Abstract
Background:
A lot of studies have shown periodontal diseases as a risk factor for adverse pregnancy outcomes. The association between periodontitis and preeclampsia has been studied recently with controversy. Considering the importance of preventing preeclampsia as a dangerous and life-threatening disease in pregnant women, the present study was carried out.
Methods:
Two hundred and ten pregnant women participated in this case-control study (105 controls & 105 cases) during years 2007 and 2008. Preeclamptic cases were defined as blood pressure ≥140/90mmHg and proteinuria +1. Control group were pregnant women with normal blood pressure without proteinuria. Both groups were examined during 48 hours after child delivery. Plaque Index (PLI), Pocket Depth (PD), Clinical Attachment Level (CAL), Bleeding On Probing (BOP), Gingival Recession (GR) were measured on all teeth except for third molars and recorded as periodontal examination. Data was analyzed using t-test, chi-square, and Mann-Whitney U statistical tests.
Results:
There was no significant difference between the two study groups for PD. CAL, GR, BOP significantly increased in the case group (P< 0.02). This study showed that preeclamptic cases were more likely to develop periodontal disease (P< 0.0001). Eighty three percent of the control group and 95% of the case group had periodontal disease (P< 0.005) which had shown that preeclamptic cases were 4.1 times more likely to have periodontal disease (OR= 4.1).
Conclusion:
Preeclamptic cases significantly had higher attachment loss and gingival recession than the control group.
Keywords: Periodontal disease, Preeclampsia, Pregnancy
Introduction
Periodontal disease is chronic infection of gingiva and the dental supportive structures that is caused by periopathogen microorganisms and it is recognized by extensive damage to the dental supportive structures such as alveolar bone that is accompanied by forming pocket and gingival recession. The mechanism of this process includes direct tissue damage as a result of bacterial plaque and indirect damage due to the bacterial effects on the immune system and the initiation of the host’s inflammatory response. Periodontal disease occurs in up to 15% of the fertile women and a large proportion of pregnant women (1). The severity of periodontitis is measured by clinical attachment loss (CAL); higher CAL is representative of severe disease.
In the year 2006, Offenbacher et al. were among the first who reported the relationship between periodontal disease on one hand, and premature labor and low birth weight on the other (2). As a result, researches were carried out on grounds of finding the link between periodontal disease and the complications of pregnancy such as preeclampsia. Preeclampsia is a rapidly progressing syndrome in pregnant women that is characterized by the blood pressure equal or greater than 140/90 mmHg after the week 20 of pregnancy along with +1 proteinuria in urine sample. The reasons of this syndrome could be listed as abnormal thromboplastic invasion of uterine vessels, immunologic mismatch between mother and child, lack of mother’s proper compatibility with the cardiovascular and inflammatory changes of pregnancy, diet, and genetics (3). Preeclampsia is one of the main causes of maternal mortality and the death of their fetuses in the world (3–7) with prevalence of 3–5 percent in the pregnant women (8). It mostly happens in the first pregnancy, and usually in the second and the third trimester (5) also in multiple gestation pregnancies (4). The treatment is the termination of the pregnancy with the least trauma to mother, and consequent childbirth (3).
Periodontal disease has been introduced as a possible risk factor for complications in pregnancy including preeclampsia in a number of studies (1, 5–7, 9, 10); however, the matter was not confirmed in certain other researches (4). Considering the previous contradictory research results and the importance of preventing preeclampsia as a dangerous and life-threatening disease in pregnant women, the present study was carried out.
Materials and Methods
This case-control study was carried out on 210 pregnant women including some 105 pregnant women suffering from preeclampsia as the case group and another 105 healthy pregnant women as the control group through sequential admissions to Mahdiyeh, Shohadaye Tajrish, and Imam Hossein Medical Centers between 2007 and 2008 until the number of the cases reached to the desired figure.
Those women suffering from preeclampsia, diagnosed by a gynecologist, were examined for periodontal disease in a maximum period of 48 h after the labor. At the same time, those pregnant women who did not suffer from preeclampsia and had labor on the same day or in a time period of 48 h were considered as the control group and underwent the periodontal examination, too. Then, informed consents were taken from those who wished to participate in the study. The inclusion criteria were being over 18 yr old and having a minimum number of 15 teeth as well as having no systemic disease, no history of infection during pregnancy and no periodontal therapy within 6 mo before pregnancy.
Those people who required prophylactic antibiotics to continue their treatments, diabetics, smokers, alcoholics, also the patients with chronic hypertension, congenital heart diseases, heart murmurs, heart valves problems, multiple gestation, patients who were positive for Human immunodeficiency virus (HIV), those who had taken drugs causing gingival proliferation such as phenytoin, cyclosporine A, patients with severe dental decays, people who had taken aspirin or Non-steroidal anti-inflammatory drugs (NSAIDs), those with endocrine diseases, those with collagen diseases such as lupus, also patients using drugs that affect sex hormones, patients with poly cystic ovary or abnormal uterus, and those with kidney diseases were excluded from the present study.
The case and the control groups were similar for age, the number of pregnancies, the number of labors with live babies, prenatal cares, and the level of literacy. The periodontal examinations included measuring the pocket depth (PD), clinical attachment loss (CAL), bleeding on probing (BOP), gingival recession (GR), and plaque index (PLI) in all teeth except the wisdom teeth. PLI was measured according to O’leary (11), PD in four mesiobuccal, midbuccal, distobuccal, and lingual points by William’s probe in millimeters; CAL, the distance between cementoenamel junctions (CEJ) through the depth of the pocket in the four above-mentioned points were measured and recorded. Bleeding on probing (BOP) was calculated according Lenox and Kopczyk (11). Chronic periodontitis was classified according to the severity and the extent of the disease. If there was an involvement in less than 30% of the areas, local periodontitis would be reported. The severity of the disease according to the level of CAL was classified as follows: CAL equal or less than 2mm and CAL equal or greater than 3 mm were considered Mild, and Moderate to Severe, respectively.
Eventually, since the acquired data had a normal distribution, they were analyzed by T-test, chi-square, and Mann-Whitney U statistical tests. P-values less than 0.05 were considered statistically significant.
Results
The distribution of the individual, social, economical, hygienic, and treatment characteristics demonstrated that the individuals of both groups were similar according to age, occupation, the level of literacy, the size of the accommodation, the method of using the accommodation, the dimension of the household, the number of children, drinking tea or coffee, blood group, body mass index (BMI), the consanguineous relationship with their spouses, the time interval between the last childbirth and the present one, the week of gestation, the number of the previous pregnancies, the number of abortions, the history of low birth weight, the history of cesarean section, the history of preeclampsia, and the state of their dental plaques that their slight differences were statistically not significant.
In the group of control women, all had normal labor, and in the group of the case women, all had cesarean section. The mean duration of pregnancy in the control group and in the case group was 37.9± 1.8 wk and 35.36± 3.35 wk, respectively. T-test showed the difference was statistically significant (P< 0.0001). In the healthy group, one subject (1%) had stillbirth or a baby who required neonatal intensive care unit (NICU), but the incidence of the same in the case group was 11 patients (10.5%) and it was statistically significant (P< 0.005).
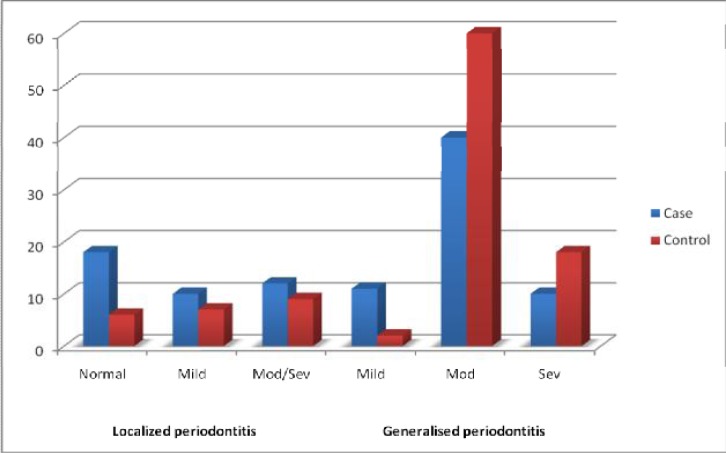
The extent of CAL was 1.26±1.14 mm, and 1.7±1.1 mm in the control group and in the case group, respectively. Therefore, the Mann-Whitney U test illustrated that the increase of CAL was higher in the case group than the control group (P< 0.01) The mean level of gingival recession (GR) in the control group was 0.13±0.15 mm and in the case group was 0.24±0.45 and the above-mentioned test showed that the difference was statistically significant (P< 0.02). BOP was 77% more than 20% in the control group while it was 89% more than 20% in the case group, and it was statistically significant (P< 0.02). The level of PD was similar in both groups (P< 0.2) (Table 1). The pregnant women in the case group were exposed to more severe periodontal diseases in comparison with the control group and the chi-square test showed that the difference was statistically significant (P< 0.0001) (Fig. 1).
Table 1:
The distribution of the pregnant women in both the control and the case groups divided according to the condition of preeclampsia and in terms of periodontal indices
|
Preeclampsia
|
||||||
|---|---|---|---|---|---|---|
| Control | Case | P value | ||||
| Periodontal Index | PD | 2.29±0.69 | 2.41±0.39 | P<0.2 | ||
| GR | 0.13±0.15 | 0.24±0.45 | P<0.02 | |||
| CAL | Percentage | mean±SD | 1.26±1.14 | .7±1.1 | P<0.01 | |
| CAL <3 | 100(95) | 93 (89) | ||||
| CAL≥3 | 5(5) | 12(11) | P<0.07 | |||
| BOP | Percentage | x±SD | 35.56±18.31 | 38.51±17.88 | P<0.01 | |
| BOP<20 | 24(23) | 12(11) | P<0.02 | |||
| BOP≥20 | 81(77) | 93(89) | ||||
Fig. 1:
The distribution of 210 studied cases according to their conditions of periodontal disease and divided in relation to the condition of preeclampsia
The distribution of the people in both groups according to the existence or nonexistence of the periodontal disease and division on the basis of preeclampsia is indicative of the fact that if women suffer from preeclampsia, it is 4.1 times more probable to face the periodontal disease than the healthy women (Odds ratio (OR) = 4.1) and with a probability of 95%, the real level of OR is estimated to range from a minimum of 1.5 to as high as 11.5 in the community (Table 2).
Table 2:
The distribution of the individuals in both the case and the control groups according to existence or nonexistence of the periodontal disease divided in terms of the condition of preeclampsia
|
Preeclampsia
|
P value | |||
|---|---|---|---|---|
| Control | Case | |||
| Periodontal disease | Negative | 18(17) | 5(5) | P< 0.005 |
| Positive | 87(83) | 100(95) | ||
| Total | 105(100) | 105(100) | ||
Discussion
The relationship between periodontal disease and preeclampsia has been brought into attention in recent years. Of course, the available researches for investigating the matter do not have a rather long history, and in our country in particular, no comprehensive study has been presented yet. Therefore, considering the research vacuum in this field, also considering the reports indicative of high neonatal and maternal mortality due to preeclampsia (3–7), the present study was carried out. This research showed that in women suffering from preeclampsia, the higher severity of periodontal disease is seen and these people are four times more prone to losing their periodontal attachments.
Approximately, all existing studies had similar results if compared with our present study except one that did not confirm the link (4). In this study, the periodontal indices such as PD, CAL, GR, and BOP are similar to the present study and only PLI was calculated by Sillness and Loe method that in our study was calculated by O’Leary method. The inclusion and exclusion criteria were similar to the present study. Nonetheless, the reason for the difference may possibly lie in the different definitions made for the periodontal disease, or the racial differences between the studied communities.
In another studies, the relationship between the periodontal disease and the incidence of preeclampsia has been reported with different ORs that is in the direction of the present study, despite the fact that in these researches, the existence and the severity of the periodontal disease were defined differently (5–7, 9). In one of these studies, the diagnosis of periodontal disease was based on PD, and CAL was not taken into account. The OR of this study was 2.1 (6). In another study, the OR of 3.47 was resulted (5). In a study by Cota, certain intervening variables were not equalized in the case and the control groups including chronic hypertension, smoking, and the number of labors. The OR was 1.88 in this study (7). In the present study, an OR of 4.1 was resulted and it was higher than the aforesaid researches that it could be due to the higher prevalence of preeclampsia in Iranian race that requires further investigations.
On the whole, some similarities between preeclampsia and atherosclerosis have been mentioned (2–4). In both diseases, endothelial dysfunction exists. Certain epidemiologic factors render the person susceptible to preeclampsia and atherosclerosis such as obesity, history of hypertension, black race. One of the reasons for abnormalities in endothelial function is the presence of severe inflammatory responses (7). Chronic inflammation such as periodontal disease is among the effective factors in preeclampsia. The periodontal disease as a disorder that the endotoxins of microorganisms and the inflammatory cytokines have roles in exacerbating thrombosis and the formation of atherosclerosis plaques, is one of the causative factors in preeclampsia. The same process may probably occur in placenta that leads to preeclampsia, i.e. the transmission of microorganisms from mouth to placenta and causing inflammation in it that may ultimately damage the endothelium of the placental vessels and result in clinical demonstration of preeclampsia that in one study on the serum obtained from umbilical cord, the presence of fetal IgM against oral pathogens (P. gingivalis) was proven (6). Nevertheless, one should consider that the causes of both periodontal disease and preeclampsia are multifactorial and this fact has to be considered when the results are being interpreted as in the present study in the control group on the healthy women, moderate to severe periodontitis existed in 50% of the individuals, yet they never had preeclampsia, whereas in the case group, 78% had moderate to severe periodontitis. Hence, it could be interpreted that those people with preeclampsia have higher rates of periodontal disease in comparison with the healthy individuals that in turn the occurrence of preeclampsia leads to the birth of premature babies.
In some studies the rate of c-reactive protein (CRP) was higher in the individuals with preeclampsia than the healthy pregnant women (10, 12), and if moderate to severe periodontal disease accompanied by high CRP existed, the risk of preeclampsia incidence alone would tangibly be higher than any other complication and the reason for high CRP in pregnant women has been mentioned to reflect the existence of chronic inflammatory disease.
In conclusion, noting the results of the previous researches and the present study is quite important in order to prevent the cases of preeclampsia and the birth of premature or deceased babies also the consequences; hence, cohort studies particularly by using other parameters and on bigger number of patients, and the periodontal treatment together with its investigation is necessary.
Ethical Considerations
Ethical issues including plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc. have been completely observed by the authors.
Acknowledgments
The authors declare that there is no conflict of interests.
References
- 1.Boggess KA, Edelstein BL. Oral health in women during preconception and pregnancy: implications for birth outcomes and infant oral health. Matern Child Health J. 2006;10(5 Suppl):S169–74. doi: 10.1007/s10995-006-0095-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Offenbacher S, Lin D, Strauss R, et al. Effects of periodontal therapy during pregnancy on periodontal status, biologic parameters, and pregnancy outcomes: a pilot study. J Periodontol. 2006;77(12):2011–24. doi: 10.1902/jop.2006.060047. [DOI] [PubMed] [Google Scholar]
- 3.Cunningham FG, Hauth JC, Leveno KJ, Gilstrap L, Bloom SL, Wenstrom KD. Williams obstetrics. New York (NY): 2005. pp. 761–808. [Google Scholar]
- 4.Khader YS, Jibreal M, Al-Omiri M, Amarin Z. Lack of association between periodontal parameters and preeclampsia. J Periodontol. 2006;77(10):1681–87. doi: 10.1902/jop.2006.050463. [DOI] [PubMed] [Google Scholar]
- 5.Canakci V, Canakci CF, Canakci H, et al. Periodontal disease as a risk factor for pre-eclampsia: a case control study. Aust NZJ Obstet Gynaecol. 2004;44(6):568–73. doi: 10.1111/j.1479-828X.2004.00323.x. [DOI] [PubMed] [Google Scholar]
- 6.Boggess KA, Lieff S, Murtha AP, Moss K, Beck J, Offenbacher S. Maternal periodontal disease is associated with an increased risk for preeclampsia. Obstet Gynecol. 2003;101(2):227–31. doi: 10.1016/s0029-7844(02)02314-1. [DOI] [PubMed] [Google Scholar]
- 7.Cota LO, Guimaraes AN, Costa JE, Lorentz TC, Costa FO. Association between maternal periodontitis and an increased risk of preeclampsia. J Periodontol. 2006;77(12):2063–69. doi: 10.1902/jop.2006.060061. [DOI] [PubMed] [Google Scholar]
- 8.Contreras A, Herrera JA, Soto JE, Arce RM, Jaramillo A, Botero JE. Periodontitis is associated with preeclampsia in pregnant women. J Periodontol. 2006;77(2):182–8. doi: 10.1902/jop.2006.050020. [DOI] [PubMed] [Google Scholar]
- 9.Kunnen A, Blaauw J, van Doormaal JJ, et al. Women with a recent history of early-onset pre-eclampsia have a worse periodontal condition. J Clin Periodontol. 2007;34(3):202–7. doi: 10.1111/j.1600-051X.2006.01036.x. [DOI] [PubMed] [Google Scholar]
- 10.Ruma M, Boggess K, Moss K, et al. Maternal periodontal disease, systemic inflammation, and risk for preeclampsia. Am J Obstet Gynecol. 2008;198(4):389 e381–85. doi: 10.1016/j.ajog.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 11.Perry DA. Carranza's Clinical Periodontology. 10th ed. Saunders Elsevier; California St. Louis: 2006. Plaque control for the periodontal patient; pp. 728–44. [Google Scholar]
- 12.Herrera JA, Parra B, Herrera E, et al. Periodontal disease severity is related to high levels of C-reactive protein in pre-eclampsia. J Hypertens. 2007;25(7):1459–64. doi: 10.1097/HJH.0b013e3281139ea9. [DOI] [PubMed] [Google Scholar]