Abstract
Parthenium dermatitis is a widespread and distressing dermatoses in rural and urban India caused by the air borne allergen of the Compositae weed Parthenium hysterophorus. Parthenium dermatitis has been thought to be mediated solely by type IV hypersensitivity, but recently a combined immediate (type I) and delayed (type IV) hypersensitivity mechanism has been postulated in the initiation and perpetuation of parthenium dermatitis, especially in sensitized subjects with an atopic diathesis. Initially, the exposed sites of the body are involved. Later in the course of the disease, unexposed sites may get involved. Various clinical presentations have been described in parthenium dermatitis. Typically, it presents as an air borne contact dermatitis (ABCD) involving the eyelids and nasolabial folds Other presentations include a photodermatitis (essentially a pseudo photodermatitis), atopic dermatitis, seborrheic dermatitis, exfoliative dermatitis, hand dermatitis. Photosensitive lichenoid dermatitis and prurigo nodularis are rarer presentations. Uncommon presentations have been described in parthenium dermatitis. They include prurigo nodularis-like lesions and photosensitive lichenoid eruption. Three cases are presented, two of whom presented as polymorphic-like lesions and one as prurigo nodularis. All three patch tested positive to parthenium on Day 2. Prick testing was positive in two of the three patients. Parthenium dermatitis mimicking polymorphic light eruption has not been reported. Histopathology revealed vasculitis in the lesional skin in two of the patients. Although leukocytoclastic vasculitis has been reported earlier from the prick-tested site, this is the first report demonstrating the presence of vasculitis in lesional skin of parthenium dermatitis.
Keywords: Leukocytoclastic vasculitis, parthenium dermatitis, patch test, polymorphic light eruption, prurigo nodularis
INTRODUCTION
Parthenium hysterophorus is an exotic weed accidentally introduced in India in 1956 through imported food grains. The characteristic presentation is an ABCD. Other presentations include a photodermatitis (essentially a pseudo photodermatitis), atopic dermatitis, seborrheic dermatitis, exfoliative dermatitis, and hand dermatitis. Photosensitive lichenoid dermatitis and prurigo nodularis are rarer presentations.[1] Parthenium dermatitis has been thought to be mediated solely by type IV hypersensitivity, but recently a combined immediate (type I) and delayed (type IV) hypersensitivity mechanism have been postulated in the initiation and perpetuation of parthenium dermatitis, especially in sensitized subjects with an atopic diathesis.[2] The patch test detects delayed hypersensitivity (type IV), while the skin prick test (SPT) detects immediate hypersensitivity (type I). A positive SPT comprises 2 responses – an immediate reaction seen within 15-20 minutes characterized by a wheal and flare and a delayed reaction or the late phase reaction (LPR), which occurs at about 5-6 hours and may persist for 1-2 days. It presents as a nodule which is painful rather than itchy. Clinically, the late phase reaction (LPR) of the type I hypersensitivity reaction is thought to be responsible for the chronic skin and bronchial reactivity in atopic patients with dermatitis or bronchial asthma, respectively.[3] The LPR of the Type I hypersensitivity reaction shows histopathology consistent with leukocytoclastic vasculitis.[4] Leukocytoclastic vasculitis has been reported from the LPR of the prick tested site in parthenium dermatitis,[5] but this is the first report of vasculitis-like picture seen in the histopathology of lesional skin.
We present three patients with uncommon presentations of parthenium dermatitis (polymorphic light eruption (PLE)-like in two and prurigo nodularis in one), out of which two showed vasculitis-like picture in lesional skin. These were the patients who showed a positive prick test and an LPR to parthenium leaf.
Patch testing was carried out with Indian Standard Series (ISS) and readings interpreted as recommended by the International Contact Dermatitis Research Group (ICDRG). Patches were applied using Finn Chambers® on Scanpor® tape (Systopic Pharmaceuticals) and removed after 2 days. Prick testing was carried out with parthenium leaf, parthenium antigen extract (containing 500 PNU), glycerinated saline as negative control, and histamine as positive control (Creative Drug Industries, Allergology Division, Navi Mumbai, India). Serum IgE (N- upto 100 IU/ml) was measured by the chemiluminescence immunoassay system (ADVIA Centaur, Bayer Health Care, Mumbai, India).
CASE REPORTS
Case 1
A 25-year-old house wife presented with pruritic, hypopigmented scaly patches involving the sun exposed sites of the face, neck, pinnae of 6 months duration [Figure 1]. She reported aggravation on exposure to sunlight. She gave a history of allergic rhinitis since adolescence. Clinically, the diagnosis of PLE was considered and she was treated with topical medications (sunscreens and corticosteroids). Since she failed to show improvement, she was investigated for parthenium sensitivity and collagen vascular disease. Complete blood picture (CBC), renal and hepatic functions were within normal limits. Antinuclear antibody (ANA) was negative. Serum IgE was 644 IU/ml. Prick testing with parthenium was positive. (Both the immediate reaction at 15 minutes and delayed reaction at 30 minutes). Following patch testing with ISS, she tested positive to parthenium. (++ on Day 2). Biopsy from a scaly lesion over the neck showed hyperkeratosis, papillomatosis, acanthosis, mimimal spongiosis in the epidermis and perivascular neutrophilic infiltrate with occasional eosinophils in the dermis. Karryorhexis and leukocytoclastic vasculitis with extravasated RBC's was seen [Figure 2].
Figure 1.

Hypopigmented scaly patches over the face and neck
Figure 2.
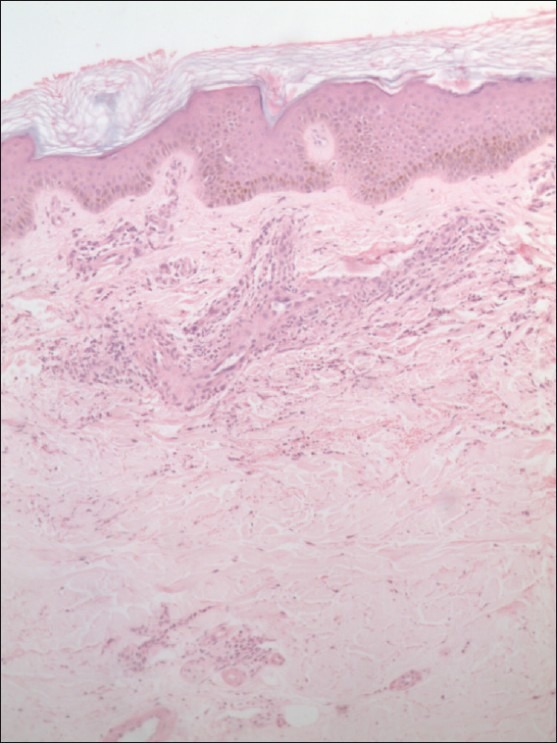
Spongiosis, karyorrhexis and leukocytoclastic vasculitis seen in the lesional skin biopsy (H and E, ×10).
The patient achieved clearance of skin lesions after initiating azathioprine 50 mg daily in addition to antihistamines, topical corticosteroids and sunscreens. On follow-up 2 months later, she was free of skin lesions.
Case 2
A 52-year-old farmer with acrofacial vitiligo of 20 years presented with papules resembling PLE with depigmentation over the eye brows, forearms, pinnae of ears of 9 months duration with aggravation on exposure to sun light [Figure 3]. There was no personal or family history of atopy. Polymorphic light eruption (PLE) with koebnerization of vitiligo in the dermatitic areas was considered. Prick test to parthenium was negative. Serum IgE was 6.31 IU/ml. Patch test to parthenium was positive (++ on Day 2). Skin biopsy from the PLE- like depigmented lesions over the forearm showed epidermal hyperkeratosis, focal parakeratosis, acanthosis and spongiosis. Focal basal vacuolar damage and exocytosis of lymphocytes were seen. The upper dermis showed perivascular lymphohistiocytic infiltrate with occasional eosinophils consistent with PLE. There was no vasculitis [Figure 4]. He was treated with azathioprine 50 mg daily, topical corticosteroids and sunscreens. The pruritic papules resolved with repigmentation 2 months after initiating treatment, but the acrofacial vitiliginous lesions remained as such.
Figure 3.
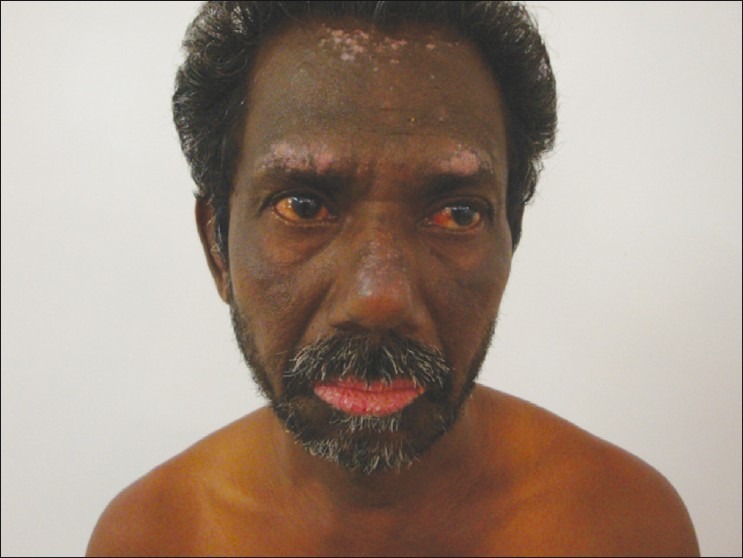
Depigmented PLE- like lesions over the eye brows, forearms, pinnae of ears
Figure 4.
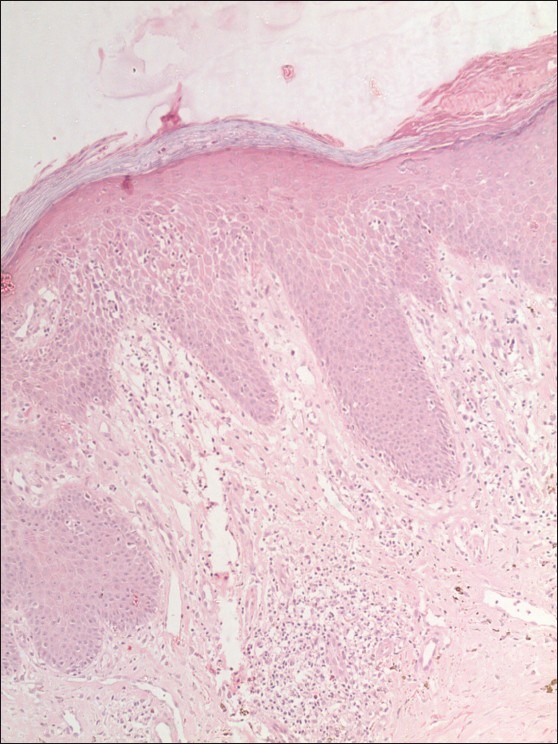
Spongiosis, focal basal vacuolar degeneration, peri-vascular lymphohistiocytic infiltrate with occasional eosinophils consistent with PLE. (H and E, ×10)
Case 3
A 25-year-old textile mill worker presented with intensely pruritic prurigo- like papules over the forearms and legs of 3 years duration and dermatitis over the pinnae of ears of 6 months duration [Figure 5]. He gave a history of photoaggravation. There was a history of atopy in the patient (allergic rhinitis) and his mother (bronchial asthma). Serum IgE was 685.7 IU/ml. Prick testing and patch testing to parthenium was positive (++ on Day 2). Biopsy of a prurigo- like papule from forearm showed perivascular infiltrate of lymphocytes and few eosinophils with few lymphocytes within the vessel wall. Vertically oriented collagen bundles were seen. The histopathological picture was consistent with prurigo nodularis and lymphocytic vasculitis [Figure 6]. His skin lesions responded to topical sunscreens, corticosteroids and azathioprine 50 mg daily for 2 months. Subsequently, he stopped medications and presented with recurrence of lesions after 6 months.
Figure 5.

Pruritic prurigo- like papules over the forearms, legs and pinnae
Figure 6.
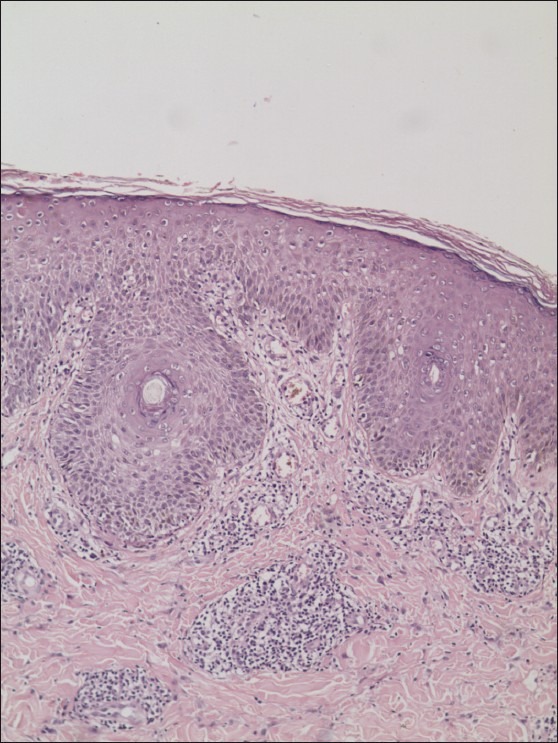
Vertically oriented collagen bundles in the dermis and lymphocytes seen within vessel wall consistent with prurigo nodularis and lymphocytic vasculitis (H and E, ×10)
DISCUSSION
Parthenium dermatitis is a widespread and distressing dermatoses in rural and urban India caused by the air borne allergen of the Compositae weed Parthenium hysterophorus. Parthenium dermatitis has been thought to be mediated solely by type IV hypersensitivity, but recently a combined immediate (type I) and delayed (type IV) hypersensitivity mechanism has been postulated in the initiation and perpetuation of parthenium dermatitis, especially in sensitized subjects with an atopic diathesis.[2]
Unusual presentation of skin lesions with photoaggravation should incite a search for parthenium sensitivity. PLE/ PLE-like skin lesions have not been reported in parthenium dermatitis. In addition, leukocytoclastic vasculitis was observed in the lesional skin of the PLE- like lesion. This patient had a history of atopy (allergic rhinitis), raised serum IgE and a positive prick test and LPR to parthenium leaf. The LPR of the type I hypersensitivity reaction shows histopathology consistent with leukocytoclastic vasculitis.[6] The role of combined type I hypersensitivity and type IV hypersensitivity in perpetuating parthenium dermatitis has been reported.[2,4] It is possible that in an atopic person sensitized to parthenium the resultant LPR (type I) and delayed hypersensitivity (type IV) that occurs following contact of parthenium allergen results in the perpetuation of dermatitis in the skin, akin to the perpetuation of bronchial reactivity in atopic patients with bronchial asthma.
Case 2 diagnosed as PLE with depigmentation had no history of atopy and serum IgE was normal. Parthenium dermatitis could possibly have precipitated the PLE lesions which depigmented by the Koebner reaction as the patient already had vitiligo. Lesional biopsy failed to show vasculitis. In Case 2, the negative prick test, absent history of atopy and normal serum IgE in this patient could account for the absence of vasculitis in lesional skin. In this case. the dermatitis is possibly mediated solely by type IV hypersensitivity
Case 3 demonstrated lymphocytic vasculitis in addition to changes of prurigo nodularis. It is well known that the infiltrating cells in the early stage of leukocytoclastic vasculitis are neutrophils and in late lesions lymphocytes may be predominant.[7] Thus, in this patient it is possible that the biopsied lesion was in the late stage.
The various clinical presentations of parthenium dermatitis have been puzzling. Delayed hypersensitivity alone does not explain the varying clinical patterns and photo aggravation. Atopic dermatitis is known to be a photoaggravated dermatoses. The combined type IV and type I hypersensitivity to parthenium could solve this puzzle. Prurigo nodularis and PLE/PLE-like lesions are increased in patients with an atopic diathesis.[8] However, both dermatoses are not associated with lesional vasculitis. Histologic study of prurigo nodularis in 136 patients showed vasculitis only in one.[9] It is relatively uncommon to find vasculitis in prurigo. The presence of type I hypersensitivity to parthenium as evidenced from a positive personal/family history of atopy, positive prick test to parthenium and raised serum IgE could explain the varied clinical manifestations and presence of vasculitis in lesional skin of parthenium dermatitis.
CONCLUSION
The additional role of the type I hypersensitivity (LPR) could possibly explain the presence of vasculitis in lesional skin of atopic patients (two out of the three cases), and the absence of vasculitis in one case who showed a negative prick test and did not have a family history of asthma or allergic rhinitis.
These case reports stress on the importance of investigating for parthenium dermatitis when patients present with unusual manifestations and photoaggravation. This is the first report to observe and document vasculitis in the lesional skin of atopic patients with parthenium dermatitis.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Lakshmi C, Srinivas CR. Parthenium: wide angle view. Indian J Dermatol Venereol Leprol. 2007;73:296–306. doi: 10.4103/0378-6323.35732. [DOI] [PubMed] [Google Scholar]
- 2.Lakshmi C, Srinivas CR. Type I Hypersensitivity to Parthenium hysterophorus in patients with parthenium dermatitis. Indian J Dermatol Venereol Leprol. 2007;73:103–5. doi: 10.4103/0378-6323.31895. [DOI] [PubMed] [Google Scholar]
- 3.Coico R, Sunshine G, Benjamini E, editors. Immunology a Short Course. 5th ed. New Jersey: Wiley Liss; 2003. Hypersensitivity reactions type I; pp. 199–211. [Google Scholar]
- 4.Samolitis N, Leiferman KM, Gleich GJ. The IgE-mediated cutaneous late-phase reaction. In: Greaves MW, Kaplan AP, editors. Urticaria and Angioedema. New York: Marcel Dekker; 2006. pp. 119–40. [Google Scholar]
- 5.Lakshmi C, Srinivas CR, Jayaraman A. Ciclosporin in parthenium dermatitis- A report of 2 cases. Contact Dermatitis. 2008;59:245–8. doi: 10.1111/j.1600-0536.2007.01208.x. [DOI] [PubMed] [Google Scholar]
- 6.Lakshmi C, Srinivas CR. Parthenium dermatitis caused by immediate and delayed hypersensitivity. Contact Dermatitis. 2007;57:64–5. doi: 10.1111/j.1600-0536.2007.01145.x. [DOI] [PubMed] [Google Scholar]
- 7.Barnhill RL, Nousari CH, Xu X, Barksdale SK. Elder DE, Elenitsas R, Johnson BL, Jr, Murphy GF, Xu X. Lever's histopathology of the skin. New Delhi: Lippincott Williams and Wilkins; 2009. Vascular diseases-small vessel neutrophilic/leukocytoclastic vasculitis; pp. 215–7. [Google Scholar]
- 8.Jorizzo JL, Gath S, Smith EB. Prurigo: Clinical review. J Am Acad Dermatol. 1981;4:723–9. doi: 10.1016/s0190-9622(81)80205-8. [DOI] [PubMed] [Google Scholar]
- 9.Weigelt N, Metze D, Ständer S. Prurigo nodularis: Systematic analysis of 58 histological criteria in 136 patients. J Cutan Pathol. 2010;37:578–86. doi: 10.1111/j.1600-0560.2009.01484.x. [DOI] [PubMed] [Google Scholar]


