Abstract
Acute generalized exanthematous pustulosis (AGEP) is a pustular eruption, mainly drug induced often accompanied by fever and neutrophilic leukocytosis presenting as scarlatiniform erythema over the flexures evolving into numerous tiny non follicular pustules. We present a case report of a 56-year old woman, who had undergone mastectomy, treated with lapatinib for metastatic disease, and who presented with multiple erythematous papules and plaques with peripheral pustules. She also developed painful pyogenic granuloma-like lesions over the pulp of toe and over the proximal nail folds.All the lesions subsided following withdrawal of lapatinib. Although AGEP has been reported with imatinib (a multikinase inhibitor), there have been no reports of serious reactions with lapatinib, an EGFR inhibitor. This case could represent the first case report of AGEP to the EGFR inhibitor, lapatinib.
Keywords: Lapatinib, acute generalized exanthematous pustulosis, epidermal growth factor receptor inhibitor, pyogenic granuloma-like lesion
INTRODUCTION
Acute generalized exanthematous pustulosis (AGEP) is a pustular eruption, mainly drug induced, often accompanied by fever and neutrophilic leukocytosis appearing as scarlatiniform erythema over the flexures evolving into numerous tiny non-follicular pustules. We report a case of AGEP to the epidermal growth factor receptor (EGFR) inhibitor, lapatinib.
CASE REPORT
A 56-year old woman presented with erythema, scaling and oozing from the flexures,and erythematous scaly papules and plaques over the back, trunk, thighs and forearms of 4-month duration [Figure 1]. She complained of generalized weakness and feverishness. The skin lesions had started gradually and increased in extent and intensity in the last 1 month. The face and seborrheic areas of the chest were spared. The periphery of the papules and plaques were studded with pustules [Figure 2]. Painful lesions resembling pyogenic granuloma were present over the pulp of the right toe and over the proximal nail folds of both thumbs [Figures 3 and 4]. She complained of breathlessness, weakness and feverishness inspite of the temperature being normal. In March 2008, she underwent left mastectomy for ductal carcinoma breast (HER-2 receptor 3+ - strongly positive) with supraclavicular metastasis detected in May 2009. She was treated for metastatic breast cancer with lapatinib and capecitabine. She developed the lesions described above two months after initiating treatment with the two drugs. Upon developing skin lesions, capecitabine was withdrawn but lapatinib was continued in view of metastatic disease. Her skin lesions progressively increased, with marked aggravation since 1 month. She had no personal or family history of psoriasis.
Figure 1.

Discrete and confluent scaly, erythematous papules over the back
Figure 2.

Scarlatiniform erythema of the flexures, with the periphery of the papules and plaques showing pustules
Figure 3.

Painful pyogenic granuloma-like lesions over the right toe
Figure 4.

Painful pyogenic granuloma-like lesions over the proximal nail folds of the thumbs
Clinically, pustular psoriasis and AGEP were considered in the differential diagnoses. Lapatinib was withheld for a week and she was treated with topical corticosteroids and antihistamines (amitryptiline) for the burning pain over the finger and toe pulps. She had relief of symptoms and the flexural lesions cleared. Investigations revealed anemia (Hb-9.6g %) and increased polymorphs (80%), total count- 10.3Χ10-3/΅L. There were no hepatic, renal or pulmonary side effects after initiation of therapy. Biopsy of the pustule and plaque revealed subcorneal and intraspinous collection of neutrophils with spongiosis, upper dermal edema, perivascular inflammatory cell infiltrate of neutrophils, lymphocytes and eosinophils, neutrophilic vasculitis and extravasation of RBC confirming AGEP [Figures 5 and 6]. She refused further testing - (patch testing and epicutaneous testing).
Figure 5.
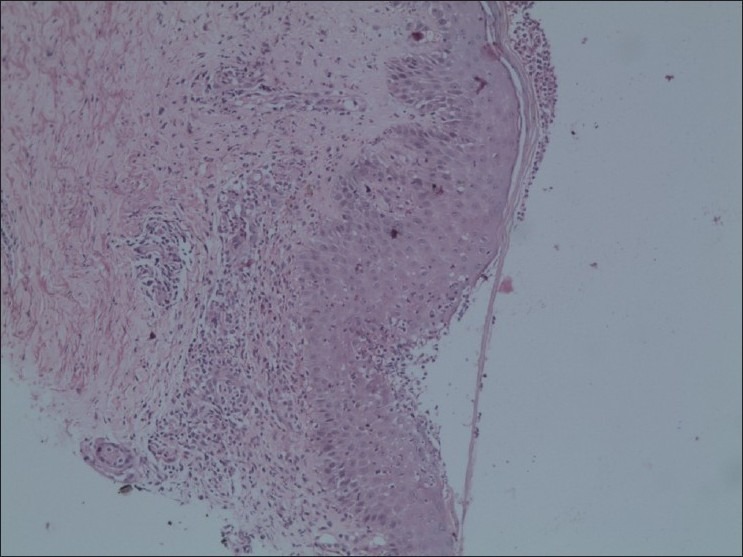
Subcorneal and intraspinous collection of neutrophils with spongiosis, upper dermal edema, perivascular inflammatory cell infiltrate of neutrophils, lymphocytes and eosinophils, neutrophilic vasculitis and extravasation of RBC (H&E, ×10)
Figure 6.

Dermis with vasculitis and extravasation of RBCs (H&E, ×40)
After the withdrawal of lapatinib, lesions showed clearing, but she was advised by the oncologist to restart the medication at a lower dose (from 1250 to 750 mg). As lapatinib was reintroduced while lesions were clearing, they recurred on restarting lapatinib but were less severe. Systemic prednisolone 30 mg/day, tapered to 10 mg/day over a month, was administered to control the reaction and she was reasonably controlled with this maintenance dose 1 month later, but for erythema and few lesions over the flexures [Figure 7]. Her breathlessness and feverishness subsided and the pyogenic granuloma-like lesions over the proximal nail folds and over the pulp of the toe showed signs of resolution [Figures 8 and 9]. She subsequently stopped the medication on her own and achieved complete clearance of the erythema. The pyogenic-granuloma-like lesions resolved completely. There was no recurrence of any skin lesions 6 months after stopping lapatinib.
Figure 7.

Skin lesions resolving after withdrawal of lapatinib and institution of systemic corticosteroids
Figure 8.

Lesion over the pulp of right toe showing resolution
Figure 9.

Resolution of lesions over the proximal nail folds
DISCUSSION
Lapatinib is an oral dual kinase inhibitor belonging to the EGFR antagonist group of drugs targeting both the ErbB1 and ErbB2 receptors. Epidermal growth factor receptor or ErbB1 is a member of the ErbB family is a 170-kd transmembrane protein with an extracellular ligand-binding domain and an intracellular protein tyrosine kinase. Upon ligand binding, the phosphorylated protein kinase activates a signal transduction pathway regulating proliferation, differentiation, migration and apoptosis of cells.[1]
ErbB1 (or HER-1) is overexpressed in 27-30% of breast tumors and ErbB2 (or HER-2) is overexpressed in 20-25% of breast cancers.[2] Lapatinib, a dual tyrosine kinase inhibitor has shown efficacy in breast cancer and as a result its use has been approved, in combination with capecitabine, for the treatment of disease positive for the human EGFR.[3] Our patient showed strong positivity of 3+ for ErbB2 receptors.
The most frequent adverse effects of lapatinib include diarrhea, rash, nausea and fatigue. The skin rash is characterized by papules and pustules over the face, chest and back resembling folliculitis or an acneiform drug eruption.[2] This appears within 1 and 3 weeks of treatment and peaks at about the fifth week, subsiding within 4 weeks of withdrawal of treatment.[1,2] Dermatologic adverse reactions to EGFR inhibitors include follicular or pustular lesions, painful periungual granulation-type or friable pyogenic granuloma-like changes, fissures of the lateral nail folds and/or distal finger tufts, hair changes, dry skin, hypersensitivity reactions and mucositis.[1] Our patient had non-follicular pustules and scarlatiniform erythema and scaling with marked accentuation over the flexures, with sparing of the face and seborrheic areas clinically suggestive of AGEP which was confirmed by histopathology. The skin rash associated with the skin toxicity of EGFR inhibitors is follicular and involves the face and seborrheic areas. The painful pyogenic granuloma-like lesions of the proximal nail folds and finger pulp are possibly related to the skin toxicity of lapatinib also described with other EGFR inhibitors.[1] Pustular psoriasis was considered in the differential diagnosis, but the presence of eosinophils in addition to intraspinous collections of neutrophils and the rapid clearance of lesions after withdrawal of lapatinib, and recurrence after reintroduction favored the diagnosis of AGEP.[4] Also after lapatinib was stopped by the patient on her own there was complete clearance of lesions with no recurrence after 6 months. Leucocytoclastic vasculitis is also reported in a few cases of AGEP and is not seen in pustular psoriasis.[4] Serious adverse skin reactions like Stevens-Johnson syndrome and AGEP have been reported with imatinib, a multikinase inhibitor which is a first-line therapy for chronic myeloid leukemia.[5] To date, four cases of imatinib-induced AGEP have been described and in one patient this been referred to as "scarlatiniform erythema with non-follicular pustules confined to flexural areas."[6,7] Another patient had "fever, exfoliative dermatitis, and non-follicular pustules."[8] All these patients developed the eruption within 1-3 months after the start of imatinib therapy. Imatinib induces AGEP via inhibition of tyrosine kinases by a mechanism similar to that seen in mercury-induced AGEP.[6] Capecitabine is a prodrug that is metabolized to 5-fluorouracil (5-FU). Cardiotoxicity is the commonest adverse effect. Extensive literature search has not revealed capecitabine to cause AGEP.
Signal transduction inhibitors are new chemotherapeutic agents in cancer therapy. There are two categories, EGFR receptor inhibitors and multikinase inhibitors. Various adverse reactions have been reported with multikinase inhibitors, whereas reported reactions to EGFR inhibitors have been comparatively milder. Although AGEP has been reported with imatinib (a multikinase inhibitor), there have been no reports of serious reactions with lapatinib, an EGFR inhibitor. This case could represent the first case report of AGEP to the EGFR inhibitor, lapatinib.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Agero AL, Dusza SW, Benvenuto-Andrade C, Busam KJ, Myskowski P, Halpern AC. Dermatologic side effects associated with the epidermal growth factor receptor inhibitors. J Am Acad Dermatol. 2006;55:657–70. doi: 10.1016/j.jaad.2005.10.010. [DOI] [PubMed] [Google Scholar]
- 2.Moy B, Goss PE. Lapatinib-associated toxicity and practical management recommendations. Oncologist. 2007;12:756–65. doi: 10.1634/theoncologist.12-7-756. [DOI] [PubMed] [Google Scholar]
- 3.Gasent Blesa JM, Canales JL, Candel A. One year of complete clinical response in a metastatic breast cancer patient treated with a combination of lapatinib and gemcitabine. Curr Oncol. 2010;17:64–8. doi: 10.3747/co.v17i2.422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Weedon D, Strutton G. Skin Pathology. In: Weedon D, Strutton G, editors. Acute generalized exanthematous pustulosis. 2nd ed. Churchill-Livingstone: Edinburgh; 2002. pp. 136–7. [Google Scholar]
- 5.Heidary N, Naik H, Burgin S. Chemotherapeutic agents and the skin: an update. J Am Acad Dermatol. 2008;58:545–70. doi: 10.1016/j.jaad.2008.01.001. [DOI] [PubMed] [Google Scholar]
- 6.Brouard MC, Prins C, Mach-Pascual S, Saurat JH. Acute generalized exanthematous pustulosis associated with ST1571 in a patient with chronic myeloid leukemia. Dermatology. 2001;203:57–9. doi: 10.1159/000051705. [DOI] [PubMed] [Google Scholar]
- 7.Schwarz M, Kreuzer KA, Baskaynak G, Dφrken B, le Coutre P. Imatinib-induced acute generalized exanthematous pustulosis (AGEP) in two patients with chronic myeloid leukemia. Eur J Haematol. 2002;69:254–6. doi: 10.1034/j.1600-0609.2002.02830.x. [DOI] [PubMed] [Google Scholar]
- 8.Valeyrie L, Bastuji-Garin S, Revuz J, Bachot N, Wechsler J, Berthaud P, et al. Adverse cutaneous reactions to imatinib (ST1571) in Philadelphia chromosome-positive leukemias: A prospective study of 54 patients. J Am Acad Dermatol. 2003;48:201–6. doi: 10.1067/mjd.2003.44. [DOI] [PubMed] [Google Scholar]


