Abstract
A 7-day-old premature female infant presented with rapidly progressive, erythematous, annular skin lesions from the 5th day of life. She was diagnosed provisionally as a case of neonatal lupus erythematosus and was investigated accordingly. Histopathological examination of the skin biopsy specimen revealed presence of hyphae of dermatophytes in the stratum corneum, and the diagnosis was changed to tinea corporis. Differential diagnosis of the annular erythema of infancy has been discussed and the importance of scraping a scaly lesion for KOH preparation in the diagnostic work-up of such a patient has been highlighted.
Keywords: Annular erythema, neonatal lupus erythematosus, tinea corporis
INTRODUCTION
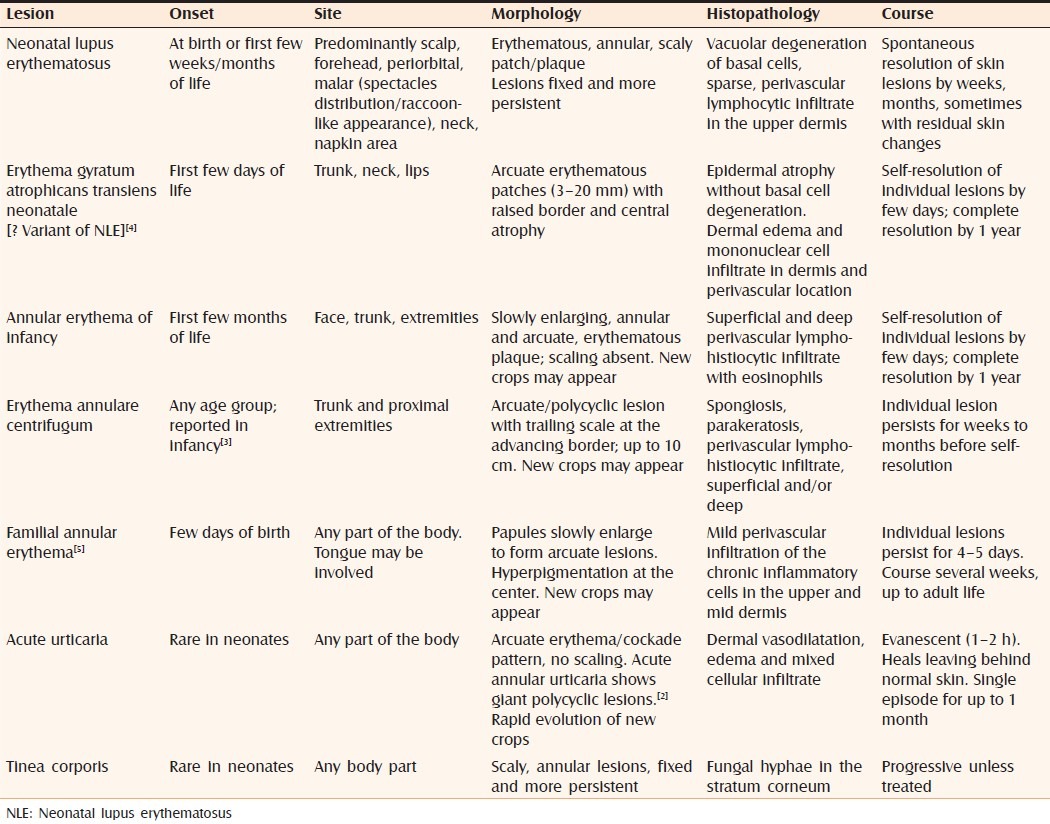
Skin lesions that are described under the broad rubric of ‘Annular erythemas’ can be arcuate, circinate, polycyclic or serpiginous, which may spread centrifugally or remain fixed.[1] Such skin lesions are not so common during the neonatal period. Various causes of annular erythema during the first few days or weeks of life have been presented in Table 1.[1–5] These vary from benign conditions like “annular erythema of infancy” to “neonatal lupus erythematosus (NLE),” with serious systemic involvement. Hence, differentiation of these conditions is of immense importance for effective management. Occurrence of erythema annulare centrifugum, acute urticaria and tinea corporis (TC) are only incidental during the initial days of life. Erythema chronicum migrans, although mentioned as one of the differential diagnoses of annular erythema of infancy, has not been reported at a very early age.
Table 1.
CASE REPORT
A 7-day-old, pre-term, female neonate under observation at the intensive care unit was referred for evaluation of the skin lesions that appeared on the 5th post-partum day and thereafter progressed rapidly.
The infant's mother was a 23-year-old healthy primigravida, with uneventful course of pregnancy until 34 weeks, when there was premature rupture of membrane with evidence of fetal distress necessitating emergency lower segment caesarean section.
Clinical examination revealed an alert infant weighing 1.98 kg with good reflexes. A cutaneous examination showed multiple brightly erythematous, annular lesions distributed over the neck, back, arms and dorsa of the hands, sparing the face [Figure 1]. The center of the lesions showed fine, detachable scales without any atrophy. Individual lesions were persistent and enlarging since their appearance.
Figure 1.

Erythematous annular lesions on the back of the neonate
A provisional diagnosis of NLE was considered in this case and the infant was investigated accordingly. The mother did not suffer from any remarkable illness since childhood. There was also no history suggestive of photosensitivity or any active collagen vascular disorder.
Complete hemogram and urinalysis of both the infant and the mother were within normal limits. Cardiac screening of the infant did not reveal any conduction defect. The Venereal Diseases Research Laboratory test was negative in the mother. Antinuclear antibody and antibodies against SS-A/Ro and SS-B/La were not detectable in the mother or the child. A skin biopsy was performed from one of the skin lesions on the back of the infant.
The H&E stained skin biopsy specimen showed hyperkeratotic and acanthotic epidermis with the presence of tubular structures in the stratum corneum suggestive of fungal hyphae. The dermis was unremarkable. A Periodic Acid Schiff stain confirmed the presence of fungal hyphae in the stratum corneum [Figure 2].
Figure 2.
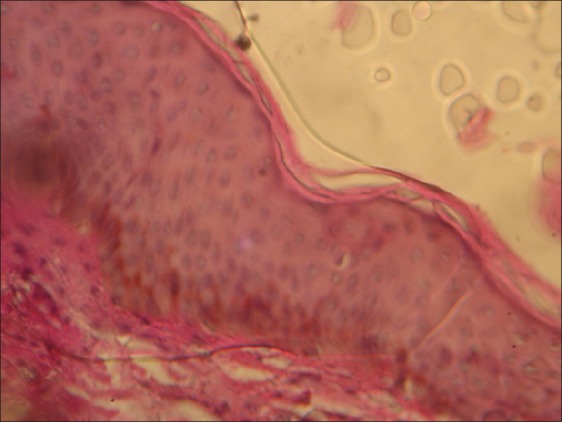
Histopathological section of the skin showing fungal hyphae (Periodic Acid Schiff stain, ×100)
The diagnosis was revised as “tinea corporis” and the infant was advised topical application of terbinafine hydrochloride cream (1%) once daily. The source of the infection was searched and the child's grandmother, who used to handle the child bare-handed while assisting breast-feeding, was found to have onychomycosis of a few finger nails. With topical antifungal treatment, the infant's skin lesions improved significantly in 2 weeks and there was complete clearance in 4 weeks. The baby's grandmother was advised monthly pulse therapy with systemic terbinafine.
DISCUSSION
Clinically, annular erythemas of infancy can be distinguished by mode of onset, evolution, distribution and morphology of skin lesions, associated features and family history [Table 1]. Clinical diagnosis is confirmed by laboratory tests. A battery of tests may be required for differentiation of these conditions. Scraping and potassium hydroxide (KOH) preparation from scale detects fungal hyphae in cases with TC. Presence of thrombocytopenia and positivity for markers of collagen vascular disorders (antinuclear antibody, anti-Ro/anti-La antibody) on screening of mother and child are suggestive of NLE. According to some authors, an anti-Ro/anti-La antibody test should be performed in all cases of annular skin lesions in infancy to avoid missing a diagnosis of NLE.[6] Cardiac screening with electrocardiogram for conduction defects is a must in such cases. Histopathological examination of the skin biopsy sample taken from the edge of the annular lesion is helpful in the diagnosis of the condition.
Dermatophyte infection in the first few days of life is not commonly encountered and hence not suspected in this case. However, this infection has been documented in neonates as early as on the 2nd day of life.[7] Different clinical variants of this infection occur among neonates, e.g. TC, tinea capitis, tinea faciei and onychomycosis.[7–10] In the published English literature, most frequent reports in the neonatal period are of tinea capitis. The inflammatory variant of tinea capitis, kerion, has also been reported in neonates.[11] Dermatophytic onychomycosis, although rare, may occur at this age.[10]
Any of the anthropophilic, geophilic or zoophilic dermatophytes may affect neonates. Dermatophytes known to cause neonatal infections are M. canis (commonest), T. tonsurans, T. rubrum, T. mentagrophytes, M. gypseum and T. violaceum.[12,13] There is a report of two species of fungi causing tinea capitis in an infant.[12] Transmission of these fungi from infected handlers, as in our case, is the usual mode of acquiring infection by the newborn.[13] Pet animals with active infection may be an important source of infection, transmitting zoophilic dermatophytes. Animals may also represent a healthy carrier state of M. gypseum, a geophilic fungus.[9] When the source of infection is not identifiable, fomites or household environment may be considered.[8]
Clinical features are usually similar to older children. Pre-mature, low-birth weight neonates may have a rapidly progressive infection due to inadequate barrier function of the skin, as in the index case.
Treatment of dermatophyte infection in neonates includes topical antifungals like azoles and terbinafine. Systemic antifungal drugs like itraconazole (3–5 mg/kg/day X 4–6 weeks) may be used for tinea capitis.[14] Pulse therapy with oral itraconazole solution has been used in older infants with tinea capitis.[8,14] Family members of the infected neonates must be examined and treated accordingly. Fomite and environmental decontamination should be considered too.
Annular erythema of infancy poses a diagnostic challenge for dermatologists. In the process of working up this case, an important lesson is learnt; scrape a scaly lesion, irrespective of its presentation and the age of the infant
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Horii KA, Nopper AJ. Textbook of pediatric dermatology. 2nd ed. Vol. 1. Oxford: Blackwell Science; 2006. Annular erythemas; pp. 718–25. [Google Scholar]
- 2.Tamayo-Sanchez L, Ruiz-Maldonado R, Laterza A. Acute annular urticaria in infants and children. Pediatr Dermatol. 1997;14:231–4. doi: 10.1111/j.1525-1470.1997.tb00246.x. [DOI] [PubMed] [Google Scholar]
- 3.Fried R, Schonberg IL, Lih JZ. Erythema annulare centrifugum (Darrier) in a newborn. J Pediatr. 1957;50:66–7. doi: 10.1016/s0022-3476(57)80014-6. [DOI] [PubMed] [Google Scholar]
- 4.Puig L, Moreno A, Alomar A, de Moragas JM. Erythema gyratum atrophicans transiens neonetale: A variant of cutaneous neonatal lupus erythematosus. Pediatr Dermatol. 1987;5:112–6. doi: 10.1111/j.1525-1470.1988.tb01150.x. [DOI] [PubMed] [Google Scholar]
- 5.Beare JM, Froggatt P, Jones JH, Neill DW. Familial annular erythema. Br J Dermatol. 1966;78:59–68. doi: 10.1111/j.1365-2133.1966.tb12176.x. [DOI] [PubMed] [Google Scholar]
- 6.Kettler AH, Stone MS, Bruce S, Tschen JA. Annular eruptions of infancy and neonatal lupus erythematosus. Arch Dermatol. 1987;123:298–9. [PubMed] [Google Scholar]
- 7.Ghorpade A, Ramanan C, Durairaj P. Trichophyton mentagrophytes infection in a two-day-old infant. Int J Dermatol. 1991;30:207–10. doi: 10.1111/j.1365-4362.1991.tb03854.x. [DOI] [PubMed] [Google Scholar]
- 8.Chang SE, Kang SK, Choi JH, Sung KJ, Moon KC, Koh JK. Tinea capitis due to Trichophyton rubrum in a neonate. Pediatr Dermatol. 2002;19:356–8. doi: 10.1046/j.1525-1470.2002.00100.x. [DOI] [PubMed] [Google Scholar]
- 9.Criado RP, Costa RA, Vasconcellos C, de Oliveira Ramos R, Silva CS, de Souza SFR. Tinea faciei in an infant caused by Microsporum gypseum simulating a dry impetigo. Pediatr Dermatol. 2005;22:536–8. doi: 10.1111/j.1525-1470.2005.00134.x. [DOI] [PubMed] [Google Scholar]
- 10.Sachdeva S, Gupta S, Prasher P, Aggarwal K, Jain VK, Gupta S. Trichophyton rubrum onychomycosis in a 10-week-old infant. Int J Dermatol. 2010;49:108–9. doi: 10.1111/j.1365-4632.2008.03969.x. [DOI] [PubMed] [Google Scholar]
- 11.Aste N, Pinna AL, Pau M, Biggio P. Kerion Celsi in a newborn due to Microsporum canis. Mycoses. 2004;47:236–7. doi: 10.1111/j.1439-0507.2004.00967.x. [DOI] [PubMed] [Google Scholar]
- 12.Ungar SL, Lande TA. Tinea capitis in a newborn caused by two organisms. Pediatr Dermatol. 1997;14:229–30. doi: 10.1111/j.1525-1470.1997.tb00245.x. [DOI] [PubMed] [Google Scholar]
- 13.Surpam RB, Deshpande SD, Saraswathi K, Amladi S, Savant S. Trichophyton violaceum: A rare isolate in 18-day-old neonate. Indian J Med Microbiol. 2006;24:292–3. doi: 10.4103/0255-0857.29391. [DOI] [PubMed] [Google Scholar]
- 14.Koumantaki E, Georgala S, Rallis E, Papadavid E. Microsporum canis tinea capitis in an 8-month old infant successfully treated with 2 weekly pulses of oral itraconazole. Pediatr Dermatol. 2001;18:60–2. doi: 10.1046/j.1525-1470.2001.018001060.x. [DOI] [PubMed] [Google Scholar]


