Abstract
Background:
The main goal was to address the prevalence of enteric protozoan parasites in rural areas of Bandar-Abbas, southern Iran and to compare the results with the only conducted study in 1978.
Methods:
This descriptive study was performed from 2009 through 2010 on the 565 fecal samples. Formalin-ether concentration technique was performed and the analysis was carried out using Chi-square test in SPSS software version 13.5. Finally, the comparison of our results with the only previous study which was accomplished by Sheiban and Rezaeian in 1978 was done.
Results:
The overall prevalence of the protozoan parasites was 48.8%. However, the prevalence of pathogen parasites was 23%. Previous research in 1978 showed 80.4% infectivity. The most protozoan parasites were Blastocystis hominis (25.53%), Giardia lamblia (17.2%) and Entamoeba coli (15.95%). Previous study in 1978 found Entamoeba coli as the most common protozoa. Our finding revealed that the rate of single infectivity was much higher compared to previous research. The most frequency of infection was in children.
Conclusion:
The remarkable decrease of protozoan parasites is mainly due to progress in health care in the villages; however more effort should be done with the goal of eradicating infectious agents.
Keywords: Enteric protozoan parasites, Prevalence, Iran
Introduction
Water-food borne gastrointestinal infections are considered as a major public health burden worldwide (1, 2). Intestinal protozoan parasites are a major group leading to gastrointestinal infections especially in tropical and subtropical areas (3). There are about 3.5 billion infected people by protozoa and/or helminthes in the world (4) as well as 58 million children suffer from these infections every year (5). Symptoms associated with enteric protozoa include non specific symptoms such as diarrhea, abdominal pain, nausea, vomiting, lack of appetite, weight loss and abdominal distension (5, 6). These infections can be life-threatening in immuncompromised patients and malnourished individuals (5). Although some intestinal parasites such as Giardia lamblia remain as a health problem in developed and developing countries (7) but in the most industrialized countries, there is a decrease in the frequency of parasites by improving health status and standardized control programs (8). Indeed, poor hygienic conditions in developing countries account for the most parasitic infections (8). Climate, poor socioeconomic statues, life style of inhabitants and human behavior are among the other important factors, which can affect the incidence of parasitic infections in these regions (8–10).
Most prevalent locations for occurrence of intestinal parasitic infections are the tropical and sub-tropical areas including rural zones of southern part of Iran (10–12). Main reasons are socio-economic status, geographic factors (6, 13), poverty, lack of sanitation, lack of healthy toilet training, inadequate personal hygiene and lack of water filtration. A previous national research in Iran (2005) revealed that the prevalence of intestinal parasitic infections was estimated 19.3% that 10.9% of them were Giardia lamblia and 1.0% was Entamoeba histolytica (8). Some recent studies in rural and semirural settings of western, northwestern and northeastern of Iran in 2006 (14) and in south of Iran in 2004–2006 (12) showed the most common intestinal protozoa were E. coli and G. lamblia. Other study in 2004 regarding E. histolytica cyst passers in several parts of Iran confirmed the highest rate was seen in southern Iran (10). The only research regarding enteric protozoan parasites in villages of Bandar-Abbas was conducted by Sheiban and Rezaeian in 1978 who found 80.4% infectivity with intestinal parasites in inhabitants of rural areas of Bandar-Abbas (11).
The main goal of the present study was to address the prevalence of enteric protozoan parasites in rural areas of Bandar-Abbas, Iran and to compare the results with the only conducted study, held in 1978.
Materials and Methods
This descriptive study was performed from 2009 through 2010 on the 565 fecal samples. Stool samples were collected in clean cups from inhabitants of four rural areas of Bandar-Abbas including Takht, Goduo, Gishan and Chahestan (Fig. 1). For all participants, the questionnaires were filled which included age, gender, medical history and clinical manifestation (such as diarrhea, abdominal pain, fever, vomiting). Initially, stool samples of each person were checked macroscopically and in the case of diarrhea direct examination was performed in order to detect any motile protozoa. In the next step, 10% formalin was added to the samples as preservative and all samples were carried to Parasitology Laboratory, School of Public Health, Tehran University of Medical Sciences, Tehran, Iran. Formalin-ether concentration technique was performed according to Garcia protocol (15). The smears were monitored by staining with Lugol’s iodine solution for detection of protozoan parasites (15). Samples found positive for protozoan parasites based on their distinctive morphology. The analysis was carried out using Chi-square test in SPSS software version 13.5, with a probability (P) value of <0.05. Finally, the comparison of our results with the only previous study which was accomplished by Sheiban and Rezaeian in 1978 was done (11).
Fig. 1:
The map of Bandar-abbas and the villages
Results
This study was performed in four villages of Bandar-abbas: Takht, Goduo, Gishan and Chahestan. The samples were collected randomly from 565 inhabitants of the mentioned villages, 72 cases (12.7%) had clinical manifestations such as fever, dyspepsia, abdominal pain, diarrhea and vomiting that 38(52.7%) of these cases were infected with protozoan parasites. From 493 people who were without any clinical manifestations, there were 240 (48.7%) infected cases. Out of the 565 samples, 240 were from female and 325 were from male. Of these, 102 female (42.5%) and 174 male (53.5%) were infected with at least one protozoan parasite. Prevalence of G. lamblia was 21% in men and 11.6% in women. In addition, 5.5% of men and 6.2% of women had E. histolytica/dispar.
The age range of people included in this study was 1–68 yr and the most frequency of infections was in the range of 11–15 yr (41.3%). Of note, the most common infections in this range were Blastocystis hominis. The frequencies of the protozoan parasites in different range of ages in 2009 were shown in Table 1. The rate of single and multiple infections was 55.9% and 44.1%, respectively.
Table 1:
Prevalence of intestinal protozoan parasites in different age groups in four villages of Bandar Abbas in 1978 and 2009
| Range of age (year) | E. histolytica/dispar (%) | G. lamblia (%) | E. coli (%) | Blastocystis (%) | I. butschlii (%) | C. mesnili (%) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| 1978 | 2009 | 1978 | 2009 | 1978 | 2009 | 1978 | 2009 | 1978 | 2009 | 1978 | 2009 | |
| 0–5 | 26.5 | 0 | 48.9 | 21.4 | 44.8 | 7.1 | NR* | 28.6 | 2 | 0 | 0 | 0 |
| 6–10 | 28.2 | 4.5 | 28.2 | 34.1 | 55.7 | 20.5 | NR* | 22.7 | 10.3 | 0 | 7.1 | 4.5 |
| 11–15 | 28.1 | 9.8 | 27.6 | 13.1 | 57.7 | 29.5 | NR* | 35 | 9.7 | 3.3 | 13.5 | 1.6 |
| 16–20 | 39.5 | 0 | 25.5 | 0 | 60.4 | 5.6 | NR* | 22.2 | 25.5 | 0 | 4.6 | 0 |
| 21–40 | 42.5 | 6.2 | 30.3 | 15.4 | 61.9 | 0 | NR* | 18.5 | 12.9 | 0 | 9.6 | 0 |
| ≥ 41 | 57 | 5.3 | 17.5 | 5.3 | 75.1 | 5.3 | NR* | 5.3 | 13.5 | 5.3 | 19.6 | 5.3 |
| Total | 34.6 | 5.8 | 28.6 | 17.2 | 59.5 | 15.9 | NR* | 24.6 | 11.3 | 1.6 | 9.5 | 2.1 |
Not Reported
Endolimax nana and Trichomonas hominis have not detected in the present study
The overall prevalence of the protozoan parasites was calculated as 48.8%. The protozoan parasites were B. hominis (25.53%), G. lamblia (17.2%), and E. coli (15.95%).Overall, 110 infected cases (39.9%) in Takht, 42 infected cases (15.2%) in Goduo, 49 infected cases (17.8%) in Gishan and 75 infected cases (27.2%) in Chahestan were detected.
Discussion
In the present study 48.8% of people from rural areas of Bandar-Abbas were infected with at least one enteric protozoan parasite. As we expected, there was a clear decrease in the frequency of the intestinal protozoa in these regions compared to the previous research by Sheiban and Rezaeian, who found 80.4% infectivity with protozoan parasites (11). It is worth mentioning that although prevalence has decreased compared to past, 48.8% prevalence reflects a high frequency of parasites in the region indicating a clear need for more sanitary facilities. Of course the frequency of pathogen genera was about 23%. It is interesting that the present study showed a change in the pattern of the protozoan genera compared to the previous study (11). In the previous study the most common protozoa was E. coli (59.5%), E. histolytica/dispar (34.6%) and G. lamblia (28.6%) (11). Our study confirmed that the most prevalent protozoan was B. hominis compared to 1978 when E. coli was detected as the most common protozoan parasite (11). It should be noted that B. hominis was not reported in 1978 and therefore there is a possibility that this protozoa was also common at that time (Table 1).
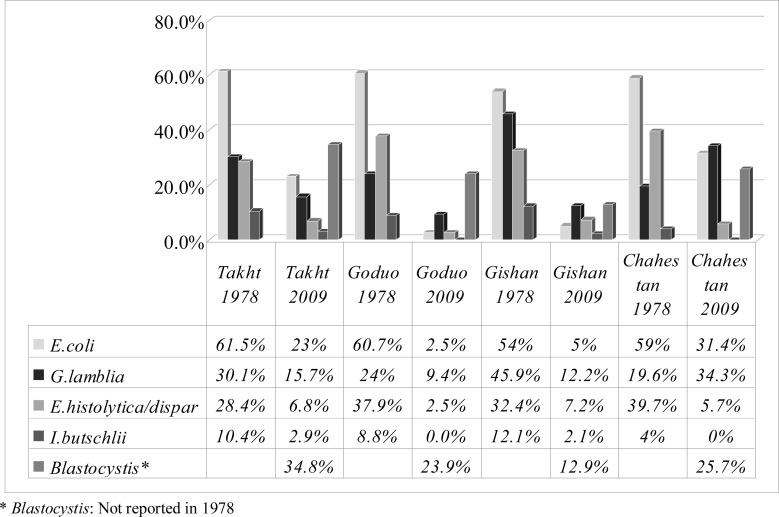
Besides, the prevalence of all kind of parasites has decreased significantly, for example, prevalence of E. histolytica/dispar in Takht changed from 28.4% (11) to 6.38%. Also, in the previous study, there was a high frequency of E. histolytica/dispar in Chahestan and G. lambelia had the highest frequency in Gishan, but in our study B. hominis had the highest frequency in all villages followed by G. lambelia and E. coli respectively. The prevalence of different protozoan parasites in 1978 and 2009 are shown in Fig. 2.
Fig. 2:
Comparison of intestinal protozoan prevalence in four villages of Bandar-Abbas in 1978 and 2009
In previous study, the percentage of single and multiple infections was 32.85% and 63.14%, respectively (11). The difference of percentage of single and multiple infections in 1978 and 2009 was shown in Table 2.
Table 2:
Comparison of single and multiple intestinal protozoan infections in four villages of Bandar-Abbas in 1978 and 2009
| Locality | Total | Infection (%) | ||||
|---|---|---|---|---|---|---|
| Single | Multiple | |||||
|
| ||||||
| 2009 | 1978 | 2009 | 1978 | 2009 | 1978 | |
| Takht | 39.8 | 78.2 | 51.8 | 32.6 | 48.2 | 67.4 |
| Goduo | 15.2 | 81.0 | 73.8 | 20.3 | 26.2 | 79.7 |
| Gishan | 17.8 | 87.8 | 59.2 | 50.8 | 40.8 | 49.2 |
| Chahestan | 27.2 | 79.1 | 50 | 37.0 | 50 | 63.0 |
| Total | 48.8 | 80.4 | 55.9 | 35.1 | 44.1 | 64.9 |
In our study, there was a significant difference between gender and prevalence of disease (P= 0.00). This finding was similar to the previous study of (11).
Although the results of our study showed B. hominis and G. lamblia as the most common parasites, but E.coli also had a high frequency in these regions which followed results of other studies in the other parts of country (12, 14, 16). This is important to note that human behavior, customs and life style of the inhabitants can directly affect the infectious agents of these regions (17). One important explanation regarding the obvious decrease between our result and previous findings in 1978 is the recent progresses in socioeconomic statues in these regions. Three decades ago, the inhabitants of rural area in Bandar-Abbes used to be nomadic without adequate services. Simple transmission rout (oral-fecal) of enteric protozoan parasites coupled with usage of unfiltered water (9) as well as low literacy of inhabitants were all responsible for the high rate of infections in the past 30 yr (11). The findings of Hooshyar et al. suggested that the cyst viability is longer in the tropical zones (10).
There are several studies regarding prevalence of intestinal parasites in different regions of Iran which all revealed that G. lamblia is one of the most common parasites (8, 11, 12, 14, 18). However, there was only one study in rural area of Bandar Abbas (11). A previous study in north of Iran showed prevalence of parasites in apparently healthy people was as follows: Trichostrongylus sp. 6.4%, G. lamblia 3.8%, Cryptosporidium sp. 2.5%, E. coli 2.5%, E. histolytica 1.2% (18). In another study that has been done on 3825 stool specimen from north, south and centre of Iran, E. histolytica was detected in only 1.52% of collected stool samples in microscopically examination which 3.45% of them was E. histolytica by PCR (19). Although in previous studies E. histolytica was one of important and common parasites (8, 14, 15), but according to the present studies we can conclude E. histolytica/dispar has a less important role in protozoan intestinal disease (6, 12–14).
In conclusion, in the past 30 yr, there have been no studies in villages of Bandar Abbas and therefore the present study has been the second one in the region. Epidemiological research conducted regularly is necessary for control and preventive strategy programs. Although the present study showed, a decrease in total prevalence of enteric protozoan parasites but 48.8% prevalence and 23% prevalence of pathogen parasites is still high and there is a clear need for more progress. Inhabitants are in need of more guidance regarding personal and social sanitary precautions. The remarkable decrease of protozoan parasites is mainly due to progress in health care in the villages; however more effort should be done with the goal of eradicating infectious agents.
Ethical Considerations
Ethical issues including plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc. have been completely observed by the authors.
Acknowledgments
This study was carried out as a part of a PhD thesis and was founded by the Tehran University of Medical Sciences. We also would like to thank the help of Miss S. Farnia and F. Tarighi and healthcare providers in all health centers throughout the Hormozgan, Iran. The authors declare that they have no conflicts of interest.
References
- 1.Guarrant RL, Hughes JM, Lima NL, Crane J. Diarrhea in developed and developing countries: magnitude, special settings, and etiologies. Rev Infect Dis. 1990;12(suppl):S41–S50. doi: 10.1093/clinids/12.Supplement_1.S41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Farthing MJG. Giardia lamblia. In: Blaser MJ, Smith PD, Ravdin JI, Greenberg HB, Guerrant RL, editors. Infections of the Gastrointestinal Tract. New York: Raven Press; 1995. pp. 1081–106. [Google Scholar]
- 3.Ravdin JI. Amebiasis. Clin Infect Dis. 1995;20:1453–66. doi: 10.1093/clinids/20.6.1453. [DOI] [PubMed] [Google Scholar]
- 4.Schuster H, Chiodini PL. Parasitic infections of intestine. Current Opinion in Infectious Diseases. 2001;14:587–591. doi: 10.1097/00001432-200110000-00013. [DOI] [PubMed] [Google Scholar]
- 5.Escobedo AA, Almirall P, Alfonso M, Cimerman S, Rey S, Terry SL. Treatment of intestinal protozoan infections in children. Arch Dis Child. 2009;94:478–482. doi: 10.1136/adc.2008.151852. [DOI] [PubMed] [Google Scholar]
- 6.Niyyati M, Rezaeian M, Zahabion F, Hajarzadeh R, Kia EB. A survey on intestinal parasitic infections in patients referred to a hospital in Tehran. Pak J Med Sci. 2009;25(1):87–90. [Google Scholar]
- 7.Mandell GL, Bennett JE, Dolin R. Principles and practice of infectious diseases. 6th ed. New York: Churchill Livingstone Press; 2007. pp. 2888–93. [Google Scholar]
- 8.Sayyari AA, Imanzadeh F, Bagheri Yazdi SA, Karami H, Yaghoobi M. Prevalence of intestinal parasitic infections in the Islamic Republic of Iran. East Mediterr Health J. 2005;11:377–83. [PubMed] [Google Scholar]
- 9.Miné JC, Rosa JA. Frequency of Blastocystis hominis and other intestinal parasites in stool samples examined at the Parasitology Laboratory of the School of Pharmaceutical Sciences at the São Paulo State University, Araraquara. Rev Soc Bras Med Trop. 2008;41(6):565–69. doi: 10.1590/s0037-86822008000600004. [DOI] [PubMed] [Google Scholar]
- 10.Hooshyar H, Rezaian M, Kazemi B, Jeddi-Tehrani M, Solaymani-Mohammadi S. The distribution of Entamoeba histolytica and Entamoeba dispar in northern, central, and southern Iran. Parasitol Res. 2004;94:96–100. doi: 10.1007/s00436-004-1175-8. [DOI] [PubMed] [Google Scholar]
- 11.Sheiban F, Rezaian M. Study on intestinal protozoa in seven villages of Bandarabass. Iranian J Publ Health. 1981;10:1–4. 82. [Google Scholar]
- 12.Haghighi A, Salimi Khorashad A, Nazemalhosseini Mojarad E, Kazemi B, Rostami Nejad M, Rasti S. Frequency of enteric protozoan parasites among patients with gastrointestinal complaints in medical centers of Zahedan, Iran. R Soc of Trop Med and Hyg. 2009;103:452–54. doi: 10.1016/j.trstmh.2008.11.004. [DOI] [PubMed] [Google Scholar]
- 13.Shojaei Arani A, Alaghehbandan R, Akhlaghi L, Shahi M, Rastegar Lari A. Prevalence of intestinal parasites in a population in south of Tehran, Iran. Rev Inst Med Trop S Paulo. 2008;50(3):145–49. doi: 10.1590/s0036-46652008000300003. [DOI] [PubMed] [Google Scholar]
- 14.Solaymani-Mohammadi S, Rezaian M, Babaei Z, Rajabpour A, Meamar AR, Pourbabai AA, et al. Comparison of a stool antigen detection kit and PCR for diagnosis of Entamoeba histolytica and Entamoeba dispar infections in asymptomatic cyst passers in Iran. J Clin Microbiol. 2006;44:2258–61. doi: 10.1128/JCM.00530-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Garcia LS. Diagnostic Medical Parasitology. 4th ed. Washington D.C: ASM Press; 2001. [Google Scholar]
- 16.Zali MR, Jafari Mehr A, Rezaian M, Meamar AR, Vaziri S, Mohraz M. Prevalence of intestinal parasitic pathogens among HIV-positive individuals in Iran. Jpn J Infect Dis. 2004;57:267–80. [PubMed] [Google Scholar]
- 17.Akhlaghi L, Shamseddin J, Meamar AR, Razmjou E, Oormazdi H. Frequency of Intestinal Parasites in Tehran. Iranian J Parasitol. 2009;4(2):44–47. [Google Scholar]
- 18.Daryani A, Sharif M, Meigouni M, Baba Mahmoudi F, Rafiei A, Gholami Sh, Khalilian A, Gohardehi Sh, Mirabi AM. Prevalence of Intestinal Parasites and Profile of CD4+ Counts in HIV+/AIDS People in North of Iran. Pak J Biol Sci. 2009;12:1277–81. doi: 10.3923/pjbs.2009.1277.1281. [DOI] [PubMed] [Google Scholar]
- 19.Nazemalhosseini Mojarad E, Nochi Z, Sahebekhtiari N, Rostami Nejad M, Dabiri H, Zali MR, Kazemi B, Haghighi A. Discrimination of Entamoeba Moshkovskii in patients with gastrointestinal disorders by Single-Round PCR. Jpn J Infect Dis. 2010;63:136–38. [PubMed] [Google Scholar]