Abstract
Background:
Fairness in financial contribution for health was determined by WHO (World Health Report, 2000) as the third goal of health systems which is measured by fairness in financial contribution index (FFCI). The aim of this study was to estimate FFCI and quantify extent of catastrophic household heath expenditures.
Methods:
We conducted a descriptive study during May 2008. Subjects were chosen by “Systematic Random sampling” among residents of Maskan’s population-based research center (Maskan Center) in Kermanshah, Iran. After completing informed consent form, we collected data using a questionnaire by interview with head of family. In order to describing data and estimating FFCI, we used descriptive statistics and WHO methodology, respectively. Households with catastrophic expenditures and impoverished households were defined as those with health expenditures over 40% and 50% of their ability to pay, respectively.
Results:
The mean age of head of families was 48.96±12.86 years. From 189; 12.7% of household’s heads were female. 75.1% of households were covered by at least one health insurance scheme. FFCI was 0.57. The proportion of households facing catastrophic health expenditures was 22.2% (95% CI=16.3%–28.1%)
Conclusion:
The rate of FFCI among participants implied an inequality in health financing contribution. In addition, many of households (22.2%) faced catastrophic health expenditures while according to WHO estimation, the figure in the whole country was 2% in 1999. Our study revealed the importance of protecting households against the costs of ill-health.
Keywords: Fair Financing Contribution Index (FFCI), Catastrophic health expenditures
Introduction
Health systems are responsible not only for improving health status of population but also for responding to people’s expectations and for protecting them against the financial burden of illness (1). A carefully planned health financing system creates revenues for health, meanwhile makes the needed services affordable for people and protects them from devastating costs (2).
Financial fairness implies that the distribution of financial risks households face because of their payments to the health system is based on their capacity to pay not the risks of sickness (1). Ability to pay is the proportion of household income remaining after spending for basic subsistence needs, which is called effective income. It is a more reliable criterion for purchasing power than total income of households (3).
“The concept of fairness in household financial contribution to the health system was introduced by WHO and was defined as an equal burden where every household would pay an equal share of its capacity to the health system. The ratio of a household’s health payments to its capacity to pay is called the household financial contribution (HFC)” (4). In order to measure dispersions from the equal burden criterion, a fairness of financial contribution index (FFCI) was developed. The index varies from 0 to 1, with 1 representing perfect fairness (1).
WHO estimated that FFC score (FFCI) among all member states in 2000 varied between 0.99 in Colombia to 0.46 in Sierra Leone. This index in Iran equals to 0.92 in 2000. Using this index, Iran health system performance in fair financing contribution was ranked at 112–113 between 191 WHO member states (1). In 2003, WHO reported that in Iran, out-of-pocket payments are high, and the poor are not protected from catastrophic costs, as they should, it seems therefore that health system financing is not well equitable (5).
Iranian government has planned for improving equity in health care financing as stated in the Fourth Economic, Social, and Cultural Development Plan (2005–2009). In the mid-1990s the reform to health care financing in Iran started by extending of insurance coverage to uninsured rural and the urban Iranian population (6).
Material and Methods
We conducted a descriptive study and entered 217 households who were chosen by “Systematic Random Sampling” among residents of Maskan’s population-based research center (Maskan Center) in Kermanshah, west of Iran. This center has a population over than 18000 people with a diverse socioeconomic status making our sample representative of Kermanshah’s population. Kermanshah is a province center (Kermanshah province) in west of Iran with a population 1,255,319. After completing informed consent form, we collected data using a questionnaire by interview with household’s head. In the present study the 2003 World Health Survey questionnaire that developed by WHO for assessing health systems performance was used. In the case of developing countries is seem that consumption or even expenditure are better indices of ability to pay than income (7). The recall period for total household expenditure, outpatient services, hospitalization, traditional medicine, dentists, medications, health care products, and laboratory tests was the most recent month. In addition, hospitalization costs in the previous 11 mo were questioned (excluding the most recent month). Based on WHO definition, households with catastrophic expenditures were defined as those with health expenditures above 40% of household’s capacity to pay (8). In order to describing demographic characteristics and the magnitude and distribution of health expenditures, we used descriptive statistics such as frequency, standard deviation, and percentage. The basic indicator of HFC at the household level was estimated. We used WHO methodology for estimating Household Financing Contribution (HFC) as below:
“The health financing contribution of a household (HFCh) is defined as the ratio of total household spending (HS) on health and its total capacity to pay. Capacity to pay was defined as total non-food expenditure.
HFCh can be summarized in the following formula:
(Please note that the subscript h denotes household level data)
The numerator corresponds to total household health expenditure (HSh) which is the sum of prepayment and out-of-pocket (oop) payment to the health system. It can be simplified into the following formula:
The denominator is a measure of the household’s permanent above subsistence income estimated for a household’s total expenditure (EXPh) incremented by adjusted tax payments used on health not already included in total expenditure such as income tax and property tax (aTaxh) and net of food expenditure (Foodh).
From this, the inequality index and the score of fairness in financing are constructed as follows:
The inequality index is based on the mean of the cubed absolute difference between the financial contribution of a given household and the mean of financial contribution of all households in a country (HFC-bar), and normalized by the maximum value of the cubed difference of this fraction (0.125). The score is defined by adjusting the inequality index in the following way to provide a value from which countries may be ranked:
Fairness in financial contribution, or score= 1-(4*II) The score ranges between 0 and 1 and countries with scores tending to 1 have fairer health financing system” (9, 10).
SPSS software version 12.00 was used for data entering and analysis.
Results
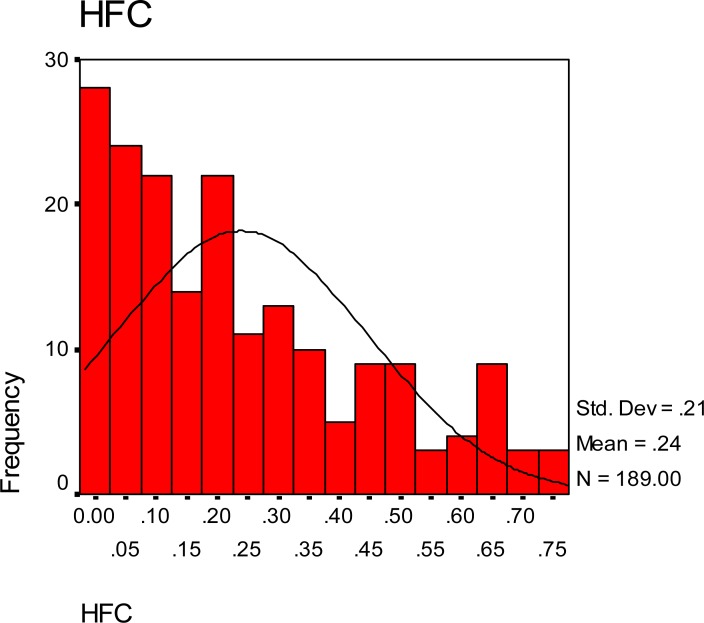
Among 217 households entered in the study, 28 households were excluded because of reporting their income as zero, unusual prepayment based on their occupations or the type of insurance. From 189 households, 12.7% of them were female-headed families. The mean age of head of families was 48.96±12.86 yr and 75% of families were covered by at least one health insurance scheme. Fair financing contribution index was 0.57, which intend to inequality. The mean and median of Household Financing Contribution were 0.23 and 0.18, respectively. As we depicted in figure 1, this measure among 75% of households was lesser than or equal to 0.36 and positively skewed. 22.2% (95%CI= 16.3%–28.1%) of the households (42 households) faced catastrophic health expenditures (Fig.1).
Fig. 1:
Distribution of Household Financing Contribution among subjects
In addition, the rate of families that suffered impoverishment due to health spending was 13.8% (26 households). 39.2% (74 households) had one member younger than 12 yr old, 23.3% (44 households) had at least one member older than 60 yr old, 5.3% of households had at least one member with chronic condition and 24.9% were uninsured. Also, because of financial burden of health expenditures 21.7% of the households sold their jewelry, 15.9% used up their saving such as bank account, 49.2% borrowed money from someone other than a friend or family and 15.3% were supported by family members or friends from outside the household. Table 1 showed the distribution of demographic variables and other baseline characteristics in details among households.
Table 1:
Distribution of demographic variables and other baseline characteristics among households
| Variables | All households (n= 189) n (%) |
|---|---|
| Age mean ± SD | 48.96± 12.86 |
| Sex: Female | 24 (12.7) |
| One member younger than 12 yr old | 74 (39.2) |
| One member older than 60 years old | 44 (23.3) |
| one member with chronic condition | 10 (5.3) |
| Insurance Coverage | 142 (75.1) |
| Complementary Insurance Coverage | 37 (19.6) |
| Households who selling their jewelry | 41 (21.7) |
Discussion
Our results showed that FFC index in kermanshah city was 0.57 which implied an inequality in health financing contribution. The figure is very lower than FFC index for the whole country (0.92) stated in the World Health Report 2000 (1). There is some evidence of inequality in financing that increases the prevalence of catastrophic health expenditure (11).
As stated in WHO report:” from 1980 to 2001 out-of-pocket expenditure has soared from 48% to 58% of the total health expenditure in Iran”(12). According to article 90 of the Act of Iran Fourth Socio-economic Development Plan (2005–2009), FFCI should be improved to 0.90 and share of households facing catastrophic health expenditures should be decreased to 1% until the final year of the plan (13). In order to achieve these goals much should be done at least for our study area. On the other hand, our results showed that 22.2% of the households faced catastrophic health expenditure. A study conducted by Kavosi et al. in Tehran revealed that 11.8% of households faced catastrophic health expenditure in 2006 (14). When comparing the result of our study with Tehran study and other similar studies we should consider that socioeconomic status of Kermanshah is different from other provinces because of Iraq-Iran war (imposed war) effects and economic damage consequences, whereas Tehran is the capital and economic center of Iran. Better economic status decreases the likelihood of facing catastrophic health expenditure (3). Results of a study which carried out in Burkina Faso showed that 6–15% of the households incurred catastrophic payments (15). The rate is 8–14% in Thailand (16). Among 59 countries, the proportion of households facing catastrophic payments varied from less than 0.01% in Czech Republic and Slovakia to 10.5% in Vietnam (3). A survey showed that 11.7% of households in Georgia face catastrophic health expenditures (17).
Since financial considerations prevent many poor households from seeking health care, therefore the findings of our study and similar studies could underestimate the proportion of households face catastrophic costs. P. Sakesna et al. focused on this limitation. They combined the reported out-of-pocket expenditures for patients used needed health services with the predicted out-of-pocket expenditures for patients who did not use health services and estimated the total potential rate of catastrophic health expenditures in Kenya (17).
Evidence suggests that in Iran one of the major problems of health financing which puts burden on the households is high out-of-pocket expenditure (12). The world health report 2006 estimated that total private expenditure on health accounts for 52.7% of total health expenditure. Private finance sources can be seen to constitute a high proportion of total health expenditure in Iran. From an equity point of view, private financing of health care is considered unpleasant (17). On the other hand, out-of-pocket payments constitute 94.8% of private expenditure on health in Iran (18). In other words, nearly 50% of health expenditure is out-of-pocket, which is higher than WHO estimate for developing countries. According to WHO report in 2009 out-of-pocket payments incurred by households for medical services received, are estimated to account for 45% of health expenditure in the developing world (19).
It is useful to consider the problem stated in WHO report: “The widely practiced balance billing and informal payment contribute to the high out-of-pocket expenditure. The informal or under the table payment is due primarily to the public sector doctors owning and running private practices. Sometime patients have to pay to the doctors to obtain consultancies and surgeries in public facilities. Further, retrospective payment mechanisms, especially fee-for-service have since incentives to induce demand for health care, which leads to increased co-payment adding to out-of-pocket expenses. As indicated elsewhere sometimes physicians charge higher fees than the national tariffs-patients have to pay the difference between the bill size and the amount reimbursable by the insurance schemes-a phenomenon called balance billing” (12).
Raising the amount of total health expenditure paid by out-of-pocket payments increases the range of catastrophic costs (3).” High level of out-of-pocket spending for health care has a variety of harmful effects. Some people are deterred from using health services or from continuing treatment because they cannot afford to pay. People who use services may need to cut spending on basic needs such as food, clothing, housing and children’s education to meet health costs” (20, 21). In some cases, households use up their saving, sell assets and incur a debt. Results of our study showed that 49.2% of the households incurred a debt, 21.7% sold their jewelry and 15.9% used up their saving to meet health costs. Inefficiency is among other problems in health financing schemes in Iran. For instance, although the coverage of health insurance is high, the current overlap between diverse health insurance schemes guides to inefficiencies. Furthermore, the weak management between these schemes will lead to duplication of coverage (12).
In conclusion, findings of our study indicate that there are several strategies for improving equity in health care financing and decreasing the extent of catastrophic payments. First, Steps need to be taken for reducing the share of out-of-pocket payments in total health expenditure and increasing reliance on some form of prepayment mechanisms including pooling of risks among different groups within the population. In principle, increasing the share of prepayment in health financing system will decrease the rate of households facing catastrophic payments. Secondly, the more budget should be allocated by the government for health care and efficiency of using existing resources need to be improved. In addition, available funds should be used fairly and proficiently by applying suitable provider payment systems.
Furthermore, health care financing contribution should be distributed based on capacity to pay so that pay for health need not to impoverish households or deter them from obtaining needed care. Finally, financial transparency and accountability in health system should be promoted.
Study Limitations
The indirect costs of seeking care, such as transport, food, accommodation, and lost earnings associated with illness usually do not include in income and expenditure surveys. In addition, some poor households may decrease food expenditures for meeting health care needs; therefore, presented figures could underestimate the reality.
Ethical Considerations
Ethical issues including plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc. have been completely observed by the authors.
Acknowledgments
We would like to thank all of participants whom enrolled in this study for their collaborations. Support was provided by Kermanshah University of Medical Sciences. The authors declare that they have no conflicts of interest.
References
- 1.World Health organization (WHO) The World Health Report 2000. Health Systems: Improving Performance; Geneva: 2000. pp. 35–40. [Google Scholar]
- 2.World Health Organization (WHO) Everybody’s Business: strengthening health systems to improve health outcomes. WHO’s framework for action; Geneva: 2007. pp. 21–22. [Google Scholar]
- 3.Xu K, Evans D, Kawabata K, Zeramdini R, Klavus J, Murray C. Household catastrophic health expenditure: a multicountry analysis. Lancet. 2003;362:111–117. doi: 10.1016/S0140-6736(03)13861-5. [DOI] [PubMed] [Google Scholar]
- 4.Xu K, Klavus J, Evans D, et al. Health systems performance Assessment. World Health organization; 2003. The Impact of Vertical and Horizontal Inequality on the Fairness in Financial Contribution Index; p. 557. [Google Scholar]
- 5.World Health organization (WHO) The world Health Report 2003. Shaping the future; Geneva: 2003. p. 107. [Google Scholar]
- 6.Hajizadeh M, Connelly LB. Equity of Health Care Financing in Iran. Australian Centre for Economic Research on Health; 2009. p. 36. Working Paper No.5. [Google Scholar]
- 7.Ping yu C, Whynes D, Sach T. Equity in health care financing: The case of Malysia. International Journal for Equity in Health. 2000;7(15) doi: 10.1186/1475-9276-7-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health organization, Department of health systems financing . Designing health financing systems to reduce catastrophic health expenditure. Technical briefs for policy makers; 2005. p. 2. No.2. [Google Scholar]
- 9.Murray C, Julio Frenk. A Framework for Health system performance Assessment. WHO; Geneva: 1999. GPE Discussion paper No.6. [Google Scholar]
- 10.Kawabata K, Knaul F, Xu K, Lydon P. WHO fair financing Methodology. WHO; Geneva: 2001. pp. 1–9. [Google Scholar]
- 11.World Health organization . Country Cooperative strategy for WHO and the Islamic Republic of Iran 2005–2009. Regional office for the Eastern Mediterranean; Cairo: 2006. pp. 30–63. [Google Scholar]
- 12.World Health organization, Regional Health systems observatory . Health System profile:Islamic Republic of Iran. 2006. pp. 33–43. [Google Scholar]
- 13.Management and Planning Organization of Iran . Iran Fourth Socio-Economic Development Act. Government of Islamic Republic of Iran; Tehran: 2004. p. 114. [Google Scholar]
- 14.Kavosi Z, Rashidian A, Pourmalek F, Majdzadeh R, Pourreza A, Mohammad K, Arab M. Measuring household exposure to catastrophic health care expenditures: a Longitudinal study in Zone 17 of Tehran. Hakim Research Journal. 2009;12(2):38–47. [Google Scholar]
- 15.SU T, Kouyate B, Flessa S. Catastrophic expenditure for health care in a low-income society: a study from Nouna District, Burkina Faso. Bulletin of the World Health Organization. 2006;84:21–27. doi: 10.2471/blt.05.023739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Limwattanon S, Tangcharoensathien V, Parkongsai P. Catastrophic and Poverty impact of health payments: results from national household survey in Thailand. Bulletin of the World Health Organization. 2007;85:600–606. doi: 10.2471/BLT.06.033720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gotsadze G, Zoidze A, Rukhadze N. Household Catastrophic health expenditure: evidence from Georgia and its policy implications. BMC Health Service Research. 2009;9:69. doi: 10.1186/1472-6963-9-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.World Health Organization (WHO) the World Health Report 2006: working together for health. Geneva: 2006. Statistical annex; pp. 178–189. [Google Scholar]
- 19.Chunling Lu, chin Brian, Li Guohong, Christopher JL. Limitations of methods for measuring out-of-pocket and catastrophic private health expenditure. Bulletin of the World Health Organization. 2009;87:238–44. doi: 10.2471/BLT.08.054379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.World Health Organization Paying for Health Services. 2007. Fact sheet No 320.
- 21.World Health Organization . Toolkit on monitoring health systems strengthening: Health systems financing. Geneva: 2008. p. 6. [Google Scholar]