Abstract
Background:
The recent devastating earthquake of December 26 in Bam, 2003 created various risk factors; caused a sharp increase in incidence of anthroponotic cutaneous leishmaniasis (ACL) cases and reached to an epidemic proportion. The objective of this study was to evaluate the status of ACL cases five years before the earthquake compared to the cases occurred five years after the earthquake (1999–2008).
Methods:
Status of disease was assessed retrospectively for the five years before the earthquake and prospectively for the five years after the earthquake. Identification was confirmed by smear and polymerase chain reaction (PCR).
Results:
The mean annual incidence of ACL for the period from 1999 to 2003 was 1.9 per 1000 comparing to post earthquake period, which was 7.6 per 1000. Most of the infection was in individuals of <20 years, more frequently in females before the earthquake, whilst in contrast, there was a progressive rise in the number of cases, significantly in male individuals of >20 years (P< 0.0001) in post earthquake era. The anatomical distribution of lesions considerably changed during the two periods. Most of the cases were limited to three zones within the city prior to the earthquake, whereas it was spread throughout different zones after the earthquake. PCR indicated that the CL was due to Leishmania tropica in the city.
Conclusion:
The results strongly suggest that in natural disasters such as earthquakes various precipitating factors in favor of disease will be created, which in turn provide a suitable condition for propagation of the vector and the transmission of the parasite.
Keywords: Cutaneous leishmaniasis, Leishmania tropica, Epidemiology, Earthquake, Iran
Introduction
The global epidemiology of cutaneous leishmaniasis (CL) has been changed, mainly due to population movement, individual risk factors, and environmental changes (1–3). This disease is among the most emerging parasitic diseases in recent years, posing a public health problem in many parts of the world (4–8). In Iran, two species of CL due to Leishmania major and L. tropica are present with different clinical features and diverse epidemiology (9). Many of the provinces of Iran are endemic by these two species. However, CL in Bam is anthroponotic (ACL), where vaccine trials of single and multiple doses of auto-claved L. major against ACL have currently been carried out (10,11). It is mainly endemic in the city, where the person-to-person transmission is maintained by Phlebotomus sergenti (12–14). Approximately 85% of the CL cases are present in the city of Bam, while only 15% in small towns and in rural communities in the district (unpublished data). At present, ACL appears to be more prevalent than before and becoming a public health threat of considerable magnitude in Bam. ACL produces painless lesions of the skin, often healing to disfiguring scars. Some clinical forms of the ACL such as leishmaniasis recidivans may last many years and rarely responds to treatment, lead to a destructive and disfiguring lesion (15, 16). To the best of our knowledge, there are no published scientific paper regarding the impact of earthquake on the epidemiology of CL and most of the studies focused on the general health aspects and well-being of the survivors (17). Iran is prone to natural disasters such as earthquake. The city of Bam, the center of Bam district, is located along the Zagros Mountain range, 200 Km east of Kerman province in southeastern Iran. The population of the district consists 200000 including 100000 urban and 150000 rural. At 5: 45 a.m. on December 26, 2003, a devastating earthquake of 7.6 on the Richter scale struck the city of Bam and neighboring rural areas, southeast of Iran (Fig. 1).
Fig. 1:
Map of Iran showing location of Bam district, south-eastern Iran where the massive earthquake has occurred
Approximately 30000 people were killed, 35000 wounded, 60000 became homeless and the 2500 yr old historic Citadel of Bam (Arg-e-Bam) was completely destroyed. Consequently, overall 90% of the health facilities including hospitals, health centers, and health houses were destroyed. There were major damages to roads, water pipelines, electricity, and other socio-economic infrastructures. Special attention was paid by the government and National Governmental Organizations (NGOs), disastrous people were housed in tents, and relief materials were distributed (18). More than 20 temporary treatment centers, medical and rehabilitating camps were established. Simultaneously, a disease surveillance system for delivery of primary health care (PHC) was formed.
The present work has been conducted to evaluate the status of the CL cases during the five years before the earthquake as compared to the cases occurred during the corresponding years after the earthquake (1999–2008).
Materials and Methods
National control program
A national control program has been developed by the National Center for Disease Control Office along with an Expert Committee from endemic areas of the country. The protocol was approved and formally adopted by the Ministry of Health and became a part of the national policy and the government commitment. This protocol has been implemented in Bam since 2006. Control strategies were designed, using simple measures, immediately implemented to prevent epidemic situation.
Data collection
Prior to this study, the status of CL was assessed. Since CL represents a significant burden for health services in Bam, it has long been a reportable disease and a part of the PHC system. A base-line survey was conducted in retrospective manner, at the start of the project for the five years prior to the earthquake, from March 1999 to February 2003. Demographic and clinical characteristics of the population and infected individuals including the time of manifestation of the disease, age, sex, location, and number of lesions, type of treatment and distribution of cases in the district were assessed. Prospective data on disease and demographic information were collected in similar manner as stated before, for the five years after the earthquake also from Mar 1999 to Feb 2008.
CL control and treatment center
Long before the earthquake, CL control programs and surveillance activities, at both technical and economical levels were integrated into PHC system. The major consideration was how to control CL within the PHC strategy. During the organization of the Center for Control and Treatment, it was crucial to include locally appropriate CL control measures, taking into account not only technical aspects but also social and behavioral factors as well. In 2005 because of a high increase in recorded cases a health clinic, as a headquarters was established to control and coordinate various activities involved including; diagnosis and identification of cases, active and passive case-detections, vector control methods, training, health education, data entry and analysis, environmental management, elimination of stray dogs, treatment of patients (free of charge) and referral of non-healing cases. Permanent supplies of the vital products such as equipments, drugs, reagents, repellents, insecticides and mosquito nets, were prepared.
Training health personnel
The health personnel involved in the control activities were trained to have clear understanding of the program, to recognize possible cases of CL and to obtain samples for confirmations of diagnosis. The trained qualified personnel were employed on a full time basis.
Health education
Sensitization of public such as press, TV, handouts, poster education, and offering rewards were part of the public health educational programs. Messages were concentrated mainly on to encourage population to comply with the ongoing activities including the correct use of bed nets and sanitation. The role of sand flies in transmitting the disease, distribution and impregnation of bed nets, curtains, doors and windows and installing traps, were explained.
Environmental management
Due to infrastructural destruction, nearly 10 million tons of constructions and rubbles were removed. Special attentions were paid to improving housing, sanitation, and community participation in the control of ACL in affected areas. Cleaning and sanitation operation in dwellings and household environments, land clearance around villages combined with insecticide spraying to eliminate actual and potential sand fly reproduction sites, were in high priority. The elimination of stray dogs by shooting was justified for various reasons connected with health.
Chemical and physical barriers
Personal protection measures including application of stick insect repellents such as diethyl toluamide 33%, to skin or clothing to reduce man-vector contact, were undertaken. Spraying of residual insecticide of pyrethroid (deltamethrin), mainly outside and around the houses at the beginning of the active season for the sand flies was applied one or two times annually during the five years after the earthquake. Use of effective mosquito netting, treated with permethrin and applied on front doors, windows and also impregnation of curtains.
Diagnosis and identification
Skin scraping was taken from the margin of active lesion, smeared on a glass slide, methanol fixed, Giemsa stained and microscopically checked for amastigote stage. To identify the causative agent, another specimen was cultured into a tube containing NNN medium, then transferred into RPMI-1640 for further identification of causative species by polymerase chain reaction (PCR), as described in details elsewhere (19). All 11448 cases were diagnosed by direct smear preparations and about 5% of the cases (570 cases) were cultured. Altogether, 66 random cases were identified during the years after the earthquake. A pair of primers; upstream (5′TCGCAGAACGCCCCTACC3′) and the downstream (5′AGGGGTTGGTGTAAAATAGGC3′) specific for conserved sequences of kDNA of Leishmania was used. The differentiation was based on the size of the products. Two Leishmania species provided amplified fragments of about 800 bp for L. tropica and 620 bp for L. major, L. tropica and L. major of known isolates were used as references.
Treatment of patients
As an ACL, the highest priority was to diagnose and treat the patients promptly, to reduce the human reservoir. The standard treatment based on the national protocol was meglumine antimoniate (Glucantime), administrated by systemic or intra-lesional injection at the recommended dosage of 20 mg/ kg/day for 20 d, mainly along with cryotherapy using liquid nitrogen. Clinical forms including cases of leishmaniasis recidivans (chronic relapsing CL) that is a prevalent phenomenon in Bam were referred for treatment (15).
Statistical analysis
The statistical analysis was performed using SPSS 17 software. The χ2-test was used for comparing categorical data and P< 0.05 was considered as significant.
Results
Altogether, 2102 cases were diagnosed five years before the earthquake (1999–2003) compared to 9346 cases five years after the earthquake (2004–2008). A similar pattern of incidence was observed between the two periods. In the period between 1999 through 2004 (five years before and one year after the earthquake) there was a non-significant excess of cases, whereas the incidence of ACL was sharply increased there after, reaching to an epidemic level during 2006. The mean annual incidence of ACL for the period between 1999–2003 was 1.9 per 1000 comparing to post earthquake period (2004–2008) which was 7.6 per 1000 (Fig. 2). Overall cases of ACL were nearly 4.4 times higher, five years after the earthquake than the cases registered during the same length of time before the earthquake.
Fig. 2:
Incidence of cutaneous leishmaniasis in Bam: A comparative evaluation of pre- and post-earthquake years (1999–2008)
Most of the infections were in individuals of age< 20 yr, closely divided among children< 6 yr (40%) and 6–20 yr (42%), five years before the earthquake, whereas it was 18% in older age group of >20 yr, at the same period of time. Conversely, after the earthquake during 2004–2008 there was gradually a progressive rise, observed in the number of CL cases by age in children <6 yr (12%), in 6–20 yr (43%), while mostly in individuals of >20 yr (45%) (Table 1). There was a significant difference between the age groups five years before and after the earthquake (P< 0.0001). Majority of cases were found in females (53.4%), to lower extent in males (46.6%), five years before the earthquake (Table 2). On the other hand, the proportion of females (43.7%) males (56.3%) ratio reversed five years after the earthquake, though with a significant difference between sexes during the two periods (P< 0.0001).
Table 1:
Cutaneous leishmaniasis in Bam: A comparative evaluation of pre- and post-earthquake cases by age (1999–2008)
| Age (year) | Before earthquake | After earthquake | ||
|---|---|---|---|---|
|
|
||||
| No. | Percent | No. | Percent | |
| <6 | 841 | 40 | 1121 | 12 |
| 6–20 | 882 | 42 | 4019 | 43 |
| >20 | 378 | 18 | 4206 | 45 |
| Total | 2102 | 100.0 | 9346 | 100.0 |
Table 2:
Cutaneous leishmaniasis in Bam: A comparative evaluation of pre- and post-earthquake cases by sex(1999–2008)
| Sex | Before earthquake | After earthquake | ||
|---|---|---|---|---|
|
|
||||
| No. | Percent | No. | Percent | |
| Female | 979 | 53.4 | 4084 | 43.7 |
| Male | 1122 | 46.6 | 5262 | 56.3 |
| Total | 2102 | 100.0 | 9346 | 100.0 |
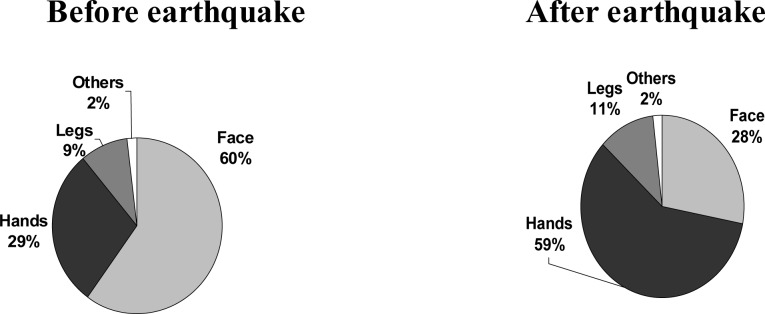
The anatomical distributions of lesions were considerably different during the two periods; majority on face (60%), hands (29%), legs (9%) and others (2%) in the period before the earthquake. In contrast, the distribution site of lesions changed, conversely to hands (59%), face (28%), legs (11%) and others (2%), five years after the earthquake (Fig. 3). The degree of severity of lesions, revealed a pronounced difference between the two periods as the mean number of lesions was 1.3 vs. 1.5, five years before and after the earthquake, respectively (P< 0.0001). Further identification of 66 random cases by PCR indicated that L. tropica was the sole species after the earthquake. Most of the cases (70%) originally belonged to three zones, five years before the earthquake; Kamarbandi Boulvard of Mahdab was the most infected zone, followed by 900 Metri Boulvard and Moalem Boulvard. When the period after the earthquake was considered, cases were distributed throughout the twelve different zones within the city of Bam.
Fig. 3:
Cutaneous leishmaniasis in Bam: A comparative evaluation of pre- and post-earthquake cases by location of lesion (1999–2008)
Discussion
This is the first report of epidemic of CL occurred in recent years in Bam, after the earthquake. These epidemiological data indicate that the number of infected people was nearly 4.4 times higher, five years in post-earthquake years than the number of cases occurred before the earthquake within the same period of time (five years). In terms of severity of the lesions, there was statistically significant difference between the number of lesions during the two periods, after or before the earthquake.
Data showed that all age groups were affected, although older ages of >20 yr seemed to be more at risk of contracting CL infection than any other age groups, five years after the earthquake. This epidemiological event also shows that more cases of CL, clearly in excess of normal expectancy, occurred more likely among non–immune male individuals. In fact, during the period after the earthquake the population of Bam has increased considerably, mainly due to massive movement of labor forces and contractors connected to the large–scale construction works, new project development and for various occupational opportunities created after the earthquake. According to the official authorities, about 30000 new comers, mostly professional workers arrived to the district for the above purposes, immediately after the earthquake that might not have immunity against CL. The clinical features of the CL cases observed in the post-earthquake period were in contrast with those patients infected before the earthquake. Obviously, after the earthquake more males of >20 yr, majority with lesions located on hands or legs were infected. The reason for such a shift is not well clear. It seems that adult males more frequently arrived to the area and were more mobile in offering different services than females, thus traveling more commonly to the affected areas of high risk.
Modification of the physical environment as an event after the earthquake may have a drastic effect on the relative abundance of vectors, on levels of transmission and on actual or potential sand fly breeding sites. Despite all efforts and activities to clean physically and chemically the environment and to reduce or eliminate the breeding areas against sand flies; the presence of vector during the one-year survey in 2007 was indicative of a highly widespread vector population throughout the city. The disease used to be prevalent in three zones within the city prior to the earthquake as compared to the cases found everywhere within the city, throughout different zones after the earthquake. The reason for such occurrence is mainly due to creation of various risk factors in favor of disease transmission in different zones. In ACL focus, in order to reduce the human reservoir; diagnosing and treatment of the patients at the earliest possible time, should be of high priority. Unfortunately, in spite all efforts the treatment has not been a factor in preventing transmission of the disease in Bam, mainly due to incomplete course of treatment mainly in children. Moreover, patients currently do not respond well to meglumine antimoniate (Glucantime) and resistant forms of CL have become a major concern in recent years (20).
The number of the kDNA indicated that the CL was due to L. tropica in the period after the earthquake in the district (unpublished data). Similar findings were reported from Bam, previously (21), however, they found over 95% of ACL cases caused by L. tropica. Similarly, presumptive identification based on extrinsic characteristics including clinical appearance, the mean number of lesions and the site of involvement, were indicative of L. tropica as the causative agent of ACL in Bam. In addition, prior survey of monthly activities of sand fly vectors indicated that Phlebotomus papatasi was the main vector in the area (12).
Undoubtedly a partial increase in incidence rate could be due to more precise and sensitive reporting, better case detection and improved control strategies after the earthquake, however the trend reveals that the increase is more frequently observed than expected.
After a major earthquake, several environmental risk factors have been involved in emergence of the new epidemic condition in Bam. The recent expansion of the city and villages, development of previously uninhabited areas, new settlements and individual risk factors, constitute other factors. Various confounding factors have contributed to the occurrence of new epidemic of CL in several countries (22–25). Outbreaks are characteristics of CL, particularly in long-standing endemic foci such as Bam, more likely in presence of the major risk factors, can erupt into epidemic. It seems that the trend of CL cases has steadily decreased during 2007–2008, but any judgment at this point may not be true in future findings, as nearly 25000 labor forces in 2007 and 2008 have already left the district, mainly due to termination of the whole construction project .
Our findings showed that creation of various risk factors, occupational opportunities and new project development in Bam, where the CL infection is endemic, bringing non-immune newcomer manpower into the area, consequently resulting in increased incidence rate.
In conclusion, the results presented here strongly suggest that in natural disasters such as earthquake, various risk factors in favor of disease will be created, which in turn provide a suitable condition for propagation of the vector and transmission of the parasite.
Ethical Considerations
Ethical issues including plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc. have been completely observed by the authors.
Acknowledgments
The authors would like to thank the personnel in Bam Health System, Kerman Leishmaniasis Research Center, and Kerman University of Medical Sciences for their help in carrying out this study. This project was supported by Kerman University of Medical Science and Ministry of Health. The authors declare that there is no conflict of interests.
References
- 1.Ashford RW. The leishmaniasis as emerging and reemerging zoonoses. Int J Parasitol. 2000;30:1269–81. doi: 10.1016/s0020-7519(00)00136-3. [DOI] [PubMed] [Google Scholar]
- 2.Desjeux P. The increase in risk factors for the leishmaniasis worldwide. Trans Roy Soc Trop Med Hyg. 2001;95:239–43. doi: 10.1016/s0035-9203(01)90223-8. [DOI] [PubMed] [Google Scholar]
- 3.Klaus S, Axelrod O, Jonas F, Frankenburg S. Changing patterns of cutaneous leishmaniasis in Israel and neighboring territories. Trans Roy Soc Trop Med Hyg. 1994;88:649–50. doi: 10.1016/0035-9203(94)90209-7. [DOI] [PubMed] [Google Scholar]
- 4.Desjeux P. Leishmaniasis: current situation and new perspectives. Comp Immunol Microbiol Infect Dis. 2004;27:305–18. doi: 10.1016/j.cimid.2004.03.004. [DOI] [PubMed] [Google Scholar]
- 5.Fazaeli A, Fouladi B, Sharifi I. Emergence of cutaneous leishmaniasis in a border area at south-east of Iran: an epidemiological survey. J Vector Borne Dis. 2009;46:36–42. [PubMed] [Google Scholar]
- 6.Ramaoui K, Guernaoui S, Boumezzough A. Entomological and epidemiological study of a new focus of cutaneous leishmaniasis in Morocco. Parasitol Res. 2008;103:859–63. doi: 10.1007/s00436-008-1068-3. [DOI] [PubMed] [Google Scholar]
- 7.Razmjou S, Hejazy H, Motazedian MH, Baghaei M, Emami M, Kalantary M. A new focus of zoonotic cutaneous leishmaniasis in Shiraz, Iran. Trans Roy Soc Trop Med Hyg. 2009;103:727–30. doi: 10.1016/j.trstmh.2008.12.013. [DOI] [PubMed] [Google Scholar]
- 8.Soccol VT, de Castro EA, Schnell e Schühli G, de Carvalho Y, Marques E, Pereira Ede F, Alcantara Fde S, Machado AM, Kowalthuk W, Membrive N, Luz E. A new focus of cutaneous leishmaniasis in the central area of Paraná State, southern Brazil. Acta Trop. 2009;111(3):308–15. doi: 10.1016/j.actatropica.2009.05.013. [DOI] [PubMed] [Google Scholar]
- 9.Momeni AZ. Clinical picture of cutaneous leishmaniasis. In: Nadim, Javadian, Mohebali, Momeni, editors. Leishmania parasite and leishmaniasis. 3rd ed. Center for University Publication; Tehran: 2008. pp. 50–67. [Google Scholar]
- 10.Sharifi I, Fekri AR, Aflatoonian MR, Khamesipour A, Nadim A, Ahmadi Mousavi MR, Momeni A, Dowlati Y, Godal T, Zicker F, Smith GP. Randomized vaccine trial of single dose of killed Leishmania major plus BCG against anthroponotic cutaneous leishmaniasis in Bam, Iran. Lancet. 1998a;351:1540–44. doi: 10.1016/S0140-6736(98)09552-X. [DOI] [PubMed] [Google Scholar]
- 11.Sharifi I, Fekri AR, Aflatoonian MR, Ahmadi Mousavi MR, Nadim A, Khamesipour A, Nassir KM, Dowlati Y, Moulton L, Zicker F, Smith GP, Modabber F. Abstract Book of the Second World Congress on Leishmaniasis. Hersonissos, Crete; Greece: 2001. Multiple doses of autoclaved Leishmania major vaccine against anthroponotic cutaneous leishmaniasis in Bam, Iran; p. 89. [Google Scholar]
- 12.Aghasi M, Sharifi I. Survey of the funna and monthly activity of the sand fly as the vector of the cutaneous leishmaniasis in Bam. J Kerman Univ Med Sci. 2003;10:85–91. [Google Scholar]
- 13.Nadim A, Aflatoonian MR. Anthroponotic cutaneous leishmaniasis in Bam, southeast Iran. Iranian J Publ Health. 1995;24:15–24. [Google Scholar]
- 14.Sharifi I, Fekri AR, Aflatoonian MR, Nadim A, Nikian Y, Khamesipour A. Cutaneous leishmaniasis in primary school children in the south – eastern Iranian city of Bam, 1994–95. Bull of the WHO. 1998b;76(3):289–93. [PMC free article] [PubMed] [Google Scholar]
- 15.Esfandiarpour I, Dabiri SH. Treatment of cutaneous leishmaniasis recidivans with a combination of allopurinol and meglumine antimoniate: a clinical and histologic study. Int J Dermatol. 2007;46:848–52. doi: 10.1111/j.1365-4632.2007.03086.x. [DOI] [PubMed] [Google Scholar]
- 16.Sharifi I, Fekri AR, Aflatoonian MR, Khamesipour A, Mahboudi F, Dowlati Y, Nadim A, Modabber F. Leishmaniasis recidivans among school children in Bam, South-east Iran, 1994–2006. Int J Dermatol. 2010;49:557–61. doi: 10.1111/j.1365-4632.2010.04419.x. [DOI] [PubMed] [Google Scholar]
- 17.Anonymous. The Government of the Islamic Republic of Iran and WHO Joint Project for: “Reconstruction of Health Services in Bam”. World Health Organization (WHO); 2004. Available at: http://www.emro.who.int/eha/BamPan16.pdf. [Google Scholar]
- 18.Abolghasemi H, Radfar MH, Khatami M, Nia MS, Amid A, Briggs SM. International medical response to a natural disaster: lessons learned from the Bam earth-quake experience. Prehosp Disaster Med. 2006;21:141–47. doi: 10.1017/s1049023x00003599. [DOI] [PubMed] [Google Scholar]
- 19.Mahboudi F, Abolhassan M, Yaran M, Mobtaker H, Azizi M. Identification and differentiation of Iranian Leishmania species by PCR amplification of kDNA. Scand J Infect Dis. 2001;33(8):596–98. doi: 10.1080/00365540110026746. [DOI] [PubMed] [Google Scholar]
- 20.Pour R, Sharifi I, Kazemi B, Zarean M. Identification of nonresponsive isolates to glucantime in patients with cutaneous leishmaniasis in Bam. J Kerman Uni Med Sci. 2011;18(2):123–33. [Google Scholar]
- 21.Sharifi I, Ardehali S, Motazadian H, Aflatoonian MR. Identification and characterization of Leishmania isolates in school children in Bam, southeastern Iran. Iranian J Med Sci. 1997;22:82–88. [Google Scholar]
- 22.El–Safi SH, Peters W. Studies on the leishmaniasis in the Sudan. 1. Epidemic of cutaneous leishmaniasis in Khartoum. Trans Roy Soc Trop Med Hyg. 1991;85:44–7. doi: 10.1016/0035-9203(91)90151-n. [DOI] [PubMed] [Google Scholar]
- 23.Jacobson RL, Eisenberger CL, Svobodova M, Banesh G, Sztern J, Carvalho J, Nasereddin A, El Fari M, Shalom U, Volf P, Votypka J, Dedet JP, Pratlong F, Schonian G, Schnur LF, Jaffe CL, Warburg A. Outbreak of cutaneous leishmaniasis in northern Israel. J Infect Dis. 2003;188:1065–74. doi: 10.1086/378204. [DOI] [PubMed] [Google Scholar]
- 24.Kolaczinski J, Brooker S, Reyburn H, Rowland M. Epidemiology of anthroponotic cutaneous leishmaniasis in Afghan refugee camps in northwest Pakistan. Trans Roy Soc Trop Med Hyg. 2004;98:373–78. doi: 10.1016/j.trstmh.2003.11.003. [DOI] [PubMed] [Google Scholar]
- 25.Reyburn H, Rowland M, Mohsen M, Khan B, Davies C. The prolonged epidemic of anthroponotic cutaneous leishmaniasis in Kabul, Afghanistan: bringing down the neighborhood. Trans Roy Soc Trop Med Hyg. 2003;97:170–76. doi: 10.1016/s0035-9203(03)90111-8. [DOI] [PubMed] [Google Scholar]