Abstract
Background:
Exposure to formaldehyde (FA) causes irritative effects and induces nasopharyngeal cancer; the International Agency for Research on Cancer (IARC, Lyon) classified FA as carcinogenic to humans, Group 1. Many studies have been published so far concerning the occupational exposure of industrial workers, embalmers, pathologists and anatomists to FA but very few data regarding medical examiners are available.
Methods:
To assess the extent to which subjects were exposed to FA, airborne concentrations of this chemical were measured by High Performance Liquid Chromatography (HPLC). In September–October 2006 we examined the personnel, which worked in an autopsy room (medical examiners) and in three laboratories of pathologic anatomy of the University Medical School of Bari, Policlinico Hospital, Southern Italy. Irritative effects were also investigated.
Results:
All the personal exposure data obtained exceeded the National Institute for Occupational Safety and Health Threshold Limit Value-Time Weighted Average (NIOSH TLV-TWA: 0.02 mg/m3) and, in a few cases, even the American Conference of Industrial Hygienists Threshold Limit Value-Ceiling level (ACGIH TLV-C: 0.37 mg/m3).
Conclusion:
Irritative effects in more than 50% of the workers enrolled, increasing the risk of injuries.
Keywords: Occupational exposure, Formaldehyde, Air sampling, Occupational Health
Introduction
Formaldehyde (FA) is organic carbonyl compound that is commonly present in both indoor and outdoor environments. Occupational exposure to FA occurs in a wide variety of occupations and industries. As an aqueous solution (formalin), FA is widely used as a tissue preservative in autopsy rooms and in pathologic anatomy laboratories to preserve biological specimens.
Several studies showed that exposure to FA vapour at high concentration cause irritation of eyes, nose, throat, and respiratory tract of workers (1). Particularly, the studies about workers or students exposed to FA at mean levels above or equal to 1.2 mg/m3, showed that exposed people complained about eye and nasal irritation effects (2). Major concern is connected to FA carcinogenic effects. The IARC classified FA as Group 1, carcinogenic to humans, since sufficient epidemiological evidence was found that it causes nasopharyngeal cancer in humans (3). Several studies associated pathologists FA occupational exposure with elevated risks for cancer at various sites although this findings remain controversial (4).
Epidemiological data, concerning FA in fact, fail to raise a definitive conclusion regarding the carcinogenicity of FA. Experimental data indicated that in rats the carcinogenic activity of FA was associated with cytotoxic proliferative mechanism. Therefore Duhayon et al. (5) suggested that, to protect from these effects associated with FA exposure should be sufficient to protect from its potential carcinogenic effects, if any in humans.
Italian legislation does not provide for threshold limit values of FA. For this reason, we base on the values that the ACGIH and the NIOSH fix. In fact, the ACGIH (6) set a TLV-C for FA at 0.37 mg/m3. The NIOSH (7), due to the FA carcinogenic effects, recommended a TLV-TWA of 0.02 mg/m3 and a TLV-C of 0.12 mg/m3.
As a very few data regarding medical examiners occupational exposure to FA is available, the aim of this study was to characterize the occupational exposure to FA in an autopsy room and in a quarter of pathologic anatomy laboratories. The symptoms reported by the workers were also investigated and discussed.
Materials and Methods
FA exposure sources: Autopsy room
In September–October 2006 the autopsies were performed by four teams of specialists and post-graduate students practicing forensic medicine of the University Medical School of Bari, Policlinico Hospital. In a room next to the autopsy one, a variable number of plastic containers (200– 300 ml) were filled with formalin by post-graduate students, before each autopsy. During the autopsies, the organs from the cadavers were stored in the containers, which were handled, opened and closed by post-graduate students. The specialists examined the cadavers and gave instructions to the students about their tasks.
Pathologic anatomy laboratories
The examinations of the anatomic samples from autopsies or biopsies were performed in different steps (sampling, processing, etc.), some of which could expose the worker (technician or post-graduate student) to FA vapours. In the “sampling” step particularly, the worker handled the anatomic piece from the container filled with formalin and, before slicing, rinsed it under current water for 10–15 min. This step might imply the worker’s exposure to FA vapours due to the short distance from the formalin jar. The work shift exposure was also variable because of the unpredictable daily number of samples to be processed. The successive analytical steps involved the use of formalin without direct handling by the workers.
Subjects
Four specialists (all males) and six post-graduate medical students in legal medicine (four females and two males) were enrolled as well as two technicians (both male) and four post-graduate medical students (all female) working in the pathologic anatomy laboratories of the University Medical School of Bari, Policlinico Hospital, Southern Italy.
The working activity was monitored for ten autoptic sessions and six working days in the pathologic anatomy laboratories. Personal, indoor and outdoor samplings were performed simultaneously in September–October 2006.
We obtained an informed consent of each worker. An occupational medicine specialist investigated for each subject, the pathological anamnesis in order to verify the individual status as history of allergy, asthma, hay fever, upper respiratory infections. The physician also performed a medical examination.
Before and after the monitored work-shift, each worker enrolled in the study answered to a reliable and valid questionnaire about symptoms potentially related with airborne FA exposure, according to the ones used by Arts (2) and Kulle (8). Main issues were: olfactory perception, eye irritation, nose and throat irritation, cough, nose congestion, chest tightness and headache.
We divided the subjects in two groups (high exposure and low exposure) to evaluate the role of FA exposure on the reported symptoms.
Sites
The autopsy room was located in a basement. There were two doors leading to the corridor and to the refrigerator room. The doors were kept open during the autopsies, as well as the unique window of the site.
The three pathologic anatomy laboratories were located at the first floor of the building. In each of them, different steps of the working process were carried out. The sampling of the anatomic pieces was performed in Laboratory 1. These three rooms are equipped with air conditioners for the air temperature control. At the end of the work shift, the workers turn off the air conditioners and open the window to ensure natural ventilation.
Air sampling and analysis
Area samples were taken in the centre of the four rooms and at outdoor stations at 1.5 m above the floor. Personal samplers were pinned to the lapel of the enrolled workers.
Air samples were collected while autopsies and/or laboratory activities were performed and lasted about 180 and 250 min respectively in the autopsy room and in the pathology laboratories.
Air sampling was performed using Radiello® diffusive samplers which collect airborne carbonyl compounds as 2, 4-dinitrophenyihydrazine (DNPH) derivatives. The cartridges were sealed, kept dark and stored at 4° C until acetonitrile desorption within three days of collection. Sampling, storage and analysis were performed according to Radiello® manifacture instructions.
Analysis was performed by HPLC. A Series 200 (Perkin Elmer, U.S.A.) liquid chromatograph and an ultraviolet absorbance detector set to 365 nm were employed. Suitable dilutions of the standard calibration mix for aldehydes analysis (certified external standards, Sigma Aldrich) were used to determine the concentrations in the samples, based on the peak areas. Quality control was done by analyzing a blank cartridge for each pack of adsorbent cartridges; the analytical data were corrected by subtracting the value of the blank.
Statistical analysis
The Statistical Package for the Social Sciences program (SPSS, version 14.0, Chicago, IL, USA) was employed for statistical analysis. Mann-Whitney and Kruskall-Wallis tests were performed. To evaluate the confounding effect of smoking, odds ratios were calculated. We fit a multinomial logistic model to study the association between different levels of formaldehyde exposure and irritative symptoms, after adjustment for the potential confounding factors. In a second logistic model we compare two exposed groups (FA exposure ≤ or > 0.1 mg/m3). The level of significance was set at a P-value lower than 0.05.
Results
Table 1 shows the general characteristics of the subjects enrolled.
Table 1:
General characteristics of the subjects enrolled
| Sex | Mean | Smokers | Mean years smoked (only smokers) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| M | F | Age (yr) | Height (cm) | Weight (kg) | BMI | Exposure (min) | ||||
| Autopsy room | Medical examiners-specialists | 4 | 52 | 173 | 78.3 | 26.1 | 180 | 75% | 23.3 | |
| Post-graduate students | 2 | 4 | 33 | 171 | 65.2 | 22.1 | 33% | 7.5 | ||
| Pathologic anatomy laboratories | laboratory technicians | 2 | 46 | 160 | 63.5 | 25.3 | 250 | 50% | 25 | |
| Post-graduate students | 4 | 37 | 165 | 54.2 | 19.8 | 25% | 10 | |||
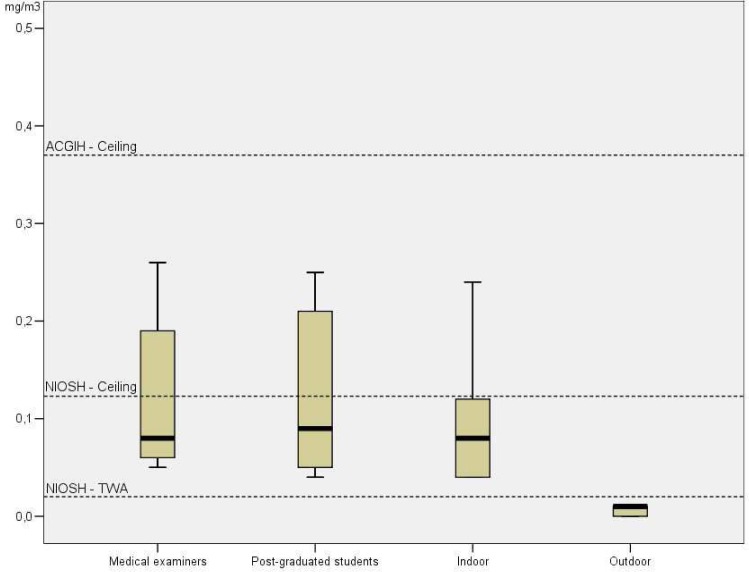
Each worker took part in one or more monitored autopsies or work shifts in the pathologic anatomy laboratories. Table 2 shows the measured airborne FA levels in the autopsy room. Outdoor FA levels were found to be negligible, compared to indoor and personal exposure levels, suggesting that indoor and professional sources play a major role in determining the workers exposure to FA. Indoor personal exposure levels always exceeded the NIOSH TLV-TWA (7) (Fig. 1). No statistically different personal exposure levels were found between medical examiners (specialists) and post-graduate students. Table 3 reports the exposure data from the pathology anatomy laboratories.
Table 2:
Airborne formaldehyde levels in the autopsy room (mg/m3)
| Samples | n | Mean | Median | SD | Range |
|---|---|---|---|---|---|
| Autopsy room (indoor) | 10 | 0.10 | 0.08 | 0.07 | 0.04–0.24 |
| Personal (medical examiner - specialist) | 10 | 0.12 | 0.08 | 0.08 | 0.05–0.26 |
| Personal (post — graduate student) | 10 | 0.12 | 0.09 | 0.08 | 0.04–0.25 |
| Personal (average) | 20 | 0.12 | 0.09 | 0.08 | 0.04–0.26 |
| Outdoor | 5 | 0.01 | 0.01 | 0.01 | < LOD-0.01 |
Fig. 1:
Autopsy room formaldehyde levels compared to threshold levels
Table 3:
Airborne formaldehyde levels in the pathology anatomy laboratories (mg/m3)*
| Samples | n | Mean | Median | SD | Range |
|---|---|---|---|---|---|
| Laboratory 1 (indoor) | 6 | 0.24 | 0.24 | 0.08 | 0.11–0.34 |
| Laboratory 2 (indoor) | 6 | 0.12 | 0.13 | 0.05 | 0.06–0.17 |
| Laboratory 3 (indoor) | 6 | 0.06 | 0.05 | 0.02 | 0.04–0.08 |
| Indoor (average) | 18 | 0.14 | 0.11 | 0.09 | 0.04–0.34 |
| Personal (laboratory technician) | 8 | 0.10 | 0.10 | 0.05 | 0.06–0.19 |
| Personal (post - graduate student) | 11 | 0.25 | 0.23 | 0.12 | 0.11–0.49 |
| Personal (average) | 19 | 0.19 | 0.17 | 0.12 | 0.06–0.49 |
| Outdoor | 3 | 0.01 | 0.01 | 0.01 | < LOD- 0.01 |
P-value < 0.05
As expected, the FA levels registered in the pathologic anatomy laboratories were found to be higher than the outdoors (Table 3).
The FA levels in the three laboratories appeared to be statistically different (Kruskall-Wallis test, P< 0.05) and the highest personal exposure levels were recorded in the Laboratory 1 where the washing and slicing of the anatomic pieces was performed.
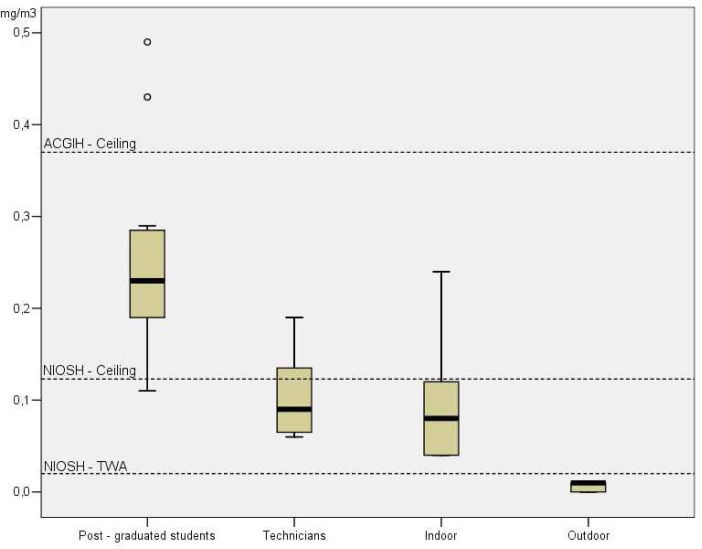
The exposure levels of the post-graduate students that worked in Laboratory 1 (Fig. 2) appeared to be statistically higher than those of the technicians (Mann-Whitney test, one tailed, P< 0.05). According to the FA levels recorded in the Laboratory 1 (Table 3), even the personal exposure of the post-graduate students working in the Laboratory 1 resulted to be higher than those reported in the other two laboratories.
Fig. 2:
Formaldehyde personal exposure levels in pathologic anatomy compared to threshold levels
None of the workers enrolled declared to suffer of such symptoms before the work-shift, but after the monitored work-shift, the incidences of the investigated irritative symptoms were odour detection 61%, pharynx irritation 50%, eye irritation 39%, irritation and congestion of nose 33%, headache 31%, chest tightness 19%, and cough 17% (Table 4).
Table 4:
Incidence of the investigated symptoms
| Occurrences after workshift | Incidence | |
|---|---|---|
| Eye irritation | 14 | 39% |
| Cough | 6 | 17% |
| Odour detection | 22 | 61% |
| Pharynx/larinx irritation | 18 | 50% |
| Nose irritation | 12 | 33% |
| Headache | 11 | 31% |
| Nose congestion | 12 | 33% |
| Chest tightness | 7 | 19% |
The smell of FA was detected by the 61% of the workers enrolled and their median FA exposure was 0.16 mg/m3 (Table 5). None of the workers enrolled, showed atopic dermatitis, as well as suffered of asthma.
Table 5:
Formaldehyde exposure levels (mg/m3) and reported symptoms
| Mean | Median | S.D. | Range | |
|---|---|---|---|---|
| Eye irritation | 0.21 | 0.20 | 0.13 | 0.07 - 0.49 |
| Cough | 0.21 | 0.18 | 0.16 | 0.07 - 0.49 |
| Odour detection | 0.18 | 0.16 | 0.11 | 0.06 - 0.49 |
| Pharynx/larynx irritation | 0.18 | 0.15 | 0.13 | 0.05 - 0.49 |
| Nose irritation | 0.17 | 0.13 | 0.12 | 0.05 - 0.49 |
| Headache | 0.17 | 0.15 | 0.12 | 0.07 - 0.49 |
| Nose congestion | 0.16 | 0.11 | 0.11 | 0.11 - 0.45 |
| Chest tightness | 0.14 | 0.11 | 0.08 | 0.06 - 0.29 |
There was no significant statistical difference in irritative effects of smokers/non-smokers and male/female. Notwithstanding, a positive association among smoke and odour detection was found as well as a positive association among smoke and pharynx/larynx irritation, chest tightness and, particularly, nose irritation. Multivariate analysis, after adjustment for the potential confounding factors (gender, age, BMI, smoking), showed a no significant statistical association between FA exposure and irritative effects. In addiction, we observed that for subjects exposed to high levels of FA, the probability of irritative effects is higher but no significantly.
Discussion
Formaldehyde exposure is a recognized pollutant in the pathologic anatomy laboratories; our data showed that personal exposures up to three-fold the NIOSH TLV-C (7) might occur, sometimes exceeding even the ACGIH TLV-TWA (6). FA observed exposure levels in the autopsy room were generally lower than those found in the pathologic anatomy laboratories. Nevertheless, in a few cases the FA values were higher than the NIOSH TLV-C (7).
In the pathologic anatomy laboratories we observed environmental FA concentration mean lower than 0.37 mg/m3, founded by Taino et al. (9). Nevertheless, if we consider the personal exposure, we observed values of our post-graduate students that do not differ from the values observed by Taino (9). The ones which resulted to be lower are the values related to the laboratory technicians.
The data recorded in the Laboratory 1 agreed with the findings of Kilburn et al. (10) who found that the concentrations of airborne FA in areas where tissue specimens were prepared and sampled were 0.25–2.3 mg/m3.
Mean and median exposure levels of post-graduate students exceeded the airborne concentrations reported by Orsière et al. (4), and even the NIOSH TLV-C (7). According to the FA levels recorded in the Laboratory 1 (Table 3), even the personal exposure of the post-graduate students working in the Laboratory 1 resulted to be higher than those reported in the other two laboratories, exceeding the ACGIH threshold level (6).
We remarked that workers exposure assessment to FA should be carried out by personal exposure measurement rather than on the basis of indoor levels in order not to underestimate it as indoor measurement could be misleading (11).
Despite the findings of Paustembach et al. (1) and Proietti et al. (12), we found that eye irritation occurred at slightly higher concentrations than those needed to produce nose and throat irritation. Although Kulle (8) estimated the threshold for eye irritation to be between 0.61–1.23 mg/m3, we observed this symptom at lower value, equal to 0.21 mg/m3.
While Kulle (8) and Arts et al. (2) observed sensory irritation at levels of 1.23 mg/m3 and higher, we already found nose congestion, headache and nose irritation at levels of 0.16–0.17 mg/m3, but we agreed with Kulle (8) in order to the value of odour detection. Indeed, we observed a mean value of odour detection equal to 0.18 mg/m3, which was in accordance with the threshold detected in Kulle study (8).
The smell of FA was detected by the 61% of the workers enrolled and their median FA exposure was 0.16 mg/m3 (Table 5) according to the absolute odour threshold that has been shown to be between 0.06 and 0.22 mg/m3 (World Health Organization - WHO (13).
Ryan et al. (14) reported an average FA level of 0.9 mg/m3 for what concern eye irritation and burning nose and eyes in workers exposed. This value is likely to be due to transient exposure peaks. Despite the findings of Ryan, our workers declared to suffer from these symptoms even if they were exposed to maximum FA levels of 0.49 mg/m3. Ryan et al. (14) suggested that transient FA peak concentrations, not detected by work shift long sampling, could be responsible for the health effects reported.
The air collection technique that we used in this study might lead, in fact, to underestimate peak exposures which are likely to be connected with the “sampling” step in the pathologic anatomy laboratories.
We remarked, according to Arts et al. (2), that irritative health effects analysis, based on observations from workplace exposure, could be biased by the simultaneous exposure to contaminants other than FA. The indoor air pollution levels were probably related with the poor ventilation only provided by open windows and doors.
In addition, our study showed irritative effects in more than 50% of the workers enrolled and exposed to FA levels below 0.50 mg/m3. These subjective symptoms may lead to a loss of attention in medical examiners and pathologists, thus increasing the risk of injuries connected with the use of blades and scalpels. We consider that FA constitutes a danger both for health and safety of exposed health officers.
Furthermore, the issue of whether a very low FA exposure level can cause an increase in the allergic sensitivity of the upper airways has to be resolved. Mizuki et al. (15) and Liss et al. (16) suggested that gaseous FA exposure might exacerbate basic allergic symptoms. Moreover people with chemical sensitivity demonstrated worse symptoms after FA exposure with a consequent worsening of asthma. None of our workers suffered for asthma, even if 19% of them related chest tightness.
Despite the findings of Takahashi et al. (17) of workers with episodes of atopic dermatitis related to formaldehyde exposure, none of the workers enrolled, showed this skin irritation.
Considering the observed irritative effects, as well as the potential cancerogenic effect of FA, it is mandatory that its airborne levels should be kept as low as possible.
On this basis, it is essential to draw up environmental monitoring programmes, in order to evaluate occupational exposure and to assess the efficacy of any preventive measure adopted. Indeed, the following prevention measures should be adopted:
- Reduction of the quantities of FA handled in the laboratories;
- Provision to technicians of appropriate masks for the protection of airways (filtering masks with carbon filters);
- Adoption of adequate access procedures to laboratories;
- Banning of non-authorized staff from the laboratories (in particular members of staff subject to particular restriction, i.e. pregnant women etc.);
- Prohibition of use of the cloaks as deposits;
- Installation of dedicated chemical cloaks with aspiration from the bottom and suited filters;
- Installation of a suitable system of forced ventilation that guarantees the correct exchange of the air in the laboratories.
Ethical Considerations
Ethical issues Including plagiarism, Informed Consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc. have been completely observed by the authors.
Acknowledgments
Research conducted with Grant from the University of Bari “Aldo Moro”, Southern Italy. The authors declare that there is no conflict of interests.
References
- 1.Paustembach D, Alarie Y, Kulle T, et al. A recommended occupational exposure limit for formaldehyde based on irritation. J Toxicol Environ Health. 1997;50(3):217–63. 21. [PubMed] [Google Scholar]
- 2.Arts JHE, Rennen MAJ, de Heer C. Inhaled formaldehyde: evaluation of sensory irritation in relation to carcinogenicity. Regul Toxicol Pharmacol. 2006;44(2):144–60. doi: 10.1016/j.yrtph.2005.11.006. [DOI] [PubMed] [Google Scholar]
- 3.International Agency for Research on Cancer Monographs on the Evaluation of the Carcinogenic Risk of Chemicals to Humans (IARC, 2006). No. 88- Formaldehyde, 2-Butoxyethanol and 1-tert Butoxy-2-propanol. [PMC free article] [PubMed] [Google Scholar]
- 4.Orsière T, Sari-Minodier I, Iarmarcovai G, Botta A. Genotoxic risk assessment of pathology and anatomy laboratory workers exposed to formaldehyde by use of personal air sampling and analysis of DNA damage in peripheral lymphocytes. Mutat Res. 2006;16(1–2):605. 30–41. doi: 10.1016/j.mrgentox.2006.01.006. [DOI] [PubMed] [Google Scholar]
- 5.Duhayon S, Hoet P, Van Made-Fabry G, Lison D. Carcinogenic potential of formaldehyde in occupational settings: a critical assessment and possible impact on occupational exposure levels. Int Arch Occup Envir Health. 2007;81:695–710. doi: 10.1007/s00420-007-0241-9. [DOI] [PubMed] [Google Scholar]
- 6.American Conference of Governmental Industrial Hygienists (ACGIH . TLV and BEIs. Cincinnati (OH): Signature Publications; 2009. [Google Scholar]
- 7.National Institute for Occupational Safety and Health, Pocket Guide to Chemical Hazards (NIOSH 2005. Department of Health and Human Services, Centers of Desease Control and Prevention, Publication No.149.
- 8.Kulle TJ. Acute odor and irritation response in healthy nonsmokers with Formaldehyde exposure. Inhal Toxicol. 1993;5:323–32. [Google Scholar]
- 9.Taino G, Strada L, Barbieri D, et al. Valutazione dell’esposizione occupazionale a formaldeide in un laboratorio di anatomia patologica. G Ital Med Lav Erg. 2008;30(3 Suppl 2):126–128. [Google Scholar]
- 10.Kilburn KH, Moro A. Reproductive and maternal effects of formaldehyde (HCHO) in rats. Fed Proc. 1985;44:535. [Google Scholar]
- 11.Ohmichi K, Komiyama M, Matsuno Y, et al. Formaldehyde exposure in a gross anatomy laboratory - personal exposure level in higher than indoor concentration. Environ Sci Pollut Res Int. 2006;13(2):120–4. doi: 10.1065/espr2005.06.265. [DOI] [PubMed] [Google Scholar]
- 12.Proietti L, Sandonã PB, Longo B, Gulino S, Duscio D. Esposizione Occupazionale a formaldeide in un servizio di anatomia patologica. G Ital Med Lav Erg. 2002;24(1):32–34. [PubMed] [Google Scholar]
- 13.World Health Organization (WHO . Environmental Health Criteria 89: formaldehyde. International Programme on Chemical Safety; Geneva: 1989. p. 219. [Google Scholar]
- 14.Ryan TJ, Burroughs GE, Taylor K, Kovein RJ. Video exposure assessments demonstrate excessive laboratory formaldehyde exposures. Appl Occup Environ Hyg. 2003;18(6):450–57. doi: 10.1080/10473220301424. [DOI] [PubMed] [Google Scholar]
- 15.Mizuki M, Tsuda T. Relationship between atopic factors and phisycal symptoms induced by gaseous FA exposure during an anatomy dissection course. Arerugi. 2001;50(1):21–8. [PubMed] [Google Scholar]
- 16.Liss GM, Tarlo SM, Doherty J, et al. Physician diagnosed asthma, respiratory symptoms and associations with workplace tasks among radiographers in Ontario, Canada. Occup Environ Med. 2003;60:254–261. doi: 10.1136/oem.60.4.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Takahashi S, Tsuji K, Okazaki F, et al. Prospective study of clinical symptoms and skin tests reactions in medical students exposed to formaldehyde gas. J Dermatol. 2007;34(5):283–289. doi: 10.1111/j.1346-8138.2007.00274.x. [DOI] [PubMed] [Google Scholar]