Abstract
It is now well known that tumor immunosurveillance contributes to the control of cancer growth. Many mechanisms can be used by cancer cells to avoid the antitumor immune response. One such mechanism relies on the capacity of cancer cells or more generally of the tumor microenvironment to generate adenosine, a major molecule involved in antitumor T cell response suppression. Adenosine is generated by the dephosphorylation of extracellular ATP released by dying tumor cells. The conversion of ATP into adenosine is mediated by ectonucleotidase molecules, namely, CD73 and CD39. These molecules are frequently expressed in the tumor bed by a wide range of cells including tumor cells, regulatory T cells, Th17 cells, myeloid cells, and stromal cells. Recent evidence suggests that targeting adenosine by inhibiting ectonucleotidases may restore the resident antitumor immune response or enhance the efficacy of antitumor therapies. This paper will underline the impact of adenosine and ectonucleotidases on the antitumor response.
1. Introduction
Tumor immunology is an intensely investigated field of research, even though its clinical applications in the field of cancer treatment are currently limited. It is now well established that the molecular mechanisms leading to cell transformation and cancer generation induce the appearance of neoantigens and danger signals. These molecules give rise to the immune response which drives tumor rejection (a phenomenon called immunosurveillance), but some cancer cells escape this rejection by limiting tumor antigen expression (a phenomenon called immunoediting) mainly by inducing active immune tolerance mechanisms [1]. These mechanisms include the proliferation and local accumulation of immunosuppressive cells, including regulatory T cells (Tregs), Th17 cells, and myeloid-derived immunosuppressive cells (MDSCs). This tolerance (a phenomenon called immunoescape) prevents cancer rejection by the immune system and blunts the efficacy of immunotherapy [2]. All these events have been clearly demonstrated in mice models for years.
In humans, recent data demonstrate that infiltration of the tumor bed by CD8 and memory T cells correlates with good outcomes, while tumor-bed infiltration by immunosuppressive cells correlates with poor outcomes [3–5]. Such data raise the hypothesis that the immune response also controls tumor growth in humans. We may wonder whether therapies that shift immune tolerance towards the antitumor immune response could lead to tumor eradication. Chemotherapies such as cyclophosphamide, 5-Fluoro ruracil, and gemcitabine [6–9] by their capacity to eliminate immunosuppressive cells such as Tregs and MDSCs can restore the antitumor immune response. On the other hand, it is now widely accepted that the antitumor efficacy of many chemotherapy drugs is in part due to their induction of antitumor immune responses [10–12]. In addition, drugs, like anti-CTLA-4 mAb and anti-PD1 mAb, that directly target immune suppression, have either been approved by FDA or are under clinical investigation in many cancer types with very impressive clinical results [13].
Many strategies are currently used to target immune suppression. One is to target adenosine (a purine nucleoside) or enzymes that catalyze the generation of adenosine, namely, ectonucleotidase molecules CD39 and CD73. In this paper, we will propose a synthetic focus on the impact of this pathway on the antitumor immune response and its therapeutic potential. For this, we will describe not only the effect of adenosine on cancer cells, immune cells, and endothelial cells, but also how adenosine is produced by ectonucleotidase expressing cells.
2. Effect of Adenosine in the Context of Cancer
Adenosine is constitutively present in the extracellular media at a very low concentration, but its concentration increases in many metabolically stressful conditions, notably in the tumor microenvironment [14, 15]. Following its release, adenosine binds to membranous adenosine receptors, which belong to a family of G-protein-coupled receptors [16]. This family is composed of four different members called adenosine A1, A2A, A2B, and A3 receptors, which mediate different cellular pathways through adenosine binding. A1 and A3 receptors induce a decrease in intracellular cAMP, while A2A and A2B receptors induce activation of adenylate cyclase resulting in increased intracellular levels of cAMP. A1 and A3 receptors also induce the activation of phosphatidyl-Inositol 3 kinase (PI3K) and protein kinase C (PKC). At low concentrations of adenosine, only high-affinity A1, A2A, and A3 receptors are involved, whereas at high concentrations, like those observed in the tumor microenvironment, the low-affinity A2B receptor is involved in the signaling [17].
Because adenosine receptors are widely expressed, adenosine can influence immune, cancer, and endothelial cell functions (Figure 1).
Figure 1.
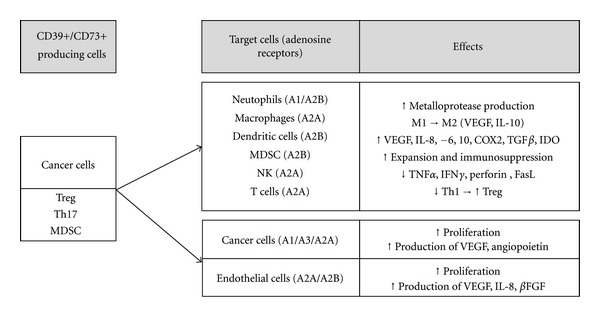
Effects of adenosine produced by CD39+/CD73+ cells on target cells. Cancer cells, Tregs, Th17, and MDSCs could produce adenosine through degradation of ATP/ADP by CD39 and CD73. Then adenosine binds on target cells, such as immune cells, cancer cells, or endothelial cells and modifies their activity.
2.1. Adenosine and Its Effect on the Immune System
Taking into account the different affinities between adenosine and its receptors and the fact that adenosine receptors are differentially expressed depending on the cell type, adenosine has the ability to act variably on immune cells. Adenosine binding to A1 or A2B receptors on neutrophils thus induces their activation, promotes their inflammatory activity, and induces chemotaxis and adherence of neutrophils to endothelial cells. In the context of cancer, neutrophil activation may be deleterious notably because neutrophils are able to produce metalloproteases, which foster matrix modification and promote metastases. Neutrophils can also promote chronic inflammation, which promotes tumor growth [18, 19].
Macrophages are also affected by adenosine. A2A receptor activation switches macrophages from an M1- to an M2-like phenotype. This switch needs the previous activation of macrophages by TLR (toll-like receptor) agonists to upregulate the A2A receptor. This event enhances the capacity of macrophages to produce VEGF (vascular endothelial growth factor) and IL-10, two cytokines that promote tumor growth [20].
Adenosine has been shown to promote MDSC functions in an A2B receptor-dependent manner. Indeed, adenosine leads to MDSC expansion and may promote tumor tolerance in this way [21].
Adenosine could act on the A2A receptor of natural killer (NK) cells and could blunt their capacity to produce tumor necrosis factor-α (TNF-α) and interferon-γ (IFN-γ) [22]. In addition, increased levels of adenosine in the tumor microenvironment inhibit the lytic activity of NK cells in an A2A receptor-dependent manner [23]. Adenosine also inhibits both perforin and FasL cytotoxic molecules, thus, limiting the ability of NK cells to mediate the lysis of tumor cells. Adenosine could also modify NKT cell response by increasing their production of IL-4 and transforming growth factor-β (TGF-β), while decreasing their production of IFN-γ [24].
Dendritic cells (DCs) are a critical component of the immune response and are aimed at controlling T-cell polarization. During tumor growth, DCs invade the tumor bed and differentiate under hypoxic and inflamed conditions. In this context, DCs are in contact with high concentrations of adenosine. The stimulation of adenosine receptors skews DC differentiation towards a distinct cell population characterized by the expression of both DC and macrophage cell surface markers. Pharmacologic analysis identified the A2B receptor as the mediator of adenosine's effects on DCs. Unlike normal myeloid DCs, adenosine-differentiated DCs have impaired allostimulatory activity and express high levels of angiogenic, proinflammatory, immune suppressor, and tolerogenic factors, including VEGF, IL-8, IL-6, IL-10, Cyclo-Oxygenase-2 (COX-2), TGF-β, and Indoleamine 2,3-dioxygenase (IDO) [25]. In addition, they promote tumor growth in mice. However, the overall effect of A2B activation on DCs is not fully understood because some other reports suggest that adenosine could increase IL-6 production and favor Th17 responses [26].
Adenosine could also have a major impact directly on T cell subsets. Signaling through the TCR (T cell receptor) causes a rapid increase in A2A receptor mRNA levels, which correlate with a significant increase in cAMP accumulation in these cells [27]. In vitro, antigen recognition in the setting of A2A receptor activation by specific agonists induces T-cell anergy, even in the presence of costimulation such as CD28 triggering [28]. T cells initially stimulated in the presence of an A2A receptor agonist also fail to proliferate and to produce IL-2 and IFN-γ after restimulation. Engagement of an A2A receptor in vivo inhibits IL-6 expression while enhancing the production of TGF-β. TGF-β in the absence of IL-6 promotes the differentiation of naive T cells into Treg cells. Consequently, treating mice with adenosine agonists not only inhibits Th1 effector cell generation but also promotes the generation of Tregs [28]. In conclusion, exposure to adenosine during T cell activation promotes long-term T-cell anergy and the induction of Tregs, both of which lead to a drastically impaired antitumor immune response.
2.2. Effects of Adenosine on Cancer Cells
Adenosine may affect cancer growth through direct binding on its specific receptors expressed at the cell surface of tumor cells (Figure 2). More particularly, A1 receptor is mainly involved in tumor cell proliferation and induces activation of the cell cycle. A1 receptor could inhibit p27, a molecule that promotes senescence and limits proliferation [29]. A3 receptor is expressed in many cancers and seems to be overexpressed in cancer cells compared with normal cells [30]. The major effect of A3 receptor activation is to promote angiogenesis. Adenosine, in an A3-dependent manner, increases hypoxia-inducible factor-1α (HIF-1α) protein expression in response to hypoxia in human melanoma, glioblastoma, and colon cancer cells [31–33]. Adenosine also mediates the production of VEGF and Angiopoietin by tumor cells in an A3-dependent manner [34]. Some reports have also demonstrated that human chronic lymphocytic leukemia (CLL) [35], myeloma [36] and melanoma cells [37] express functional A2A receptors. Activation of these receptors could modulate the response to chemotherapy. The A2A receptor also increases erythropoietin (EPO) production in hepatocellular carcinoma (Hep3B) cells [38].
Figure 2.
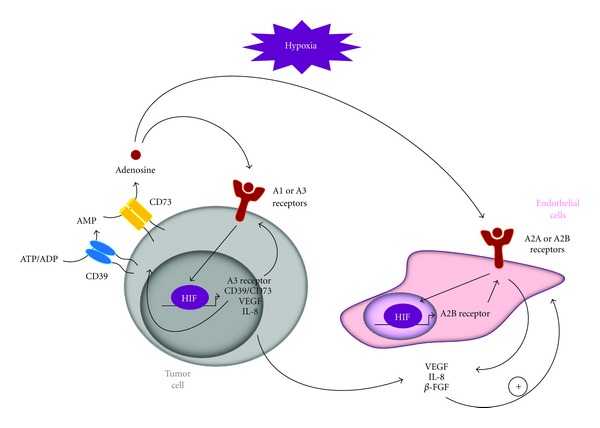
Hypoxia mediated expression of ectonucleotidases and adenosine receptors. HIF is induced under hypoxic conditions in cancer cells and directly increases the expression of (1) ectonucleotidases CD39 and CD73, which generate adenosine from ATP/ADP, (2) adenosine receptors that could, after binding of adenosine, activate HIF, and (3) angiogenic molecules VEGF and IL-8. These (again with β-FGF) also produced by endothelial cells (through binding of adenosine on specific receptors) could induce proliferation of these cells.
Adenosine does not always induce cancer cell proliferation; some reports mentioned that adenosine could also induce cancer cell death or inhibit cell proliferation [17].
2.3. Effects of Adenosine on Endothelial Cells
A2A and A2B receptors exert a strong proangiogenic effect. The A2A receptor is expressed by endothelial cells and is associated with vasodilation [39]. A2A mediates the production of VEGF and the proliferation of endothelial cells [40]. A2B receptors are expressed in human neoangiogenic endothelial cells, where they play a role in the regulation of the expression of angiogenic factors like VEGF, interleukin-8 (IL-8), and βFGF (basic fibroblast growth factor) [41, 42]. A2B receptors are also involved in mRNA and protein increases of IL-6 in human astrocytoma cells, thus, promoting STAT3 (Signal transducer and activator of transcription 3) mediated angiogenesis [43].
3. Production of Adenosine by Ectonucleotidases
The dominant pathway leading to extracellular adenosine production is the extracellular dephosphorylation of ATP by ectonucleotidases. This degradation requires two enzymes called CD39 (ectonucleoside triphosphate diphosphohydrolase 1-Entpd1) and CD73 (ecto-5′-nucleotidase-Nt5e). CD39 hydrolyzes ATP and ADP to AMP, which is further hydrolyzed to adenosine by CD73. The conversion of ATP into AMP by CD39 is reversible by the action of extracellular kinases such as adenylate kinase. By contrast, the conversion of AMP into adenosine by CD73 is reversible only after the transport of adenosine into cells where it can be converted into AMP by adenosine kinase. CD39 is expressed on endothelial cells [44] and on many types of activated hematopoietic cells such as B cells, NK cells, and activated T cell subsets and also on monocytes/macrophages and dendritic cells [45, 46]. CD39 degrades ATP produced by activated platelets and thus inhibits the generation of thrombi, and may act on tumor angiogenesis by this pathway [47]. CD39 expression on leukocytes is indispensable for the generation of adenosine and consequently dictates their immunosuppressive functions [48].
CD73 is considered the rate-limiting enzyme in the generation of extracellular adenosine [49]. CD73 catalyzes the dephosphorylation of purine and pyrimidine ribo- and deoxyribonucleoside monophosphates to the corresponding nucleosides. This molecule notably drives the conversion of AMP into adenosine. This antigen is expressed on some immune cells such as activated B but not on naive T cells [50, 51], endothelial cells [44], follicular dendritic cells [52], epithelial cells [53], and fibroblasts [54]. In the tumor microenvironment, CD73 expression is regulated by hypoxia [55–57]. In addition, some factors found in the tumor microenvironment such as TNF-α, IL-1β [58], prostaglandin E2 (PGE2) [59], TGF-β [60], and IL-6 [61] could also upregulate ectonucleotidase expression, whereas IFN-γ and IL-4 have been shown to downregulate CD73 expression [59, 62].
4. Expression and Role of Ectonucleotidases in Cancer
Many studies on CD39 or CD73-deficient animals have shown that the expression of ectonucleotidase on cancer cells and on host cells (hematopoietic and nonhematopoietic cells) is involved in tumor progression [63–68].
4.1. Effects and Expression of Ectonucleotidases on Cancer Cells
Ectonucleotidase expression has been observed in many human cancer types such as melanoma, breast cancer, colon cancer, glioma, leukemia, gastric, and head and neck cancers [69]. The prognostic role of ectonucleotidase expression in cancer cells remains largely unclear. In a small cohort of breast cancer patients, expression of CD73 in cancer cells seemed to correlate with survival [70]. In a cohort of colorectal cancer patients, high expression of CD73 was observed in about 50% of tumor samples and this overexpression correlated significantly with poor tumor differentiation, nodal status, and a high T stage. Overall survival in patients with high expression of CD73 was poorer than in patients with low expression of CD73 [71]. The expression of ectonucleotidases on chronic lymphocytic leukemia cells correlates with a better prognosis [72]. In another study, CD39 was found to be widely expressed in CLL lymph nodes, whereas CD73 is only expressed in proliferative centers. Ectonucleotidase-expressing LLC cells produce adenosine, which mediates drug-induced resistance via an AMPc-dependent autocrine loop [35].
For example, immunoediting may select cancer cells that highly express ectonucleotidases; that is, cells better armed to fight against the antitumor immune response. HIF induced under hypoxia could increase ectonucleotidase expression through direct binding on response elements located within the ectonucleotidase promoters [55].
Ectonucleotidase expression on tumor cells and on tumor exosomes (small vesicles secreted by cancer cells) may increase local concentrations of adenosine and could blunt the antitumoral immune response [73, 74]. Indeed, blockade of the A2A receptor on CD8 T cells inhibits the growth of strongly immunogenic melanomas [73]. A2B receptor blockade acts on DC subsets and enhances tumor Ag presentation and cytokine-mediated T cell activation [75].
Adenosine-receptor promoters contain an HIF-1α response element that drives expression of these receptors in hypoxic cells including endothelial cells [76], cancer cells [77], and DCs [78]. In fact, adenosine receptors have been found in many cancer types in mice and humans. Thus hypoxia induces a vicious circle involving the adenosine pathway, by enhancing the production of adenosine via the upregulation of both ectonucleotidases and adenosine receptors.
4.2. Ectonucleotidase Expression on Tregs
Tregs are one of the key immunosuppressive cells in the context of cancer. Regulatory T cells (Tregs) were initially identified in both mice and humans as CD4+ T cells constitutively expressing CD25 and inhibiting the immune response of effector T cells. In cancer-bearing animals or patients, Tregs expand, migrate to tumor sites, and suppress the antitumor immune response mediated by NK cells, CD4+, CD8+ T cells, and myeloid cells, through different molecular mechanisms [79]. In experimental tumor models as well as in cancer-bearing patients, the accumulation of Tregs generally progresses during tumor growth. Treg accumulation was first described among peripheral blood leukocytes in cancer-bearing patients [80], in the spleen of tumor-bearing rodents and also in the tumor itself [81], where a high infiltration of Tregs correlates with a poor prognosis in most cancer types [82]. Therefore, Tregs are usually considered a major cell population involved in immune tolerance, which protects cancer cells from antitumor immunity.
The mechanism of Treg-mediated immunosuppression remains unclear, and many mechanisms of action have been proposed. Recently, murine Tregs were shown to express membranous CD73 and CD39 and to be able to transform ATP into adenosine. Functionally, the coexpression of CD39 and CD73 with the pericellular generation of adenosine dictates the suppressive functions of Treg cells on A2A-positive effector T cells [83]. In humans, ectonucleotidases have also been observed on Tregs [84]. Tregs could be induced from naive T cells by TCR triggering in the presence of TGF-β. A recent report demonstrated that triggering of the TCR induced expression of CD39 and CD73 on these cells [60]. Finally CD39 expression on Tregs has also been shown to inhibit NK cell activity and to promote hepatic metastasis in a murine melanoma cancer model [64] and T cell anergy in human follicular lymphoma [85]. However, the molecular mechanism that leads to ectonucleotidase expression in Tregs and their role in the control of tumor growth remains unclear.
4.3. Ectonucleotidase Expression on Th17 Cells
Th17 cells are CD4+ T cells developed by TCR triggering with a combination of IL-6 and TGF-β. After induction, IL-23, an IL-12 family member, maintains Th17 cell polarization [86]. Th17 cells have emerged as key participants in a wide range of autoimmune disorders, including inflammatory bowel disease, psoriasis, and ankylosing spondylitis [87]. Th17 expansion has been shown in the blood, bone marrow, and spleen of tumor-bearing mice. Th17 cell expansion has also been observed in human cancers such as melanoma, prostate cancer, fibrosarcoma, andadvanced head and neck cancers [88–90], and Th17 infiltration is associated with a poor outcome in colon and liver cancers [91, 92]. The role of Th17 cells in cancer immunity remains controversial. Many reports have suggested that Th17 may promote tumor growth in mice and humans. IL-17 produced by Th17 has been shown to promote angiogenesis and inflammation through STAT3 signaling and MDSC mobilization [93, 94]. On the other hand, the adoptive transfer of tumor-specific Th17 cells could control tumor growth as a result of their ability to promote cytotoxic T cell activation [95, 96]. These studies suggest that Th17 cells may exert regulatory or inflammatory functions in the context of cancer depending on the cytokine microenvironment. Our recent work tried to reconcile these discrepancies. We made the seminal observation that in vitro Th17 cells generated with IL-6 and TGF-β express CD39 and CD73, while inflammatory Th17 cells generated with IL-6, IL-1β, and IL-23 do not. Ectonucleotidase expression on Th17 leads to adenosine release and the suppression of effector Tcells. The expression of ectonucleotidases was dependent on IL-6-driven STAT3 activation and TGF-β-mediated downregulation of zinc finger protein growth factor independent-1 (Gfi-1), both of which transcriptionally regulate ectonucleotidase expression during Th17 cell differentiation. Ectonucleotidase expression on Th17 cells is relevant in the context of tumor growth as wild-type Th17 cells promote tumor growth while Th17 cells obtained from CD39-deficient mice remain unable to affect tumor growth. Thus, our data suggest that the expression of ectonucleotidases dictates the immunosuppressive fate of Th17 cells in cancer [61].
4.4. Ectonucleotidase Expression on MDSCs
Myeloid-derived suppressor cells (MDSCs) have been identified in cancer patients and in tumor-bearing mice as a population of immature myeloid cells with the ability to suppress T cell activation. In mice, MDSCs are uniformly characterized by the expression of the cell-surface antigens Gr1, Ly-6C/G, and CD11b, while in humans, MDSCs are typically found in the Lin−CD11b+CD33+HLA-DR−subset. Given that MDSCs from naive mice were generally found to lack immunosuppressive properties, it has been shown that MDSCs require activation signals, such as cytokines or exosome membrane-bound Hsp72, from tumor cells to support their suppressive functions on T cells [97, 98].
Recently, Ryzhov et al. have shown that CD11b+Gr1high Ly-6G+ cells express high levels of CD73 at the cell surface. This correlates with high ecto-5′-nucleotidase enzymatic activity, which contributes to the expansion and the immunosuppressive properties of MDSCs [21]. The relevance of these observations in the control of tumor progression needs to be established.
5. Inhibition of Ectonucleotidase Activity as a Therapeutic Approach in Cancer
On the assumption that adenosine production promotes tumor proliferation, neoangiogenesis, and directly blunts antitumor effector cells, and that ectonucleotidases are highly expressed on tumor cells (and correlate with a poorer overall survival rate) and on immunosuppressive cells, it should be of great interest to inhibit the adenosine receptor on target cells or adenosine production by ectonucleotidases to promote the antitumor response.
Even though targeting adenosine receptors seems to be relevant, it could have an uncertain impact on tumor treatment. For example, it has been shown that targeting A2A receptors could dampen etoposide-mediated CLL cell death [35], while enhancing the effects of melphalan, lenalidomide, bortezomib, and doxorubicin on multiple myeloma [36].
Thus, targeting ectonucleotidase activity seems to be more appropriate. Inhibition of CD39 activity by polyoxometalate-1 (POM-1), a pharmacologic inhibitor of nucleoside triphosphate diphosphohydrolase activity, abrogated melanoma tumor growth in wild-type mice but not in CD39-null animals indicating a specific effect of POM-1 on host CD39 [64].
The inhibition of CD73 has been more thoroughly studied. A specific blocking antibody suppressed the growth of established 3-methylcholanthrene-induced tumors or prostate tumors and inhibited the development of lung metastases [99]. Moreover the inhibitor α,β-methyleneadenosine 5′-diphosphate (APCP) also affected thymoma or ovarian tumor growth and B16F10 lung metastasis formation [66–68].
Recent reports demonstrate that chemotherapies, in addition to their cytotoxic effects, mediate an immune effect via the release of ATP, emphasizing the importance of inhibiting ectonucleotidases [10, 100]. The use of ectonucleotidase inhibitors or blocking antibodies in association with chemotherapies that facilitate ATP production could thus be focused on patients with ectonucleotidase-overexpressing tumors. For this, patients should be screened for ectonucleotidase expression on cancer cells and on tumor infiltrating cells, and ATP producing chemotherapeutic drugs should be selected, notably thanks to the in vivo imaging method that allows the real-time measurement of ATP within the tumor interstitium developed by the Di Virgilio team [101].
6. Conclusion
Clear understanding of the mechanisms involved in tumor-induced tolerance is a capital objective to develop effective antitumor immunotherapies. It is clear that ectonucleotidase expression on cancer cells as well as immune cells that infiltrate the tumor bed facilitates tumor development. Adenosine production that results from the transformation of extracellular ATP by ectonucleotidases promotes tumor cell proliferation, neoangiogenesis and blunts antitumor effector cells. Thus a promising strategy to simultaneously reduce these effects would be to target ectonucleotidases using blocking antibodies or inhibitors of ectonucleotidases or adenosine receptors. This inhibition could be a new avenue to explore to improve the efficacy of classical cytotoxic agents by enhancing extracellular ATP levels which would sustain the antitumor immune response.
Acknowledgments
The authors thank P. Bastable for carefully reading the paper. F. Ghiringhelli was supported by ARC, FRM, INCA, and Ligue contre le Cancer, M. Bruchard by fellowships from the Ministère de l'Enseignement Supérieur et de la Recherche, F. Chalmin by fellowships from Ligue contre le cancer, and C. Rébé by Ligue contre le cancer comité Grand-Est.
References
- 1.Schreiber RD, Old LJ, Smyth MJ. Cancer immunoediting: integrating immunity’s roles in cancer suppression and promotion. Science. 2011;331(6024):1565–1570. doi: 10.1126/science.1203486. [DOI] [PubMed] [Google Scholar]
- 2.Mellman I, Coukos G, Dranoff G. Cancer immunotherapy comes of age. Nature. 2011;480(7378):480–489. doi: 10.1038/nature10673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pagès F, Berger A, Camus M, et al. Effector memory T cells, early metastasis, and survival in colorectal cancer. New England Journal of Medicine. 2005;353(25):2654–2666. doi: 10.1056/NEJMoa051424. [DOI] [PubMed] [Google Scholar]
- 4.Fridman WH, Pagès F, Sautès-Fridman C, Galon J. The immune contexture in human tumours: impact on clinical outcome. Nature Reviews Cancer. 2012;12(4):298–306. doi: 10.1038/nrc3245. [DOI] [PubMed] [Google Scholar]
- 5.Fridman WH, Galon J, Pagès F, Tartour E, Sautès-Fridman C, Kroemer G. Prognostic and predictive impact of intra- and peritumoral immune infiltrates. Cancer Research. 2011;71(17):5601–5605. doi: 10.1158/0008-5472.CAN-11-1316. [DOI] [PubMed] [Google Scholar]
- 6.Ghiringhelli F, Ménard C, Terme M, et al. CD4+CD25+ regulatory T cells inhibit natural killer cell functions in a transforming growth factor-β-dependent manner. Journal of Experimental Medicine. 2005;202(8):1075–1085. doi: 10.1084/jem.20051511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ghiringhelli F, Puig PE, Roux S, et al. Tumor cells convert immature myeloid dendritic cells into TGF-β-secreting cells inducing CD4+CD25+ regulatory T cell proliferation. Journal of Experimental Medicine. 2005;202(7):919–929. doi: 10.1084/jem.20050463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vincent J, Mignot G, Chalmin F, et al. 5-Fluorouracil selectively kills tumor-associated myeloid-derived suppressor cells resulting in enhanced T cell-dependent antitumor immunity. Cancer Research. 2010;70(8):3052–3061. doi: 10.1158/0008-5472.CAN-09-3690. [DOI] [PubMed] [Google Scholar]
- 9.Suzuki H, Takatsuka S, Akashi H, et al. Genome-wide profiling of chromatin signatures reveals epigenetic regulation of microRNA genes in colorectal cancer. Cancer Research. 2011;71(17):5646–5658. doi: 10.1158/0008-5472.CAN-11-1076. [DOI] [PubMed] [Google Scholar]
- 10.Ghiringhelli F, Apetoh L, Tesniere A, et al. Activation of the NLRP3 inflammasome in dendritic cells induces IL-1β-dependent adaptive immunity against tumors. Nature Medicine. 2009;15(10):1170–1178. doi: 10.1038/nm.2028. [DOI] [PubMed] [Google Scholar]
- 11.Apetoh L, Ghiringhelli F, Tesniere A, et al. Toll-like receptor 4-dependent contribution of the immune system to anticancer chemotherapy and radiotherapy. Nature Medicine. 2007;13(9):1050–1059. doi: 10.1038/nm1622. [DOI] [PubMed] [Google Scholar]
- 12.Zitvogel L, Apetoh L, Ghiringhelli F, Kroemer G. Immunological aspects of cancer chemotherapy. Nature Reviews Immunology. 2008;8(1):59–73. doi: 10.1038/nri2216. [DOI] [PubMed] [Google Scholar]
- 13.Pardoll DM. The blockade of immune checkpoints in cancer immunotherapy. Nature Reviews Cancer. 2012;12(4):252–264. doi: 10.1038/nrc3239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Martin DS, Bertino JR, Koutcher JA. ATP depletion + pyrimidine depletion can markedly enhance cancer therapy: fresh insight for a new approach. Cancer Research. 2000;60(24):6776–6783. [PubMed] [Google Scholar]
- 15.Sperlágh B, Erdélyi F, Szabó G, Vizi ES. Local regulation of [3H]-noradrenaline release from the isolated guinea-pig right atrium by P2X-receptors located on axon terminals. British Journal of Pharmacology. 2000;131(8):1775–1783. doi: 10.1038/sj.bjp.0703757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fredholm BB, Irenius E, Kull B, Schulte G. Comparison of the potency of adenosine as an agonist at human adenosine receptors expressed in Chinese hamster ovary cells. Biochemical Pharmacology. 2001;61(4):443–448. doi: 10.1016/s0006-2952(00)00570-0. [DOI] [PubMed] [Google Scholar]
- 17.Gessi S, Merighi S, Sacchetto V, Simioni C, Borea PA. Adenosine receptors and cancer. Biochimica et Biophysica Acta. 2011;1808(5):1400–1412. doi: 10.1016/j.bbamem.2010.09.020. [DOI] [PubMed] [Google Scholar]
- 18.Haskó G, Cronstein BN. Adenosine: an endogenous regulator of innate immunity. Trends in Immunology. 2004;25(1):33–39. doi: 10.1016/j.it.2003.11.003. [DOI] [PubMed] [Google Scholar]
- 19.Inoue Y, Chen Y, Pauzenberger R, Hirsh MI, Jnger WG. Hypertonic saline up-regulates A3 adenosine receptor expression of activated neutrophils and increases acute lung injury after sepsis. Critical Care Medicine. 2008;36(9):2569–2575. doi: 10.1097/CCM.0b013e3181841a91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Grinberg S, Hasko G, Wu D, Leibovich SJ. Suppression of PLCβ2 by endotoxin plays a role in the adenosine A2A receptor-mediated switch of macrophages from an inflammatory to an angiogenic phenotype. American Journal of Pathology. 2009;175(6):2439–2453. doi: 10.2353/ajpath.2009.090290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ryzhov S, Novitskiy SV, Goldstein AE, et al. Adenosinergic regulation of the expansion and immunosuppressive activity of CD11b+Gr1 + cells. Journal of Immunology. 2011;187(11):6120–6129. doi: 10.4049/jimmunol.1101225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Miller JS, Cervenka T, Lund J, Okazaki IJ, Moss J. Purine metabolites suppress proliferation of human NK cells through a lineage-specific purine receptor. Journal of Immunology. 1999;162(12):7376–7382. [PubMed] [Google Scholar]
- 23.Raskovalova T, Huang X, Sitkovsky M, Zacharia LC, Jackson EK, Gorelik E. GS protein-coupled adenosine receptor signaling and lytic function of activated NK cells. Journal of Immunology. 2005;175(7):4383–4391. doi: 10.4049/jimmunol.175.7.4383. [DOI] [PubMed] [Google Scholar]
- 24.Nowak M, Lynch L, Yue S, et al. The A2aR adenosine receptor controls cytokine production in iNKT cells. European Journal of Immunology. 2010;40(3):682–687. doi: 10.1002/eji.200939897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Novitskiy SV, Ryzhov S, Zaynagetdinov R, et al. Adenosine receptors in regulation of dendritic cell differentiation and function. Blood. 2008;112(5):1822–1831. doi: 10.1182/blood-2008-02-136325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wilson JM, Kurtz CC, Black SG, et al. The A2B adenosine receptor promotes Th17 differentiation via stimulation of dendritic cell IL-6. Journal of Immunology. 2011;186(12):6746–6752. doi: 10.4049/jimmunol.1100117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lappas CM, Sullivan GW, Linden J. Adenosine A2A agonists in development for the treatment of inflammation. Expert Opinion on Investigational Drugs. 2005;14(7):797–806. doi: 10.1517/13543784.14.7.797. [DOI] [PubMed] [Google Scholar]
- 28.Zarek PE, Huang CT, Lutz ER, et al. A2A receptor signaling promotes peripheral tolerance by inducing T-cell anergy and the generation of adaptive regulatory T cells. Blood. 2008;111(1):251–259. doi: 10.1182/blood-2007-03-081646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mirza A, Basso A, Black S, et al. RNA interference targeting of A1 receptor-overexpressing breast carcinoma cells leads to diminished rates of cell proliferation and induction of apoptosis. Cancer Biology and Therapy. 2005;4(12):1355–1360. doi: 10.4161/cbt.4.12.2196. [DOI] [PubMed] [Google Scholar]
- 30.Koscsó B, Csóka B, Pacher P, Haskó G. Investigational A3 adenosine receptor targeting agents. Expert Opinion on Investigational Drugs. 2011;20(6):757–768. doi: 10.1517/13543784.2011.573785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Merighi S, Benini A, Mirandola P, et al. Hypoxia inhibits paclitaxel-induced apoptosis through adenosine-mediated phosphorylation of bad in glioblastoma cells. Molecular Pharmacology. 2007;72(1):162–172. doi: 10.1124/mol.106.031849. [DOI] [PubMed] [Google Scholar]
- 32.Merighi S, Benini A, Mirandola P, et al. Adenosine modulates vascular endothelial growth factor expression via hypoxia-inducible factor-1 in human glioblastoma cells. Biochemical Pharmacology. 2006;72(1):19–31. doi: 10.1016/j.bcp.2006.03.020. [DOI] [PubMed] [Google Scholar]
- 33.Merighi S, Benini A, Mirandola P, et al. A3 adenosine receptors modulate hypoxia-inducible factor-1α expression in human A375 melanoma cells. Neoplasia. 2005;7(10):894–903. doi: 10.1593/neo.05334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Feoktistov I, Ryzhov S, Goldstein AE, Biaggioni I. Mast cell-mediated stimulation of angiogenesis: cooperative interaction between A2B and A3 adenosine receptors. Circulation Research. 2003;92(5):485–492. doi: 10.1161/01.RES.0000061572.10929.2D. [DOI] [PubMed] [Google Scholar]
- 35.Serra S, Horenstein AL, Vaisitti T, et al. CD73-generated extracellular adenosine in chronic lymphocytic leukemia creates local conditions counteracting drug-induced cell death. Blood. 2011;118(23):6141–6152. doi: 10.1182/blood-2011-08-374728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rickles RJ, Tam WF, Giordano TP, et al. Adenosine A2A and Beta-2 adrenergic receptor agonists: novel selective and synergistic multiple myeloma targets discovered through systematic combination screening. Molecular Cancer Therapeutics. 2012;11(7):1432–1442. doi: 10.1158/1535-7163.MCT-11-0925. [DOI] [PubMed] [Google Scholar]
- 37.Merighi S, Mirandola P, Milani D, et al. Adenosine receptors as mediators of both cell proliferation and cell death of cultured human melanoma cells. Journal of Investigative Dermatology. 2002;119(4):923–933. doi: 10.1046/j.1523-1747.2002.00111.x. [DOI] [PubMed] [Google Scholar]
- 38.Fisher JW, Brookins J. Adenosine A2A and A2B receptor activation of erythropoietin production. American Journal of Physiology. 2001;281(5):F826–F832. doi: 10.1152/ajprenal.2001.281.5.F826. [DOI] [PubMed] [Google Scholar]
- 39.Zatta AJ, Matherne GP, Headrick JP. Adenosine receptor-mediated coronary vascular protection in post-ischemic mouse heart. Life Sciences. 2006;78(21):2426–2437. doi: 10.1016/j.lfs.2005.09.035. [DOI] [PubMed] [Google Scholar]
- 40.Takagi H, King GL, Robinson GS, Ferrara N, Aiello LP. Adenosine mediates hypoxic induction of vascular endothelial growth factor in retinal pericytes and endothelial cells. Investigative Ophthalmology and Visual Science. 1996;37(11):2165–2176. [PubMed] [Google Scholar]
- 41.Iino M, Ehama R, Nakazawa Y, et al. Adenosine stimulates fibroblast growth factor-7 gene expression via adenosine A2B receptor signaling in dermal papilla cells. Journal of Investigative Dermatology. 2007;127(6):1318–1325. doi: 10.1038/sj.jid.5700728. [DOI] [PubMed] [Google Scholar]
- 42.Gessi S, Fogli E, Sacchetto V, et al. Adenosine modulates HIF-1α, VEGF, IL-8, and foam cell formation in a human model of hypoxic foam cells. Arteriosclerosis, Thrombosis, and Vascular Biology. 2010;30(1):90–97. doi: 10.1161/ATVBAHA.109.194902. [DOI] [PubMed] [Google Scholar]
- 43.Vazquez JF, Clement HW, Sommer O, Schulz E, Van Calker D. Local stimulation of the adenosine A2B receptors induces an increased release of IL-6 in mouse striatum: an in vivo microdialysis study. Journal of Neurochemistry. 2008;105(3):904–909. doi: 10.1111/j.1471-4159.2007.05191.x. [DOI] [PubMed] [Google Scholar]
- 44.Kas-Deelen AM, Bakker WW, Olinga P, et al. Cytomegalovirus infection increases the expression and activity of ecto-ATPase (CD39) and ecto-5′nucleotidase (CD73) on endothelial cells. FEBS Letters. 2001;491(1-2):21–25. doi: 10.1016/s0014-5793(01)02085-3. [DOI] [PubMed] [Google Scholar]
- 45.Kansas GS, Wood GS, Tedder TF. Expression, distribution, and biochemistry of human CD39: role in activation-associated homotypic adhesion of lymphocytes. Journal of Immunology. 1991;146(7):2235–2244. [PubMed] [Google Scholar]
- 46.Koziak K, Sévigny J, Robson SC, Siegel JB, Kaczmarek E. Analysis of CD39/ATP diphosphohydrolase (ATPDase) expression in endothelial cells, platelets and leukocytes. Thrombosis and Haemostasis. 1999;82(5):1538–1544. [PubMed] [Google Scholar]
- 47.Robson SC, Sévigny J, Zimmermann H. The E-NTPDase family of ectonucleotidases: structure function relationships and pathophysiological significance. Purinergic Signalling. 2006;2(2):409–430. doi: 10.1007/s11302-006-9003-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dwyer KM, Deaglio S, Gao W, Friedman D, Strom TB, Robson SC. CD39 and control of cellular immune responses. Purinergic Signalling. 2007;3(1-2):171–180. doi: 10.1007/s11302-006-9050-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Resta R, Yamashita Y, Thompson LF. Ecto-enzyme and signaling functions of lymphocyte CD73. Immunological Reviews. 1998;161:95–109. doi: 10.1111/j.1600-065x.1998.tb01574.x. [DOI] [PubMed] [Google Scholar]
- 50.Yang L, Kobie JJ, Mosmann TR. CD73 and Ly-6A/E distinguish in vivo primed but uncommitted mouse CD4 T cells from type 1 or type 2 effector cells. Journal of Immunology. 2005;175(10):6458–6464. doi: 10.4049/jimmunol.175.10.6458. [DOI] [PubMed] [Google Scholar]
- 51.Yamashita Y, Hooker SW, Jiang H, et al. CD73 expression and fyn-dependent signaling on murine lymphocytes. European Journal of Immunology. 1998;28(10):2981–2990. doi: 10.1002/(SICI)1521-4141(199810)28:10<2981::AID-IMMU2981>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 52.Airas L. CD73 and adhesion of B-cells to follicular dendritic cells. Leukemia and Lymphoma. 1998;29(1-2):37–47. doi: 10.3109/10428199809058380. [DOI] [PubMed] [Google Scholar]
- 53.Strohmeier GR, Lencer WI, Patapoff TW, et al. Surface expression, polarization, and functional significance of CD73 in human intestinal epithelia. Journal of Clinical Investigation. 1997;99(11):2588–2601. doi: 10.1172/JCI119447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Nemoto E, Kunii R, Tada H, Tsubahara T, Ishihata H, Shimauchi H. Expression of CD73/ecto-5′-nucleotidase on human gingival fibroblasts and contribution to the inhibition of interleukin-1α-induced granulocyte-macrophage colony stimulating factor production. Journal of Periodontal Research. 2004;39(1):10–19. doi: 10.1111/j.1600-0765.2004.00698.x. [DOI] [PubMed] [Google Scholar]
- 55.Synnestvedt K, Furuta GT, Comerford KM, et al. Ecto-5′-nucleotidase (CD73) regulation by hypoxia-inducible factor-1 mediates permeability changes in intestinal epithelia. Journal of Clinical Investigation. 2002;110(7):993–1002. doi: 10.1172/JCI15337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Eltzschig HK, Ibla JC, Furuta GT, et al. Coordinated adenine nucleotide phosphohydrolysis and nucleoside signaling in posthypoxic endothelium: role of ectonucleotidases and adenosine A2B receptors. Journal of Experimental Medicine. 2003;198(5):783–796. doi: 10.1084/jem.20030891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ledoux S, Runembert I, Koumanov K, Michel JB, Trugnan G, Friedlander G. Hypoxia enhances Ecto-5′-nucleotidase activity and cell surface expression in endothelial cells: role of membrane lipids. Circulation Research. 2003;92(8):848–855. doi: 10.1161/01.RES.0000069022.95401.FE. [DOI] [PubMed] [Google Scholar]
- 58.Kalsi K, Lawson C, Dominguez M, Taylor P, Yacoub MH, Smolenski RT. Regulation of ecto-5′-nucleotidase by TNF-α in human endothelial cells. Molecular and Cellular Biochemistry. 2002;232(1-2):113–119. doi: 10.1023/a:1014806916844. [DOI] [PubMed] [Google Scholar]
- 59.Dalh Christensen L, Andersen V. Natural killer cells lack ecto-5’-nucleotidase. Natural Immunity. 1992;11(1):1–6. [PubMed] [Google Scholar]
- 60.Regateiro FS, Howie D, Nolan KF, et al. Generation of anti-inflammatory adenosine byleukocytes is regulated by TGF-β. European Journal of Immunology. 2011;41(10):2955–2965. doi: 10.1002/eji.201141512. [DOI] [PubMed] [Google Scholar]
- 61.Chalmin F, Mignot G, Bruchard M, et al. Stat3 and Gfi-1 transcription factors control Th17 cell immunosuppressive activity via the regulation of ectonucleotidase expression. Immunity. 2012;36(3):362–373. doi: 10.1016/j.immuni.2011.12.019. [DOI] [PubMed] [Google Scholar]
- 62.Savic V, Stefanovic V, Ardaillou N, Ardaillou R. Induction of ecto-5’-nucleotidase of rat cultured mesangial cells by interleukin-1β and tumour necrosis factor-α. Immunology. 1990;70(3):321–326. [PMC free article] [PubMed] [Google Scholar]
- 63.Jackson SW, Hoshi T, Wu Y, et al. Disordered purinergic signaling inhibits pathological angiogenesis in Cd39/Entpd1-null mice. American Journal of Pathology. 2007;171(4):1395–1404. doi: 10.2353/ajpath.2007.070190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sun X, Wu Y, Gao W, et al. CD39/ENTPD1 expression by CD4+Foxp3+ regulatory T cells promotes hepatic metastatic tumor growth in mice. Gastroenterology. 2010;139(3):1030–1040. doi: 10.1053/j.gastro.2010.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Künzli BM, Bernlochner MI, Rath S, et al. Impact of CD39 and purinergic signalling on the growth and metastasis of colorectal cancer. Purinergic Signalling. 2011;7(2):231–241. doi: 10.1007/s11302-011-9228-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Stagg J, Divisekera U, Duret H, et al. CD73-deficient mice have increased antitumor immunity and are resistant to experimental metastasis. Cancer Research. 2011;71(8):2892–2900. doi: 10.1158/0008-5472.CAN-10-4246. [DOI] [PubMed] [Google Scholar]
- 67.Wang L, Fan J, Thompson LF, et al. CD73 has distinct roles in nonhematopoietic and hematopoietic cells to promote tumor growth in mice. Journal of Clinical Investigation. 2011;121(6):2371–2382. doi: 10.1172/JCI45559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Jin D, Fan J, Wang L, et al. CD73 on tumor cells impairs antitumor T-cell responses: a novel mechanism of tumor-induced immune suppression. Cancer Research. 2010;70(6):2245–2255. doi: 10.1158/0008-5472.CAN-09-3109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Beavis PA, Stagg J, Darcy PK, Smyth MJ. CD73: a potent suppressor of antitumor immune responses. Trends in Immunology. 2012;33(5):231–237. doi: 10.1016/j.it.2012.02.009. [DOI] [PubMed] [Google Scholar]
- 70.Leth-Larsen R, Lund R, Hansen HV, et al. Metastasis-related plasma membrane proteins of human breast cancer cells identified by comparative quantitative mass spectrometry. Molecular and Cellular Proteomics. 2009;8(6):1436–1449. doi: 10.1074/mcp.M800061-MCP200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wu X-R, He X-S, Chen Y-F, et al. High expression of CD73 as a poor prognostic biomarker in human colorectal cancer. Journal of Surgical Oncology. 2012;106(2):130–137. doi: 10.1002/jso.23056. [DOI] [PubMed] [Google Scholar]
- 72.Pulte D, Furman RR, Broekman MJ, et al. CD39 expression on T lymphocytes correlates with severity of disease in patients with chronic lymphocytic leukemia. Clinical Lymphoma, Myeloma and Leukemia. 2011;11(4):367–372. doi: 10.1016/j.clml.2011.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ohta A, Gorelik E, Prasad SJ, et al. A2A adenosine receptor protects tumors from antitumor T cells. Proceedings of the National Academy of Sciences of the United States of America. 2006;103(35):13132–13137. doi: 10.1073/pnas.0605251103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Clayton A, Al-Taei S, Webber J, Mason MD, Tabi Z. Cancer exosomes express CD39 and CD73, which suppress T cells through adenosine production. Journal of Immunology. 2011;187(2):676–683. doi: 10.4049/jimmunol.1003884. [DOI] [PubMed] [Google Scholar]
- 75.Cekic C, Sag D, Li Y, Theodorescu D, Strieter RM, Linden J. Adenosine A2B receptor blockade slows growth of bladder and breast tumors. Journal of Immunology. 2012;188(1):198–205. doi: 10.4049/jimmunol.1101845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kong T, Westerman KA, Faigle M, Eltzschig HK, Colgan SP. HIF-dependent induction of adenosine A2B receptor in hypoxia. FASEB Journal. 2006;20(13):2242–2250. doi: 10.1096/fj.06-6419com. [DOI] [PubMed] [Google Scholar]
- 77.Merighi S, Benini A, Mirandola P, et al. Caffeine inhibits adenosine-induced accumulation of hypoxia-inducible factor-1α, vascular endothelial growth factor, and interleukin-8 expression in hypoxic human colon cancer cells. Molecular Pharmacology. 2007;72(2):395–406. doi: 10.1124/mol.106.032920. [DOI] [PubMed] [Google Scholar]
- 78.Yang M, Ma C, Liu S, et al. HIF-dependent induction of adenosine receptor A2B skews human dendritic cells to a Th2-stimulating phenotype under hypoxia. Immunology and Cell Biology. 2010;88(2):165–171. doi: 10.1038/icb.2009.77. [DOI] [PubMed] [Google Scholar]
- 79.Shevach EM. Mechanisms of Foxp3+ T regulatory cell-mediated suppression. Immunity. 2009;30(5):636–645. doi: 10.1016/j.immuni.2009.04.010. [DOI] [PubMed] [Google Scholar]
- 80.Wolf AM, Wolf D, Steurer M, Gastl G, Gunsilius E, Grubeck-Loebenstein B. Increase of regulatory T cells in the peripheral blood of cancer patients. Clinical Cancer Research. 2003;9(2):606–612. [PubMed] [Google Scholar]
- 81.Ghiringhelli F, Larmonier N, Schmitt E, et al. CD4+CD25+ regulatory T cells suppress tumor immunity but are sensitive to cyclophosphamide which allows immunotherapy of established tumors to be curative. European Journal of Immunology. 2004;34(2):336–344. doi: 10.1002/eji.200324181. [DOI] [PubMed] [Google Scholar]
- 82.Ladoire S, Martin F, Ghiringhelli F. Prognostic role of FOXP3+ regulatory T cells infiltrating human carcinomas: the paradox of colorectal cancer. Cancer Immunology, Immunotherapy. 2011;60(7):909–918. doi: 10.1007/s00262-011-1046-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Deaglio S, Dwyer KM, Gao W, et al. Adenosine generation catalyzed by CD39 and CD73 expressed on regulatory T cells mediates immune suppression. Journal of Experimental Medicine. 2007;204(6):1257–1265. doi: 10.1084/jem.20062512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Schuler PJ, Harasymczuk M, Schilling B, Lang S, Whiteside TL. Separation of human CD4+CD39+ T cells by magnetic beads reveals two phenotypically and functionally different subsets. Journal of Immunological Methods. 2011;369(1-2):59–68. doi: 10.1016/j.jim.2011.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Hilchey SP, Kobie JJ, Cochran MR, et al. Human follicular lymphoma CD39+-infiltrating T cells contribute to adenosine-mediated T cell hyporesponsiveness. Journal of Immunology. 2009;183(10):6157–6166. doi: 10.4049/jimmunol.0900475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Chen Z, O’Shea JJ. Th17 cells: a new fate for differentiating helper T cells. Immunologic Research. 2008;41(2):87–102. doi: 10.1007/s12026-007-8014-9. [DOI] [PubMed] [Google Scholar]
- 87.van den Berg WB, Miossec P. IL-17 as a future therapeutic target for rheumatoid arthritis. Nature Reviews Rheumatology. 2009;5(10):549–553. doi: 10.1038/nrrheum.2009.179. [DOI] [PubMed] [Google Scholar]
- 88.Miyahara Y, Odunsi K, Chen W, Peng G, Matsuzaki J, Wang RF. Generation and regulation of human CD4+ IL-17-producing T cells in ovarian cancer. Proceedings of the National Academy of Sciences of the United States of America. 2008;105(40):15505–15510. doi: 10.1073/pnas.0710686105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Sfanos KS, Bruno TC, Maris CH, et al. Phenotypic analysis of prostate-infiltrating lymphocytes reveals T H17 and Treg skewing. Clinical Cancer Research. 2008;14(11):3254–3261. doi: 10.1158/1078-0432.CCR-07-5164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Su MF, Wang CF, Zhao YM, Wu JX, Zhang Y. Expression and clinical significance of IL-17 and IL-21 in patients with acute leukemia. Journal of Experimental Hematology. 2010;18(5):1143–1146. [PubMed] [Google Scholar]
- 91.Liu J, Duan Y, Cheng X, et al. IL-17 is associated with poor prognosis and promotes angiogenesis via stimulating VEGF production of cancer cells in colorectal carcinoma. Biochemical and Biophysical Research Communications. 2011;407(2):348–354. doi: 10.1016/j.bbrc.2011.03.021. [DOI] [PubMed] [Google Scholar]
- 92.Zhang JP, Yan J, Xu J, et al. Increased intratumoral IL-17-producing cells correlate with poor survival in hepatocellular carcinoma patients. Journal of Hepatology. 2009;50(5):980–989. doi: 10.1016/j.jhep.2008.12.033. [DOI] [PubMed] [Google Scholar]
- 93.He D, Li H, Yusuf N, et al. IL-17 promotes tumor development through the induction of tumor promoting microenvironments at tumor sites and myeloid-derived suppressor cells. Journal of Immunology. 2010;184(5):2281–2288. doi: 10.4049/jimmunol.0902574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Wang LF, Chiu HC, Hsu CJ, Liu CY, Hsueh YH, Miaw SC. Epicutaneous sensitization with a protein antigen induces Th17 cells. Journal of Dermatological Science. 2009;54(3):192–197. doi: 10.1016/j.jdermsci.2008.12.011. [DOI] [PubMed] [Google Scholar]
- 95.Martin-Orozco N, Muranski P, Chung Y, et al. T helper 17 cells promote cytotoxic T cell activation in tumor immunity. Immunity. 2009;31(5):787–798. doi: 10.1016/j.immuni.2009.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Muranski P, Boni A, Antony PA, et al. Tumor-specific Th17-polarized cells eradicate large established melanoma. Blood. 2008;112(2):362–373. doi: 10.1182/blood-2007-11-120998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Gabrilovich DI, Nagaraj S. Myeloid-derived suppressor cells as regulators of the immune system. Nature Reviews Immunology. 2009;9(3):162–174. doi: 10.1038/nri2506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Chalmin F, Ladoire S, Mignot G, et al. Membrane-associated Hsp72 from tumor-derived exosomes mediates STAT3-dependent immunosuppressive function of mouse and human myeloid-derived suppressor cells. Journal of Clinical Investigation. 2010;120(2):457–471. doi: 10.1172/JCI40483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Stagg J, Beavis PA, Divisekera U, et al. CD73-Deficient mice are resistant to carcinogenesis. Cancer Research. 2012;72(9):2190–2196. doi: 10.1158/0008-5472.CAN-12-0420. [DOI] [PubMed] [Google Scholar]
- 100.Michaud M, Martins I, Sukkurwala AQ, et al. Autophagy-dependent anticancer immune responses induced by chemotherapeutic agents in mice. Science. 2011;334(6062):1573–1577. doi: 10.1126/science.1208347. [DOI] [PubMed] [Google Scholar]
- 101.Pellegatti P, Raffaghello L, Bianchi G, Piccardi F, Pistoia V, Di Virgilio F. Increased level of extracellular ATP at tumor sites: in vivo imaging with plasma membrane luciferase. PLoS ONE. 2008;3(7) doi: 10.1371/journal.pone.0002599.e2599 [DOI] [PMC free article] [PubMed] [Google Scholar]


