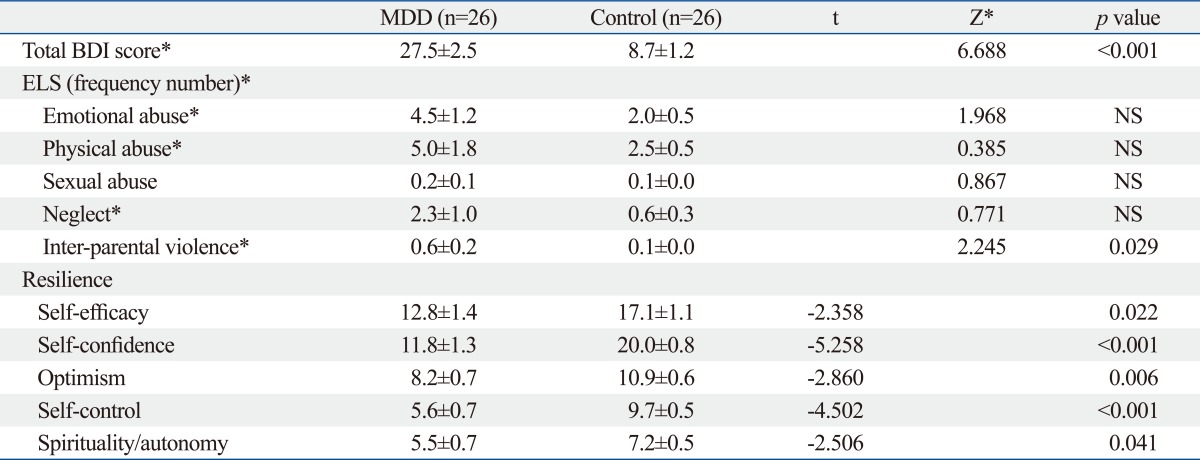
Among ELS factors, the patient group reported significantly increased experiences of exposure to inter-parental violence compared to the control group (Z=2.245, p=0.029). All of the factor scores on the resilience scale were significantly decreased in the patient group compared to the control group (Table 2).
Table 2.
Comparisons of Psychological Characteristics between the Major Depressive Disorder and Control Groups
BDI, Beck Depression Inventory; ELS, early life stress; MDD, major depressive disorder patient group; NS, not significant.
Values are presented as mean±standard error.
*Mann-Whitney tests were performed for variables which did not assume equal distribution.
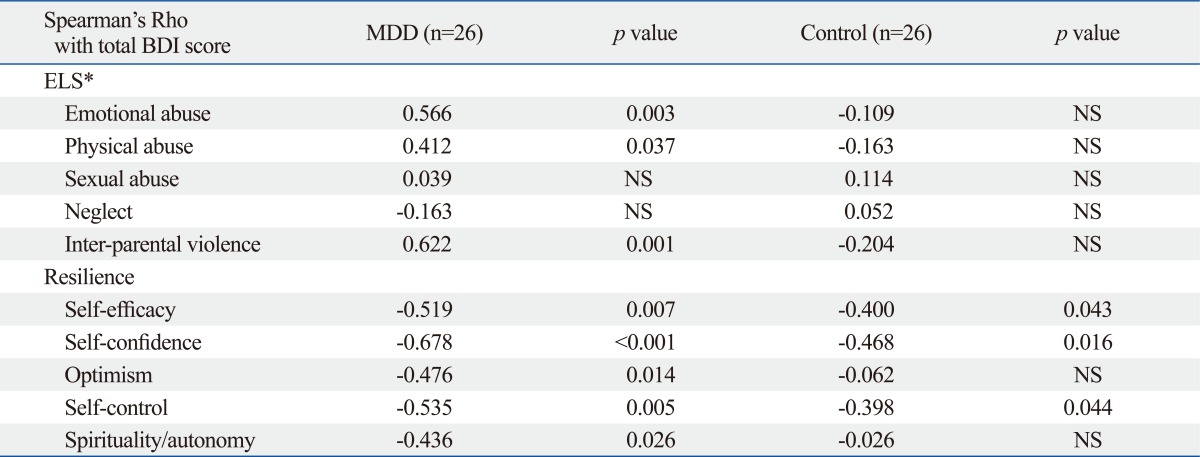
The results of the Spearman correlation analyses are presented in Table 3. In the MDD group, depressive symptom severity showed a significant positive correlation with emotional and physical abuse and inter-parental violence frequencies (emotional abuse: r=0.566; physical abuse: r=0.412; inter-parental violence: r=0.622), as well as a significant negative correlation with all of the resilience factor scores (self-efficacy: r=-0.519, self-confidence: r=-0.678; optimism: r=-0.476; self-control: r=-0.535; spirituality/autonomy: r=-0.436). In the control group, depressive symptom scores showed no significant correlation with ELS factors. In this group, several resilience factors were negatively correlated with depressive symptom severity (self-efficacy: r=-0.400; self-confidence: r=-0.468; self-control: r=-0.398).
Table 3.
Relationship of Depressive Symptom Severity with ELS and Resilience Factors
BDI, Beck Depression Inventory; ELS, early life stress; MDD, major depressive disorder patient group; NS, not significant.
*ELS frequency scores were transformed using the natural log function for normal distribution.
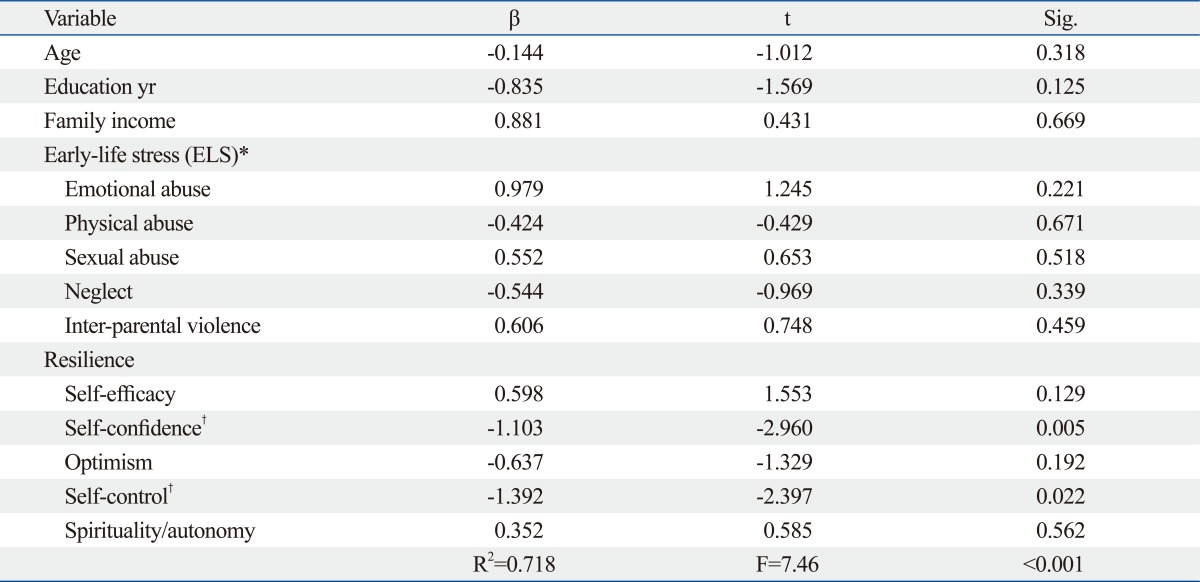
The results of the linear regression analysis of depressive symptoms are summarized in Table 4. In the present study, the linear regression model was significant, explaining 71.8% of total variance in depressive symptoms scores in this group (R2=0.718, F=7.46, p<0.001). Among resilience factors, depressive symptom severity was significantly associated with self-confidence (beta=-1.103, t=-2.960, p=0.005) and self-control (beta=-1.392, t=-2.397, p=0.022). ELS factors did not show a significant association with depressive symptom score in the final regression model.
Table 4.
Multiple Regression Analysis of Depressive Symptoms for Early-Life Stress and Resilience (n=52)
Dependent variable: Beck Depression Inventory score.
*ELS frequency scores were transformed using the natural log function for normal distribution.
†Results with two-sided probability less than 0.05 were considered significant.
DISCUSSION
In the present study, MDD patients reported greater experience of early life stress and decreased resilient capacity compared to the control group. This is the first study to report on ELS and resilience profiles for MDD patients in Korea. ELS has consistently been reported to increase the risk of developing MDD.2 Specifically, patients in the MDD group in this study reported significantly greater exposure to inter-parental violence. Among adverse experiences during early life, exposure to inter-parental violence has received less attention than other well-known stressful events such as child abuse or neglect. However, a recent large-scale longitudinal cohort study revealed that exposure to inter-parental violence had an independent impact on adulthood depressive symptoms, even when controlling for other family- or social-level stressors.16 If a child frequently encounters parental conflict, he or she may develop a pessimistic attitude toward the world or marital relations, and may lead to the development of a dysfunctional cognitive style concerning the self and others, which can induce depressive disorders later on.
Emotional and physical abuse is also an important ELS factor because it could have a life-long negative impact on a child's mental health. The present study found that depressive symptoms in the MDD group showed positive correlation with physical and emotional abuse as well as inter-parental violence. Since physical abuse may only be the tip of the iceberg in regards to dysfunctional parent-child relationships, mental health professionals should pay attention to the emotional context of physical abuse, and screen for possible concealed histories of emotional abuse.17 In a large Asian community sample study, physical abuse was significantly associated with inter-parental violence. Additionally, the authors reported that experiencing dual violence during childhood could have a long-term detrimental impact on a young adult's mental health.18 These adverse experiences are also considered important predisposing factors to the development of psychopathology later on into adulthood.19
Moreover, resilience factor scores on the resilience scale were significantly lower in the MDD group than in the control group. Among them, all of the resilience factor scores showed a significant inverse correlation with depressive symptom severity in the MDD group, and the among the resilience factors, self-control and self-confidence were significantly associated with depressive symptom severity in the final regression model. A previous study reported that positive self-esteem and ego function predicted resilient functioning in maltreated children, whereas relationship function had more of an effect on resilient functioning in non-maltreated children.20 For those who have experienced significant ELS, resilience might be a more important factor for protecting against the development and aggravation of depressive symptoms. Even though resilience is generally considered to have trait-like characteristics, resilience capacity can be changed. Longitudinal research, conducted from 1975 to 1993, emphasized the importance of the changeability of resilience properties via interaction with the environment,21 which was consistent with other studies.22 Using the dynamic characteristics of resilience, teenagers who underwent the Pennsylvania Resiliency Program showed less depressive symptoms compared to the control group.23 Reduced resilience capacity in the MDD group may be related to depressive disorder. However, this suggestion needs to be validated by future studies in which changes in resilience after remission of depressive episodes are assessed.
This study has several limitations. First, the ELS profiles of the subjects were assessed with a retrospective self-report questionnaire. Recall bias or deficits24 in addition to a propensity to report negative self and other evaluations25 associated with MDD may confound the ELS results in the patient group. However, retrospective and prospective studies that investigated individuals who were exposed to trauma demonstrated an increased morbidity for MDD,26 and greater ELS in MDD patients has been consistently reported in epidemiologic studies.3,4,27,28 Moreover, a role for adverse childhood experiences in the development of major depression has been demonstrated in twin studies.29,30 Follow-up assessments of ELS profiles after remission of depressive symptoms in the patient group could be conducted to expound on the confounding effect of major depressive episodes in future studies. Second, this was a cross-sectional study, and was unable to observe changes in resilience and ELS profiles after treatment. Consecutive assessment of resilience and ELS over the treatment course of MDD may help to further define the relationship between ELS, resilience, and depressive symptoms in MDD. Third, the effects of medication on the ELS profile, resilience, and emotional response in the patient group could not be assessed. We could not control for the effects of medication in this study because it was a natural observational study in usual outpatient clinics. Also, we could not evaluate the relationships for ELS and resilience with medication response in this patient group because it is a cross-sectional multicenter study. Fourth, a relatively small number of subjects were enrolled. More than 100 subjects need to be enrolled to conduct regression analyses with ten significant independent variables. Further study including a larger number of subjects needs to be conducted to replicate and validate the results of this study. Fifth, as only self-report questionnaires or scales were used in this study, clinician-rating scales should be considered in future study to generate results that are more meaningful. Finally, there is no published data on the convergent or external validity of the Korean Early-Life Abuse Experience Questionnaire. Validation study thereon or development of other validated questionnaire needs to be performed.
In the present study, we found a possibility that resilience capacity, especially self-confidence and self-control factors, could ameliorate depressive symptoms in patients with MDD. ELS, including inter-parental violence, physical abuse and emotional abuse, might be a risk factor for developing depression. Assessing ELS profiles and developing intervention programs for enhancing resilience capacity in treating MDD should be considered.
ACKNOWLEDGEMENTS
Members of the Korean Affective Neuroscience Study Group, who are supported by the Korean Society of Biological Psychiatry, participated in conducting this study. This study was supported by Korea Research Foundation (2009-0093893 and 2006-2005152) and by the 2010 Jisan Cultural Psychiatric Research Grant from the Korean Foundation of Neuropsychiatric Research.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Pechtel P, Pizzagalli DA. Effects of early life stress on cognitive and affective function: an integrated review of human literature. Psychopharmacology (Berl) 2011;214:55–70. doi: 10.1007/s00213-010-2009-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Heim C, Newport DJ, Mletzko T, Miller AH, Nemeroff CB. The link between childhood trauma and depression: insights from HPA axis studies in humans. Psychoneuroendocrinology. 2008;33:693–710. doi: 10.1016/j.psyneuen.2008.03.008. [DOI] [PubMed] [Google Scholar]
- 3.McCauley J, Kern DE, Kolodner K, Dill L, Schroeder AF, DeChant HK, et al. Clinical characteristics of women with a history of childhood abuse: unhealed wounds. JAMA. 1997;277:1362–1368. [PubMed] [Google Scholar]
- 4.Edwards VJ, Holden GW, Felitti VJ, Anda RF. Relationship between multiple forms of childhood maltreatment and adult mental health in community respondents: results from the adverse childhood experiences study. Am J Psychiatry. 2003;160:1453–1460. doi: 10.1176/appi.ajp.160.8.1453. [DOI] [PubMed] [Google Scholar]
- 5.Dube SR, Anda RF, Felitti VJ, Chapman DP, Williamson DF, Giles WH. Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: findings from the Adverse Childhood Experiences Study. JAMA. 2001;286:3089–3096. doi: 10.1001/jama.286.24.3089. [DOI] [PubMed] [Google Scholar]
- 6.Block J, Kremen AM. IQ and ego-resiliency: conceptual and empirical connections and separateness. J Pers Soc Psychol. 1996;70:349–361. doi: 10.1037//0022-3514.70.2.349. [DOI] [PubMed] [Google Scholar]
- 7.Masten AS, Best KM, Garmezy N. Resilience and development: contributions from the study of children who overcome adversity. Dev Psychopathol. 1990;2:425–444. [Google Scholar]
- 8.Southwick SM, Vythilingam M, Charney DS. The psychobiology of depression and resilience to stress: implications for prevention and treatment. Annu Rev Clin Psychol. 2005;1:255–291. doi: 10.1146/annurev.clinpsy.1.102803.143948. [DOI] [PubMed] [Google Scholar]
- 9.Han OS, Hong JP. Korean version of Structured Clinical Interview for DSM-IV. Seoul: Hana Medical Publishing Company; 2000. [Google Scholar]
- 10.Oh HJ. Effects of chldhood abuse and exposure to parental violence on problem in drinking in later life (In Korean) Seoul: Yonsei University; 2004. [Thesis] [Google Scholar]
- 11.Straus MA. Measuring intrafamily conflict and violence: the conflict tactics (CT) scales. J Marriage Fam. 1979;41:75–88. [Google Scholar]
- 12.Jang HJ. The development of a child abuse assessment scale (In Korean) Seoul, Korea: Sookmyung Women's University; 1998. [doctoral dissertation] [Google Scholar]
- 13.Connor KM, Davidson JR. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC) Depress Anxiety. 2003;18:76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- 14.Baek HS, Lee KU, Joo EJ, Lee MY, Choi KS. Reliability and validity of the Korean version of the connor-davidson resilience scale. Psychiatry Investig. 2010;7:109–115. doi: 10.4306/pi.2010.7.2.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rhee MK, Lee YH, Park SH, Sohn CH, Chung YC, Hong SK, et al. A standardization study of Beck Depression Inventory I - Korean version (K-BDI): reliability and factor analysis. Korean J Psychopathol. 1995;4:77–95. [Google Scholar]
- 16.Roustit C, Renahy E, Guernec G, Lesieur S, Parizot I, Chauvin P. Exposure to interparental violence and psychosocial maladjustment in the adult life course: advocacy for early prevention. J Epidemiol Community Health. 2009;63:563–568. doi: 10.1136/jech.2008.077750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rees CA. Understanding emotional abuse. Arch Dis Child. 2010;95:59–67. doi: 10.1136/adc.2008.143156. [DOI] [PubMed] [Google Scholar]
- 18.Shen AC. Long-term effects of interparental violence and child physical maltreatment experiences on PTSD and behavior problems: a national survey of Taiwanese college students. Child Abuse Negl. 2009;33:148–160. doi: 10.1016/j.chiabu.2008.07.006. [DOI] [PubMed] [Google Scholar]
- 19.Boxer P, Terranova AM. Effects of multiple maltreatment experiences among psychiatrically hospitalized youth. Child Abuse Negl. 2008;32:637–647. doi: 10.1016/j.chiabu.2008.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cicchetti D, Rogosch FA. The role of self-organization in the promotion of resilience in maltreated children. Dev Psychopathol. 1997;9:797–815. doi: 10.1017/s0954579497001442. [DOI] [PubMed] [Google Scholar]
- 21.Egeland B, Carlson E, Sroufe LA. Resilience as process. Dev Psychopathol. 1993;5:517–528. [Google Scholar]
- 22.Montpetit MA, Bergeman CS, Deboeck PR, Tiberio SS, Boker SM. Resilience-as-process: negative affect, stress, and coupled dynamical systems. Psychol Aging. 2010;25:631–640. doi: 10.1037/a0019268. [DOI] [PubMed] [Google Scholar]
- 23.Gillham JE, Reivich KJ, Freres DR, Chaplin TM, Shatté AJ, Samuels B, et al. School-based prevention of depressive symptoms: a randomized controlled study of the effectiveness and specificity of the Penn Resiliency Program. J Consult Clin Psychol. 2007;75:9–19. doi: 10.1037/0022-006X.75.1.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Burt DB, Zembar MJ, Niederehe G. Depression and memory impairment: a meta-analysis of the association, its pattern, and specificity. Psychol Bull. 1995;117:285–305. doi: 10.1037/0033-2909.117.2.285. [DOI] [PubMed] [Google Scholar]
- 25.Gara MA, Woolfolk RL, Cohen BD, Goldston RB, Allen LA, Novalany J. Perception of self and other in major depression. J Abnorm Psychol. 1993;102:93–100. doi: 10.1037//0021-843x.102.1.93. [DOI] [PubMed] [Google Scholar]
- 26.Breslau N, Davis GC, Peterson EL, Schultz LR. A second look at comorbidity in victims of trauma: the posttraumatic stress disorder-major depression connection. Biol Psychiatry. 2000;48:902–909. doi: 10.1016/s0006-3223(00)00933-1. [DOI] [PubMed] [Google Scholar]
- 27.Brown GW, Moran P. Clinical and psychosocial origins of chronic depressive episodes. I: a community survey. Br J Psychiatry. 1994;165:447–456. doi: 10.1192/bjp.165.4.447. [DOI] [PubMed] [Google Scholar]
- 28.Chapman DP, Whitfield CL, Felitti VJ, Dube SR, Edwards VJ, Anda RF. Adverse childhood experiences and the risk of depressive disorders in adulthood. J Affect Disord. 2004;82:217–225. doi: 10.1016/j.jad.2003.12.013. [DOI] [PubMed] [Google Scholar]
- 29.Kendler KS, Kessler RC, Neale MC, Heath AC, Eaves LJ. The prediction of major depression in women: toward an integrated etiologic model. Am J Psychiatry. 1993;150:1139–1148. doi: 10.1176/ajp.150.8.1139. [DOI] [PubMed] [Google Scholar]
- 30.Nelson EC, Heath AC, Madden PA, Cooper ML, Dinwiddie SH, Bucholz KK, et al. Association between self-reported childhood sexual abuse and adverse psychosocial outcomes: results from a twin study. Arch Gen Psychiatry. 2002;59:139–145. doi: 10.1001/archpsyc.59.2.139. [DOI] [PubMed] [Google Scholar]