Abstract
An unusual case of palmar implantation dermoid causing paresthesia in the fingers is reported. The tumor was successfully excised with relief of the symptoms. The report discusses important points regarding management of such tumors.
Keywords: Epidermoid cyst, implantation dermoid, inclusion cyst, hand tumour
INTRODUCTION
Soft tissue tumors of the hand are a frequently seen entity, and may arise from any tissue of the hand. Most of them present as a painless superficial swelling and seldom place nerve, vessel or tendons at risk. We present here an interesting case of palmar implantation dermoid causing paresthesia in the fingers. Surgical excision safeguarding the neurovascular bundle was performed with uneventful recovery.
CASE REPORT
A 26-year-old, right-handed computer professional presented with a swelling in the left palm with associated tingling in the ring and little fingers. [Figure 1] The patient sustained a knife injury on the palm while cutting vegetables 1 year ago. For the last 8 months, the patient noticed a gradually increasing painless swelling in the left palm and started experiencing tingling in the ring and little fingers since 2 months. The clinical examination revealed a 2.5 cm × 2.5 cm smooth, nontender, nonmobile, noncompressible firm swelling over the volar aspect of the distal palmar crease adjacent to the IVth web space of the left hand. There was paresthesia of the left ring and little fingers, but no distinct neural deficit was noted. The plain radiograph was suggestive of features of soft tissue swelling. A clinical diagnosis of implantation dermoid was made and the swelling was completely excised under brachial block, under loupe magnification with proximal tourniquet control. The encapsulated swelling was carefully dissected from the underlying flexor tendons safeguarding the common digital neurovascular bundles [Figure 2]. The specimen measured 2.8 cm × 2.8 cm and histopathological analysis confirmed the diagnosis of epidermoid inclusion cyst. The patient became symptom-free, with complete recovery from paresthesia after the surgery [Figure 3].
Figure 1.
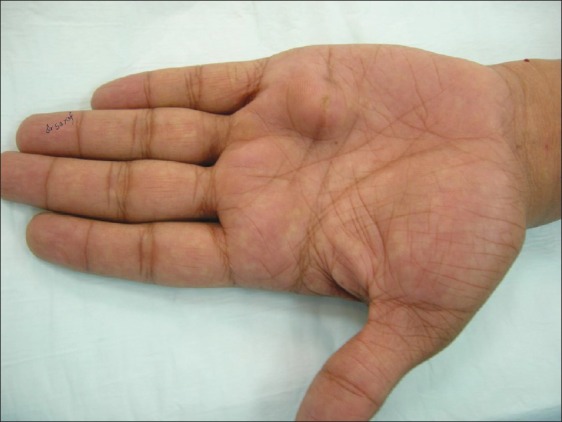
Swelling in the left palm
Figure 2.
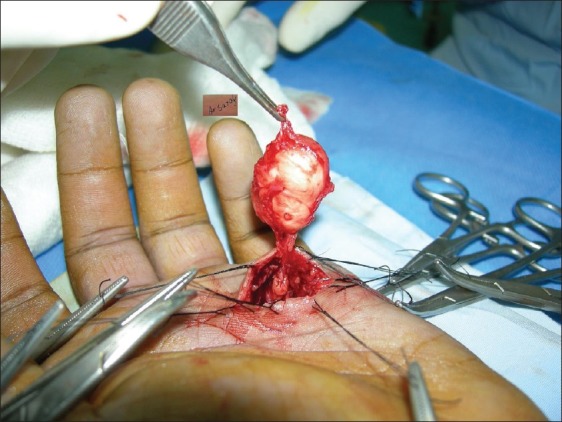
Safe dissection from the underlying neurovascular structures
Figure 3.

One month post-op
DISCUSSION
True epidermoid inclusion cysts result from the implantation of epidermal elements in the dermis, and can result from any trauma or surgical procedure. Theoretically, any skin puncture, laceration or incision has the potential to implant epidermal elements into the dermis and subcutaneous tissue, where continued production of keratin and other epidermal products produces a thick-walled cyst containing white cheesy material.[1] They are frequently seen in farmers, factory workers, carpenters and tailors who are subject to repeated minor traumas to the hand.[2] They are occasionally seen in the scars of surgical incisions and following other surgical procedures of the hand. HPV infection, ultraviolet exposure and eccrine duct obstruction are also suggested to be the additional factors in the development of palmoplantar epidermoid cysts.[3–5]
The epidermoid inclusion cysts of the hands usually present as asymptomatic, slowly enlarging, painless, superficial localized swellings over the volar aspect of the hand, especially the distal portion of the digits. Occasional cases of epidermoid inclusion cyst arising from deeper structures like tendon and phalangeal bones have also been reported.[6–8] Clinically, the phalangeal lesions typically arise in the distal phalanx and present with variable degrees of pain, swelling, nail deformity[9] and, sometimes, erythema. Some of the studies have proposed the origin of phalangeal cyst due to direct traumatic implantation of epidermal fragments into the bone or migration of a fragment of the nail bed into the bone or faulty embryogenesis.[10,11] The epidermoid cysts are usually benign lesions; however, rare cases of malignancies have also been reported.[12–14]
Because epidermoid inclusion cysts are often site-specific, the history of associated trauma and basic clinical examination is enough to clinch the diagnosis. The imaging studies do not lead to definitive diagnosis but are advised as part of a comprehensive evaluation. X-ray is the basic study usually asked for. Ultrasonography may occasionally be useful while computed tomography and magnetic resonance imaging[15] are helpful in delineating the anatomy of the soft tissue tumors, although seldom necessary to guide the treatment. Fine needle aspiration cytology (FNAC) may often be helpful in making cytological diagnosis if enough keratin or sebaceous material is obtained. Histologically, the inclusion epidermoid cysts are lined with stratified squamous epithelium with granular cell layer and are filled with eosinophilic lamellated keratinous material. The inflammatory response may or may not be present and, in the cysts of long duration, calcification may be seen.
Epidermoid inclusion cysts of the hand need to be differentiated from ganglions, giant cell tumors of the tendon sheath, lipomas and bony and arthropathic swellings.[16,17]
Because most of the hand dermoid cysts are benign and asymptomatic, surgical intervention is not warranted. The surgical treatment is needed for symptomatic cysts causing interference with hand function. The treatment requires careful complete excision, which can easily be accomplished with regional anesthesia under pneumatic tourniquet.[18] Removal of the entire cyst wall is necessary to avoid the recurrence.[19]
SUMMARY
Soft tissue tumors of the hand are quite common and can arise from any structure from skin down to the bone. The detailed clinical history and evaluation often clinches the diagnosis. Asymptomatic cases can be conservatively managed while symptomatic cases require surgical excision. Adequate knowledge of hand anatomy, meticulous dissection and magnification is a must to avoid the risk of damage to the underlying neurovascular structures.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Lucas GL. Epidermoid inclusion cysts of the hand. J South Orthop Assoc. 1999;8:188–92. [PubMed] [Google Scholar]
- 2.McFarland GB. Soft tissue tumors. In: Green DP, editor. Operative hand surgery. 2nd ed. New York: Churchill Livingstone; 1988. [Google Scholar]
- 3.Egawa K, Honda Y, Inaba Y, Ono T, De Villiers EM. Detection of human papillomaviruses and eccrine ducts in palmoplantar epidermoid cysts. Br J Dermatol. 1995;132:533–42. doi: 10.1111/j.1365-2133.1995.tb08707.x. [DOI] [PubMed] [Google Scholar]
- 4.Egawa K, Kitasato H, Ono T. A palmar epidermoid cyst, showing histological features suggestive of eccrine duct origin, developing after a bee-string. Br J Dermatol. 2000;143:469–70. doi: 10.1046/j.1365-2133.2000.03697.x. [DOI] [PubMed] [Google Scholar]
- 5.Park HS, Kim WS, Lee JH, Yang JM, Lee ES, Jang KT, et al. Association of human papillomavirus infection with palmoplantar epidermal cysts in Korean patients. Acta Derm Venereol. 2005;85:404–8. doi: 10.1080/00015550510032878. [DOI] [PubMed] [Google Scholar]
- 6.O’Hara JJ, Stone JH. An intratendinous epidermoid cyst after trauma. J Hand Surg Am. 1990;15:477–9. doi: 10.1016/0363-5023(90)90065-y. [DOI] [PubMed] [Google Scholar]
- 7.Hinrichs RA. Epidermoid cyst of the terminal phalanx of the hand.Case report and brief review. JAMA. 1965;194:1253–4. [PubMed] [Google Scholar]
- 8.Hamad AT, Kumar A, Anand Kumar C. Intraosseous epidermoid cyst of the finger phalanx: A case report. J Orthop Surg (Hong Kong) 2006;14:340–2. doi: 10.1177/230949900601400322. [DOI] [PubMed] [Google Scholar]
- 9.Baran R, Broutart JC. Epidermoid cyst of the thumb presenting as pincer nail. J Am Acad Dermatol. 1988;19:143–4. doi: 10.1016/s0190-9622(88)80236-6. [DOI] [PubMed] [Google Scholar]
- 10.Handa U, Kumar S, Mohan H. Aspiration cytology of epidermoid cyst of terminal phalanx. Diagn Cytopathol. 2002;26:266–7. doi: 10.1002/dc.10075. [DOI] [PubMed] [Google Scholar]
- 11.Mcgraw P, Bonvento B, Moholkar K. Phalangeal intraosseous epidermoid cyst. Acta Orthop Belg. 2004;70:365–7. [PubMed] [Google Scholar]
- 12.Bauer B. Carcinoma arising in a sebaceous cyst. IMJ Ill Med J. 1979;156:174–6. [PubMed] [Google Scholar]
- 13.Lopez-Rios F, Rodriguez-Peralto JL, Castano E, Benito A. Squamous cell carcinoma arising in a cutaneous epidermal cyst: Case report and literature review. Am J Dermatopathol. 1999;21:174–7. doi: 10.1097/00000372-199904000-00012. [DOI] [PubMed] [Google Scholar]
- 14.Cameron DS, Hilsinger RL., Jr Squamous cell carcinoma in an epidermal inclusion cyst: Case report. Otolaryngol Head Neck Surg. 2003;129:141–3. doi: 10.1016/S0194-59980300466-2. [DOI] [PubMed] [Google Scholar]
- 15.Horcajadas AB, Lafuente JL, de la Cruz Burgos R, Muñiz SH, Roca SA, Ortega SG, et al. Ultrasound and MR findings in tumor and tumor-like lesions of the fingers. Eur Radiol. 2003;13:672–85. doi: 10.1007/s00330-002-1477-0. [DOI] [PubMed] [Google Scholar]
- 16.Lucas GL. Epidermoid inclusion cysts of the hand. J South Orthop Assoc. 1999;8:188–92. [PubMed] [Google Scholar]
- 17.Goebel SX, Rasi LM, Stern PJ. Multiple epidermal inclusion cysts in a patient with rheumatoid arthritis: A case report. J Hand Surg Am. 2000;25:768–71. doi: 10.1053/jhsu.2000.8641. [DOI] [PubMed] [Google Scholar]
- 18.Ariyan S. Benign and Malignant Soft Tissue Tumors of the hand. In: McCarthy JG, editor. Plastic Surgery. United States: WB Saunders Company; 1990. [Google Scholar]
- 19.Lincoski CJ, Bush DC, Millon SJ. Epidermoid cysts in the hand. J Hand Surg Eur Vol. 2009;34:792–6. doi: 10.1177/1753193409347509. [DOI] [PubMed] [Google Scholar]


