Abstract
Background:
Chemical peels are the mainstay of a cosmetic practitioner's armamentarium because they can be used to treat some skin disorders and can provide aesthetic benefit.
Objectives:
To compare 15% TCA peel and 35% glycolic acid peel for the treatment of melasma.
Material and Methods:
We selected 30 participants of melasma aged between 20 and 50 years from the dermatology outpatient department and treated equal numbers with 15% TCA and 35% glycolic acid.
Results:
Subjective response as graded by the patient showed good or very good response in 70% participants in the glycolic acid group and 64% in the TCA group.
Conclusions:
There was statistically insignificant difference in the efficacy between the two groups for the treatment of melasma.
Keywords: Acne scarring, glycolic acid, melasma, peels, photoaging, TCA
INTRODUCTION
Chemical peels are used to create injury at a specific skin depth with the goal of stimulating new skin growth and improving surface texture and appearance.[1] The exfoliative effect of chemical peels stimulates new epidermal growth and collagen with more evenly distributed melanin. Chemical peels are classified by the depth of action into superficial, medium, and deep peels. Specific peeling agents should be selected based on the disorder to be treated and used with an appropriate peel depth, determined by the histological level or severity of skin pathology to maximize success.[2] However, other considerations, such as skin characteristics, area of skin to be treated, safety issues, healing time, and patient adherence, should also be taken into account for best overall results.
In addition, chemical peels may be readily combined with other resurfacing and rejuvenation procedures, often providing synergistic treatment and more flexibility in tailoring treatments specific to patient needs and conditions.[3] Melasma is an acquired hyperpigmentation of the face affecting predominantly women. Multiple etiologic factors have been implicated: high estrogen states (pregnancy, oral contraceptives), genetic factors, cosmetics, and autoimmune thyroid disease. Sunlight exposure appears to be essential for its development. Conventional therapy for melasma consists of keratolytic (tretinoin, resorcin, glycolic, and trichloroacetic acids, etc.) and depigmenting agents (hydroquinone kojic and azelaic acids). It has been established that chemical peels potentiate the effect of the depigmenting agents.
MATERIAL AND METHODS
All patients reporting to the dermatology outpatient department with melasma were subjected to Wood's light to determine the type of melasma (epidermal, dermal or mixed). Only participants with epidermal type were included in this study. Thirty participants with epidermal type of melasma aged between 20 and 50 years were selected. Written informed consent of the participants was taken. The hospital ethics committee approved the study. Participants with dermal or mixed type of melasma, pregnant females, females on oral contraceptive pills, participants with a history of hypertrophic scars or keloids, recurrent herpes infection, active dermatitis or unrealistic expectations were excluded from the study. Selected participants were divided into two groups of 15 each. They were primed two weeks before with kojic acid 2% or tretinoin 0.25%. Each group was treated with either 15% TCA or 35 % glycolic acid (GA).
Melasma Area and Severity Index (MASI) scores were calculated in all the participants at the beginning of each peel session and after each peel. MASI score was calculated by the following formula [Kimbrough-Green CK, Griffiths CE, Finkel LJ, Hamilton TA, Bulengo-Ransby SM, Ellis CN, et al. Topical retinoic acid (tretinoin) for melasma in black patients. A vehicle-controlled clinical trial. Arch Dermatol 1994;130:727-33.] The severity of the melasma in each of the four regions (forehead, right malar region, left malar region and chin) is assessed based on three variables: percentage of the total area involved (A), darkness (D), and homogeneity (H).
A numerical value assigned for the corresponding percentage area involved is as follows: 0=no involvement; 1=<10% involvement; 2=10-29% involvement; 3=30-49% involvement; 4=50-69% involvement; 5=70-89% involvement; and 6=90-100% involvement. The darkness of the melasma (D) is compared to the normal skin and graded on a scale of 0 to 4 as follows: 0=normal skin color without evidence of hyperpigmentation; 1=barely visible hyperpigmentation; 2=mild hyperpigmentation; 3=moderate hyperpigmentation; 4=severe hyperpigmentation. Homogeneity of the hyperpigmentation (H) is also graded on a scale of 0 to 4 as follows: 0=normal skin color without evidence of hyperpigmentation; 1=specks of involvement; 2=small patchy areas of involvement <1.5 cm diameter; 3=patches of involvement >2 cm diameter; 4=uniform skin involvement without any clear areas).
To calculate the MASI score, the sum of the severity grade for darkness (D) and homogeneity (H) is multiplied by the numerical value of the areas (A) involved and by the percentages of the four facial areas (10-30%).
Total MASI score: Forehead 0.3 (D+H)A + right malar 0.3 (D+H)A + left malar 0.3 (D+H)A+chin 0.1 (D+H)A.
Participants were strictly instructed to apply sun block cream during and after therapy along with emollients in unlimited quantities. Peels were performed every 3 weeks for a maximum of six sessions or clearance of melasma whichever was earlier.
The data collected was analysed using Chi-square test.
RESULTS
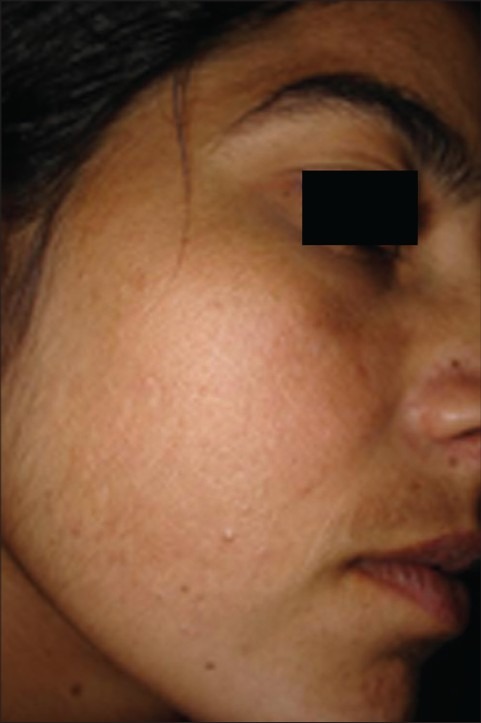
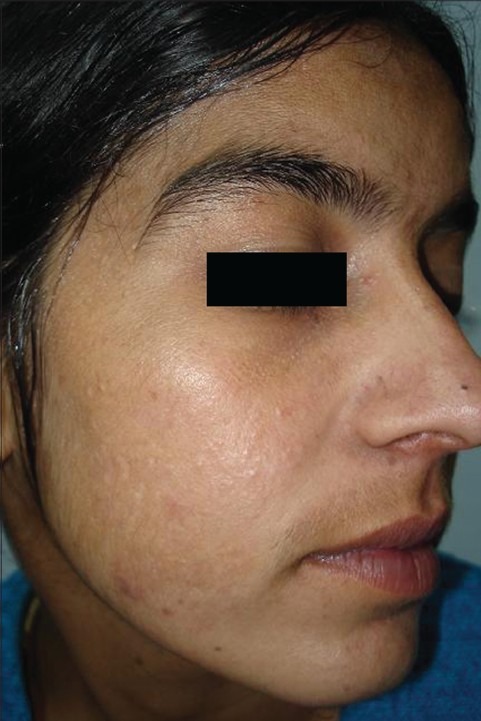
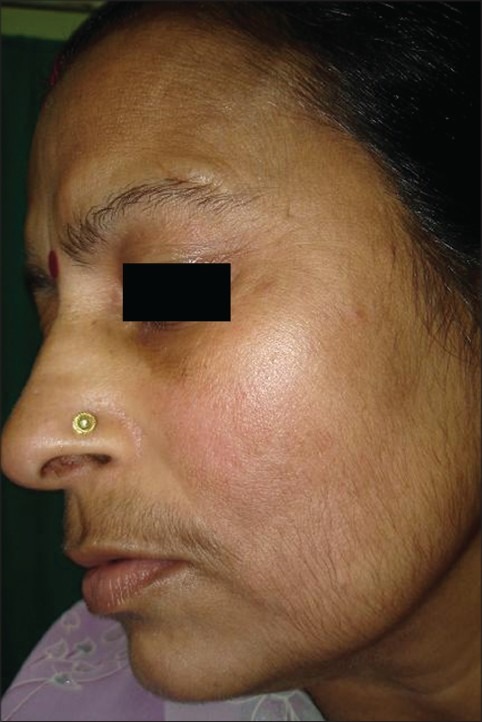
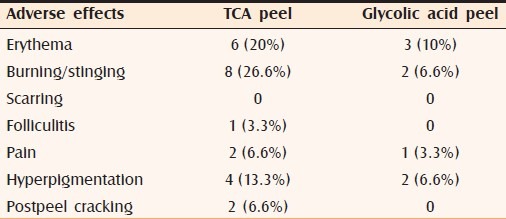
The pattern of melanosis was malar in 40%, mixed in 40% and centrofacial in 20% of participants [Table 1]. Eighteen (60%) participants were between 31 and 40 years, eight (26.6%) were between 41 and 50 years, and four (13.35%) were between 20 and 30 years of age. Females outnumbered males and the female: male ratio was 6.5:1. The pattern of melanosis was of malar type in 40% participants, mixed in 40% participants and centrofacial in 20% participants. Subjective evaluation showed a good or very good response in 70% participants of the GA group [Figure 1a and b] and 64% in the TCA group [Figure 2a and b], which was statistically insignificant. Pregnancy (40%), oral contraceptives (30%) and outdoor occupation (30% of participants) were assessed as some of the likely aetiological factors [Table 2]. The average decrease in MASI score form baseline in both the groups was found to be statistically significant (p=0.269). Comparison of decrease in MASI scores between both the two groups was not statistically significant (P<=0.228) [Table 3]. Common adverse effects [Table 4] were burning sensation (TCA - 26.6%, GA - 6.6% of participants), post-peel erythema (TCA - 20%, GA - 10%), pain (TCA - 6.6%, GA - 3.3%), hyperpigmentation (TCA - 13.35%, GA - 6.6%) and post-peel cracking of skin (TCA - 6.6%, GA - none). After treatment participants were asked to evaluate the discomfort from the two different peeling solutions. They found the TCA peel caused more discomfort slight pain and strong stinging during the application, excessive desquamation during the next 4--5 days, which interfered with their daily activities. The glycolic acid procedure was associated with immediate stinging and burning, which were most pronounced at first visit.
Table 1.
Pattern of melanosis
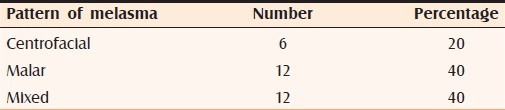
Figure 1a.
Melasma in a 22 year-old-girl before treatment
Figure 1b.
After five sessions of 35% glycolic acid in the same patient
Figure 2a.
Melasma in a 40-year-old lady before treatment
Figure 2b.

After treatment with 15% TCA in the same patient
Table 2.
Etiology of melasma
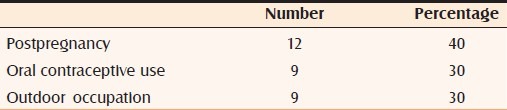
Table 3.
MASI score before and after treatment
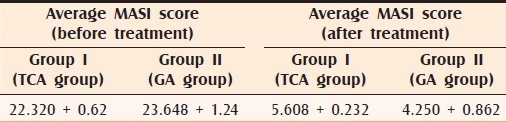
Table 4.
Adverse effects of peels
DISCUSSION
Melasma is a symmetric progressive hyperpigmentation of the facial skin that occurs in all races but has a predilection for darker skin phenotypes. Depigmenting agents, laser, and chemical peeling have been used alone and in combination for the treatment of melasma.[4] Melasma has been associated with hormonal imbalance, sun damage, and genetic predisposition.[5] Clinically, melasma can be divided into centrofacial, malar, and mandibular, according to the pigment distribution on the skin. By Wood's light examination, melasma can be classified into epidermal, dermal or mixed type.
Clinicians and participants often use chemical peels as an adjunct to medical therapy because they produce complementary rapid therapeutic effects and improvements in skin appearance and texture.[6] Peels may allow topical agents to penetrate more efficiently into the skin and may improve postinflammatory hyperpigmentation.[7] With good technique, peels are beneficial in dark-skinned participants.[8] Chemical peeling has a low rate of complications and is popular due to the low costs involved and to a technique which is easy to learn.[9] Chemical peels useful in treating melasma are trichloroacetic acid, Jessner's solution, alpha-hydroxy acid preparations, and salicylic acid, alone or in various combinations. These have been found to be particularly useful for melasma of varying severity.[10]
The gold standard for chemical peeling agents is TCA. It has been well studied and is versatile in its ability to create superficial, medium-depth and deep peels. It is stable, inexpensive, and causes no systemic toxicity. It is easy to perform, as the peel depth correlates with the intensity of skin frost and there is no need to neutralize a TCA peel.[11,12] In the treatment of melasma, a few studies were done using TCA as a chemical peeling agent. Some studies used TCA alone (up to 30%) in the classic full face peeling technique, or focally using higher concentrations of TCA up to 50%.[13] Other studies used TCA in combination with topical vitamin C.[14] Some other studies used TCA in combination with other treatment modalities, such as Q-switched Alexandrite laser or pulsed dye laser (PDL).[15] Melasma is more prevalent in darker complexioned individuals in whom there is a higher tendency for pigmentary change to develop. In such individuals living in tropical countries, hyperpigmentation is also common with superficial peels, especially TCA, possibly on account of intense ultraviolet exposure.[16] When dermatologists initially began using TCA, the usual strength was 20-25%. Trichloroacetic acid (TCA) was not as predictable as phenol. With phenol peels, there is uniform penetration to a certain level; then the action stops. This is not the case with TCA: there are “hot spots” where the TCA penetrates deeper for no apparent reason. These hot spots are less troublesome as the concentration is decreased. The results with TCA are coat-dependent (i.e., dependent on the number of layers applied), whereas the results with alpha-hydroxy acids are time-dependent. The more the coats, the deeper the peel; therefore, multiple coats of a 15% TCA can mimic the results of one or two coats of 35% TCA.[17,18] These diluted peels take more time and more coats, so we have more time to watch the blanch develop and we can discontinue applications at the desired level.[19] The weaker strengths of trichloroacetic acid gives us more time to observe these color changes in the skin as they occur.[20] In our study, based on the above data, we tried to avoid hyperpigmentation, a commonly observed adverse effect with 35% TCA, by using a lower (15%) concentration of TCA.
After treatment participants were asked to evaluate the discomfort from the two different peeling solutions. They found the TCA peel caused more discomfort, slight pain and strong stinging during the application and excessive desquamation during the next 4-5 days, that interfered with their daily activities. The glycolic acid procedure was associated with immediate stinging and burning that was most pronounced at first visit.
CONCLUSION
Chemical peels remain popular for the treatment of some skin disorders and for aesthetic improvement. Participants who are willing to undergo continued treatment are likely to be the best candidates. Using peels less frequently but on a continuous basis is beneficial to help keep improvement ongoing, especially for superficial peels. Medium peels and deep peels are used more judiciously over time, but can address particularly difficult conditions effectively. Clinicians should evaluate the Fitzpatrick skin type and ethnic background as part of the process of selecting whether a peel is an appropriate therapy and which peel is best suited for the individual patient. Finally, it is important for participants to maintain a good sun protection regimen to optimize the clinical results achieved with chemical peels.
To conclude, chemical peeling with 15% TCA and 35% glycolic acid significantly reduces MASI scores and both are equally effective in the treatment of melasma. It was also seen that adverse effects were more with TCA peels compared to glycolic acid peels. More studies need to be conducted with different concentrations of TCA (15% and higher) and glycolic acid (35--70%) using larger samples of people and in other pigmentary disorders.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Ghersetich P, Teofol LM, Gantcheva M. Chemical peeling: How, when, why? J Eur Acad Dermatol Venererol. 1997;8:1–11. [Google Scholar]
- 2.Wiest L. Chemical peels in aesthetic dermatology. Hautarzt. 2004;55:611–3. doi: 10.1007/s00105-004-0734-3. [DOI] [PubMed] [Google Scholar]
- 3.Wiest L. Current peeling methods. Hautarzt. 2003;29:21–6. [Google Scholar]
- 4.Ortonne JP, Passeron T. Melanin pigmentary disorders: Treatment update. Dermatol Clin. 2005;23:209–26. doi: 10.1016/j.det.2005.01.001. [DOI] [PubMed] [Google Scholar]
- 5.Grimes PE. Melasma, etiologic and therapeutic considerations. Arch Dermatol. 1995;131:1453–7. doi: 10.1001/archderm.131.12.1453. [DOI] [PubMed] [Google Scholar]
- 6.Atzori L, Brundu MA, Orru A, Biggio P. Glycolic acid peeling in the treatment of acne. J Eur Acad Dermatol Venereol. 1999;12:119–22. [PubMed] [Google Scholar]
- 7.Landau M. Chemical peels. Clin Dermatol. 2008;26:200–8. doi: 10.1016/j.clindermatol.2007.09.012. [DOI] [PubMed] [Google Scholar]
- 8.Monheit GD. Chemical peels, advances in dermatologic surgery. Skin Ther Lett. 2004;9:6–11. [PubMed] [Google Scholar]
- 9.Monheit GD, Chastain MA. Chemical peels. Facial Plast Surg Clin North Am. 2001;9:239–55. [PubMed] [Google Scholar]
- 10.Monheit GD. The Jessner's-trichloroacetic acid peel. An enhanced medium-depth chemical peel. Dermatol Clin. 1995;13:277–83. [PubMed] [Google Scholar]
- 11.Lawrence N, Leonhardt JM. Trichloroacetic acid (TCA) peels. In: Rubin MG, Dover JS, Alam M, editors. Chemical peels. 9th ed. Elsevier Inc; 2006. pp. 77–8. [Google Scholar]
- 12.Ekmekny P, Bostanci S, Gurgey E. The efficacy of chemical peeling performed with Jessner's solution and 35% TCA in the treatment of melasma. Klin J Dermatol. 2001;11:211–6. [Google Scholar]
- 13.Kalla G, Garg A, Kachhawa D. Chemical peeling glycolic acid versus trichloroacetic acid in melasma. Indian J Dermatol Venereol Leprol. 2001;67:82–4. [PubMed] [Google Scholar]
- 14.Soliman MM, Ramadan SA, Bassiouny DA, Abdelmalek M. Combined trichloroacetic acid peel and topical ascorbic acid versus trichloroacetic acid peel alone in the treatment of melasma: A comparative study. J Cosmet Dermatol. 2007;6:89–94. doi: 10.1111/j.1473-2165.2007.00302.x. [DOI] [PubMed] [Google Scholar]
- 15.Lee GY, Kirn HJ, Whang KK. The effect of combination treatment of the recalcitrant pigmentary disorders with pigmented laser and chemical peeling. Dermatol Surg. 2002;28:1120–3. doi: 10.1046/j.1524-4725.2002.02112.x. [DOI] [PubMed] [Google Scholar]
- 16.Roberts WE. Chemical peeling in ethnic/dark skin. Dermatol Ther. 2004;17:196–205. doi: 10.1111/j.1396-0296.2004.04020.x. [DOI] [PubMed] [Google Scholar]
- 17.Al Waiz MM, Al Sharqi AI. Medium-depth chemical peels in the treatment of acne scars in dark skinned individuals. Dermatol Surg. 2002;28:383–7. doi: 10.1046/j.1524-4725.2002.01081.x. [DOI] [PubMed] [Google Scholar]
- 18.Monheit GD. Medium-depth chemical peels. Dermatol Clin. 2001;19:413–25. doi: 10.1016/s0733-8635(05)70282-5. [DOI] [PubMed] [Google Scholar]
- 19.Coleman WP, 3rd, Futrell JM. The glycolic acid trichloroacetic acid peel. J Dermatol Surg Oncol. 1994;20:76–80. doi: 10.1111/j.1524-4725.1994.tb03753.x. [DOI] [PubMed] [Google Scholar]
- 20.Cook KK, Cook WR., Jr Chemical peel of nonfacial skin using glycolic acid gel augmented with TCA and neutralized based on visual staging. Dermatol Surg. 2000;26:994–9. doi: 10.1046/j.1524-4725.2000.026011994.x. [DOI] [PubMed] [Google Scholar]


