Abstract
This study investigated whether overgeneral autobiographical memory (OGM) predicts the course of depression in adolescents. As part of a larger longitudinal study of risk for emotional disorders, 55 adolescents with a past history of major depressive disorder or minor depressive disorder completed the Autobiographical Memory Test. Fewer specific memories predicted the subsequent onset of a major depressive episode (MDE) over a 16-month follow-up period, even when covarying baseline depressive symptoms. This main effect was qualified by an interaction between specific memories and chronic interpersonal stress: Fewer specific memories predicted greater risk of MDE onset over follow-up at high (but not low) levels of chronic interpersonal stress. Thus, our findings suggest that OGM, in interaction with chronic interpersonal stress, predicts the course of depression among adolescents, and highlight the importance of measuring interpersonal stress in OGM research.
Keywords: Autobiographical memory, Memory specificity, Depression, Stress
Since Williams and Broadbent (1986) published their seminal article on the autobiographical memories of suicide attempters, overgeneral autobiographical memory (OGM) has emerged as an important cognitive marker for depression in general. When asked to retrieve a specific memory in response to a cue word, depressed individuals are less specific and/or more overgeneral in their memory retrieval than nondepressed individuals (Williams et al., 2007). Rather than recalling a memory of a particular event that lasted for less than one day (e.g., “my 13th birthday party”), depressed individuals often generate memories that refer to a class of events (categoric memories, e.g., “parties with my friends”) or to events lasting longer than one day (extended memories, e.g., “my week-long vacation”). OGM has been linked to (and may exert a causal influence on) important aspects of psychological functioning, including impaired interpersonal problem solving (Williams et al., 2007). Furthermore, OGM predicts the onset of depressive symptoms in vulnerable individuals (e.g., Mackinger, Loschin, & Leibetseder, 2000), and a worse course of depression (e.g., Brittlebank, Scott, Williams, & Ferrier, 1993). Thus, additional research on OGM may further understanding of the etiology, course, and consequences of depression.
OGM as a Predictor of the Course of Depression
Compared to those who exhibit less OGM, clinically depressed individuals who retrieve fewer specific and/or more categoric memories have higher levels of depressive symptoms at follow-up, even after covarying baseline symptoms (e.g., Brittlebank et al., 1993). Furthermore, OGM measured at one point in time when individuals are not depressed has been positively related to levels of depressive symptoms at follow-up. For example, compared to those who retrieved fewer categoric memories, pregnant women who retrieved more categoric memories to negative cue words reported higher levels of depressive symptoms 3 months after giving birth, again after covarying baseline depressive symptoms (Mackinger et al., 2000). In addition to predicting higher symptom levels, OGM has also been found to predict the continuation of major depressive disorder (MDD) diagnoses. Specifically, patients with MDD who exhibited higher levels of OGM upon hospital admission were more likely than patients not characterized by OGM to still meet criteria for MDD 3–4 weeks later, even when covarying depressive symptoms at admission (Hermans et al., 2008). Few studies have examined whether OGM predicts MDD recurrence, although the extant results are mixed. Spinhoven et al. (2006) failed to find that OGM in individuals in remission from MDD predicted new onsets of a major depressive episode (MDE) over a 24-month follow-up. Even though OGM predicted MDD diagnosis at 6-month follow-up in a sample of assault victims (Kleim & Ehlers, 2008), it is not clear in that study whether MDD diagnoses at the 6-month follow-up represented new onsets of depression. These findings could indicate that OGM predicts the maintenance and/or the recurrence of depression. Thus, more research is necessary to understand whether OGM predicts the recurrence of depression.
OGM, Stress, and Depression
Several studies suggest that OGM may interact with stress to contribute to depression. For example, a greater frequency of stressful life events predicted higher levels of depressive symptoms 4–6 weeks later, although only among students with greater OGM at baseline (Gibbs & Rude, 2004). Researchers have recently emphasized the role of chronic stress (i.e., stress ongoing for a prolonged period) in the development of depression, with some finding that chronic stress is more strongly related to depressive symptoms than acute stress (McGonagle & Kessler, 1990). However, few investigations have examined the interaction of OGM and chronic stress. Anderson, Goddard, and Powell (2009) did find that decreased memory specificity significantly moderated the relationship between chronic daily hassles and depressive symptoms in a nonclinical undergraduate sample. Specifically, more daily hassles over the past 3 months predicted higher depressive symptoms at follow-up, and this relationship was stronger for individuals who retrieved fewer specific memories at baseline. These results provide initial evidence that OGM and chronic stress may interact to predict the course of depression. However, Anderson et al. (2009) only used a checklist measure of daily hassles to predict later depressive symptoms, and self-report checklist stress measures have many limitations. Indeed, many experts (e.g., Monroe, 2008) have discouraged their use in research on clinical disorders. Interview-based measures are instead the current gold-standard for assessing stress.
Moreover, no work has yet examined whether particular types of chronic stress interact with OGM more than others to contribute to depression. Interpersonal stress is thought to have special significance for depression, especially in adolescents (e.g., Rudolph, 2009). Interpersonal stressors may interfere with normative developmental processes that occur in adaptive relationships, like establishing a healthy sense of self, thereby increasing risk for depression. Interpersonal stress, such as poor family relationship quality, has been found to predict initial MDD onset in female adolescents (Eberhart & Hammen, 2006). Furthermore, in a sample of patients with rheumatoid arthritis and osteoarthritis, only interpersonal conflict events (and not non-interpersonal stressful events) were significantly correlated with depressive symptoms (Zautra, Burleson, Matt, Roth, & Burrows, 1994). Given evidence that interpersonal stress may be more depressogenic than non-interpersonal stress, we hypothesized that OGM would interact with chronic interpersonal stress in predicting the course of depression (e.g., by heightening the depressogenic effects of chronic interpersonal stress).
OGM in Adolescents
Despite extensive research on OGM in depressed adults, relatively few studies have investigated OGM in adolescents. Although adolescents with MDD have been shown to exhibit more OGM than nondepressed adolescents (e.g., Park, Goodyer, & Teasdale, 2002), no study has examined whether OGM predicts the course of depression in adolescents with a history of depression. Depression often emerges in adolescence (Kessler et al., 2003), and studying OGM in adolescents may have important implications. If OGM predicts the course of depression in adolescents, then OGM could potentially serve as a target for prevention and intervention (Park et al., 2002). Preliminary research suggests that memory specificity training interventions have promising results for individuals with depression (e.g., Raes, Williams, & Hermans, 2009). Longitudinal research examining OGM and the development and course of depression in adolescents can help build an empirical foundation for such strategies.
Goals of the Current Study
We investigated the predictive relationship between OGM and the course of depression in adolescents. Participants were high school students with a past history of MDD or minor depressive disorder (mDD) who are a subset of those in the Northwestern-UCLA Youth Emotion Project (YEP), a prospective longitudinal study examining risk factors for emotional disorders. We included those with a history of mDD because subthreshold depression (like mDD) during adolescence is associated with a substantial risk of subsequent MDD onset. In one investigation (Fergusson, Horwood, Ridder, & Beautrais, 2005), the odds ratios for subsequent MDD onset during young adulthood for adolescents with MDD and for adolescents with subthreshold depression (defined as exhibiting at least depressed mood or loss of interest for 2 or more weeks, but not meeting the diagnostic cutoff of five or more symptoms or endorsing clinically significant distress and/or impairment) were both 2.4. Given the clinical significance of subthreshold depression and the recent emphasis on dimensional, rather than categorical, models of psychopathology (e.g., Watson, 2005), we included individuals who were in remission from either MDD or mDD at the time of the AMT administration.
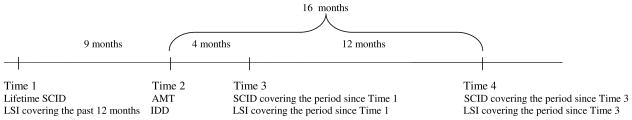
Four time points of the larger investigation were of interest in the current study: Time 1 (a baseline assessment of psychopathology and life stress), Time 2 (an assessment of OGM and depressive symptoms), and Times 3 and 4 (annual follow-up assessments of psychopathology and life stress; see Figure 1). We examined whether OGM predicted the subsequent onset of a MDE from Time 2 through Time 4 (a 16-month follow-up period). In addition, we hypothesized that OGM would interact with chronic interpersonal stress. Although interpersonal stress is conceptualized as a vulnerability for depression across the lifespan, such stress might be especially important during adolescence, a critical period for the formation of interpersonal identity. In sum, we investigated whether OGM predicted subsequent MDE onset over a 16-month follow-up in late adolescents in remission from MDD or mDD, both alone and in interaction with chronic interpersonal stress.
Figure 1.
Timeline of the study presenting the mean number of months between time points. At Time 1, a lifetime SCID and LSI for the past 12 months were administered. Approximately 9 months later, participants completed the AMT and IDD at Time 2. At Time 3, approximately 4 months after Time 2, SCID and LSI interviews covering the period since Time 1 were administered. SCID and LSI interviews covering the period since Time 3 were administered at Time 4, approximately 12 months after Time 3 and 16 months after Time 2.
Method
Participants
Participants were from a larger sample of 627 adolescents in an 8-year longitudinal study of risk factors for emotional disorders (the Youth Emotion Project, YEP). At recruitment, participants were juniors at one of two public high schools, one in suburban Chicago and one in suburban Los Angeles. At screening, participants completed the neuroticism scale of the Eysenck Personality Questionnaire (EPQ-R-N; Eysenck & Eysenck, 1975), and were categorized as low-, medium-, and high-scorers. High-EPQ-R-N scorers were oversampled to obtain a behavioral high-risk sample for the development of emotional disorders. Approximately 9 months after the Time 1 assessment (M =9.1, SD =1.5), a random subset of the sample (n =333) completed a cognitive task battery at Time 2, which included the AMT.
Of the 333 individuals who completed the AMT, we examined the subset of 55 participants who were in full remission from MDD or mDD at Time 2. Forty-one participants had at least one prior episode of MDD, and 14 had at least one prior episode of mDD, according to DSM-IV criteria. We excluded individuals with a current or past diagnosis of bipolar I or II (n=4). Consistent with DSM-IV guidelines, full remission status was defined as no longer meeting MDD or mDD criteria for at least 2 months prior to Time 2. Participants had to complete a measure of depressive symptoms at Time 2 (this was covaried in the analyses). At Time 2, these 55 participants ranged in age from 16 to 18 years (M =17.1, SD =.4), and were predominantly female (75%) and ethnically diverse. Thirty-two individuals also had a current or past history of at least one more Axis I disorder (e.g., social phobia, specific phobia, attention-deficit/hyperactivity disorder).
Materials
Structured Clinical Interview for DSM-IV
Advanced graduate students and Bachelor’slevel research assistants assigned Axis I diagnoses using the SCID (First, Spitzer, Gibbon, & Williams, 1994). Interviewer training included approximately 30 hours of extensive self-study, didactics, role-playing, tests of diagnostic ability based on interview audio recordings, and observation of live interviews by doctoral-level supervisors. Interviewers’ assessments were supervised by doctoral-level clinical psychologists. At Time 2, all participants had a history of at least one episode of MDD or mDD associated with clinically significant distress and/or impairment. In addition, in this study we predicted the onset of clinically significant MDEs over follow-up. SCID diagnoses of clinically significant MDD and mDD have had good inter-rater reliability in this study. Kappas for clinically significant MDD at Times 1, 3, and 4 were .83, .65, and .84, respectively. Percent agreement for clinically significant mDD at Time 1 was .99.1
UCLA Life Stress Interview
The LSI (Hammen, 1991) is a semi-structured interview assessing ongoing stress in 10 domains: close friendship, social life, romantic relationships, family relationships, neighborhood environment, academic performance, work environment, financial status, personal health, and health of the individual’s family. These interviews were conducted by the same personnel who administered SCIDs, and LSI training was similar to that for the SCID. Interviewers rated chronic stress in each domain on a 1 to 5 scale (1 = superior conditions, 5 = exceptionally poor conditions). The LSI chronic stress ratings used in the current investigation had adequate to good inter-rater reliability (median intraclass correlation coefficient =.69). We averaged the close friendship, social life, romantic relationships, and family relationships domain ratings to create a chronic interpersonal stress composite. High scores on this composite reflect chronic stress in one or more domains such as a serious lack of social support or emotionally unavailable or neglectful parents. To test the specificity of chronic interpersonal stress, we created a chronic non-interpersonal stress composite by averaging the other six non-interpersonal domain ratings.
Inventory to Diagnose Depression
The IDD (Zimmerman, Coryell, Corenthal, & Wilson, 1986) is a 22-item self-report scale with items corresponding to DSM-III criteria for MDD. It has good internal consistency and high convergent validity. In this study, the total score was calculated to measure levels of depressive symptoms at Time 2 (the suicide item was excluded).
Autobiographical Memory Test
The AMT (Williams & Broadbent, 1986) is a cuing methodology used to elicit autobiographical memories. Trained undergraduates, graduate students, and Bachelor’s-level research assistants instructed participants to generate a unique specific memory within 30 seconds of being presented with a cue word. The experimenter presented each cue individually from a booklet. Up to seven practice items were administered, and participants only received feedback during practice trials. The experimental portion of the AMT had 16 trials divided into positive (happy, loved, successful, energetic, comfortable, brave, safe, calm) and negative (lonely, failure, sad, hopeless, afraid, angry, tense, worried) cues; trials alternated between the two types. No feedback was given on experimental trials, but scripted queries were sometimes used to clarify the meaning of the initial response. All responses were made orally and tape-recorded.
On each trial, responses were scored as falling into one of five categories: specific memory, extended memory, categoric memory, semantic associate (a response containing general semantic information, but no personal memory), or omission. Response coding had good inter-rater reliability [kappas for within-site (N =73) and cross-site (N =37) reliability were both .78]. As is common in OGM research (e.g., Kleim & Ehlers, 2008), we used the proportion of specific memories as our OGM measure, collapsing responses across cue valence.2
Procedure
At Time 1, participants were administered a lifetime SCID and an LSI covering the past 12 months. Approximately 9 months later (M =9.1, SD =1.5) at Time 2, participants completed the AMT and IDD (mean time between AMT and IDD administration =28 days, SD =57). Participants completed their first and second annual follow-up assessments at Times 3 and 4, approximately 4 months (M =3.9, SD =2.1) and 16 months after Time 2 (M =16.2, SD =2.5), respectively. At these two time points, the SCID and LSI were administered to gather diagnostic and life stress data for the time since the previous diagnostic and life stress interview. Participants had to complete Time 4 in order to be included in the present analyses. In the current investigation, we used data from the LSI at Time 3 as our chronic stress measure because this assessment covered the time of the AMT.
Results
Descriptive Statistics
Descriptive statistics for the AMT, IDD, and LSI are presented in Table 1. Most participants generated specific memories on the majority of trials. The mean levels of chronic interpersonal and non-interpersonal stress measured at Time 3 correspond to mild-moderate stress. The mean IDD total score falls in the minimal-mild range of depressive symptoms, thereby reflecting that participants were not currently depressed at the AMT. As in Anderson et al. (2009), the proportion of specific memories was not significantly correlated with IDD scores. However, the proportion of specific memories did have significant negative correlations with chronic stress. The proportion of specific memories was also significantly negatively correlated with the probability of MDE onset over follow-up, whereas IDD score was positively correlated with the probability of MDE onset over follow-up. There were 10 cases of a MDE onset over the follow-up period between Time 2 and Time 4.
Table 1.
Descriptive Statistics and Intercorrelations between AMT Performance, Chronic Life Stress, Depressive Symptoms, and Onset of a Major Depressive Episode (MDE) over Follow-up from Time 2 through Time 4 (N = 55)
| 1 | 2 | 3 | 4 | 5 | M | SD | Range of Possible Values | |
|---|---|---|---|---|---|---|---|---|
| 1. AMT proportion of specific memories | .82 | .15 | 0–1 | |||||
| 2. Mean chronic interpersonal stress | −.30* | 2.49 | .41 | 1–5 | ||||
| 3. Mean chronic non-interpersonal stress | −.31* | .40** | 2.19 | .31 | 1–5 | |||
| 4. IDD total scorea | −.04 | .36** | .06 | 17.43 | 9.09 | 0–84 | ||
| 5. MDE onset over follow-up | −.28* | .17 | −.19 | .28* | 18.2%b |
Note.
IDD administered at Time 2, within approximately 1 month of the AMT.
The percentage of participants who experienced the onset of a MDE from Time 2 through Time 4.
p < .05.
p < .01.
OGM and Chronic Interpersonal Stress as Predictors of MDE Onset over Follow-up
We used logistic regression to examine whether the proportion of specific memories, chronic interpersonal stress at Time 3, and/or their interaction predicted MDE onset from Time 2 through Time 4. Predictors were standardized, and each predictor was added on a different step.
We entered mean IDD total score at Time 2 on the first step, and it was a significant predictor of MDE onset [odds ratio (O.R.) = 2.00, p =.045]. The second step of adding the proportion of specific memories was also significant (O.R. =.45, p =.048). As the proportion of specific memories decreased, the probability of MDE onset over the 16-month follow-up increased. The third step for chronic interpersonal stress was not significant (O.R. =1.03, p =.94).
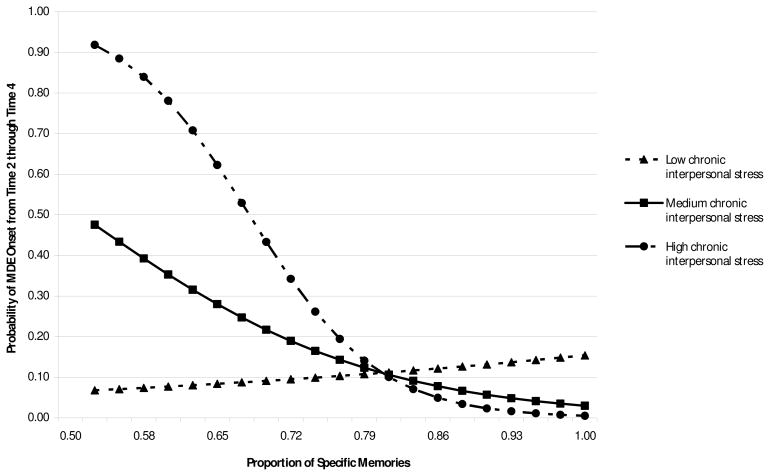
The step for the interaction between the proportion of specific memories and chronic interpersonal stress was significant (O.R. =.22, p =.02).3 We probed this interaction by examining the relationship between the proportion of specific memories and the probability of MDE onset over follow-up at low, medium, and high levels of chronic interpersonal stress (i.e., at values of one standard deviation below the mean, the mean, and one standard deviation above the mean on the chronic interpersonal stress variable). Simple slope tests revealed that the proportion of specific memories was a significant predictor of MDE onset over follow-up for high levels of chronic interpersonal stress (O.R. =.08, p =.02), and the simple slope test approached conventional levels of statistical significance for medium levels of chronic interpersonal stress (O.R. =.33, p =.053). For these stress levels, as memory specificity decreased, the probability of MDE onset over follow-up increased (see Figure 2). The proportion of specific memories was not a significant predictor of MDE onset over follow-up for low chronic interpersonal stress levels (O.R. =1.35, p =.65).
Figure 2.
Probability of MDE onset from Time 2 through Time 4 as a function of specific memories and chronic interpersonal stress. Values on the x-axis reflect the range of the proportion of specific memories in this sample. Low and high chronic interpersonal stress represent values of one standard deviation below and above the mean on this variable, respectively, and medium chronic interpersonal stress represents the mean value.
We also ran the logistic regression analysis with both chronic interpersonal and non-interpersonal stress entered together to test the specificity of the relationship with chronic interpersonal stress. The step for including chronic interpersonal and non-interpersonal stress was significant (p =.03), but only chronic non-interpersonal stress was a significant predictor, such that higher levels of chronic non-interpersonal stress were associated with a lower probability of MDE onset over follow-up (O.R. =.25). The step for the two OGM by stress interaction terms approached conventional levels of statistical significance (p =.09). In this step, the interaction between the proportion of specific memories and chronic interpersonal stress was significant (O.R. =.19, p =.04), but the interaction between the proportion of specific memories and chronic non-interpersonal stress was not significant (O.R. =1.08, p =.92). In sum, only chronic interpersonal stress significantly interacted with OGM in predicting an increased risk of MDE onset over follow-up in this sample.
Discussion
To our knowledge, this is the first study to demonstrate that OGM, in interaction with chronic interpersonal stress, predicts subsequent MDE onset in adolescents in remission from MDD or mDD. In our sample, as the proportion of specific memories decreased, the probability of MDE onset over follow-up increased for those who experienced higher levels of chronic interpersonal stress. Furthermore, our findings highlight that it is chronic interpersonal stress in particular that interacts with OGM in predicting the course of depression. When both chronic interpersonal and non-interpersonal stress were entered together, only chronic interpersonal stress predicted MDE onset in interaction with the proportion of specific memories. Although there was no significant main effect of chronic interpersonal stress, chronic non-interpersonal stress was a unique predictor of MDE onset over follow-up when it was entered along with chronic interpersonal stress. Specifically, the portion of chronic non-interpersonal stress that does not overlap with chronic interpersonal stress predicted MDE onset, with higher non-interpersonal stress levels associated with a lower probability of MDE onset over follow-up. This unexpected finding warrants replication but together these results suggest that interpersonal stress may play a more prominent role in increasing risk for depression in interaction with OGM than non-interpersonal stress.
Our findings are consistent with other studies examining the relationship between OGM, stress, and depression that have also found that the predictive relationship between OGM and higher levels of depressive symptoms at follow-up is greatest for individuals with high stress levels (Anderson et al., 2009; Gibbs & Rude, 2004). Furthermore, we extended this finding to a longer follow-up period than most research. Anderson et al. (2009) and Gibbs and Rude (2004) examined the relationship between stress, OGM, and the course of depression over 3 months and 4–6 weeks, respectively, whereas the current study followed participants over approximately 16 months. Spinhoven et al. (2006) examined recurrence over a longer period (24 months), but they did not address the possible role of stress.
One difference between the current investigation and the studies by Anderson et al. (2009) and Gibbs and Rude (2004) is that in these prior studies, the stress measure covered the time between the AMT and follow-up assessment, whereas our measure of chronic stress covered the time surrounding the AMT. Nevertheless, this aspect of our design is in accordance with the notion that cognitive bias in individuals in remission from depression may be most predictive of depressive relapse when the bias is measured under conditions of stress or induced negative mood (e.g., Segal, Gemar, & Williams, 1999). Our results are consistent with a model of depression that posits that cognitive biases may increase vulnerability to depression under certain conditions. One interpretation of our findings is that an underlying OGM bias in individuals in remission from depression may only exert an effect on depression when the bias was measured under conditions of high chronic interpersonal stress. Additionally, OGM has been associated with impaired social problem-solving (Williams et al., 2007), and it is possible that OGM may keep people from dealing effectively with their interpersonal stressors, thereby contributing to depression. OGM may also potentially block the beneficial positive reinforcement that derives from specific positive events and that would normally serve to buffer against negative stressors, thereby increasing the negative impact of stress and contributing to depression vulnerability. Additional longitudinal research measuring OGM, problem-solving, stress, and depression at more frequent intervals is needed to directly test these hypotheses, but our study does provide preliminary support.
Our finding of a significant OGM by chronic interpersonal stress interaction is important because most prior research has not examined the roles of stress and OGM in predicting the course of depression. Furthermore, we are unaware of any study using an interview-based stress measure that compares the effects of chronic interpersonal and non-interpersonal stress. Future research should continue to examine how interpersonal stress and OGM may interact to contribute to the onset and maintenance of depression. Additional work investigating the mechanisms by which this may occur would also be important. Research delineating how risk for depression is conferred will be informative, especially because OGM could potentially be a proxy indicator of more pervasive cognitive processing difficulties, such as a lack of cognitive flexibility. Our study cannot directly address this issue, but it is of interest to examine this phenomenon in future studies. Another limitation is that we did not address whether OGM predicts initial vulnerability to depression. However, we plan to examine this question in the larger longitudinal study as more participants experience first onsets of depression.
In summary, our study suggests that OGM and chronic interpersonal stress interact to influence the course of depression in adolescents. OGM is already an important phenomenon for understanding the development and maintenance of depression (e.g., Williams et al., 2007), and our results suggest that at least some of the effects of OGM are strongest at higher levels of stress.
Acknowledgments
We would like to thank the National Institutes of Health for supporting our research (Grant# R01MH065652 to Drs. Zinbarg and Mineka, and R01MH065651 to Dr. Craske), and acknowledge the assistance of the many students who helped with data collection.
Footnotes
We used percent agreement to measure inter-rater reliability given the low base rate of clinically significant mDD at Time 1. We do not report this statistic for Time 3 because there were no clinically significant cases of mDD in the cases selected for reliability.
Like some other investigators (e.g., Kleim & Ehlers, 2008), we only examined specific memories. Participants retrieved few categoric memories; the proportion of categoric memories ranged from 0 to .31 (M =.03, SD =.07). The range for the proportion of specific memories was much less restricted (range=.53–1.00).
The step for the interaction of the proportion of specific memories and chronic interpersonal stress remained significant when we only included the 41 individuals in remission from MDD at Time 2 (O.R. =.15, p =.02). However, the steps for IDD and the proportion of specific memories were no longer significant (O.R. =1.62, p =.26 for IDD; O.R. =.75, p =.56 for the proportion of specific memories).
References
- Anderson RJ, Goddard L, Powell JH. Reduced specificity of autobiographical memory as a moderator of the relationship between daily hassles and depression. Cognition and Emotion. 2009 doi: 10.1080/02699930802598029. Advance online publication. [DOI] [Google Scholar]
- Brittlebank AD, Scott J, Williams JMG, Ferrier IN. Autobiographical memory in depression: State or trait marker? British Journal of Psychiatry. 1993;162:118–121. doi: 10.1192/bjp.162.1.118. [DOI] [PubMed] [Google Scholar]
- Eberhart NK, Hammen CL. Interpersonal predictors of onset of depression during the transition to adulthood. Personal Relationships. 2006;13:195–206. [Google Scholar]
- Eysenck HJ, Eysenck SBG. Manual of the Eysenck Personality Questionnaire (adult and junior) London: Hodder & Stoughton; 1975. [Google Scholar]
- Fergusson DM, Horwood J, Ridder EM, Beautrais AL. Subthreshold depression in adolescence and mental health outcomes in adulthood. Archives of General Psychiatry. 2005;62:66–72. doi: 10.1001/archpsyc.62.1.66. [DOI] [PubMed] [Google Scholar]
- First M, Spitzer R, Gibbon M, Williams J. Structured Clinical Interview for DSM-IV Axis I Disorders. New York: Biometrics Research; 1994. [Google Scholar]
- Gibbs BR, Rude SS. Overgeneral autobiographical memory as depression vulnerability. Cognitive Therapy and Research. 2004;28:511–526. [Google Scholar]
- Hammen C. Generation of stress in the course of unipolar depression. Journal of Abnormal Psychology. 1991;100:555–561. doi: 10.1037//0021-843x.100.4.555. [DOI] [PubMed] [Google Scholar]
- Hermans D, Vandromme H, Debeer E, Raes F, Demyttenaere K, Brunfaut E, et al. Overgeneral autobiographical memory predicts diagnostic status in depression. Behaviour Research and Therapy. 2008;46:668–677. doi: 10.1016/j.brat.2008.01.018. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, et al. The epidemiology of major depressive disorder: Results from the National Comorbidity Survey Replication (NCS-R) Journal of the American Medical Association. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Kleim B, Ehlers A. Reduced autobiographical memory specificity predicts depression and posttraumatic stress disorder after recent trauma. Journal of Consulting and Clinical Psychology. 2008;76:231–242. doi: 10.1037/0022-006X.76.2.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackinger HF, Loschin GG, Leibetseder MM. Prediction of postnatal affective changes by autobiographical memories. European Psychologist. 2000;5:52–61. [Google Scholar]
- McGonagle KA, Kessler RC. Chronic stress, acute stress, and depressive symptoms. American Journal of Community Psychology. 1990;18:681–706. doi: 10.1007/BF00931237. [DOI] [PubMed] [Google Scholar]
- Monroe SM. Modern approaches to conceptualizing and measuring human life stress. Annual Review of Clinical Psychology. 2008;4:33–52. doi: 10.1146/annurev.clinpsy.4.022007.141207. [DOI] [PubMed] [Google Scholar]
- Park RJ, Goodyer IM, Teasdale JD. Categoric overgeneral autobiographical memory in adolescents with major depressive disorder. Psychological Medicine. 2002;32:267–276. doi: 10.1017/s0033291701005189. [DOI] [PubMed] [Google Scholar]
- Raes F, Williams JMG, Hermans D. Reducing cognitive vulnerability to depression: A preliminary investigation of MEmory Specificity Training (MEST) in inpatients with depressive symptomatology. Journal of Behavior Therapy and Experimental Psychiatry. 2009;40:24–38. doi: 10.1016/j.jbtep.2008.03.001. [DOI] [PubMed] [Google Scholar]
- Rudolph KD. Adolescent depression. In: Gotlib IH, Hammen CL, editors. Handbook of depression. 2. New York: Guilford Press; 2009. pp. 444–466. [Google Scholar]
- Segal ZV, Gemar M, Williams S. Differential cognitive response to a mood challenge following successful cognitive therapy or pharmacotherapy for unipolar depression. Journal of Abnormal Psychology. 1999;108:3–10. doi: 10.1037//0021-843x.108.1.3. [DOI] [PubMed] [Google Scholar]
- Spinhoven P, Bockting CLH, Schene AH, Koerter MWJ, Wekking EM, Williams JMG, et al. Autobiographical memory in the euthymic phase of recurrent depression. Journal of Abnormal Psychology. 2006;115:590–600. doi: 10.1037/0021-843X.115.3.590. [DOI] [PubMed] [Google Scholar]
- Watson D. Rethinking the mood and anxiety disorders: A quantitative hierarchical model for DSM-V. Journal of Abnormal Psychology. 2005;114:522–536. doi: 10.1037/0021-843X.114.4.522. [DOI] [PubMed] [Google Scholar]
- Williams JMG, Barnhofer T, Crane C, Hermans D, Raes F, Watkins E, et al. Autobiographical memory specificity and emotional disorder. Psychological Bulletin. 2007;133:122–148. doi: 10.1037/0033-2909.133.1.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams JMG, Broadbent K. Autobiographical memory in suicide attempters. Journal of Abnormal Psychology. 1986;95:144–149. doi: 10.1037//0021-843x.95.2.144. [DOI] [PubMed] [Google Scholar]
- Zautra AJ, Burleson MH, Matt KS, Roth S, Burrows L. Interpersonal stress, depression, and disease activity in rheumatoid arthritis and osteoarthritis patients. Health Psychology. 1994;13:139–148. doi: 10.1037//0278-6133.13.2.139. [DOI] [PubMed] [Google Scholar]
- Zimmerman M, Coryell W, Corenthal C, Wilson S. A self-report scale to diagnose major depressive disorder. Archives of General Psychiatry. 1986;43:1076–1081. doi: 10.1001/archpsyc.1986.01800110062008. [DOI] [PubMed] [Google Scholar]