Abstract
This article reports the orthodontic treatment of a patient with skeletal mandibular retrusion and an anterior open bite due to temporomandibular joint osteoarthritis (TMJ-OA) using miniscrew anchorage. A 46-year-old woman had a Class II malocclusion with a retropositioned mandible. Her overjet and overbite were 7.0 mm and -1.6 mm, respectively. She had limited mouth opening, TMJ sounds, and pain. Condylar resorption was observed in both TMJs. Her TMJ pain was reduced by splint therapy, and then orthodontic treatment was initiated. Titanium miniscrews were placed at the posterior maxilla to intrude the molars. After 2 years and 7 months of orthodontic treatment, an acceptable occlusion was achieved without any recurrence of TMJ symptoms. The retropositioned mandible was considerably improved, and the lips showed less tension upon lip closure. The maxillary molars were intruded by 1.5 mm, and the mandible was subsequently rotated counterclockwise. Magnetic resonance imaging of both condyles after treatment showed avascular necrosis-like structures. During a 2-year retention period, an acceptable occlusion was maintained without recurrence of the open bite. In conclusion, correction of open bite and clockwise-rotated mandible through molar intrusion using titanium miniscrews is effective for the management of TMJ-OA with jaw deformity.
Keywords: Orthodontic mini-implant, TMJ, Orthodontic treatment
INTRODUCTION
The etiology underlying temporomandibular joint osteoarthritis (TMJ-OA) is not fully understood; however, some contributing factors are known, including internal derangement, macrotrauma, and parafunctional habits.1-3 In addition, functional overloading appears to be an important step in the cascade of events leading to osteoarthritis of the TMJ,1,4,5 which can lead to physical disruption of cells, impaired cellular function, transient ischemia of certain cell populations and the production of neurogenic irritants.4 As a result, the joint tissues collapse. If the joint collapse occurs in both TMJs, condylar resorption causes morphologic collapse of the TMJs and a subsequent decrease in ramus height, which results in progressive mandibular retrusion with anterior open bite.4 This is called acquired open bite associated with TMJ-OA.
The malocclusion and retrognathic facial profile associated with acquired open bite can be improved by orthognathic surgery, including maxillomandibular advancement with counterclockwise rotation. However, patients with active TMJ disease and concomitant or resultant maxillofacial skeletal discrepancies who are treated with orthognathic surgery alone often have poor outcomes and significant relapse.6-8 This implies that patients with presurgical TMJ symptoms requiring mandibular advancement appear to have an increased risk of condylar resorption.9 In addition, orthognathic surgery requires surgical invasion, which carries risks and can result in significant postoperative discomfort.10 However, no significant alternative treatment for these patients has yet been reported.
Therefore, we suggest orthodontic treatment for patients with skeletal mandibular retrusion and anterior open bite due to TMJ-OA, including molar intrusion, which has a beneficial effect on both esthetic appearance and occlusion. As a result of the counterclockwise rotation of the mandible caused by molar intrusion, the condyle is repositioned, and a functional adaptation in circumoral musculature can be achieved. Here, we present an adult case of acquired open bite associated with TMJ-OA treated using miniscrew anchorage.
DIAGNOSIS AND ETIOLOGY
A 46-year 9-month-old woman presented with mandibular retrusion and circumoral musculature strain on lip closure (Figure 1). She complained of maxillary protrusion and masticatory disturbance due to her open bite. Her facial profile was convex with a severely retropositioned mandible. No facial asymmetry was observed (Figure 1). She had a vertical and horizontal open bite and severe crowding of the upper anterior teeth. The only occlusal contacts were at the bilateral molars; however, significant abrasion was detected on the anterior teeth and premolars. Although the mandibular midline was shifted 2.4 mm to the left, the maxillary midline was nearly aligned with the facial midline. Overjet and overbite were 7.0 mm and -1.6 mm, respectively. The molar relationship was Angle Class III on the left side due to a missing lower left second premolar, and Angle Class I on the right side. During mandibular excursive movement, molar guidance with balancing side contacts was detected.
Figure 1.
Pretreatment photographs (age, 46 years 9 months).
In her history, she had been conscious of her retropositioned mandible and chin; but during the past several years, the retrognathia increased. There was no family history of rheumatism or osteoarthritis.
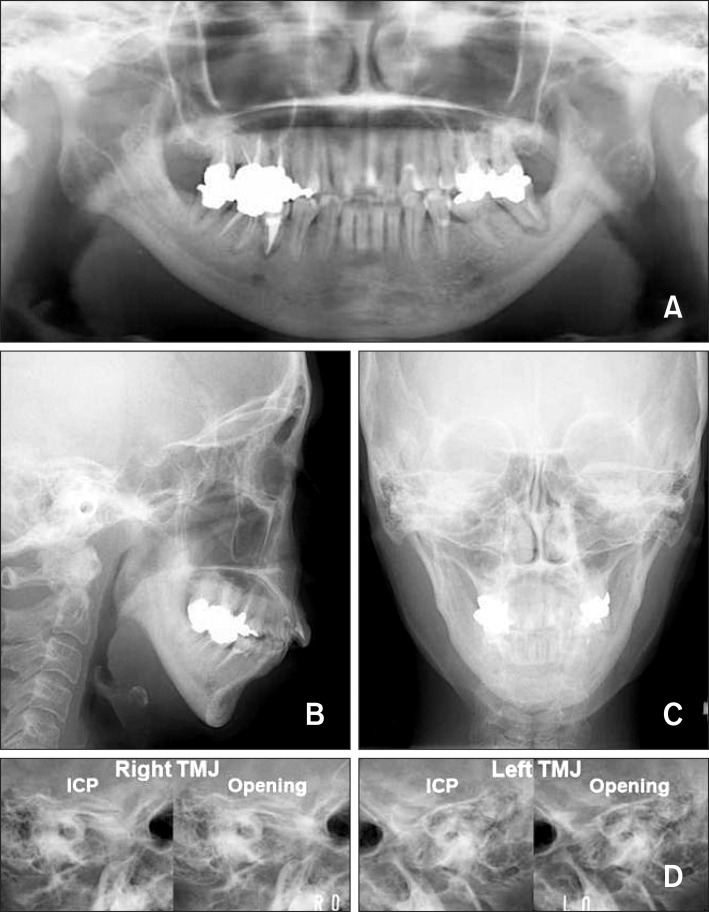
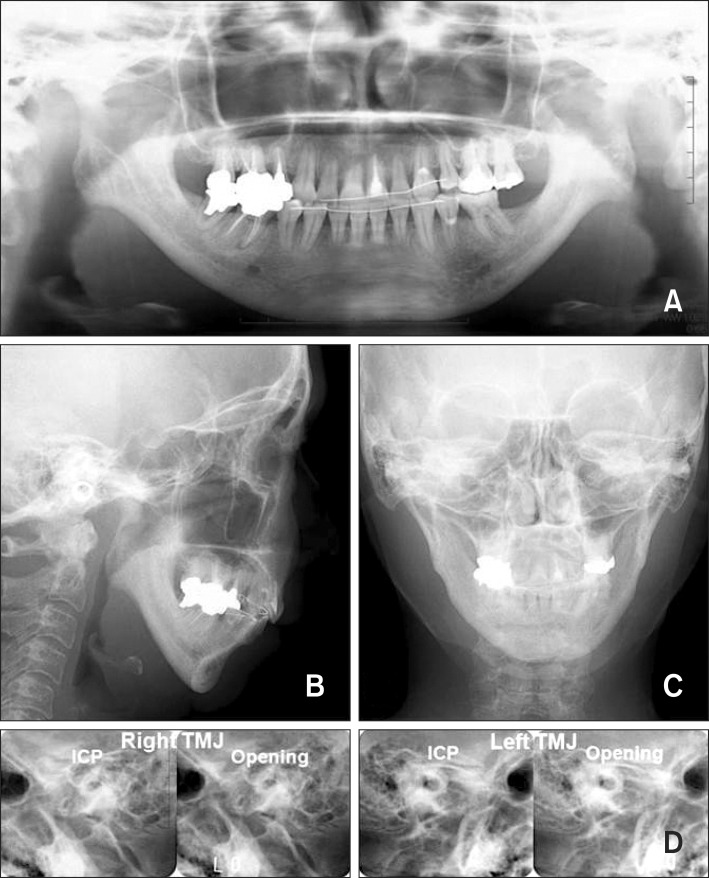
Model analysis showed an arch length discrepancy of -5.8 mm in the upper arch and -3.5 mm in the lower arch. Panoramic radiography showed the absence of the upper and lower third molars, and that the lower left second premolar had been extracted (Figure 2). The lower left second molar had little or no alveolar bone support and was a floating tooth. There was severe resorption and deformity in both condyles of the TMJs. Lateral transcranial radiography of the TMJ showed that both condyles were located anterior to the glenoid fossa, and no translations of the condyles were induced during mouth opening.
Figure 2.
Pretreatment records. A, Panoramic radiograph; B, lateral cephalograph; C, poster-anterior cephalograph; D, lateral transcranial radiograph of the temporomandibular joint (age, 46 years 9 months). ICP, Intercuspal position.
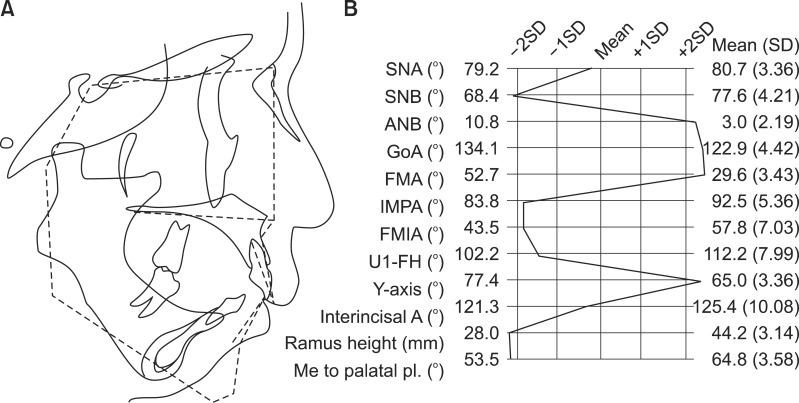
Cephalometric analysis revealed a skeletal Class II malocclusion with a severe retropositioned mandible (Figures 2 and 3). The mandibular plane and gonial angles were significantly larger than the Japanese norms (Frankfort-mandibular angle, 52.7°; Gonial angle, 134.1°).11 The mandible exhibited a backward and downward rotation with a short ramus. Although the inclination of the maxillary incisors was within the normal range, the lower incisors were labially inclined.
Figure 3.
Pretreatment cephalometric analysis. A, lateral cephalometric tracing (solid line) superimposed on the mean profilogram (dotted line); B, cephalometric measurements. SNA, Sella-Nasion-A point angle; SNB, Sella-Nasion-B point angle; ANB, A point-Nasion-B point angle; GoA, Gonial angle; FMA, Frankfort-mandibular angle; IMPA, Incisor-mandibular plane angle; FMIA, Frankfort-mandibular incisor angle; U1-FH, Axial inclination of the upper central incisor in relation to Frankfort plane; Y-axis, Angle between Frankfort plane and Sella-Gnathion line; Interincisal A, angle between the axial inclinations of the upper and lower central incisors; Ramus height, Length of the mandibular ramus (Articulare-Gonion); Me to palatal pl., Lower anterior facial height (Menton to palatal plane). SD, Standard deviation.
The patient had experienced frequent TMJ pain during mastication and at maximum mouth opening for at least 5 years. Maximum mouth opening without pain was 28.0 mm, and TMJ crepitus was detected on both sides. No muscle tenderness was observed on palpation.
TREATMENT OBJECTIVES
The diagnosis was skeletal open bite with a short mandibular ramus associated with TMJ-OA. The treatment objectives were to correct the anterior open bite, establish an ideal interincisal relationship, and to achieve an acceptable occlusion with a good functional Class I occlusion. This case was treated according to the following plan:
Extraction of both maxillary first premolars and the mandibular right second premolar.
Placement of multi-bracket appliances on both dentitions to align the teeth.
Placement of titanium miniscrews in both sides of the posterior maxilla to intrude the molars, since molar intrusion should lead to subsequent counterclockwise mandibular rotation.
Use of a transpalatal arch to prevent buccal tipping of the maxillary molars during intrusion.
TREATMENT ALTERNATIVES
To achieve an ideal overjet and overbite, several procedures were considered. Although mandibular advancement with orthognathic surgery is considered an effective treatment method, surgical treatment is not strongly recommended for patients with progressive mandibular retrusion associated with TMJ-OA. In addition, surgical treatment requires prolonged hospitalization and higher medical costs, and is the most invasive option. Therefore, conservative treatment was planned to achieve a positive overbite. We did not want to close the anterior open bite by extruding the anterior teeth, because the vertical relationship between the incisors and jaws was considered acceptable prior to orthodontic treatment, and tooth extrusion is generally considered an unstable movement. Therefore, intrusion of the maxillary molars and subsequent counterclockwise rotation of the mandible were considered good options to treat the anterior open bite in this patient.
TREATMENT PROGRESS
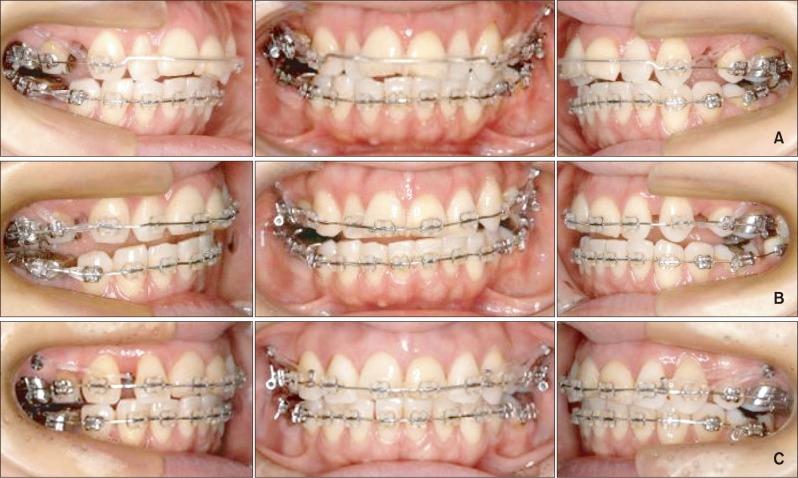
Three months after initiating splint therapy, her TMJ pain was reduced. Orthodontic treatment was then started using a multi-bracket appliance. A transpalatal arch was placed between the maxillary first molars, and both the upper first and the lower right second premolars were extracted. After the extraction, standard edgewise appliances with 0.018 × 0.025-inch slots were placed on both dentitions, except for the upper incisors (Figure 4A).
Figure 4.
Intraoral photographs during treatment. A, 6 months after the start of treatment; B, 12 months after the start of treatment; C, 18 months after the start of treatment.
After leveling and alignment, titanium miniscrews (Dual top anchor; Jeil Medical Co., Seoul, Korea) were placed at the buccal sites of the posterior maxilla, and molar intrusion and canine retraction were initiated using elastic chains from the anchor screws. At this time, the brackets were bonded onto the upper incisors. At 1 year, 0.016 × 0.022-inch Co-Cr alloy wires were placed on both arches (Figure 4B). As a result of molar intrusion, her anterior open bite was nearly corrected without the aid of vertical intermaxillary elastics. After intrusion, the canine and molar relationships were changed to almost Class I. At 1 year and 6 months, the space closing process and anterior retraction continued with the use of elastic chains from the miniscrews (Figure 4C).
After 2 years and 7 months of orthodontic treatment, an acceptable occlusion was achieved without any recurrence of TMJ symptoms, and the multi-bracket appliances were removed. Immediately after removal, lingual bonded retainers were fixed on both dentitions, and a wraparound retainer was added to the upper arch.
RESULTS
Her convex profile caused by the retrognathic mandible improved considerably (Figure 5). Her lips exhibited less lip tension upon lip closure. An acceptable occlusion was achieved, and overjet and overbite were increased to 2.2 mm and -0.7 mm, respectively. The canine and molar anteroposterior relationships were improved to Class I on both sides (Figure 5).
Figure 5.
Posttreatment photographs (age, 49 years 4 months).
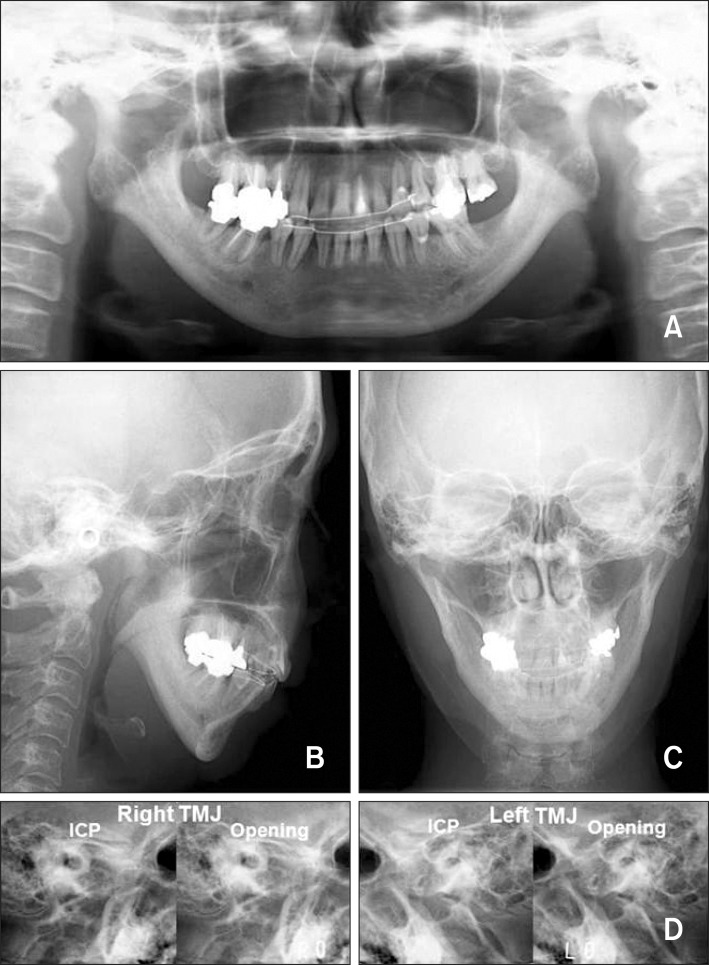
Panoramic radiography showed little or no changes in condylar structure (Figure 6). Lateral transcranial radiography of the TMJ showed that both condyles were still anterior to the glenoid fossa, and that condylar movements during mouth opening were still poor. Cephalometric analysis revealed approximately 1.5-mm maxillary molar intrusion and subsequent counterclockwise rotation of the mandible (Figure 7). Reduction of the excessive overjet was due to lingual inclination of the upper incisors.
Figure 6.
Posttreatment records. A, Panoramic radiograph; B, lateral cephalograph; C, poster-anterior cephalograph; D, lateral transcranial radiograph of the temporomandibular joint (TMJ) (age, 49 years 4 months). ICP, Intercuspal position.
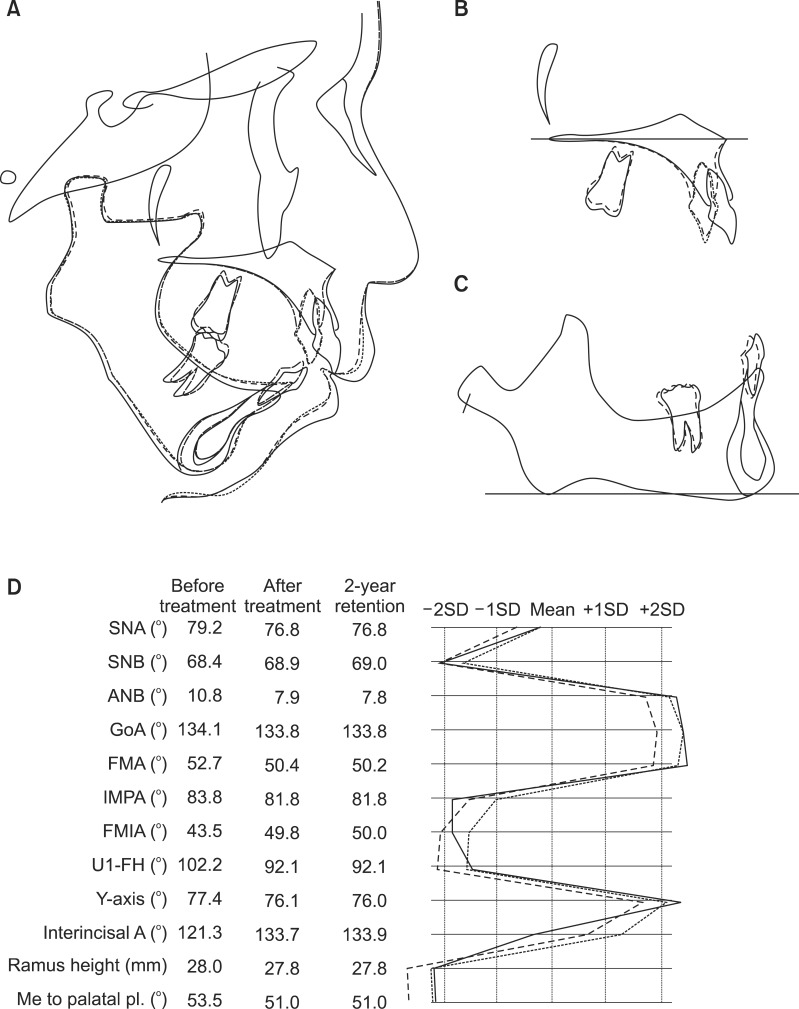
Figure 7.
Posttreatment and 2- year retention cephalometric analyses. Lateral cephalometric tracings at posttreatment (dotted line) and 2-year retention (double dotted line) superimposed on the pretreatment tracings (solid line) on the Sella-Nasion plane at Sella (A); on the palatal plane at Ptm' (B); and on the mandibular plane at Menton (C). Cephalometric measurements before treatment (solid line), after (dotted line) treatment, and at 2-year retention (double dotted line) (D). SNA, Sella-Nasion-A point angle; SNB, Sella-Nasion-B point angle; ANB, A point-Nasion-B point angle; GoA, Gonial angle; FMA, Frankfort-mandibular angle; IMPA, Incisor-mandibular plane angle; FMIA, Frankfort-mandibular incisor angle; U1-FH, Axial inclination of the upper central incisor in relation to Frankfort plane; Y-axis, Angle between Frankfort plane and Sella-Gnathion line; Interincisal A, angle between the axial inclinations of the upper and lower central incisors; Ramus height, Length of the mandibular ramus (Articulare-Gonion); Me to palatal pl., Lower anterior facial height (Menton to palatal plane). SD, Standard deviation.
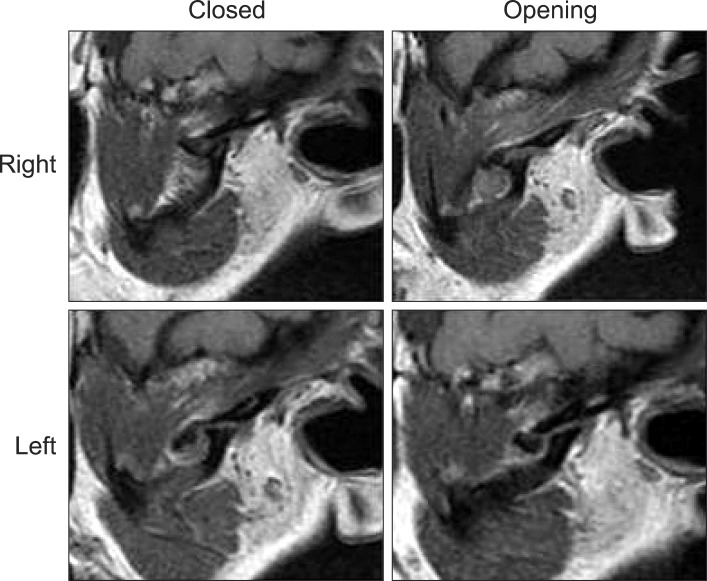
Throughout the treatment period, the patient experienced no recurrence of TMJ pain. Maximum mouth opening without pain was 38.0 mm; however, TMJ crepitus was still detected on both sides. Magnetic resonance imaging taken after treatment showed anterior disc displacement without reduction in both TMJs, and the condylar head was only black in color, which indicated cortical bone without cancellous bone and bone marrow, suggesting an avascular necrosis-like structure (Figure 8).
Figure 8.
Magnetic resonance imaging of the temporomandibular joint after active orthodontic treatment.
Two years after retention, the mandibular position was nearly unchanged (Figure 7). The circumoral musculature strain upon lip closure disappeared, and an acceptable occlusion was maintained without recurrence of TMJ symptoms (Figure 9). The shape of the upper central incisors improved with restorative treatment. The canine and molar relationships remained Class I, and no relapse of the anterior open bite was found. Overjet and overbite were 2.2 mm and 1.3 mm, respectively. Panoramic radiographs showed little or no change in condylar structure, with condylar resorption and deformity (Figure 10). Lateral transcranial radiography of the TMJ showed that the condylar movements during mouth opening were still poor.
Figure 9.
Two-year post retention photographs (age, 51 years 5 months).
Figure 10.
Two-year post retention records. A, Panoramic radiograph; B, lateral cephalograph; C, poster-anterior cephalograph; D, lateral transcranial radiograph of the temporomandibular joint (TMJ) (age, 51 years 5 months). ICP, Intercuspal position.
DISCUSSION
Although successful outcomes have been reported for orthognathic surgical management of maxillofacial skeletal discrepancies with signs and symptoms of TMJ disease,12 the outcomes depend on the pretreatment TMJ condition. Orthognathic surgeries in patients with active TMJ disease and concomitant or resultant maxillofacial skeletal discrepancies often have poor results and significant relapse.6-8,13,14 This implies that patients with TMJ symptoms have an increased risk of condylar resorption. Symptomatic and asymptomatic pre-existing TMJ pathologies that can lead to unfavorable outcomes include the following; internal derangements, progressive condylar resorption, condylar hyperplasia, osteochondroma, and congenital deformities.14
Since the TMJs are the foundation of orthognathic surgery, the resultant pathology of TMJ conditions with gross erosive changes in the articulating components of the fossa and condyle resulting in vertical height loss offers a poor base for maxillofacial skeletal and functional reconstruction. Furthermore, the degenerative and osteolytic changes in the joint components due to these conditions make these TMJ components highly susceptible to failure under the new functional loading resulting from orthognathic surgical repositioning of the maxillofacial skeleton.
Maxillomandibular advancement with counterclockwise rotation of the occlusal plane is an established procedure for patients with healthy TMJs. However, patients who had presurgical TMJ symptoms and underwent orthognathic surgery alone had a statistically significant rate of skeletal relapse related to condylar remodeling and resorption. In addition, orthognathic surgery requires surgical invasion, which carries risks and can cause postoperative discomfort. Therefore, orthognathic surgery is not recommended for patients with progressive mandibular retrusion associated with TMJ-OA. In the present case, the patient had an anterior open bite with a retropositioned mandible caused by severe condylar resorption and deformity, indicative of TMJ-OA. Therefore, conservative treatment was planned to acquire a positive overbite.
Morphologic collapse of the joint component by TMJ-OA induces a decrease in ramus height, leading to clockwise rotation of the mandible and an anterior open bite. These characteristics appear to cause TMJ overloading. The results of finite element model analysis showed that an open bite can induce greater TMJ stress than normal occlusion.15 Furthermore, clockwise rotation of the mandible, which is a major character of skeletal anterior open bite, leads to a synergistic increase in TMJ stress during clenching.15 This suggests that improvement of mandibular clockwise rotation, which results in the reduction of TMJ overloading, may be indispensable for treatment of acquired open bite associated with TMJ-OA. However, it is nearly impossible to provide skeletal improvement in patients with anterior open bites using traditional orthodontics.
Several recent studies have demonstrated effective treatment of anterior open bite patients with Class I or II jaw relationships using temporary anchorage devices (TADs), which has now been established as a new treatment strategy.10,16-19 Absolute molar intrusion, which was previously impossible with traditional orthodontic mechanics, using TADs results in counterclockwise rotation of the mandible, and the reduced overbite is increased without incisal elongation. Kuroda et al.10,17,18 reported that although the mandibular plane was rotated more than 5° by molar intrusion, the patients had no functional problems after treatment. In addition, the procedure is definitely less invasive than a Le Fort I osteotomy for maxillary impaction with a mandibular repositioning osteotomy, and provides superior morphologic improvement over orthognathic surgery.18 Therefore, absolute anchorage with TADs was used in the present case.
Superimposition of the cephalometric tracings before and after treatment showed counterclockwise rotation of the mandible due to upper molar intrusion. Because of this mandibular rotation, the mandibular plane angle was decreased by 2.3°. The mandibular condyles also exhibited rotational repositioning in the inferior direction. Consequently, due to increases in the anterior and superior areas, the joint space became nearly uniform. It would be reasonable to assume that these changes in condylar position, if accomplished with optimal occlusal support, may lead to biomechanical equilibrium in the TMJ. When TMJ-OA is progressing, the condyle deformity is more prominent with a shorter ramus height. Although TMJ-OA often has an unpredictable course, optimal condylar position and stable occlusion can achieve biomechanical equilibrium in the TMJ, and this may inhibit progression of TMJ-OA, and occasionally lead to functional and adaptive remodeling of the condyles through resorption repair.20 In the current case, there was no recurrence of TMJ symptoms during the orthodontic treatment. Although anterior disc displacement without reduction and condylar resorption and deformity persisted after treatment, all symptoms of TMJ disease disappeared, and long-term stability of both the occlusal and symptomatic states was obtained.
CONCLUSION
Growing evidence suggests that in TMJ-OA, similar to OA in other joints, overloading may initiate a series of degenerative changes, such as condylar resorption, decreased mandibular ramus height, mandibular clockwise rotation, progressive mandibular retrusion, and an anterior open bite. To date, many treatment modalities for TMJ-OA have been reported; however, the treatment outcomes depend on the preoperative TMJ conditions. Therefore, understanding the pathogenesis of TMJ-OA and its current clinical treatment is essential for developing a "good as new" treatment for TMJ-OA, including the orthodontic approach. We showed here that orthodontic correction through molar intrusion using titanium miniscrews was effective for the management of an open bite and clockwise-rotated mandible associated with TMJ-OA and jaw deformity.
Footnotes
The authors report no commercial, proprietary, or financial interest in the products or companies described in this article.
References
- 1.Tanaka E, Detamore MS, Mercuri LG. Degenerative disorders of the temporomandibular joint: etiology, diagnosis, and treatment. J Dent Res. 2008;87:296–307. doi: 10.1177/154405910808700406. [DOI] [PubMed] [Google Scholar]
- 2.Arnett GW, Milam SB, Gottesman L. Progressive mandibular retrusion-idiopathic condylar resorption. Part II. Am J Orthod Dentofacial Orthop. 1996;110:117–127. doi: 10.1016/s0889-5406(96)70099-9. [DOI] [PubMed] [Google Scholar]
- 3.Nitzan DW. The process of lubrication impairment and its involvement in temporomandibular joint disc displacement: a theoretical concept. J Oral Maxillofac Surg. 2001;59:36–45. doi: 10.1053/joms.2001.19278. [DOI] [PubMed] [Google Scholar]
- 4.Laskin D. Etiology and pathogenesis of internal derangement of the temporomandibular joint (Current controversies in surgery for internal derangements of the temporomandibular joint) Oral Maxillofac Surg Clin North Am. 1994;6:217–222. [Google Scholar]
- 5.Kuroda S, Tanimoto K, Izawa T, Fujihara S, Koolstra JH, Tanaka E. Biomechanical and biochemical characteristics of the mandibular condylar cartilage. Osteoarthritis Cartilage. 2009;17:1408–1415. doi: 10.1016/j.joca.2009.04.025. [DOI] [PubMed] [Google Scholar]
- 6.De Clercq CA, Neyt LF, Mommaerts MY, Abeloos JV, De Mot BM. Condylar resorption in orthognathic surgery: a retrospective study. Int J Adult Orthodon Orthognath Surg. 1994;9:233–240. [PubMed] [Google Scholar]
- 7.Crawford JG, Stoelinga PJ, Blijdorp PA, Brouns JJ. Stability after reoperation for progressive condylar resorption after orthognathic surgery: report of seven cases. J Oral Maxillofac Surg. 1994;52:460–466. doi: 10.1016/0278-2391(94)90341-7. [DOI] [PubMed] [Google Scholar]
- 8.Wolford LM, Reiche-Fischel O, Mehra P. Changes in temporomandibular joint dysfunction after orthognathic surgery. J Oral Maxillofac Surg. 2003;61:655–660. doi: 10.1053/joms.2003.50131. [DOI] [PubMed] [Google Scholar]
- 9.Gonçalves JR, Cassano DS, Wolford LM, Santos-Pinto A, Márquez IM. Postsurgical stability of counterclockwise maxillomandibular advancement surgery: affect of articular disc repositioning. J Oral Maxillofac Surg. 2008;66:724–738. doi: 10.1016/j.joms.2007.11.007. [DOI] [PubMed] [Google Scholar]
- 10.Kuroda S, Katayama A, Takano-Yamamoto T. Severe anterior open-bite case treated using titanium screw anchorage. Angle Orthod. 2004;74:558–567. doi: 10.1043/0003-3219(2004)074<0558:SAOCTU>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 11.Wada K, Otani S, Sakuda M. Morphometric analysis in maxillary protrusion. In: Yamauchi K, Sakuda M, editors. Maxillary Protrusion. Tokyo: Ishiyaku; 1989. pp. 95–130. [in Japanese] [Google Scholar]
- 12.Magnusson T, Ahlborg G, Svartz K. Function of the masticatory system in 20 patients with mandibular hypo- or hyperplasia after correction by a sagittal split osteotomy. Int J Oral Maxillofac Surg. 1990;19:289–293. doi: 10.1016/s0901-5027(05)80423-0. [DOI] [PubMed] [Google Scholar]
- 13.Moore KE, Gooris PJ, Stoelinga PJ. The contributing role of condylar resorption to skeletal relapse following mandibular advancement surgery: report of five cases. J Oral Maxillofac Surg. 1991;49:448–460. doi: 10.1016/0278-2391(91)90166-j. [DOI] [PubMed] [Google Scholar]
- 14.Wolford LM, Cottrell DA, Henry CH. Temporomandibular joint reconstruction of the complex patient with the Techmedica custom-made total joint prosthesis. J Oral Maxillofac Surg. 1994;52:2–10. doi: 10.1016/0278-2391(94)90003-5. [DOI] [PubMed] [Google Scholar]
- 15.Tanaka E, Tanaka M, Watanabe M, Del Pozo R, Tanne K. Influences of occlusal and skeletal discrepancies on biomechanical environment in the TMJ during maximum clenching: an analytic approach with the finite element method. J Oral Rehabil. 2001;28:888–894. doi: 10.1046/j.1365-2842.2001.00763.x. [DOI] [PubMed] [Google Scholar]
- 16.Umemori M, Sugawara J, Mitani H, Nagasaka H, Kawamura H. Skeletal anchorage system for open-bite correction. Am J Orthod Dentofacial Orthop. 1999;115:166–174. doi: 10.1016/S0889-5406(99)70345-8. [DOI] [PubMed] [Google Scholar]
- 17.Kuroda S, Sugawara Y, Tamamura N, Takano-Yamamoto T. Anterior open bite with temporomandibular disorder treated with titanium screw anchorage: evaluation of morphological and functional improvement. Am J Orthod Dentofacial Orthop. 2007;131:550–560. doi: 10.1016/j.ajodo.2006.12.001. [DOI] [PubMed] [Google Scholar]
- 18.Kuroda S, Sakai Y, Tamamura N, Deguchi T, Takano-Yamamoto T. Treatment of severe anterior open bite with skeletal anchorage in adults: comparison with orthognathic surgery outcomes. Am J Orthod Dentofacial Orthop. 2007;132:599–605. doi: 10.1016/j.ajodo.2005.11.046. [DOI] [PubMed] [Google Scholar]
- 19.Kuroda S, Tanaka E. Application of temporary anchorage devices for the treatment of adult Class III malocclusions. Semin Orthod. 2011;17:91–97. [Google Scholar]
- 20.Tanaka E, Kikuchi K, Sasaki A, Tanne K. An adult case of TMJ osteoarthrosis treated with splint therapy and the subsequent orthodontic occlusal reconstruction: adaptive change of the condyle during the treatment. Am J Orthod Dentofacial Orthop. 2000;118:566–571. doi: 10.1067/mod.2000.93966. [DOI] [PubMed] [Google Scholar]