This prospective study uses a condition-specific instrument to assess swallowing-related quality of life for patients with parathyroid disease before and after parathyroid surgery.
Keywords: Parathyroidectomy, SWAL-QOL, Quality of life, Hyperparathyroidism
Abstract
Objective.
To prospectively evaluate the impact of parathyroidectomy on swallowing-related quality of life using the Swallowing Quality Of Life (SWAL-QOL) validated outcomes assessment tool.
Background.
Many patients with primary hyperparathyroidism report nonspecific symptoms, such as fatigue, irritability, cognitive impairment, sleep disturbances, and dysphagia. To date, there have been no prospective studies evaluating swallowing function before and after parathyroid surgery.
Methods.
Patients undergoing parathyroidectomy from September 2007 to January 2009 completed the SWAL-QOL questionnaire before and one year after surgery. Data were collected on demographic and clinicopathologic variables. Comparisons were made to determine the effect of surgery on patients' perceptions of swallowing function.
Results.
Of 151 eligible patients, 102 (68%) completed the study. The mean patient age was 60 years, and 79% were female. A total of 73 patients (67%) had minimally invasive parathyroidectomies, whereas the remainder had bilateral explorations. In all, 83 patients (81%) had a parathyroid adenoma, 16 patients (16%) had hyperplasia, and 3 patients (3%) had a double adenoma on final pathologic interpretation. Mean preoperative SWAL-QOL scores were <90 for 4 of the 11 domains, indicating the perception of oropharyngeal dysphagia and diminished quality of life. Following parathyroidectomy, significant improvements were demonstrated in eight SWAL-QOL domains.
Conclusions.
Many patients with parathyroid disease have the perception of abnormal swallowing function. In these patients with symptoms of dysphagia, parathyroid surgery leads to significant improvements in many aspects of swallowing-related quality of life measured by the SWAL-QOL instrument. This study represents the first use of a condition-specific instrument to assess swallowing-related quality of life for patients with parathyroid disease before and after parathyroid surgery.
Introduction
Oropharyngeal dysphagia is defined as difficulty in swallowing secondary to structural or functional abnormalities involving the oropharynx, hypopharynx, larynx, and upper esophageal sphincter. Although the exact prevalence of dysphagia is unknown, epidemiologic studies suggest the prevalence may be as high as 22% for patients older than 50 years [1]. Impaired swallowing can cause significant morbidity and mortality [2]. Because eating is an important social activity, swallowing difficulties have been shown to negatively impact self-esteem, social role functioning, and quality of life (QOL) functioning [3–6].
Parathyroid disease usually manifests with symptoms related to hypercalcemia, such as weakness and fatigue, depression, bone pain, myalgia, osteopenia, and nephrolithiasis [7–10]. Although less common, oropharyngeal dysphagia may develop in patients with parathyroid disease as a result of direct compression of the swallowing organs by an enlarged or ectopic adenoma or carcinoma [11], spontaneous hemorrhage of a parathyroid adenoma [12–14], neuromuscular depression secondary to chronic hypercalcemia [15], or as an unintended consequence of operative neck exploration [6]. Assessment of dysphagia by means of cinefluouroscopy, modified barium swallow, manometry, and upper endoscopy are valuable in determining the extent of mechanical disability but do not measure the toll of parathyroid disease or its treatment on swallowing ability. This prospective study represents the first use of a condition-specific instrument—the Swallowing Quality Of Life (SWAL-QOL) outcomes assessment tool—to assess swallowing-related QOL in patients with parathyroid disease before and after parathyroid surgery.
Patients and Methods
SWAL-QOL Outcomes Assessment Tool
The SWAL-QOL is a 44-item dysphagia specific outcomes tool that addresses impact on dysphagia-related outcomes in 11 QOL domains important to patients: food selection, burden, physical health, mental health, social functioning, fear, eating duration, eating desire, communication, sleep, and fatigue. The conceptual framework is discussed in detail by McHorney et al. [16]. The SWAL-QOL has several clinimetric advantages, including good content validity and high internal-consistency reliability and reproducibility, suggesting that the scale is appropriate for group-level research [17, 18]. The questionnaire is self-administered and takes fewer than 15 minutes to complete. SWAL-QOL scores ranged from 0 to 100, with a score of 100 representing no impairment (the most favorable state) [18].
Study Design and Study Sample
This prospective longitudinal study enrolled a cohort of 151 consecutive patients evaluated for initial parathyroid surgery at a single center (University of Wisconsin Hospital and Clinics, Madison, WI) between September 2007 and January 2009. Patients were provided with a description of the study, and informed consent was obtained from all participants. The only inclusion criterion was the presence of hyperparathyroidism, defined as an abnormal increase in the activity of one or more parathyroid glands. We excluded patients undergoing repeat parathyroid surgery. For this study, we also excluded patients who underwent concurrent thyroid surgery and those who were unable to complete the self-administered SWAL-QOL questionnaire secondary to cognitive impairment or lack of English language fluency. The study was approved by the University of Wisconsin institutional review board.
Study participants completed the SWAL-QOL questionnaire before and 1 year after initial parathyroid surgery. In cases of nonresponse, reminders were given by phone and mail. For each domain of the SWAL-QOL questionnaire, a separate score out of 100 was calculated, with each item having the same importance. Patients who failed to return both questionnaires were excluded from the analysis.
Data Collection and Variables
Data were prospectively collected on demographic and clinicopathologic variables, including age, gender, surgical procedure (minimally invasive parathyroidectomy or bilateral exploration), mass of resected parathyroid specimen, final histopathologic diagnosis, perioperative complications, and postoperative cure of hyperparathyroidism. For purposes of this study, surgical cure was defined as normalization of the serum calcium (serum calcium level <10.2 mg/dL) at the 6-month postoperative visit. Evaluated perioperative complications included symptomatic hypocalcemia (serum calcium level <8.4 mg/dL) or recurrent laryngeal nerve injury; however, no transient or permanent complications were noted in the study cohort.
Statistical Analysis
Descriptive statistics were used to summarize demographic and clinicopathologic characteristics of the 102 patients who underwent parathyroid surgery and completed both SWAL-QOL questionnaires. Continuous data were summarized with means and standard deviations, and categorical variables were summarized by frequency and percentage. The statistical significance of the difference between pre- and postoperative domain scores was tested with the Wilcoxon signed-rank test. Associations between demographic and clinicopathologic independent variables and changes in SWAL-QOL domain scores were assessed by analysis of variance based on the ranks of the data. A p value less than .05 was considered statistically significant for all analyses. All analyses were performed with available data with SAS version 9.1 (SAS Institute, Cary, NC).
Results
Patient Characteristics
Of 151 eligible patients, 102 (68%) completed both SWAL-QOL questionnaires. Variables related to demographics, disease, and treatment for the study cohort are summarized in Table 1. Mean (SD) age was 60 (11) years, with a range of 22 to 84 years. Most patients (84%) had a single or double hyperfunctioning adenoma(s). The mean (SD) mass of the resected parathyroid specimens was 594 (721) mg. No patients experienced transient or permanent perioperative complications. Six-month postoperative biochemical data were available for 96 of 102 (94%) patients. Of these patients, 95% demonstrated surgical cure at least 6 months after surgery.
Table 1.
Patient characteristics
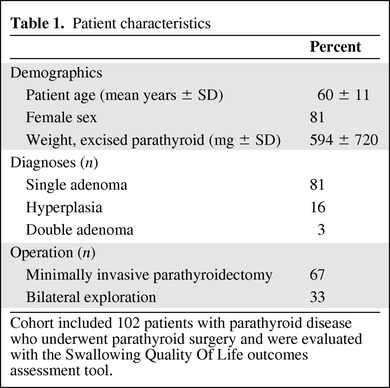
Cohort included 102 patients with parathyroid disease who underwent parathyroid surgery and were evaluated with the Swallowing Quality Of Life outcomes assessment tool.
Baseline Swallowing-Related Quality-of-Life in Patients with Parathyroid Disease
Before parathyroid surgery, mean preoperative SWAL-QOL scores were <90 for 4 of the 11 SWAL-QOL domains (Table 2), indicating the perception of oropharyngeal dysphagia and diminished swallowing-related quality of life. The lowest mean scores were observed for the domains of fatigue (59.6), sleep (60.9), physical health (85.1), and eating duration (89.8). The mean preoperative scores were lower than those reported by McHorney et al. for a sample of 40 “normal” swallowers in all SWAL-QOL domains except eating desire, food selection, and communication [18]; conversely, mean preoperative scores were higher than those reported by Greenblatt et al. for a sample of 116 patients with thyroid disease in all SWAL-QOL domains except sleep and fatigue (Table 2) [6].
Table 2.
Mean Swallowing Quality Of Life outcomes assessment tool scores
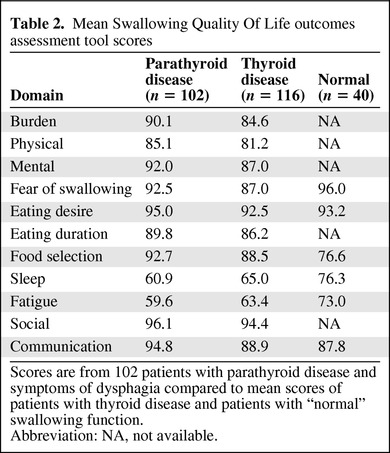
Scores are from 102 patients with parathyroid disease and symptoms of dysphagia compared to mean scores of patients with thyroid disease and patients with “normal” swallowing function.
Abbreviation: NA, not available.
Changes in Swallowing-Related Quality-of-Life after Parathyroid Surgery
After parathyroid surgery, score improvements were seen in all of the SWAL-QOL domains. Statistically significant improvement was found in the 8 of the 11 domains: burden (p < .0001), physical (p < .0001), fatigue (p < .0001), sleep (p < .0001), food selection (p = .0027), eating duration (p = .0002), mental (p = .0003), and social (p = .0058; Table 3).
Table 3.
Mean preoperative and postoperative Swallowing Quality Of Life outcomes assessment tool scores
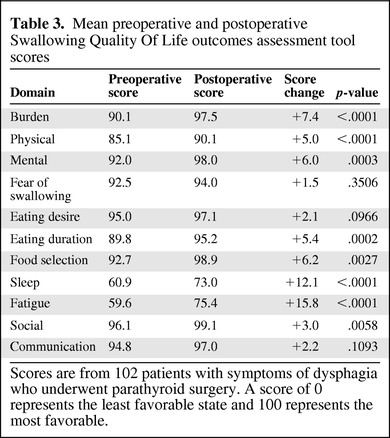
Scores are from 102 patients with symptoms of dysphagia who underwent parathyroid surgery. A score of 0 represents the least favorable state and 100 represents the most favorable.
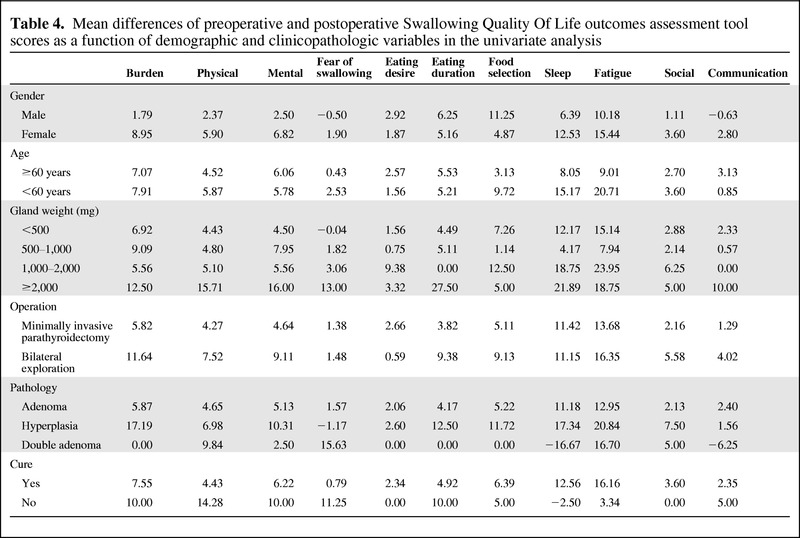
Associations between various demographic and clinicopathologic independent variables and changes in SWAL-QOL scores were measured by univariate analysis (Table 4). Female gender was associated with improvement in the domains of both burden (p = .027) and communication (p = .020). Patient age >60 years predicted a score increase in the fatigue domain (p = .019). Interestingly, biochemical cure following parathyroidectomy was associated with a decrease in the physical domain (p = .032). Although not statistically significant, the average difference in eating duration trended toward significance (p = .08) with regard to gland weight, with gland weight <500 mg demonstrating the lowest mean change. Multivariable modeling was not performed in the present study, as the univariate analysis failed to demonstrate more than one independent predictor of SWAL-QOL score change in any of the 11 domains.
Table 4.
Mean differences of preoperative and postoperative Swallowing Quality Of Life outcomes assessment tool scores as a function of demographic and clinicopathologic variables in the univariate analysis
Discussion
Clinical features that once prompted the possible diagnosis of hyperparathyroidism have become rare: nephrolithiasis, formerly seen in over half of primary hyperparathyroidism (pHPT) cases, is seen in less than 5%–20% of patients today [19, 20]. More drastic reductions have been noted in the incidence of osteopenia, a relatively common entity in patients with pHPT, and osteitis fibrosa cystica, which is currently seen in less than 5% of patients. Clearly, this evolution of pHPT to a “mild” or “asymptomatic” disease has led to considerable uncertainty regarding which patients with pHPT will truly benefit from operative therapy. Recent studies have shown that nearly 80% of patients with pHPT have nonspecific but nonetheless real symptoms that do not meet the current National Institutes of Health guidelines for operative intervention [19, 21–24]. Among these subtle, potentially reversible symptoms, oropharyngeal dysphagia may develop in patients with parathyroid disease. However, dysphagia in this patient population has not been studied in a prospective manner. Little is known about the prevalence of dysphagia in patients with parathyroid disease or whether swallowing-related symptoms improve following surgical treatment.
In this study, we used a condition-specific instrument—the SWAL-QOL outcomes assessment tool—to assess swallowing-related QOL in patients with parathyroid disease before and after parathyroid surgery. We found that mean preoperative SWAL-QOL scores were <90 for 4 of the 11 domains, indicating the perception of oropharyngeal dysphagia and diminished quality of life. Following parathyroidectomy, statistically significant improvements were demonstrated in eight SWAL-QOL domains. Finally, several patient-, disease-, and treatment-related factors predicted score improvement in multiple SWAL-QOL domains.
The impact of dysphagia on QOL in aging cohorts remains unclear. In the present study, mean preoperative SWAL-QOL domain scores were lower than those reported by McHorney et al. for a sample of 40 “normal” swallowers in all but three SWAL-QOL domains (eating desire, food selection, and communication) [18]; conversely, mean preoperative scores were higher than those reported by Greenblatt et al. for a sample of 116 patients with thyroid disease in all but two SWAL-QOL domains (sleep and fatigue) [6]. The mean age of the parathyroid disease group was 60 years, compared to 73 years for the normal cohort and 49 years for the thyroid disease group. Prior research has shown that aging may affect swallowing function [25], and older patients who experience dysphagia have decreased QOL, social isolation, and depression [26–28]. However, in the only known study evaluating the impact of dysphagia on QOL in healthy aging patients that used the SWAL-QOL survey, Leow and colleagues showed that healthy older adults experience symptoms of dysphagia more frequently than healthy young adults, but the overall SWAL-QOL scores were not significantly different [28]. Taken together, these data suggest that differences in age make comparisons of SWAL-QOL score profiles from different published studies problematic.
To date, the SWAL-QOL instrument has been used to evaluate swallowing-related QOL in patients with systemic diseases, such as Parkinson disease (PD) [28] or chronic obstructive pulmonary disease [29], or to measure changes in swallowing-related QOL in patients undergoing surgical treatment for head and neck pathology [3, 30]. Leow et al. administered the SWAL-QOL instrument to 32 patients with idiopathic PD in New Zealand [28]. Compared to the patients with early-stage PD, the patients with parathyroid disease in our series had higher baseline mean scores in all SWAL-QOL domains except sleep and fatigue; however, the latter two domains were so much lower in the parathyroid cohort that the mean SWAL-QOL score across all subsections was statistically no different (83.7 for PD vs. 86.3 for parathyroid disease, p = .6454). Patients with parathyroid disease also scored much lower in the SWAL-QOL domains of sleep and fatigue at baseline when compared to patients with thyroid disease [6], tongue cancer [30], and nasopharyngeal carcinoma (sleep only) [3].
Importantly, after parathyroid surgery, mean SWAL-QOL scores in the sleep and fatigue domains increased more than any of the other nine domains, with improvements in each being very statistically significant (p ≤ .0001). These disease-specific QOL improvements are supported by prospective analyses of patients with pHPT by Perrier et al. [31, 32]. In these studies, Perrier et al. used functional magnetic resonance imaging (fMRI), formal neuropsychiatric testing, and health-related QOL scores to assess sleep dysfunction before and after parathyroid surgery for pHPT. Interestingly, fMRI demonstrated postoperative changes in cortical activity during cognitive processing of both conflict and nonconflict tasks, with resultant improvements in sleep and social behavior. It is therefore possible that a significant component of improved swallowing-related QOL in patients with parathyroid disease may not be attributable to resolution of physical compression alone, but rather to changes in cortical activity in brain centers controlling sleep, fatigue, and/or swallowing.
A significant negative correlation was found between the physical domain score and biochemical cure of hyperparathyroidism (p = .032), suggesting the average change in physical score is lower for cured patients than uncured patients. Interestingly, 5 of 5 (100%) noncured patients were women and 4 of 5 (80%) underwent bilateral exploration. Both clinicopathologic variables demonstrate higher average change in the physical domain scores than male sex and minimally invasive parathyroidectomy, respectively, suggesting that these unique variables may contribute to this finding. However, to date, the determinants of this negative correlation remain uncertain and require further exploration.
Summary
In conclusion, these data demonstrate a high prevalence of dysphagia among patients undergoing parathyroidectomy for hyperparathyroidism, and they delineate the negative impact of dysphagia on QOL. More importantly, in these patients with symptoms of dysphagia, parathyroid surgery leads to significant improvements in many aspects of swallowing-related quality of life measured by the SWAL-QOL instrument. This research, to our knowledge, represents the first use of a condition-specific instrument to assess swallowing-related QOL in patients with parathyroid disease before and after parathyroid surgery.
Acknowledgments
This work was supported by the National Institutes of Health (T32 CA090217).
Author Contributions
Conception/Design: Sarah Schaefer, Rebecca Sippel, Herbert Chen
Provision of study material or patients: Sarah Schaefer, Herbert Chen
Collection and/or assembly of data: Linda Youngwirth, Sarah Schaefer
Data analysis and interpretation: Scott N. Pinchot, Linda Youngwirth, Victoria Rajamanickam, Rebecca Sippel, Herbert Chen
Manuscript writing: Scott N. Pinchot, Rebecca Sippel, Herbert Chen
Final approval of manuscript: Scott N. Pinchot, Linda Youngwirth, Sarah Schaefer, Rebecca Sippel, Herbert Chen
References
- 1.Howden CW. Management of acid-related disorders in patients with dysphagia. Am J Med. 2004;117(Suppl 5A):44S–48S. doi: 10.1016/j.amjmed.2004.07.017. [DOI] [PubMed] [Google Scholar]
- 2.Palmer JB, Drennan JC, Baba M. Evaluation and treatment of swallowing impairments. Am Fam Physician. 2000;61:2453–2462. [PubMed] [Google Scholar]
- 3.Lovell SJ, Wong HB, Loh KS, et al. Impact of dysphagia on quality-of-life in nasopharyngeal carcinoma. Head Neck. 2005;27:864–872. doi: 10.1002/hed.20250. [DOI] [PubMed] [Google Scholar]
- 4.Yu CL, Fielding R, Chan CL. The mediating role of optimism on post-radiation quality of life in nasopharyngeal carcinoma. Qual Life Res. 2003;12:41–51. doi: 10.1023/a:1022024827171. [DOI] [PubMed] [Google Scholar]
- 5.Ekberg O, Hamdy S, Woisard V, et al. Social and psychological burden of dysphagia: Its impact on diagnosis and treatment. Dysphagia. 2002;17:139–146. doi: 10.1007/s00455-001-0113-5. [DOI] [PubMed] [Google Scholar]
- 6.Greenblatt DY, Sippel R, Leverson G, et al. Thyroid resection improves perception of swallowing function in patients with thyroid disease. World J Surg. 2009;33:255–260. doi: 10.1007/s00268-008-9837-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fraser WD. Hyperparathyroidism. Lancet. 2009;374:145–158. doi: 10.1016/S0140-6736(09)60507-9. [DOI] [PubMed] [Google Scholar]
- 8.Chen H. Surgery for primary hyperparathyroidism: What is the best approach? Ann Surg. 2002;236:552–553. doi: 10.1097/00000658-200211000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen H, Mack E, Starling JR. A comprehensive evaluation of perioperative adjuncts during minimally invasive parathyroidectomy: Which is most reliable? Ann Surg. 2005;242:375–380. doi: 10.1097/01.sla.0000179622.37270.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen H, Wang TS, Yen TW, et al. Operative failures after parathyroidectomy for hyperparathyroidism: The influence of surgical volume. Ann Surg. 2010;252:691–695. doi: 10.1097/SLA.0b013e3181f698df. [DOI] [PubMed] [Google Scholar]
- 11.Trippe BS, Shaprio JR, Doppman JL. Dysphagia. Initial symptom of an ectopic hyperfunctioning parathyroid adenoma. JAMA. 1976;235:58–9. doi: 10.1001/jama.235.1.58. [DOI] [PubMed] [Google Scholar]
- 12.Korkis AM, Miskovitz PF. Acute pharyngoesophageal dysphagia secondary to spontaneous hemorrhage of a parathyroid adenoma. Dysphagia. 1993;8:7–10. doi: 10.1007/BF01351471. [DOI] [PubMed] [Google Scholar]
- 13.Maweja S, Sebag F, Hubbard J, et al. Spontaneous cervical haematoma due to extracapsular haemorrhage of a parathyroid adenoma: a report of 2 cases. Ann Chir. 2003;128:561–562. doi: 10.1016/s0003-3944(03)00184-6. [DOI] [PubMed] [Google Scholar]
- 14.Shundo Y, Nogimura H, Kita Y, et al. Spontaneous parathyroid adenoma hemorrhage. Jpn J Thorac Cardiovasc Surg. 2002;50:391–394. doi: 10.1007/BF02913192. [DOI] [PubMed] [Google Scholar]
- 15.Grieve RJ, Dixon PF. Dysphagia: A further symptom of hypercalcaemia? Br Med J (Clin Res Ed) 1983;286:1935–1936. doi: 10.1136/bmj.286.6382.1935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McHorney CA, Bricker DE, Kramer AE, et al. The SWAL-QOL outcomes tool for oropharyngeal dysphagia in adults: I. Conceptual foundation and item development. Dysphagia. 2000;15:115–121. doi: 10.1007/s004550010012. [DOI] [PubMed] [Google Scholar]
- 17.McHorney CA, Bricker DE, Robbins J, et al. The SWAL-QOL outcomes tool for oropharyngeal dysphagia in adults: II. Item reduction and preliminary scaling. Dysphagia. 2000;15:122–133. doi: 10.1007/s004550010013. [DOI] [PubMed] [Google Scholar]
- 18.McHorney CA, Robbins J, Lomax K, et al. The SWAL-QOL and SWAL-CARE outcomes tool for oropharyngeal dysphagia in adults: III. Documentation of reliability and validity. Dysphagia. 2002;17:97–114. doi: 10.1007/s00455-001-0109-1. [DOI] [PubMed] [Google Scholar]
- 19.Silverberg S, Bilezikian J, Bone H, et al. Therapeutic controversies in primary hyperparathyroidism. J Clin Endocrinol Metab. 1999;84:2275–2285. doi: 10.1210/jcem.84.7.5842-1. [DOI] [PubMed] [Google Scholar]
- 20.Toft A. Surgery for primary hyperparathyroidism: Sooner rather than later. Lancet. 2000;355:1478–1479. doi: 10.1016/s0140-6736(00)02158-9. [DOI] [PubMed] [Google Scholar]
- 21.Caron N, Pasieka J. What symptom improvement can be expected after operation for primary hyperparathyroidism? World J Surg. 2009;33:2244–2255. doi: 10.1007/s00268-009-9987-4. [DOI] [PubMed] [Google Scholar]
- 22.Chan A, Duh Q, Katz M, et al. Clinical manifestations of primary hyperparathyroidism before and after parathyroidectomy. A case-control study. Ann Surg. 1995;222:402–412. doi: 10.1097/00000658-199509000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.NIH conference. Diagnosis and management of asymptomatic primary hyperparathyroidism: Consensus development conference statement. Ann Intern Med. 1991;114:593–597. doi: 10.7326/0003-4819-114-7-593. [DOI] [PubMed] [Google Scholar]
- 24.Bilezikian J, Khan A, Potts JJ. Guidelines for the management of asymptomatic primary hyperparathyroidism: Summary statement from the third international workshop. J Clin Endocrinol Metab. 2009;94:335–339. doi: 10.1210/jc.2008-1763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yoshikawa M, Yoshida M, Nagasaki T, et al. Aspects of swallowing in healthy dentate elderly persons older than 80 years. J Gerontol A Biol Sci Med Sci. 2005;60:506–509. doi: 10.1093/gerona/60.4.506. [DOI] [PubMed] [Google Scholar]
- 26.de Luis DA, Izaola O, de Mateo ML, et al. Quality of life and dietary intake in elderly patients with dysphagia. Nutrition. 2006;22:584. doi: 10.1016/j.nut.2006.01.004. [DOI] [PubMed] [Google Scholar]
- 27.Miller N, Noble E, Jones D, et al. Life with communication changes in Parkinson's disease. Age Ageing. 2006;35:235–239. doi: 10.1093/ageing/afj053. [DOI] [PubMed] [Google Scholar]
- 28.Leow LP, Huckabee ML, Anderson T, et al. The impact of dysphagia on quality of life in ageing and Parkinson's disease as measured by the swallowing quality of life (SWAL-QOL) questionnaire. Dysphagia. 2010;25:216–220. doi: 10.1007/s00455-009-9245-9. [DOI] [PubMed] [Google Scholar]
- 29.McKinstry A, Tranter M, Sweeney J. Outcomes of dysphagia intervention in a pulmonary rehabilitation program. Dysphagia. 2010;25:104–111. doi: 10.1007/s00455-009-9230-3. [DOI] [PubMed] [Google Scholar]
- 30.Costa Bandeira AK, Azevedo EH, Vartanian JG, et al. Quality of life related to swallowing after tongue cancer treatment. Dysphagia. 2008;23:183–192. doi: 10.1007/s00455-007-9124-1. [DOI] [PubMed] [Google Scholar]
- 31.Mittendorf EA, Wefel JS, Meyers CA, et al. Improvement of sleep disturbance and neurocognitive function after parathyroidectomy in patients with primary hyperparathyroidism. Endocr Pract. 2007;13:338–344. doi: 10.4158/EP.13.4.338. [DOI] [PubMed] [Google Scholar]
- 32.Perrier N, Coker L, Rorie K, et al. Preliminary report: Functional MRI of the brain may be the ideal tool for evaluating neuropsychologic and sleep complaints of patients with primary hyperparathyroidism. World J Surg. 2006;30:686–696. doi: 10.1007/s00268-005-0361-x. [DOI] [PubMed] [Google Scholar]


