Abstract
Background:
The need to provide high quality prenatal care services, which take account of women’s views and specifically address their need for information, support and communication, has been advocated and group prenatal care, had been suggested as one of the ways to achieve this objective. The purpose of this study was to examine the impact of group versus individual prenatal care on satisfaction and prenatal care use.
Methods:
This was a cluster-randomized controlled trial with the health center as the randomization unit that conducted in 2007. Satisfaction was measured through a standardized questionnaire, and the Kotelchuck Adequacy of Prenatal Care Utilization Index was used to measure prenatal care utilization.
Results:
We recruited 678 women (group prenatal care, (N= 344) and individual prenatal care, (N=334) in the study. Women in group prenatal care model were more satisfied than women in individual prenatal care model in all areas evaluated, including information, communication, co-ordination and quality of care. Group care women were significantly more likely to have adequate prenatal care than individual care women were (OR=1.35 95% CI=1.26–1.44).
Conclusions:
Group prenatal care was associated with a significant improvement in client satisfaction and prenatal care utilization. This model of care has implications for the planning and provision of prenatal services within public health system, which is moving toward a better quality health care, and increasing use of services.
Keywords: Group prenatal care, Satisfaction, Prenatal care utilization
Introduction
Despite a decline in infant mortality rate, neonatal mortality rate is still high in Iran (1). Preterm birth and low birth weight are the main cause of death in newborn babies worldwide (2) and in Iran (3–5). As the health of the newborn infant is inexorably tied to the health of the mother, strategies to improve the health and care of women are also expected to improve both pregnancy and neonatal health outcomes (6). One strategy that has been implemented recently and had positive impact on neonatal outcomes including preterm birth and low birth weight is group prenatal care (7, 8). Group prenatal care is designed to address the recommended content for optimal care, and as such is designed to improve the quality of care and consequently perinatal outcomes (9).
The project reported here was a special component of a randomized controlled trial, to evaluate group prenatal care model. The primary hypotheses tested were that group care model, was more effective than the individual model with regard to specified maternal and perinatal end-points among singleton pregnancies. Satisfaction with care was also measured as it is recognized as an important and valid indicator of the quality of care (10–12). Measures of social acceptance in terms of satisfaction may be more relevant than mortality and morbidity when evaluating alternative methods of providing health care (11). Satisfaction is a major determinant of health service utilization in general (13). Lack of satisfaction with quality of care could be a major demotivating factor in the use of maternity care facilities (14).
Previous studies looking at patient satisfaction with prenatal care illustrate the importance of examining the subjective, interactional aspects of care. Mothers who are treated with respect, courtesy and dignity, and have trusting relationships with their care providers are more likely to be satisfied with the obstetric care and women respond more favorably to patient-centered care (15), lack of involvement in decision making and inadequate information and education about the care are associated with dissatisfaction (15,16).
The purpose of this study was to assess whether a group prenatal care model, was associated with greater satisfaction for women than the individual model of prenatal care. Our hypothesis is that such program can increase patient satisfaction, an important component of quality in primary care and more satisfaction can lead to more prenatal care use.
Materials and Methods
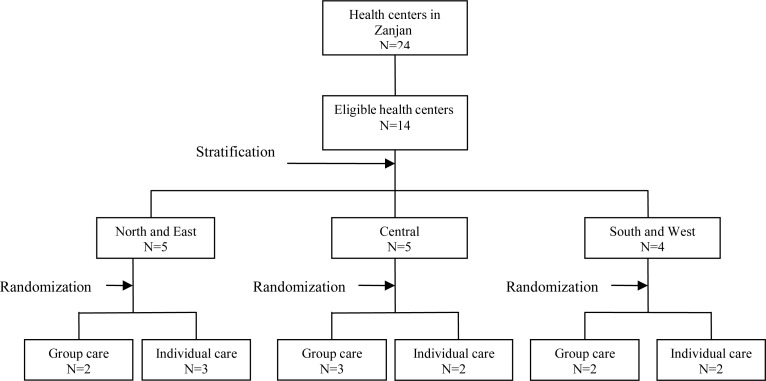
This was a cluster randomized controlled trial where the health center was the unit of randomization. The experimental group received group prenatal care and the control group received routine individual prenatal care that was the standard for the country. Zanjan was chosen as the study area. Zanjan, a city with population of around 500000 is located in the north-western region of the country. Reproductive and child health services are provided by approximately 24 public health centers in this city. In maternal health units, midwives provide prenatal and postnatal care. The services are free of charge, including free supplies of all types of supplement for pregnant women. The normal practice is for women to register for care at the nearest health center. The eligibility criteria for health centers were as follows. Each health center had to be able to provide at least 12 new patients in a period not longer than 1 mo. Intervention and control health centers had to be in the same geographical area, because they serve similar populations with regard to socio-demographic factors. Of the 24 public health centers in the city, 10 were excluded from the study because they could not provide 12 new patients in a period of 1 mo. The 14 health centers were stratified by geographical area (north and east, south and west, central) and then allocated by simple randomization within strata to the group prenatal care (N= 7) or individual prenatal care (N= 7) (Fig. 1). Women in health centers that implemented the group model were informed about the study at the booking visit. All women underwent written informed consent. Before the trial, midwives from intervention health centers participated in workshops to upgrade their knowledge and skills about the group care model they would implement. All health centers were supported and supervised by the same team during the trial. There were no additional personnel introduced into the health centers for the purpose of the trial. The women and caregivers were aware of their allocated care model.
Fig. 1:
Study design of does group prenatal care affect satisfaction and prenatal care utilization in Iranian pregnant women?
Ethical consideration
The Ethical Committees of the Tehran University of Medical Sciences approved the study.
Intervention
The model in the control health centers was the prenatal care currently offered, following guidelines formally recommended by Iranian Ministry of Health and Medical education based on the traditional western model. Clinical activities and laboratory tests were done routinely and oral iron and multivitamin supplementation were provided to all women in both models. In the intervention health centers with regard to group prenatal care, 1 to 2 groups per month were started at each health center. Each group consisted of 8 to 10 women who meet 10 times during the pregnancy for 90 to 120 min per session. Over ten sessions, group discussions focused sequentially on education and skills-building specific to prenatal and postpartum care. Group procedures promoted self-care activities and taught women to track actively changes associated with pregnancy. All prenatal care occurs within the group setting except for the initial medical assessment and medical concerns involving the need for privacy.
Groups were facilitated by a midwife trained in group prenatal care model. When group care started, at first participants engaged in self-care activities of weight and blood pressure assessment; they recorded their own results in their medical records. Then, the midwife completed individual prenatal assessments during the first 30 min of each session. Session themes included: 1) prenatal nutrition and fetal development, 2) common discomforts of pregnancy, 3) relaxation and labor, 4) pregnancy problems 5) the birth experience, 6) decisions of pregnancy and developing a birth plan, 7) infant feeding, 8) postpartum adjustment, 9) new baby care, and 10) baby and mother care. Providers were trained in a facilitative process, such that group sessions were not didactic lectures but rather an integrated discussion with input from health care providers as well as women.
Data collection
All women booking for prenatal care in the 14 health centers between May 2007 and July 2008 and fulfilled the inclusion criteria were eligible for recruitment into the trial. Inclusion criteria were: 1) pregnancy at less than 24 wk’ gestation; 2) no severe medical problems necessitating individualized case management as a high-risk pregnancy (e.g., diabetes, hypertension); and 3) willingness to participate in a randomized clinical trial.
Satisfaction with prenatal care was measured by using a standardized, closed-ended questionnaires consisted of 24 questions that were prepared based on the most recommended dimensions in a satisfaction survey in prenatal care (17–20) and the aspects of prenatal care that were expected to change as a result of the intervention (i.e., communication, quality of care, organization of care and information provision regarding maternal and perinatal health and complications). Responses to statements of satisfaction were measured on a four-point Likert scale, ranging from very satisfied (score 4) to somewhat satisfied (3), somewhat dissatisfied (2), and very dissatisfied. Possible scores range from 24 to 96. The instrument was developed in English, translated into Persian, and reviewed by three experts for clarity and cultural sensitivity; recommended changes were implemented in the questionnaire. The interview questionnaire was pilot tested and the results of the pilot testing were used to revise the questionnaire for unclear wording or ambiguity. The internal consistencies of the dimensions were examined using Cronbach’s alpha it ranged from 0.89 to 0.93 for the four factors. Cronbach’s alpha for the overall satisfaction scale was 0.91.
Because women needed to be sufficiently exposed to prenatal care in order to form their own opinion on the quality of care they had received, we administered the questionnaire to women at 34–36 wk of gestational age. The women were surveyed in a private environment, in approximately 20 min.
Adequacy of prenatal care utilization was calculated using Kotelchuck’s Adequacy of Prenatal Care Utilization (APNCU) Index (21). This index combines the timing of prenatal care initiation and the frequency of visits received after initiation (adherence). In the APNCU Index, women are classified as “Adequate Plus” if they began prenatal care by the 4th month of pregnancy and the woman made 110% or more of the expected visits; “Adequate” if prenatal care had begun by the 4th month and the woman made 80–109% of the expected visits; “Intermediate” if prenatal care had begun by the 4th month and the woman made 50–79% of the expected visits; and “Inadequate” if prenatal care began after the 4th month or the woman made less than 50% of the expected visits. The number of expected visits is based on the American College of Obstetricians and Gynecologists prenatal care visitation standards. The Kotelchuck APNCU Index was used to classify prenatal care utilization as adequate (Adequate Plus and Adequate groups combined), intermediate and, inadequate. Trained midwives who were independent of care and blinded to study assignment did structured interviews.
Data analysis
Differences in background characteristics between the two groups were examined by Student’s t-test and the chi-squared test. We used the generalized estimating equations model with STATA version SE.10 with identity link function and Gaussian distribution for calculating mean differences in satisfaction items and 95% CI and adjusting for clustered randomization. For adequacy of prenatal care, we used the generalized estimating equations model with logit link function and exchangeable correlation for calculating OR and 95% CI. P value, adjusted OR, mean differences and 95% CI were reported.
Results
Seven clinics were assigned the group care model and seven the individual care. Of 735 eligible women, 678 enrolled in the study (92% participation rate). Three hundred forty four women started care in the health centers providing the group care model and 334 women in health centers assigned the individual model. In the group prenatal care group 14 (4.1%) women had a miscarriage or fetal death and 7 (2%) could not be traced. The corresponding figures in the individual care group were 12 (3.6%) and 12 (3.6%) women. Three multiple pregnancy in group care model and two multiple pregnancy in individual care model were excluded and finally 320 women in intervention group and 308 women in control group were interviewed.
Eighty eight percent of the women were between 20 and 35 yr of age, 8.7% were under age 20, and approximately 3.3% were 36 yr old or older. Forty seven percent were nulliparous. Educational level of 48% of women was high school and more. There was no difference in age, parity, literacy, gestational age at booking, BMI (Body Mass Index), and reproductive history by model (Table 1).
Table 1:
Demographic and obstetrics characteristics of women in group and individual prenatal care
| Characteristic | Group care n=320 | Individual care n=308 | □ | □ |
|---|---|---|---|---|
|
| ||||
| n (%) | n (%) | t statistic or X2 | P | |
| Literacy | ||||
| Primary | 92 (28.8) | 95 (30.8) | ||
| Secondary | 68 (21.3) | 70 (22.7) | 1.2 | 0.75 |
| High school | 115 (35.9) | 98 (31.8) | ||
| University | 45 (14.1) | 45 (14.6) | ||
| Parity | ||||
| Primiparous | 151 (47.2) | 145 (47.1) | ||
| Multiparous | 169 (52.8) | 163 (52.9) | 0.001 | 0.52 |
| Age* | 26 (5) | 26.3 (4.7) | 0.467 | 0.49 |
| Pregnancy BMI(kg/m2) * | 24.2 (4.2) | 24.6 (4.3) | 1.27 | 0.26 |
| Gestational age at booking* | 3 (1.1) | 3.1 (1) | 0.79 | 0.37 |
| Preterm labor history** | 8 (4.7) | 10 (6.2) | 0.38 | 0.35 |
| Still birth history** | 7 (4.1) | 6 (3.6) | 0.04 | 0.52 |
| Miscarriage history | 42 (13.1) | 32 (10.3) | 1.22 | 0.32 |
| Neonatal death history** | 8 (4.7) | 11 (6.8) | 0.66 | 0.48 |
Mean (SD),
Multiple women only
Group prenatal care appeared to have great impact on satisfaction during prenatal period. In terms of the mean item score women in group care were very satisfied with prenatal care services and women in individual care group were somewhat satisfied (mean item score= 3.8, SD= 0.20 for group care and mean item score= 3.01, SD= 0.31 for individual care P< 0.000). In all measures (received information during prenatal care, co-ordination of care, relationship with provider and quality of care) women in the group care were more satisfied than women in the individual care group (Table 2). They felt better informed about labor and delivery, caring for own health during pregnancy, family planning, care of newborn, nutrition during pregnancy, problem during pregnancy, medical procedures and tests during prenatal visits and breast-feeding (Table 2). They were also more likely to say provider listen to their problem and answer their questions, their care during pregnancy was provided in a supportive and confident way, and they were more satisfied with friendliness and concern shown by providers in their feeling (Table 2). Women of group care were more satisfied with amount of time the provider spent with them during prenatal visits, arrangements for making appointments for prenatal visits and waiting time. In term of quality of care women in group care were more satisfied with completeness of their physical exam, competence of provider and overall quality of prenatal care (Table 2).
Table 2:
Women’s satisfaction with prenatal care according to prenatal care model
| Item |
Group care n=320 Mean (SD) |
Individual care n=308 Mean (SD) |
Cluster adjusted mean difference (95% CI) | P |
|---|---|---|---|---|
| Information received about: | ||||
| Labor and delivery | 3.85 (0.07) | 2 (0.05) | 1.85 (1.66–2.03) | <.0001 |
| Caring of their own health | 3.85 (0.07) | 2.69 (0.07) | 1.16 (0.95–1.37) | <.0001 |
| Family planning | 3.85 (0.06) | 2.56 (0.07) | 1.29 (1.08–1.49) | <.0001 |
| Caring of newborn | 3.83 (0.05) | 1.96 (0.05) | 1.86 (1.71–2.02) | <.0001 |
| Nutrition | 3.92 (0.04) | 3.03 (0.06) | 0.89 (0.73–1.05) | <.0001 |
| Problem during pregnancy | 3.84 (0.07) | 2.76 (0.08) | 1.08 (0.83–1.33) | <.0001 |
| Medical procedure and tests | 3.86 (0.05) | 2.27 (0.05) | 1.59 (1.44–1.74) | <.0001 |
| Breastfeeding | 3.88 (0.05) | 2.77 (0.06) | 1.12 (0.94–1.29) | <.0001 |
| Communication | ||||
| Listening to women’s problems | 3.89(0.06) | 3.02 (0.09) | 0.87 (0.62–1.12) | <.0001 |
| Answering women’s questions | 3.87 (0.07) | 2.83 (0.08) | 1.04 (0.87–1.31) | <.0001 |
| Courtesy and respect | 3.82 (0.03) | 3.8 (0.03) | 0.02 (−0.07–0.11) | 0.704 |
| Friendliness | 3.71 (0.06) | 3.36 (0.09) | 0.36 (0.12–0.59) | 0.003 |
| Manner of talking with women | 3.84 (0.03) | 3.75 (0.03) | 0.08 (−0.01–0.17) | 0.082 |
| Reassurance and emotional support | 3.64 (0.08) | 3.13 (0.11) | 0.51 (0.22–0.79) | 0.001 |
| Interest shown in women’s feeling | 3.57 (0.07) | 3.23 (0.09) | 0.34 (0.09–0.59) | 0.007 |
| Comfort during examination | 3.47 (0.09) | 3.23 (0.06) | 0.24 (0.06–0.41) | 0.008 |
| Co-ordination | ||||
| Time spent during care | 3.97 (0.01) | 3.12 (0.05) | 0.84 (0.73–0.96) | <.0001 |
| Arrangement for making appointment | 3.92 (0.01) | 3.04 (0.04) | 0.89 (0.79–0.98) | <.0001 |
| Waiting time | 3.86 (0.03) | 2.86 (0.05) | 1 (0.89–1.13) | <.0001 |
| Quality | ||||
| Overall quality of care | 3.82 (0.03) | 3.18 (0.07) | 0.64 (0.5–0.77) | <.0001 |
| Competence of provider | 3.66 (0.05) | 3.3 (0.08) | 0.34 (0.19–0.52) | <.0001 |
| Completeness of physical exam | 3.76 (0.04) | 3.18 (0.07) | 0.58 (0.43–0.72) | <.0001 |
| Overall relationship during care | 3.68 (0.06) | 3.21 (0.07) | 0.47 (0.38–0.56) | <.0001 |
| General satisfaction | 3.79 (0.03) | 3.18 (0.07) | 0.61 (0.46–0.74 | <.0001 |
Although in both models about 92% of the women initiated prenatal care by the 4th mo of pregnancy (average month of initiation was 3 mon in both models), only 37.3% of the women in individual group care received the specified number of prenatal visits (adequacy of received services). This figure for women in group care model was 70.3% that indicated group care model motivate women more likely to come to prenatal visits (Table 3).
Table 3:
Adequacy of prenatal care utilization according to prenatal care model
| APNCU Index | Group care n=320 | Individual care n=308 | Cluster adjusted OR (95%CI) | P |
|---|---|---|---|---|
| n (%) | n (%) | |||
| Adequacy of initiation | 297 (92.8) | 283(91.9) | 0.99 (0.95–1.04) | 0.68 |
| Adequacy of received services | 225 (70.3) | 115(37.3) | 1.39 (1.33–1.46) | <.0001 |
| Overall adequacy | 212 (66.3) | 113 (36.7) | 1.35 (1.26–1.44) | <.0001 |
Discussion
This study showed that the new model increased women’s satisfaction with group care compared with standard care. These findings confirmed those in other trials of group prenatal care (7, 22). The differences in satisfaction between the two groups were most obvious with information dimension.
Group care permits substantially more time compared to individual prenatal care (e.g., 120 min vs. 15 min for each visit, or 20 h vs. 1.5 h throughout the prenatal period, respectively). This provides important opportunities to gain truly the experience, knowledge, and skills necessary for a healthy pregnancy and childbirth (23).
Research revealed that women want education about what to expect during the pregnancy with respect to changes in their bodies, procedures and tests involved in prenatal care and what to expect from labor and birth (24). Lack of information and explanation during prenatal care has been associated with dissatisfaction (15, 25–27). In the current study, participants were more satisfied when their providers spent more time with them and when their providers engaged them by listening to their problems, answering their questions and interest shown in their feeling. The importance of communication in patient satisfaction with prenatal care has been repeatedly shown in prior studies of pregnant women’s satisfaction (24, 28–30). Furthermore patient-centered communication is considered a component of high-quality health care (31) and is linked to better medical adherence and outcomes (32, 33).
The women in group care gained a feeling of reassurance and emotional support through knowledge and information, and through the relationship with the care provider and other participants in group. Group prenatal care empowers women by valuing the knowledge and experience each woman brings to the group, and increases this knowledge through skills building and education. They gain confidence to conduct self-assessments, make decisions about all aspects of care, devise solutions to problems, validate and support each other in this process, and take responsibility for their own health during pregnancy and beyond. They are more confident and assured in their labors. This model of care promotes the development of a social network of pregnant women for information and emotional support. In this exciting time of growth and development, sharing with other women provides support and confirmation (23).
Social support during pregnancy not only affected satisfaction with care (26, 34, 35), but had long-term, health-promoting effects for women and could improve maternal psychosocial outcomes (34, 36).
The questions used to explore women’s satisfaction with courtesy and respect, and manner of talking with them during prenatal care showed high levels among women in both models, this could be due to a “courtesy bias”, which usually affects the answers to inquiries about satisfaction with care received, especially when women are asked in clinical settings (37).
Waiting time emerged as an important predictor of satisfaction and long waiting time has been associated with dissatisfaction with care. (38–40). Although this aspect of care was not measured in any objective way, women in group care were more satisfied with waiting time and arrangement for making appointment than women in individual care group. Group care model has ten defined 2 h sessions implemented from weeks 16 through 40 of pregnancy and groups start and end on time, so that patients do not think that their time is wasted by long waits. Instead, their time is spent communicating and building trust between patients and providers (23). In a fast-paced world with many competing demands, valuing a woman’s time by decreasing her wait at health care appointments is essential to ensuring her satisfaction with the care experience (29).
More women in group care model were satisfied with completeness of physical exam during care and competence of provider. The new role for midwives in taking responsibility for providing prenatal care in group setting might have motivated them being more careful in their approach to routine physical aspect of care. Another interpretation may be that women may perceive medical care to be better when they engage in self-care activities and when caregivers take time to explain things and their care are supportive and encouraging. Increasing women’s use of prenatal care remains a key strategy for improving both maternal (41) and infant outcomes, particularly among term infants (42). In addition, more adequate use of prenatal care is associated with more appropriate use of pediatric care (43).
Although major gains have been made since the last two decades in the proportion of mothers receiving prenatal care in Iran, a significant portion of women still fail to obtain adequate prenatal care (44, 45). In this study, group mothers were significantly more likely to have adequate care compared with women in individual care. The increased attendance at prenatal care may be reflective of an active environment with peer interaction. Furthermore, successful communication was seen as promoting prenatal care use, whereas unsuccessful communication made women less likely to come to prenatal care visits (33, 46).
Social support during pregnancy improves prenatal care use (47, 48). In addition, satisfaction with prenatal care motivates pregnant women to seek and continue prenatal care whereas dissatisfaction with prenatal care services results in decreased utilization (48–50).
Limitation
Our study has limitations inherent to satisfaction studies. One is the tendency of respondents to answer positively to questions about satisfaction because of reluctance to criticize their care providers (51). This bias is a possible problem in our study, as the interviews were conducted within health centers. However, we attempted to minimize it by conducting interviews in a separate room independent of the health care providers and with adequate assurance of confidentiality of information.
The participants in this study were selected because of their low-risk status. We have no reason to suspect that these results would not be generalizable to other settings that care for women of variable-risk status. It is possible that some of the issues perceived by women to be better addressed in group prenatal care model might be even more important to women of higher risk status, such as received information and support during prenatal care.
In conclusion, increasing attention should be given to patients’ views in health care evaluation. Policymakers and program managers should know that women’s views are determinant in greater acceptance and sustained use of services. This paper describes the women’s perceptions of two prenatal care models within a public health sector setting. Our results show that group prenatal care model is accessible and convenient, and group care women reported higher satisfaction and had more adequate prenatal care use than control women. This model of care has implications for the planning and provision of prenatal services within public health system, which is moving toward a better quality health care, and increasing use of services.
Ethical Consideration
All Ethical issues (such as informed consent, conflict of interest, plagiarism, misconduct, co-authorship, double submission, etc) have been considered carefully.
Acknowledgments
The authors gratefully acknowledge the Institutional Review Board of the Tehran University of Medical Sciences, which approved and financially supported this project. We thank all the women who participated in the trial for their willingness to cooperate and the midwives in the health centers for their cooperation. The support received from Dr Azemikhah Head of the Bureau of Mother’s health was important for the successful conduct of the study.
References
- 1.Anonymous . Reproductive health indicators database, all indicators per country/region. World Health Organization (WHO); 2008. Available from: http://www.who.int/reproductiveindicators/countrydata.asp?page=108. [Google Scholar]
- 2.Lawn JE, Cousen S, Zupan J. Four million neonatal deaths: when? where? why? Lancet. 2005;365:891–900. doi: 10.1016/S0140-6736(05)71048-5. [DOI] [PubMed] [Google Scholar]
- 3.Amani F, Barak M, Aminisani N, Dehghan MH. Neonatal mortality and its related factors in hospitals of Ardabil. Journal of Ardabil University of Medical Sciences and Health Services. 2006;4(5):305–310. [Google Scholar]
- 4.Hematyar M, Yarjou S. Causes of perinatal mortality at Javaheri hospital during a 7 years period. Medical Science Journal of Islamic Azad University, Tehran Medical Unite. 2005;1(15):37–40. [Google Scholar]
- 5.Nayeri F, Amini E, Oloomi Yazdi Z, Dehghan Naieri A. Evaluation of the cause and predisposing factors in neonatal mortality by using international coding diseases version 10 in Valiasr Hospital. Iranian Journal of Pediatrics. 2007;1(17):21–6. [Google Scholar]
- 6.Bhutta ZA, Darmstadt GL, Hasan BS, Haws RA. Community-based interventions for improving perinatal and neonatal health outcomes in developing countries: A review of the evidence. Pediatrics. 2005;115(2):519–617. doi: 10.1542/peds.2004-1441. [DOI] [PubMed] [Google Scholar]
- 7.Ickovics JR, Kershaw TS, Westdahl C, Rising SS, Klima C, Reynolds H. Group prenatal care and preterm birth weight: results from a matched cohort study at public clinics. Obstet Gynecol. 2003;102:1051–57. doi: 10.1016/s0029-7844(03)00765-8. [DOI] [PubMed] [Google Scholar]
- 8.Ickovics J, Kershaw T, Westdahl C, Magriples U, Massey Z, Reynolds H, Rising SS. Group prenatal care and perinatal outcomes: A randomized controlled trial. Obstet Gynecol. 2007;110(2, Part 1):330–39. doi: 10.1097/01.AOG.0000275284.24298.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rising SS, Kennedy HP, Klima CS. Redesigning prenatal care through Centering Pregnancy. J Midwifery Womens Health. 2004;49:398–404. doi: 10.1016/j.jmwh.2004.04.018. [DOI] [PubMed] [Google Scholar]
- 10.Donabedian A. The quality of care: how can it be assessed? Journal of American Medical Association. 1988;260:1743–48. [Google Scholar]
- 11.Avis M, Bond M, Arthur A. Satisfying solutions? A review of some unresolved issues in the measurement of patient satisfaction. J Adv Nurs. 1995;22:316–22. doi: 10.1046/j.1365-2648.1995.22020316.x. [DOI] [PubMed] [Google Scholar]
- 12.Merkouris A, Ifantopoulos J, Lanara V. Patient satisfaction: a key concept for evaluating and improving nursing services. J Nurs Manag. 1999;7:19–28. doi: 10.1046/j.1365-2834.1999.00101.x. [DOI] [PubMed] [Google Scholar]
- 13.Aldana JM, Piechulek H, Al-Sabir A. Client satisfaction and quality of health care in rural Bangladesh. Bull World Health Organ. 2001;79(6):512–17. [PMC free article] [PubMed] [Google Scholar]
- 14.Simkhada B, Van Teijlingen ER, Porter M, Simkhada P. Factors affecting the utilization of antenatal care in developing countries: systematic review of the literature. J Adv Nurs. 2008;61(3):244–60. doi: 10.1111/j.1365-2648.2007.04532.x. [DOI] [PubMed] [Google Scholar]
- 15.Harriott EM, Williams TV, Peterson MR. Childbearing in U.S. military hospitals: dimensions of care affecting women’s perceptions of quality and satisfaction. Birth. 2005;32:4–10. doi: 10.1111/j.0730-7659.2005.00342.x. [DOI] [PubMed] [Google Scholar]
- 16.Brown S, Lumley J. Satisfaction with care in labor and birth: a survey of 790 Australian women. Birth. 1994;21:4–13. doi: 10.1111/j.1523-536x.1994.tb00909.x. [DOI] [PubMed] [Google Scholar]
- 17.Erci B, Ivanov L. The relationship between women’s satisfaction with prenatal care service and the characteristics of the pregnant women and the service. Eur J Contracept Reprod Health Care. 2004;9:16–28. doi: 10.1080/13625180410001696241. [DOI] [PubMed] [Google Scholar]
- 18.Omar MA, Schiffman RF, Raymond Bingham C. Development and testing of the patient expectations and satisfaction with prenatal care instrument. Res Nurs Health. 2001;24:218–29. doi: 10.1002/nur.1024. [DOI] [PubMed] [Google Scholar]
- 19.Raube K, Handler A, Rosenberg D. Measuring satisfaction among low-income women: A prenatal care questionnaire. Matern Child Health J. 1998;2(1):25–33. doi: 10.1023/a:1021841508698. [DOI] [PubMed] [Google Scholar]
- 20.Smith L. The WOMB (WOMen’s views of Birth) antenatal satisfaction questionnaire: development, dimensions, internal reliability, and validity. Br J Gen Pract. 1999;49:971–75. [PMC free article] [PubMed] [Google Scholar]
- 21.Kotelchuck M. An evaluation of the Kessner Adequacy of Prenatal Care Index and a proposed Adequacy of Prenatal Care Utilization Index. Am J Public Health. 1994;84(9):1414–20. doi: 10.2105/ajph.84.9.1414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Grady MA, Bloom KC. Pregnancy outcomes of adolescents enrolled in a Centering Pregnancy program. J Midwifery Women Health. 2004;49:412–20. doi: 10.1016/j.jmwh.2004.05.009. [DOI] [PubMed] [Google Scholar]
- 23.Massey Z, Rising SS, Ickovics J. Centering Pregnancy group prenatal care: promoting relationship-centered care. JOGNN. 2006;35:286–94. doi: 10.1111/j.1552-6909.2006.00040.x. [DOI] [PubMed] [Google Scholar]
- 24.Handler A, Raube K, Kelly M, Giachello A. Women’s satisfaction with prenatal care settings: A focus group study. Birth. 1996;23:31–7. doi: 10.1111/j.1523-536x.1996.tb00458.x. [DOI] [PubMed] [Google Scholar]
- 25.Fraser DM. Women’s perceptions of midwifery care: a longitudinal study to shape curriculum development. Birth. 1999;26:99–107. doi: 10.1046/j.1523-536x.1999.00099.x. [DOI] [PubMed] [Google Scholar]
- 26.Hildingsson I, Radestad I. Swedish women’s satisfaction with medical and emotional aspects of antenatal care. J Adva Nurs. 2005;52(3):239–49. doi: 10.1111/j.1365-2648.2005.03584.x. [DOI] [PubMed] [Google Scholar]
- 27.Korenbrot CC, Wong ST, Stewart AL. Health promotion and psychosocial services and women’s assessments of interpersonal prenatal care in medicaid managed care. Maternal and Child Health Journal. 2005;9(2):135–49. doi: 10.1007/s10995-005-4871-9. [DOI] [PubMed] [Google Scholar]
- 28.Handler A, Rosenberg D, Raube K, Kelley M. Health care characteristics associated with women’s satisfaction with prenatal care. Medical Care. 1998;36:679–94. doi: 10.1097/00005650-199805000-00008. [DOI] [PubMed] [Google Scholar]
- 29.Handler A, Rosenberg D, Raube K, Lyons S. Prenatal care characteristics and African-American women’s satisfaction with care in a managed care organization. Women’s Health Issues. 2003;13(3):93–103. doi: 10.1016/s1049-3867(03)00031-8. [DOI] [PubMed] [Google Scholar]
- 30.Laslett AL, Brown S, Lumley J. Women’s views of different models of antenatal care in Victoria, Australia. Birth. 1997;24(2):81–9. [PubMed] [Google Scholar]
- 31.Committee on Quality Healthcare in America . Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: Institute of Medicine, National Academies Press; 2001. [Google Scholar]
- 32.Stewart M, Brown JB, Donner A. The impact of patient-centered care on outcomes. J Fam Pract. 2000;49:796–804. [PubMed] [Google Scholar]
- 33.Sans-Corrales M, Pujol-Ribera E, Gené-Badia J, Pasarín-Rua MI, Iglesias-Pérez B, Casajuana- Brunet J. Family medicine attributes related to satisfaction, health and costs. J Fam Pract. 2006;23:308–16. doi: 10.1093/fampra/cmi112. [DOI] [PubMed] [Google Scholar]
- 34.Oakley A, Hickey D, Rajan L, Rigby AS. Social support in pregnancy: does it have long-term effects? J Reprod Infant Psychol Journal of Reproductive and Infant Psychology. 1996;14:7–22. [Google Scholar]
- 35.Hodnett ED. The Cochrane Library. 1. Update Software; Oxford: 2002. Caregiver support for women during childbirth (Cochrane Review) [DOI] [PubMed] [Google Scholar]
- 36.Hodnett ED, Fredericks S. The Cochrane Library. 1. Update Software; Oxford: 2002. Support during pregnancy for women at increased risk of low birth weight babies (Cochrane Review) [Google Scholar]
- 37.Leon FR, Lundgren R, Huapaya A, Sinai I, Jennings V. Challenging the courtesy bias interpretation of favorable clients’ perceptions of family planning delivery. Evaluation Review. 2007;31(1):24–42. doi: 10.1177/0193841X06289044. [DOI] [PubMed] [Google Scholar]
- 38.Bronfman-Pertzovsky MN, Lopez-Moreno S, Magis-Rodriguez C, Moreno-Altamirano A, Rutstein S. Prenatal care at the first level of care: characteristics of providers that affect users’ satisfaction. Salud Publica de Mexico. 2003;45(6):445–54. [PubMed] [Google Scholar]
- 39.Seclen-Palacin JA, Benavides B, Jacoby E, Velasquez A, Watanabe E. Is there a link between continuous quality improvement programs and health service users’ satisfaction with prenatal care? An experience in Peruvian hospitals. Revista Panamericana de Salud Publica. 2004;16(3):49–57. doi: 10.1590/s1020-49892004000900001. [DOI] [PubMed] [Google Scholar]
- 40.Nisar N, Amjad R. Pattern of antenatal care provided at a public sector hospital Hyderabad Sindh. Journal of Ayub Medical College Abbottabad. 2007;19(4):11–3. [PubMed] [Google Scholar]
- 41.Fiscella K. Does prenatal care improve birth outcomes? A critical review. Obstet Gynecol. 1995;85:468–79. doi: 10.1016/0029-7844(94)00408-6. [DOI] [PubMed] [Google Scholar]
- 42.Alexander GR, Korenbrot CC. The role of prenatal care in preventing low birth weight. Future Child. 1995;5:103–20. [PubMed] [Google Scholar]
- 43.Kogan M, Alexander G, Jack B, Allen M. The association between adequacy of prenatal care utilization and subsequent pediatric care utilization in the United States. Pediatrics. 1998;102:25–30. doi: 10.1542/peds.102.1.25. [DOI] [PubMed] [Google Scholar]
- 44.Ansari Niaki M, Izadi Sabet F. The quality of prenatal care performance on the basis of existing care standards in health centers. Journal of Semnan University of Medical Siences. 2003;2(5):86–1. [Google Scholar]
- 45.Mirmolaei ST, Khakbazan Z, Kazemnejad A, Azari M. Prenatal care utilization rate and patientssatisfaction. The Journal of Faculty of Nursing and Midwifery. 2007;2(13):31–40. [Google Scholar]
- 46.Tandon SD, Parillo KM, Keefer M. Hispanic women’s perceptions of patient-centeredness during prenatal care: A mixed-method study. Birth. 2005;32(4):312–17. doi: 10.1111/j.0730-7659.2005.00389.x. [DOI] [PubMed] [Google Scholar]
- 47.Johnson AA, Hatcher BJ, El-Khorazaty MN, Milligan RA, Bhaskar B, Rodan MF, Richards L, Wingrove BK, Laryea HA. Determinants of inadequate prenatal care utilization by African American women. J Health Care Poor Underserved. 2007;18:620–36. doi: 10.1353/hpu.2007.0059. [DOI] [PubMed] [Google Scholar]
- 48.Daniels P, Fuji Noe G, Mayberry R. Barriers to prenatal care among black women of low socioeconomic status. Am J Health Behav. 2006;30(2):188–98. doi: 10.5555/ajhb.2006.30.2.188. [DOI] [PubMed] [Google Scholar]
- 49.Higgins P, Murray M, Williams E. Self-esteem, support, and satisfaction differences in women with adequate and inadequate prenatal care. Birth. 1994;21(1):26–33. doi: 10.1111/j.1523-536x.1994.tb00912.x. [DOI] [PubMed] [Google Scholar]
- 50.Moore P, Hepworth JT. Use of perinatal and infant health services by Mexican-American Medicaid enrollees. JAMA. 1994;272:297–304. [PubMed] [Google Scholar]
- 51.Van Teijlingen ER, Hundley V, Rennie AM, Graham W, Fitzmaurice A. Maternity satisfaction studies and their limitations: what is, must still be best. Birth. 2003;30:75–82. doi: 10.1046/j.1523-536x.2003.00224.x. [DOI] [PubMed] [Google Scholar]