Abstract
Purpose
Glycogen rich clear cell carcinoma (GRCC) of the breast is a rare subtype of invasive ductal carcinoma and involves a poor prognosis. In the literature, less than 150 cases have been reported. Many researchers have attempted to characterize GRCC according to electron microscope, flow cytometry, or clinical data. However, an organized study of the immunophenotype of GRCC has yet to be reported.
Materials and Methods
Here, we present three cases of GRCC and their immunohistochemical profiles.
Results
Histologically, all three cases contained periodic acid stain (PAS) positive and d-PAS labile granules in their clear cytoplasm. Case I showed positivity for only estrogen receptor (ER) and c-erbB2. Case II exhibited positivity for progesterone receptor and negativity for ER and c-erbB2. Case III presented with triple negative invasive carcinoma. The expression pattern of E-cadherin was concordant with epidermal growth factor receptor and c-kit, but discordant with ki-67. Among these three cases, p53-positive cases exhibited a low proliferative index (ki-67: 15%), while p53-negative cases showed a high proliferative index (ki-67: 50-60%).
Conclusion
In conclusion, the immunophenotype of GRCC is not uniform, but is similar to that of conventional ductal carcinoma.
Keywords: Breast, carcinoma, clear cell, glycogen, immunohistochemistry
INTRODUCTION
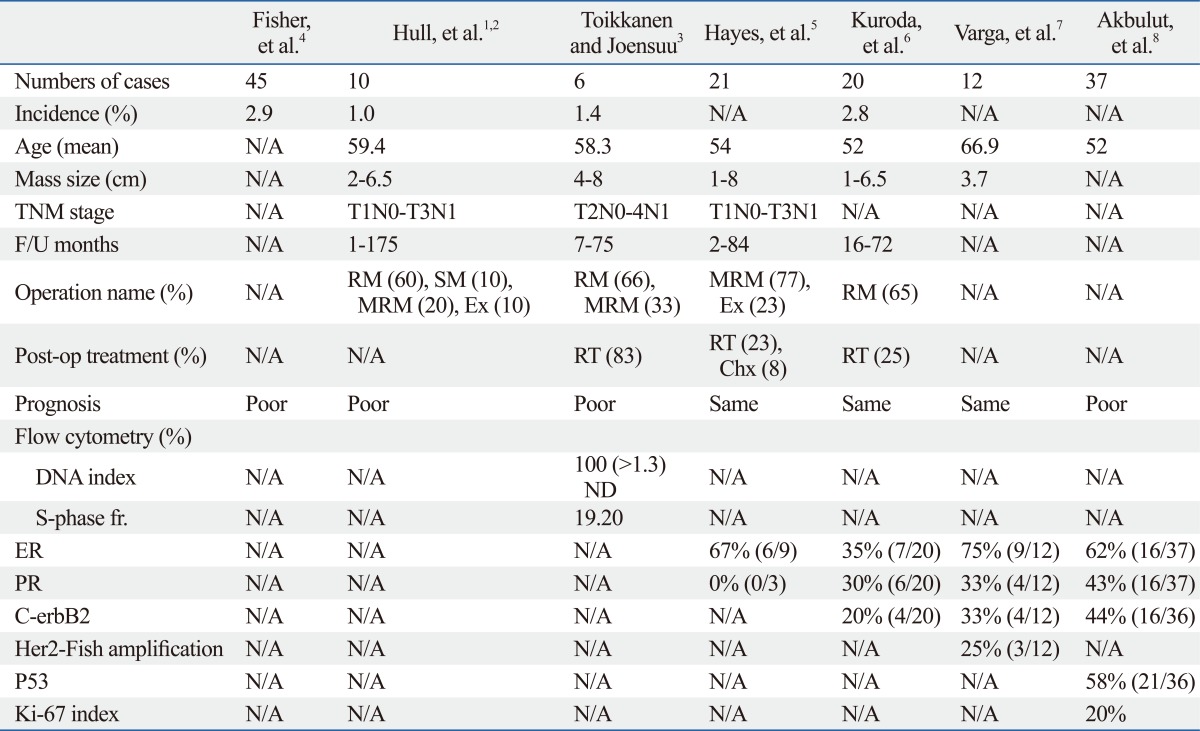
Glycogen rich clear cell carcinoma (GRCC) of the breast is known as a rare subtype of invasive ductal carcinoma, and involves a poor prognosis. It was first described by Hull, et al.1 in 1981. Since then, fewer than 150 cases have been reported. Many researchers have attempted to characterize GRCC, according to, electron microscope (EM),1,2 flow cytometry,3 or clinical data,4-6 the results of which have been summarized in Table 1.
Table 1.
GRCC in Previous Publications
N/A, not available; F/U, follow up; RM, radical mastectomy; SM, simple mastectomy; MRM, modified radical mastectomy; Ex, excision; RT, radiation therapy; Chx, chemotherapy; fr, fraction; ND, non-diploid; ER, estrogen receptor; PR, progesterone receptor; GRCC, glycogen rich clear cell carcinoma.
Hull, et al.1 confirmed intracytoplasmic glycogen of GRCC by EM and stated that the H&E and EM features of GRCC were very similar to the morphology of 13-week old fetal developing mammary gland. In diagnosing GRCC, tumor cells that contain abundant fine glycogen granules in their clear cytoplasm, are stained by periodic acid stain (PAS), but not stained by diastase-periodic acid stain (d-PAS). The incidence of GRCC is estimated to be 1 to 3% of breast carcinoma. Opinions differ with among researchers concerning the prognosis of GRCC, ranging from favorable to unfavorable.2-6 Immunohistochemical (IHC) staining for estrogen receptor (ER) is usually positive. However, IHC for progesterone receptor (PR) and c-erbB2 has been shown to vary.5-8 Other than hormone receptors, no organized study concerning the immunophenotype of GRCC has been published. Here, we present three cases of GRCC and their immunohistochemical profiles.
MATERIALS AND METHODS
Clinical data
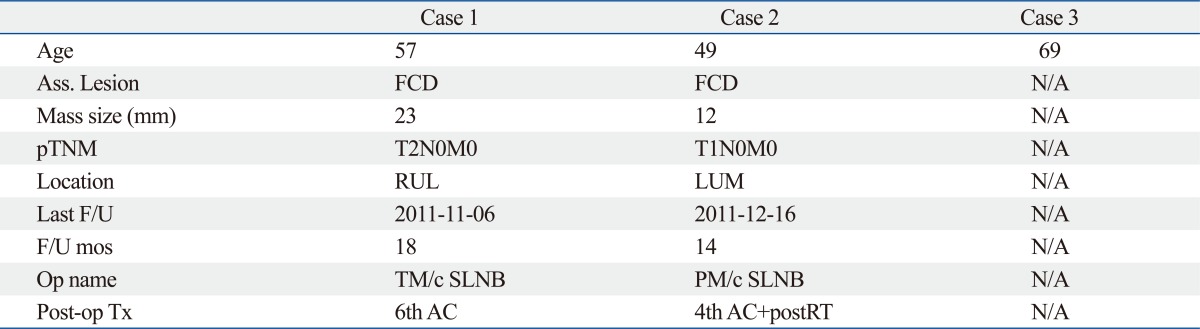
Table 2 summarizes the clinical data. There were only three cases found during the last 10 years. One case was lost to follow up after diagnosis by biopsy. The ages at diagnosis were 49 to 69 years old and follow up data were 14 months and 18 months. They were currently disease-free states. They were treated with total and partial mastectomy followed by chemotherapy and radiation therapy.
Table 2.
Clinical Findings
FCD, fibrocystic change; RUL, right upper lateral; LUM, left upper medial; F/U, follow up; TM/c SLNB, total mastectomy with sentinel node biopsy; PM/c SLNB, partial mastectomy with sentinel node biopsy; AC, cyclophosphamide+adriamycin; RT, radiation therapy; N/A, not available.
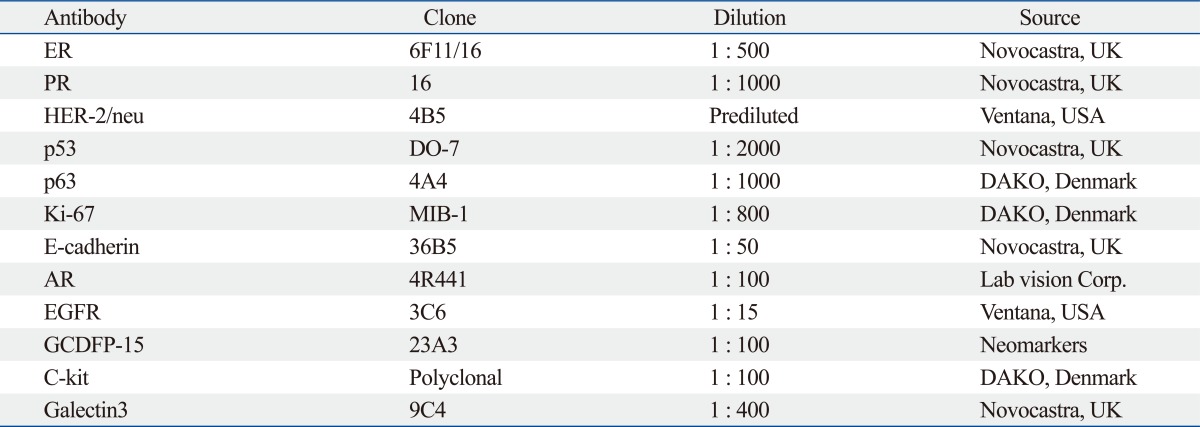
Immunohistochemical (IHC) staining
The antibodies used to conduct this study are listed in Table 3. Paraffin blocks were sectioned to a thickness of 4 um and tissues were attached on silane coated slides. The slides were baked at 60℃ for 60 minutes and washed in xylene for deparaffinization. For hydration of sections, the slides were bathed in gradient alcohol and distilled water. The antigen retrieval step was followed by boiling slides in 10 mM citrate buffer (pH6.0) for 10 minutes. Afterwards, the slides were immersed in 3% H2O2 for 15 minutes to block intrinsic hydro-peroxidase activity. The slides were incubated with primary antibodies for 2 hours at room-temperature, followed by incubation with secondary antibody (Enzyme-conjugated polymer, EnVision Detection kit, Denmark) for 15 minutes at room-temperature. A NovaRED substrate kit (VECTOR Laboratory, Burlingame, CA, USA) was applied to develop color following the manufacture's protocol. Harris hematoxylin was used for counter staining.
Table 3.
Antibodies Used in This Study
ER, estrogen receptor; PR, progesterone receptor; AR, androgen receptor; EGFR, epidermal growth factor receptor; GCDFP-15, gross cystic disease fluid protein 15.
Interpretation of immunohistochemical staining
IHC slides were evaluated by light microscopy. The scoring intensity of IHC staining was based on a three-grade system; 1 positive (weak), 2 positive (intermediate) and 3 positive (strong). The grade intensity of positive stainig was assessed as follows; nuclear positivity for ER, PR, androgen receptor (AR), p53, p63, and ki-67; cytoplasmic positivity for gross cystic disease fluid protein 15 (GCDFP-15); nuclear and cytoplasmic positivity for c-kit and galectin3; and cytoplasmic membrane positivity for c-erbB2, e-cadherin, and epidermal growth factor receptor (EGFR). Additionally, a proportional index was evaluated to describe the percentage of positivity for a few of the antibodies, including hormone receptors (ER, PR, and AR) and p53.
RESULTS
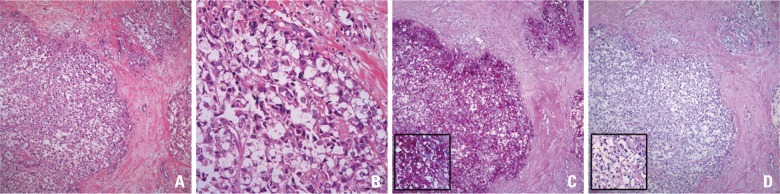
Three patients were diagnosed with invasive glycogen rich clear cell carcinoma from 2000 to 2011 at our institution. On gross examination, GRCCs appeared as well-circumscribed, irregular and solid masses. No difference was found in comparison to conventional invasive ductal carcinoma. Microscopically, GRCCs consisted of solid nests of clear cells with fine meshwork vasculatures. The individual cancer cells showed clear cytoplasm with fine granules and relatively low nuclear and cytoplasmic ratio. Nuclei were somewhat wrinkled. Nuclear membranes were irregularly thickened and their nucleoli were prominent. All of them contained PAS positive and d-PAS labile granules in the cytoplasm of more than 90% of tumor cells (Fig. 1). Mucin was not detected upon alcian blue and mucicarmin staining. Tests for GCDFP-15 were negative. The tumors were, therefore, considered to involve no apocrine differentiation.
Fig. 1.
Histologic features of GRCC. (A) Tumor shows solid nests of clear cells with fine meshwork vasculatures (×100). (B) The individual cancer cells have clear cytoplasm with fine granules, low N-C ratio, wrinkled nuclei, and prominent nucleoli (×400). (C) The granules in tumor cells are stained with PAS (×400 and ×1000 in box). (D) The granules are not stained with d-PAS (×400 and ×1000 in box). GRCC, glycogen rich clear cell carcinoma; PAS, periodic acid stain.
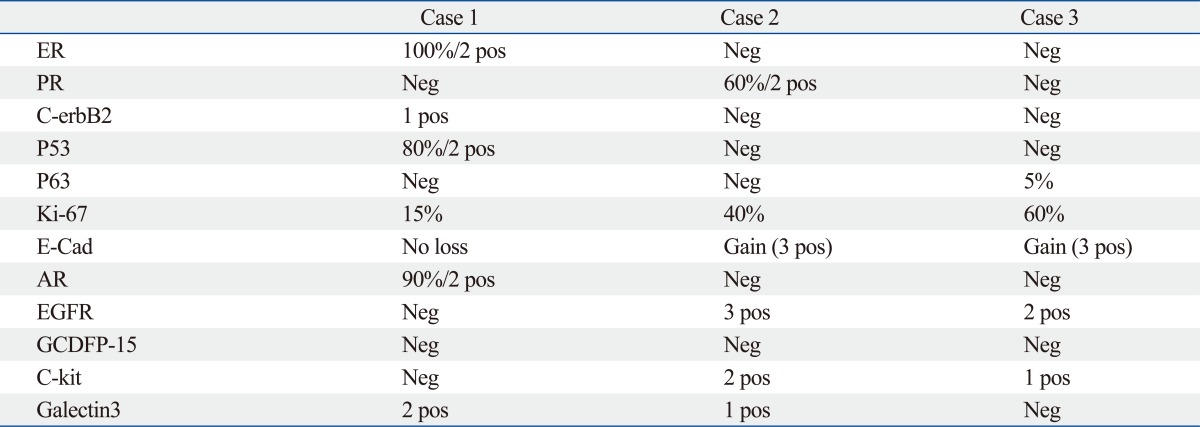
The three cases revealed three different immuno-phenotypes (Table 4). Case 1 showed positivity for ER and negativity for PR. Case 2 was positive for PR, but negative for ER. Case 3 presented with triple negative invasive carcinoma. All three cases were negative for c-erbB2. Androgen receptor was positive in the ER positive case 1. EGFR, E-cadherin, and CD117 (c-kit) showed positivity in two cases (cases 2 and 3). Among these three cases, p53-positive case exhibited a low proliferative index (ki-67: 15%), while p53-negative cases showed high proliferative index (ki-67: 50-60%).
Table 4.
Immunophenotypes of GRCC
ER, estrogen receptor; PR, progesterone receptor; E-Cad, E-cadherin; AR, androgen receptor; EGFR, epidermal growth factor receptor; GCDFP-15, gross cystic disease fluid protein 15; pos, positive; neg, negative.
DISCUSSION
GRCC is a very rare entity that exhibits distinctive clear cells with intracytoplasmic glycogen. However, no trials have been conducted to reveal the distinct characteristics of GRCC, including clinical behavior, biologic features, immunophenotypes, and genetics.2-6,8
Because of the rarity, we accumulated only three cases of GRCC out of more than 2000 cases of carcinoma over the last 10 years. Twelve different antibodies were evaluated in the three cases, the immunophenotypes of which prove not to be uniform. Based on immuno-scoring, we were able to characterize the expression patterns of targeted proteins into three groups. The first group of proteins shared the same immuno-scoring and were related to cell surface molecules, including EGFR, c-kit, and E-cadherin. The second group was related to hormone receptors, including ER and AR. The third group was characterized by p53 related proliferation.
EGFR and c-kit are both cell surface receptors important to the PI3K through AKT and RAS to MAPK signal transduction pathways, and have been shown to be involved in cell survival and proliferation,9,10 Double expression of EGFR and c-kit in breast carcinoma is known as a predictive marker of poor prognoses.11 Among our cases, ki-67, marker of cell proliferation, was also synchronously up-regulated along with up-regulation of EGFR and c-kit. Taken together, in predicting poor prognoses, expression of both EGFR and c-kit sould be associated with high mitotic index. In our GRCC cases, case 1 was both EGFR and c-kit negative with a low mitotic index, while the other two (cases 2 and 3) were positive for both with a high mitotic index. The expression pattern of EGFR and c-kit was concordant with E-cadherin and discordant with ki-67. Most studies on E-cadherin have focused on lobular carcinoma.12 The role of E-cadherin in ductal carcinoma is still unknown. The function of E-cadherin is considered related with cell adhesion molecules; thus, loss of expression would be associated with a high incidence of invasion and metastasis. A few researchers stated that up-regulation of E-cadherin would be associated with a better prognosis in invasive ductal carcinoma.13 However, the mechanism is unclear.
P53 is a well known nuclear protein that participates in cell proliferation. In benign conditions, p53 is not detectable by IHC staining. Cancer progression demonstrates accumulations of non-functional and non-degraded p53 protein in nuclei, resulting in immuno-positivity of p53 protein. Mutated p53 protein cannot suppress genetic errors leading to cancer development. Nevertheless, p53 over-expression has been considered a poor prognostic marker and accompanied by a high mitotic index in invasive ductal carcinoma.14 Our three cases demonstrate just the opposite. Case 1 showed strong positivity for p53 with low mitotic index, while cases 2 and 3 showed negativity for p53 with high mitotic index. These findings support the possibility of an association of cell proliferation with the signal transduction of surface molecules (EGFR, c-kit and E-cadherin), not with mutation of p53 protein, in GRCC.
Case 3 presented as a triple negative carcinoma and also expressed p63 protein. Case 3 was a basal-like breast cancer and was predicted to involve a poor prognosis. Increased proliferative activity as determined by ki-67 (60%) and over-expression of EGFR supported the possibility of a poor prognosis. The diagnosis of this case was confirmed only 3 months prior to the preparation of this manuscript; therefore, follow up data are currently not available. Based on IHC results, this case will require continued attention for future treatment. Presently, researchers agree that if GRCC is comparable to the conventional ductal carcinoma of the same TNM stage, the prognosis of the two types of carcinomas would be the same.7
As only three cases were available for study, the drawing of any conclusions would be limited. However, these cases did reveal different IHC characteristics for GRCC. We believe that the cases presented herein substantiate a need to re-examine the general features of GRCC. While the immunophenotypes of GRCC were not uniform, they appeared to be very similar to conventional ductal carcinoma.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Hull MT, Priest JB, Broadie TA, Ransburg RC, McCarthy LJ. Glycogen-rich clear cell carcinoma of the breast: a light and electron microscopic study. Cancer. 1981;48:2003–2009. doi: 10.1002/1097-0142(19811101)48:9<2003::aid-cncr2820480916>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 2.Hull MT, Warfel KA. Glycogen-rich clear cell carcinomas of the breast. A clinicopathologic and ultrastructural study. Am J Surg Pathol. 1986;10:553–559. doi: 10.1097/00000478-198608000-00005. [DOI] [PubMed] [Google Scholar]
- 3.Toikkanen S, Joensuu H. Glycogen-rich clear-cell carcinoma of the breast: a clinicopathologic and flow cytometric study. Hum Pathol. 1991;22:81–83. doi: 10.1016/0046-8177(91)90066-x. [DOI] [PubMed] [Google Scholar]
- 4.Fisher ER, Tavares J, Bulatao IS, Sass R, Fisher B. Glycogen-rich, clear cell breast cancer: with comments concerning other clear cell variants. Hum Pathol. 1985;16:1085–1090. doi: 10.1016/s0046-8177(85)80175-1. [DOI] [PubMed] [Google Scholar]
- 5.Hayes MM, Seidman JD, Ashton MA. Glycogen-rich clear cell carcinoma of the breast. A clinicopathologic study of 21 cases. Am J Surg Pathol. 1995;19:904–911. doi: 10.1097/00000478-199508000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Kuroda H, Sakamoto G, Ohnisi K, Itoyama S. Clinical and pathological features of glycogen-rich clear cell carcinoma of the breast. Breast Cancer. 2005;12:189–195. doi: 10.2325/jbcs.12.189. [DOI] [PubMed] [Google Scholar]
- 7.Varga Z, Zhao J, Ohlschlegel C, Odermatt B, Heitz PU. Preferential HER-2/neu overexpression and/or amplification in aggressive histological subtypes of invasive breast cancer. Histopathology. 2004;44:332–338. doi: 10.1111/j.1365-2559.2004.01843.x. [DOI] [PubMed] [Google Scholar]
- 8.Akbulut M, Zekioglu O, Kapkac M, Erhan Y, Ozdemir N. Fine needle aspiration cytology of glycogen-rich clear cell carcinoma of the breast: review of 37 cases with histologic correlation. Acta Cytol. 2008;52:65–71. doi: 10.1159/000325436. [DOI] [PubMed] [Google Scholar]
- 9.Sutton LM, Han JS, Molberg KH, Sarode VR, Cao D, Rakheja D, et al. Intratumoral expression level of epidermal growth factor receptor and cytokeratin 5/6 is significantly associated with nodal and distant metastases in patients with basal-like triple-negative breast carcinoma. Am J Clin Pathol. 2010;134:782–787. doi: 10.1309/AJCPRMD3ARUO5WPN. [DOI] [PubMed] [Google Scholar]
- 10.De Miguel MP, Cheng L, Holland EC, Federspiel MJ, Donovan PJ. Dissection of the c-kit signaling pathway in mouse primordial germ cells by retroviral-mediated gene transfer. Proc Natl Acad Sci U S A. 2002;99:10458–10463. doi: 10.1073/pnas.122249399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nalwoga H, Arnes JB, Wabinga H, Akslen LA. Expression of EGFR and c-kit is associated with the basal-like phenotype in breast carcinomas of African women. APMIS. 2008;116:515–525. doi: 10.1111/j.1600-0463.2008.01024.x. [DOI] [PubMed] [Google Scholar]
- 12.Koo JS, Jung W. Clinicopathlogic and immunohistochemical characteristics of triple negative invasive lobular carcinoma. Yonsei Med J. 2011;52:89–97. doi: 10.3349/ymj.2011.52.1.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mahler-Araujo B, Savage K, Parry S, Reis-Filho JS. Reduction of E-cadherin expression is associated with non-lobular breast carcinomas of basal-like and triple negative phenotype. J Clin Pathol. 2008;61:615–620. doi: 10.1136/jcp.2007.053991. [DOI] [PubMed] [Google Scholar]
- 14.Petitjean A, Achatz MI, Borresen-Dale AL, Hainaut P, Olivier M. TP53 mutations in human cancers: functional selection and impact on cancer prognosis and outcomes. Oncogene. 2007;26:2157–2165. doi: 10.1038/sj.onc.1210302. [DOI] [PubMed] [Google Scholar]