Abstract
Introduction:
Intermittent smokers (ITS) are an increasingly prevalent segment of smokers, yet it is unknown whether or how dependence severity may vary across ITS.
Methods:
Participants were 217 ITS (70 never daily ITS [NITS], 138 converted ITS [CITS], and 9 unknown), who smoked 4–27 days per month, and 197 daily smokers (DS), recruited for a study on smoking patterns. Participants completed questionnaires on dependence (time to first cigarette after waking, Fagerström Test of Nicotine Dependence [FTND], Nicotine Dependence Syndrome Scale [NDSS], Wisconsin Inventory of Smoking Dependence Motives [WISDM], and Hooked on Nicotine Checklist [HONC]) and recorded each cigarette in real time over 3 weeks using Ecological Momentary Assessment. Logistic regression assessed differences in dependence between groups (DS vs. ITS; CITS vs. NITS), and least squares regression examined associations between dependence and smoking behavior (mean, maximum cigarettes per day; proportion of days smoked; longest period of abstinence) within ITS.
Results:
As expected, DS were significantly more dependent than ITS: FTND, NDSS, and WISDM discriminated between ITS and DS with greater than 90% accuracy. Similarly, among ITS, NITS demonstrated lower dependence than CITS. Within ITS, dependence measures also correlated with observed smoking rate and duration of abstinence.
Conclusions:
The study confirmed that DS are more dependent than ITS and that CITS are more dependent than NITS. Importantly, ITS exhibit features of dependence, and there is meaningful variation in dependence within ITS, suggesting that some aspects of dependence may appear with very infrequent smoking. Future work should examine implications for ITS’ potential progression to daily smoking and cessation outcome.
Introduction
Nicotine dependence is often viewed as the primary determinant of cigarette smoking, with individuals smoking frequently throughout the day in order to maintain nicotine levels above a certain point, thereby staving off withdrawal symptoms (Benowitz, 2010; Stolerman & Jarvis, 1995). Maintaining systemic nicotine levels in this manner requires frequent regular smoking to counteract the rapid clearance of nicotine (within 2–3 hr; Benowitz, 2008). Such nicotine maintenance has been regarded as a hallmark of nicotine dependence and helps explain “typical” smoking, which is daily and frequent. Indeed, it has been proposed that regulators could eliminate the addictive potential of smoking and possibly eliminate smoking, if nicotine delivery could be dropped below the levels apparently necessary to maintain dependence (Benowitz & Henningfield, 1994).
While the nicotine regulation model helps explain the behavior of daily smokers (DS), this model seems less suitable for explaining the behavior of nondaily or intermittent smokers (ITS). By current estimates, a quarter to a third of adult smokers in United States are ITS (Centers for Disease Control and Prevention [CDC], 2008a, 2008b; Substance Abuse and Mental Health Services Administration [SAMHSA], 2009; though see Hassmiller, Warner, Mendez, Levy, & Romano, 2003; Wortley, Husten, Trosclair, & Chrismon, 2003). The prevalence of ITS has increased substantially in recent years (e.g., CDC, 2003; though see CDC, 2007), perhaps partly due to increasingly stringent tobacco-control measures (Shiffman, 2009b). Similar patterns are evident in Europe (Korhonen, Broms, Levalahti, Koskenvuo, & Kaprio, 2009; Lindstrom & Ostergren, 2001) and elsewhere (e.g., Asia, Latin America; World Health Organization [WHO], 2007).
We currently know little about ITS smoking behavior and dependence. In a recent study (Shiffman, Tindle, et al., 2012), ITS reported abstaining on over one-third of days and abstaining for periods of approximately five consecutive days, on average, with some reporting abstaining for 10 or more consecutive days during a 2-month period. On the days that they did smoke, ITS consumed approximately 4–5 cigarettes/day. These data suggest that ITS are less dependent than DS. This is consistent with findings from prior studies on ITS (Gilpin, Cavin, & Pierce, 1997; Hennrikus, Jeffery, & Lando, 1996) and on chippers—light smokers, most of whom smoke daily (Shiffman & Sayette, 2005).
If maintaining nicotine levels above a certain threshold—or indeed, at any level above zero—is essential to dependence, then ITS may not show any dependence at all, as they are unable to maintain nicotine levels above zero while skipping days of smoking. On the other hand, DiFranza and Wellman (2005) have argued that dependence is often evident in novice smokers, does not require nicotine maintenance, and can be seen even after smoking just a single cigarette (DiFranza et al., 2000; Scragg, Laugesen, Wellman, & DiFranza, 2000). Importantly, ITS apparently find it difficult to quit. In a national survey, Tindle & Shiffman (2011) found that many ITS had made attempts to quit smoking (more so than DS; also see Shiffman, Tindle, et al., 2012) but had very poor success rates: only about 20% of ITS who made quit efforts were abstinent for 90 days at the time of the survey. Further, one in eight ITS used medication in their quit attempt; given that medication use is not common (Shiffman, Brockwell, Pillitteri, & Gitchell, 2008), and tends to be adopted by more dependent smokers (Shiffman, Brockwell, et al., 2008), who anticipate greater difficulty quitting, this also suggests that ITS have difficulty quitting. (Cooper et al., 2010, report higher quit rates among young Air Force recruits, but this was after 6 weeks’ enforced abstinence, and included smokers who were not interested in quitting. But, see also Kotz, Fidler, & West, 2011). Together, these findings suggest that ITS may demonstrate dependence after all. The purpose of this analysis is to assess dependence in ITS, examining both comparisons to DS, and variation within ITS.
Assessing dependence is complex, and no one measure is accepted as the gold standard. The different measures are not always highly correlated (Baker et al., 2007; Courvoisier & Etter, 2008; Piper, McCarthy, et al., 2008), so may be tapping different aspects of dependence, and may also differ in their sensitivity at different degrees of dependence, with some being more sensitive at low levels of dependence, such as those found early in smoking careers, or perhaps among adult ITS (Carpenter, Baker, Gray, & Upadhyaya, 2010; Etter, Vu Duc, & Perneger, 1999; MacPherson, Strong, & Myers, 2008; Wellman, Savagneau, et al., 2006). Accordingly, our analysis incorporates multiple measures of nicotine dependence.
An important question is whether dependence is a discrete, dichotomous state that is either present or absent, or a continuum that can vary quantitatively. Psychiatric diagnosis treats all disorders as dichotomous (American Psychiatric Association [APA], 2000) and has been criticized for ignoring intermediate variations (Andersson & Ghaderi, 2006; Baker, Breslau, Covey, & Shiffman, 2012). Similarly, the Hooked on Nicotine Checklist (HONC; DiFranza et al., 2002) is typically scored dichotomously, considering endorsement of even one symptom as an indication of dependence and has similarly been criticized for classifying almost all smokers (and even some nonsmokers; Dar & Frenk, 2010; Hughes & Shiffman, 2008) as dependent. However, scored continuously, it can be sensitive to differences in loss of autonomy over smoking, even among low-rate smokers (Wellman et al., 2005). In a taxometric analysis to assess whether tobacco dependence is best construed as a continuum or as a distinct and dichotomous category, Goedeker and Tiffany (2008) reported ambiguous findings: dependence behaved more like a dichotomy, with non-DS representing a discrete group without dependence, rather than part of a continuum of dependence. However, there was also some residual variance not captured by the dichotomy, suggesting some mix of discrete and continuous properties of dependence. It is therefore of interest to assess whether there is meaningful variation in dependence among ITS.
Accordingly, a second aim of this paper is to examine variability in dependence among ITS. Some variability may be due to the fact that some ITS have previously smoked daily (Nguyen & Zhu, 2009). Those with a history of daily smoking (“converted” ITS or CITS) might still demonstrate more signs of residual dependence, despite their change in smoking behavior. Thus, we assess differences in dependence between CITS and “native” ITS (NITS).
However, merely observing differences in dependence scores might not be sufficient to demonstrate true variability in dependence among ITS: The observed variability could be spurious statistical noise. Therefore, we also evaluate whether the variability in assessed dependence was meaningfully related to relevant behaviors. It has been argued (Baker et al., 2007; Perkins, 2009) that the most meaningful indicator of dependence is the (in)ability to abstain from smoking. Indeed, ITS are of interest precisely because they seem to routinely engage in voluntary abstinence. Thus, we examined whether variations in ITS’ assessed dependence could predict how often ITS abstained (percent of days not smoking) and how long they voluntarily abstain (longest “run” of abstinence). Another key behavioral indicator of dependence is heaviness of use (Baker et al., 2012); accordingly, we also assessed ITS’ typical and heaviest cigarette consumption on days that they smoked. For these assessments of smoking behavior, we relied primarily on Ecological Momentary Assessment (EMA; Shiffman, Stone, & Hufford, 2008; Stone & Shiffman, 1994), which avoids recall and global impressions in favor of collecting real-time data, recorded in real-world environments, and has been shown to be superior to other methods of assessing smoking (Shiffman, 2009a).
In summary, we sought first to confirm that ITS would be less dependent than DS on multiple dependence measures. Next, we assessed whether there were meaningful variations in dependence among ITS, as demonstrated by variations in dependence measures associated with relevant behaviors such as smoking rate and longest duration of abstinence.
Methods
Participants
Participants were 217 ITS (138 CITS, 70 NITS, and nine unknown) and 197 DS recruited for this study via advertisement and promotion. The sample largely overlaps with that reported in Shiffman, Tindle, et al. (2012). To be eligible, volunteers had to be at least 21-years-old, report smoking for 3 years or greater, smoking at their current rate for 3 months or greater, and not be planning to quit within the next month. DS had to report smoking every day, averaging 5–30 cigarettes/day (CPD), while ITS had to report smoking 4–27 days/month, with no restrictions on number of cigarettes. We oversampled Black smokers because national surveys indicate they are more likely to be ITS. This was rebalanced in analysis by weighting by race.
ITS averaged 35.05 (SD = 12.22) years old and DS averaged 39.92 (SD = 11.82). DS had smoked for an average of 25.38 years (SD = 11.75), while ITS had smoked for an average of 18.66 years (12.79); among CITS, this was 20.51 [12.76] years but 15.26 [12.15] years for NITS. Slightly over half of subjects were male (50.90% ITS and 58.87% DS). Black subjects constituted 32.85% of the sample (29.95% ITS and 36.04% DS), with 61.35% Caucasian (63.59% ITS & 58.88% DS), and a small representation of other ethnicities (0.97% Asian, 0.72% Hispanic, and 4.11% other). Most had at least some post-high school education (85.53% of ITS and 62.66% of DS).
Procedure
Participants attended up to six laboratory sessions to assess cue reactivity (data not reported here; Shiffman, Dunbar, et al., in press) prior to monitoring their ad lib smoking using EMA for 3 weeks. Retrospective reports of CPD were collected at each visit using time line follow-back (TLFB; Sobell, Sobell, & Maisto, 1979) methods. A questionnaire battery was completed over the first 2 weeks of the study.
Assessments
Nicotine Dependence Measures
Participants completed various nicotine dependence questionnaires, including the six-item Fagerstrom Test of Nicotine Dependence (FTND) (Heatherton, Kozlowski, Frecker, & Fagerström, 1991). (The FTND includes a measure of CPD in its scoring, which leads to circularity when correlating FTND with measures of cigarette consumption. For this reason, we also created an FTND score that omitted consideration of CPD from the score. Mean differences on the FTND have been previously presented in Shiffman, Tindle, et al., 2012 but we present a more complete analysis here). The FTND has modest internal consistency (Cronbach's α = .67; Haddock, Lando, Klesges, Talcott, & Renaud, 1999). Participants also completed the Nicotine Dependence Syndrome Scale (NDSS; Shiffman, Waters, & Hickcox, 2004), a multidimensional scale yielding five subscales, and a summary score (NDSS-T) that has high internal consistency (Cronbach’s α = .86; Shiffman et al., 2004). The NDSS predicts cessation outcome (Shiffman et al., 2004), discriminates between heavy smokers and tobacco chippers, and is sensitive to variations in smoking behavior even in extremely light smokers (Shiffman & Sayette, 2005). The Wisconsin Inventory of Smoking Dependence Motives (WISDM; Piper et al., 2004) is a multidimensional measure of dependence, with subscales tapping 13 motives for smoking. The overall WISDM has strong internal consistency (Cronbach’s α > .96). The scale has been summarized into two factors, reflecting Primary (e.g., automaticity, craving, loss of control, and tolerance) and Secondary (weight management, etc.) dependence motives, with the former being more strongly associated with relapse, withdrawal, and various dependence phenomena (Piper, Bolt, et al., 2008). The HONC (DiFranza et al., 2002) is a checklist of 10 symptoms related to dependence. It correlates with smoking behavior (e.g., CPD, duration of abstinence during quit attempts) among adolescents and adults (DiFranza et al., 2002; Wellman et al., 2005) and is more sensitive to dependence than FTND in very light smokers (Wellman, Savagneau, et al., 2006). The authors of the HONC typically score the HONC dichotomously (DiFranza et al., 2002; Wellman, DiFranza, et al., 2006), considering any endorsement as indicating “loss of autonomy.” Accordingly, we score the HONC as both a dichotomous and continuous (0–10) scale.
Smoking Behavior and History
Participants completed a thorough smoking history interview, using notable life events or changes to help anchor recollections in order to boost recall accuracy (Eisenhower et al., 1991). Based on this detailed interview (but in a few cases based on simpler questioning), we classified as CITS those ITS who had previously smoked daily for 6 months or greater, in contrast to the NITS, who had always smoked nondaily. Those for whom this variable was missing (n = 9) were omitted from analyses comparing NITS and CITS.
EMA Monitoring
A detailed description of EMA monitoring can be found elsewhere (Shiffman et al., 2002; Shiffman & Paty, 2006). Briefly, participants were provided with a palmtop-computer-based electronic diary (ED) running specialized software designed for the study (invivodata, Pittsburgh, PA). Participants engaged in event-oriented (Shiffman, 2009a) monitoring of smoking and were instructed to record each cigarette as they initiated it. To capture smoking that participants failed to record in real time, participants also had two opportunities to enumerate cigarettes they had not recorded in real time—in the evening (9 p.m. to midnight, to capture cigarettes missed since waking) and upon waking (to capture cigarettes missed during the previous night)—in order to achieve a more complete tally. These data were used to capture smoking rates and days of abstinence. Participants were to engage in EMA for 21 days, but the period varied, averaging 22.08 (SD = 6.40) days.
TLFB
At each session, participants retrospectively reported CPD smoked on each day since the date of their previous study visit (though at the first session participants reported on the prior 30 days), using TLFB procedures (Sobell et al., 1979). Participants provided a mean of 69.47 (SD = 11.63) reporting days over the course of the study.
Analysis
EMA-observed Smoking Behavior
CPD reported on ED reflects the sum of all cigarettes reported by the participant each day, including the evening and waking reports. Mean and maximum CPD for smoking days during the ED monitoring period were calculated for each participant. “Abstinent days” were days on which participants reported no cigarettes in both EMA and TLFB reports. Ambiguous days in which EMA and TLFB reports conflicted were treated as smoking days. The proportion of days on which subjects smoked was calculated and arcsine transformed (2 × Arcsine√x; e.g., Cohen, Cohen, West, & Aiken, 2003). The longest run of abstinence (the span of days individuals remained continuously abstinent) was identified.
Parallel measures of smoking behavior were also derived from TLFB, for sensitivity testing. The results were essentially identical, and we therefore report only on EMA-based measures.
Dependence and Smoker Type
Univariate logistic regression was used to test for differences in dependence between groups (i.e., DS vs. ITS, CITS vs. NITS). To quantify the degree to which each dependence measure differentiated smoker type, we calculated the area under the curve for the receiver operating characteristic curve (AUC-ROC). Like an R2 value for least squares regression, higher AUC-ROC values reflect better prediction and are interpreted as the probability of correctly identifying an individual as DS (vs. ITS) based upon dependence score. Thus, AUC-ROC ranges from 0.5 (random guessing) to 1.0 (perfect prediction; Hanley & McNeil, 1982).
Dependence and Smoking Behavior
Within ITS, we assessed the relationship between dependence and smoking behaviors by running separate least square regression models for each dependence measure, examining linear and quadratic effects of smoking behavior on each dependence measure. All analyses controlled for history of daily smoking (CITS or NITS); models that did not control for smoking history yielded virtually identical results.
Results
Differences in Dependence Between ITS and DS
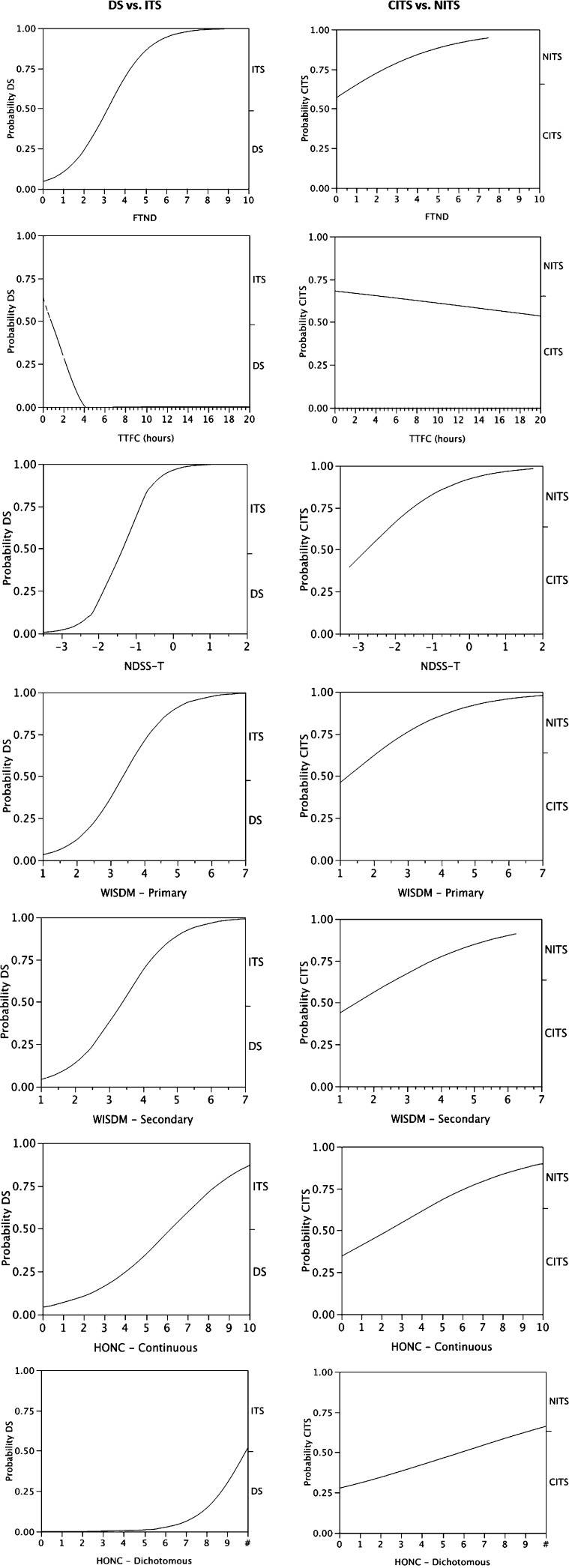
ITS were significantly less dependent than DS on every measure of dependence (Table 1). The differences were very large, as seen in the steep slopes of the logistic functions in Figure 1. Three measures (NDSS, FTND, and WISDM Primary) yielded AUC-ROC values greater than or equal to .90—that is, the measures correctly differentiated ITS from DS more than 90% of the time. When scored dichotomously, the HONC classified all DS and 93% of ITS as dependent, yielding the lowest AUC-ROC value (0.54). However, the continuous HONC achieved an AUC-ROC of 0.81.
Table 1.
Differences in Dependence Between Daily Smokers (DS) and Intermittent Smokers (ITS) and Also Within ITS
| Variable | M (SD) | Range | OR (95% CI) | Receiver operating characteristic curve |
| FTND | ||||
| DS | 5.15 (1.82) | 0–10 | 2.69 (2.29–3.24)*** | 0.93 |
| ITS | 1.42 (1.60) | 0–7 | ref | – |
| CITS | 1.69 (1.78) | 0–7 | 1.42 (1.15–1.79)*** | 0.60 |
| NITS | 0.87 (1.14) | 0–4 | ref | – |
| TTFC | ||||
| DS | 0.33 (0.51) | 0.01–3.33 | 0.21 (0.13–0.30)*** | 0.88 |
| ITS | 3.86 (4.40) | 0–20 | ref | – |
| CITS | 3.55 (4.53) | 0–20 | 0.97 (0.91–1.03) | 0.60 |
| NITS | 4.60 (4.28) | 0–14 | ref | – |
| NDSS-T | ||||
| DS | −0.44(1.00) | −2.71–+1.94 | 11.07 (7.29–17.85)*** | 0.93 |
| ITS | −2.04(0.60) | −3.07–+1.54 | ref | – |
| CITS | −1.92(0.70) | −3.07–+1.54 | 2.42 (1.41–4.38)*** | 0.61 |
| NITS | −2.21(0.44) | −2.96–−1.18 | ref | – |
| WISDM primary | ||||
| DS | 4.49 (1.19) | 1.59–6.90 | 4.18 (3.32–5.42)*** | 0.92 |
| ITS | 2.31 (1.10) | 1–6.50 | ref | – |
| CITS | 2.56 (1.21) | 1–6.50 | 1.93 (1.40–2.79)*** | 0.66 |
| NITS | 1.91 (0.78) | 1–4.38 | ref | – |
| WISDM secondary | ||||
| DS | 4.00 (1.06) | 1.18–6.78 | 3.69 (2.88–4.85)*** | 0.83 |
| ITS | 2.75 (0.90) | 1.07–6.00 | ref | – |
| CITS | 2.90 (0.98) | 1.07–6.00 | 1.63 (1.17–2.34)** | 0.61 |
| NITS | 2.50 (0.76) | 1.17–4.66 | ref | – |
| HONC continuous | ||||
| DS | 7.36 (2.19) | 1–10 | 1.65 (1.48–1.87)*** | 0.81 |
| ITS | 4.63 (2.70) | 0–10 | ref | – |
| CITS | 5.30 (2.66) | 0–10 | 1.33 (1.16–1.55)*** | 0.70 |
| NITS | 3.38 (2.39) | 0–8 | ref | – |
| HONC dichotomous | ||||
| DS | 10 (0.00) | 10–10 | p < .001a | 0.54 |
| ITS | 9.32 (2.50) | 0–10 | ref | – |
| CITS | 9.70 (1.71) | 0–10 | 1.18 (1.04-1.38) * | 0.56 |
| NITS | 8.68 (3.42) | 0–10 | ref | – |
Note. All models weighted by race. Daily smokers (DS) versus intermittent smokers (ITS) comparisons controlled for history of daily smoking (converted ITS [CITS] vs. native ITS [NITS]) among ITS. M = mean; FTND = Fagerström Test for Nicotine Dependence; TTFC = time to first cigarette (hr); NDSS = Nicotine Dependence Syndrome Scale; WISDM = Wisconsin Inventory of Smoking Dependence Motives; HONC = Hooked on Nicotine Checklist; ref = reference group.
*p < .05. **p < .01. ***p < .001.
An OR could not be computed, because all DS were classified as dependent.
Figure 1.
Differences in dependence measures Fagerström Test for Nicotine Dependence (FTND), time to first cigarette (TTFC), Nicotine Dependence Syndrome Scale (NDSS), Wisconsin Inventory of Smoking Dependence Motives (WISDM) Primary, WISDM Secondary, Hooked on Nicotine Checklist (HONC) Continuous, and HONC Dichotomous contrasting daily smokers (DS) and intermittent smokers (ITS; left column) and converted ITS (CITS) and native ITS (NITS; right column). The figures show logistic curves indicating (on the left y-axis) the projected probability of being a DS or CITS, respectively, as the x-axis score increases. (Note reverse relationship for TTFC, since higher values of TTFC are associated with reduced dependence.) Steeper curves indicate a stronger relationship. Relatively flat regions at the right and left of S-shaped curves indicate regions where the x-axis variable is completely discriminating, that is, group membership is uniform. Right y-axis shows groups being compared with tick mark indicating the proportion of subjects in each group.
On every measure except TTFC, CITS were more dependent than NITS but the effects were more modest, with AUC-ROC values in the .60–.70 range (Table 1) and as illustrated by the less-steep curves in Figure 1. The HONC classified 87% of NITS and 97% of CITS as dependent, yielding a modest AUC-ROC of 0.56, but was the most discriminating measure (AUC-ROC = 0.70) when scored continuously.
Relationship Between Dependence Measures and Smoking Behavior Among ITS
All the dependence measures showed some variation within ITS (Table 1). Continuous HONC scores spanned the entire range of the scale, and WISDM scores nearly did so as well. TTFC ranged from 0 min (smoking immediately upon waking) to 20 hr. When ITS’ NDSS scores are considered as z-scores and evaluated as percentiles against the published normative sample (Shiffman et al., 2004), ITS’ scores ranged from the 0.1th to the 94th percentile.
There was also substantial variation in ITS smoking behavior as recorded in EMA. Mean CPD (on days smoked) averaged 3.48 (SD = 2.36) cigarettes, but ranged from 1 to 17.5 CPD. The maximum CPD averaged 7.69 (SD = 5.61), ranging from 1 to 32 CPD. These two metrics were highly correlated, r = .86. The proportion of days smoked averaged 0.75 (SD = 0.26), ranging from 0.05 to 1. The longest run of abstinence averaged 2.48 (SD = 3.27) days, but ranged from 0 to 23 days. These two measures correlated r = −.84 and they correlated with mean CPD r = −.38 and .43, respectively.
Importantly, ITS with higher dependence scores also demonstrated greater dependence on the more behavioral EMA smoking measures, even when variation attributable to the NITS–CITS differences was factored out (see Table 2). ITS who smoked more heavily (on average and at maximum) also scored higher in dependence measures. Only the dichotomous HONC failed to detect variation related to cigarette consumption. The WISDM Primary Dependence measure was most strongly related to cigarette consumption. The relationship to cigarette consumption was not entirely linear for FTND and TTFC: for FTND, CPD was flat as FTND rose from 0 to 1 and then increased thereafter; for TTFC, the relationship was steep at first but the curve flattened out after TTFC exceeded 5 hr.
Table 2.
Relationship Between Measures of Dependence and Observed Smoking Behaviors Among Intermittent Smokers (ITS)
| Variable | Mean CPD | Max CPD | Max run | Proportion of days smoked | ||||
| β | p | β | p | β | p | β | p | |
| FTND | ||||||||
| Linear | 0.45 | <.0001 | 0.39 | <.0001 | −0.26 | <.0003 | 0.43 | <.0001 |
| Quadratic | 0.24 | <.02 | 0.17 | NS | 0.04 | NS | −0.14 | NS |
| TTFC | ||||||||
| Linear | −0.26 | <.0004 | −0.21 | <.003 | 0.33 | <.0001 | −0.51 | <.0001 |
| Quadratic | 0.29 | <.007 | 0.26 | <.02 | −0.12 | NS | 0.19 | <.05 |
| NDSS-T | ||||||||
| Linear | 0.44 | <.0001 | 0.37 | <.0001 | −0.34 | <.0001 | 0.46 | <.0001 |
| Quadratic | 0.12 | NS | 0.10 | NS | 0.18 | <.04 | −0.24 | <.003 |
| WISDM primary | ||||||||
| Linear | 0.53 | <.0001 | 0.51 | <.0001 | −0.41 | <.0001 | 0.53 | <.0001 |
| Quadratic | −0.07 | NS | 0.00 | NS | 0.22 | <.02 | −0.25 | <.004 |
| WISDM secondary | ||||||||
| Linear | 0.26 | <.0003 | 0.28 | <.0001 | −0.25 | <.0004 | 0.33 | <.0001 |
| Quadratic | −0.01 | NS | 0.00 | NS | 0.12 | NS | −0.13 | NS |
| HONC continuous | ||||||||
| Linear | 0.30 | <.0003 | 0.27 | <.0008 | −0.13 | NS | 0.31 | <.0002 |
| Quadratic | 0.01 | NS | −0.02 | NS | 0.08 | NS | −0.11 | NS |
| HONC- dichotomous | ||||||||
| Lineara | 0.15 | NS | 0.17 | <.04 | −0.16 | <.05 | 0.24 | <.003 |
Note. All models were weighted by race and controlled for history of daily smoking. CPD = cigarettes per day; β = standardized regression coefficient; FTND = Fagerström Test for Nicotine Dependence, modified to exclude CPD item when used in CPD models; TTFC = time to first cigarette (hr); NDSS = Nicotine Dependence Syndrome Scale; WISDM = Wisconsin Inventory of Smoking Dependence Motives; HONC = Hooked on Nicotine Checklist; NS = nonsignificant.
Only linear (not quadratic) relations are possible with a dichotomy.
ITS who had higher dependence scores (all measures) also smoked on a greater proportion of days (Table 2). These relationships were not entirely linear: For several dependence measures, the proportion of days smoked initially rose steeply and then tended to flatten at higher levels of dependence. ITS with higher dependence scores—with the exception of the HONC (whether continuous or dichotomous)—also had longer runs of voluntary abstinence. For NDSS and WISDM Primary Dependence scores, there was evidence of nonlinear effects due to flattening at higher ranges.
Discussion
As expected, we observed very large differences in dependence between DS and ITS. This confirms the expectation that smokers who regularly abstain voluntarily and do not smoke often enough to regulate nicotine levels would evidence much less of the behaviors indicative of dependence. On most measures, the differences were very large, with analyses indicating that one could easily differentiate ITS from DS based on their dependence scores alone, without knowing anything else about them. While this might seem to imply that dependence is absent in ITS, we in fact observed meaningful variations in dependence among ITS and these were systematically related to how much ITS smoked and how often and for how long they voluntarily abstained. Thus, we conclude that ITS do evidence some behaviors associated with dependence, albeit at very low levels of intensity.
That ITS are less dependent than DS is no surprise—and validates a strong a priori expectation. Even so, the magnitude of the differences is striking: For example, just knowing a smoker’s NDSS score enables one to predict with 93% certainty whether that smoker is an ITS or DS. Clearly, ITS represent extremely low-dependence smokers. Nevertheless, there were variations in dependence even with ITS, who do not seem to fit the traditional nicotine regulation model of dependence. We observed statistical variation in every measure of dependence we examined, suggesting that ITS do represent a range of dependence, albeit at the low end of the spectrum. Moreover, the observed variation in psychometric scales consistently correlated with dependence-relevant behavioral measures. Among ITS, greater dependence was associated with abstaining less often, abstaining for shorter periods, and consuming more cigarettes on smoking days. Thus, we conclude that even ITS may demonstrate some level of dependence and that dependence influences their smoking behavior. Moreover, these variations in dependence were not strictly a function of past daily smoking. Even when this was accounted for, assessed dependence still predicted greater cigarette consumption and less abstinence.
These findings are partly compatible with the mixed conclusions drawn from taxometric analyses of nicotine dependence by Goedeker and Tiffany (2008). On the one hand, nicotine dependence appeared to be a “taxon”—a discrete distinction between dependent and nondependent smokers with the latter marked by nondaily smoking. On the other hand, there appeared to be some remaining continuous variance in dependence within those discrete groups.
Variations in dependence observed among ITS may suggest that some ITS are on a trajectory toward greater dependence, however slowly. Zhu, Sun, Hawkins, Pierce, and Cummins (2003) found that 13% of ITS converted to DS over a 2-year period. Longitudinal data on ITS could assess whether those with some modicum of dependence at baseline are more likely to progress toward daily smoking. In this sense, ITS may mirror the dynamic seen in teen smoking initiates, where those with some early signs of dependence are more likely to progress in both cigarette consumption and dependence (Sterling et al., 2009).
The observed variations in dependence may also partly explain the low success rates ITS show when quitting; perhaps even these slight elevations in dependence interfere with some ITS’ ability to quit. This does not seem like a complete explanation, however. For one thing, CITS, who show slightly higher dependence, actually have higher quit rates (Tindle & Shiffman, 2011). For another, the very low intensity and prevalence of dependence does not seem enough to account for ITS’ 79% failure rate. Particularly, given that ITS score much lower than DS on the FTND and that, indeed, almost half of ITS show no signs of dependence whatsoever, scoring 0 on the FTND (Shiffman, Tindle, et al., 2012), it seems more likely that ITS smoking and difficulty quitting are maintained by other factors. We usually consider smoking to be maintained primarily by nicotine maintenance and negative reinforcement—the need to avoid craving and withdrawal when nicotine levels drop—and this concept was embedded in all the instruments we used to assess dependence. Thus, the assessments mostly show that ITS are not “trough maintainers,” in terminology of Russell (1971)—smokers motivated to avoid withdrawal by keeping nicotine levels above a certain minimal (“trough”) level. However, Russell (1971) also posited that some smokers might be “peak seekers,” who are motivated by the immediate acute effects of nicotine and thus would not have to smoke constantly. Perhaps peak seeking better explains ITS smoking, though it is not known what pharmacological effects ITS seek or achieve when they smoke. Another factor that may help maintain ITS smoking in the absence of traditionally construed dependence based on trough maintenance is stimulus control of smoking. In analyses of chippers—very low-level smokers—we found that their smoking was under considerable stimulus control, tending to occur only in some settings but not others (Shiffman & Paty, 2006). The same might be true of ITS. If so, these tight stimulus associations, along with acute effects of nicotine, could maintain intermittent smoking and make it hard to quit, in the presence of the triggering stimuli. Such stimulus control may constitute an alternate path to persistent smoking, absent traditional withdrawal-based dependence. It might even be considered an alternative form of dependence.
The fact that ITS show some signs of dependence and have difficulty quitting may need to be considered as nicotine policy is formulated. Whereas it is reasonable to assume that lowering nicotine delivery will undermine dependence that is based on nicotine regulation (Benowitz & Henningfield, 1994), it is less clear what effect it would have on the factors that maintain ITS smoking and make quitting difficult for ITS. In particular, our data do not speak to the role of nicotine in ITS smoking, much less what effects of nicotine may reinforce and maintain ITS smoking and what dose-response function may govern these effects. From a public health point of view, ITS behavior should be of some concern because ITS do suffer ill effects from smoking (Luoto, Uutela, & Puska, 2000); however, their exposure to toxins and their subsequent risk is much less than that of DS, so promoting a shift from daily to nondaily smoking would be a public health benefit.
The data also shed light on different approaches to assessing dependence. All the methods tested for assessing dependence significantly discriminated DS and ITS, and almost all also discriminated NITS and CITS. However, the dichotomous classification based on the HONC was considerably less discriminating, as it regarded all DS as dependent, and also evaluated almost all ITS—both NITS and CITS—as dependent. This is perhaps not surprising, as the HONC seems to emphasize sensitivity over specificity, regarding any single sign of dependence as sufficient to classify a smoker as dependent. In contrast, the other dependence measures consider dependence to vary continuously in severity, making finer discriminations. The fact that neither the dichotomized nor continuous HONC predicted the longest duration of voluntary abstinence may be particularly significant because DiFranza et al. (2011) regard the interval at which smokers need to smoke as a core index of the progression of dependence. This is not a definitive test, as DiFranza et al. (2011) suggest people may sometimes smoke without needing to, but it does suggest the need for a more effective measure. In any case, the continuous HONC seems more sensitive to variations in dependence behaviors among ITS.
As expected, the Primary Dependence scale of the WISDM was more strongly associated with dependence outcomes among ITS than was the Secondary motives scale of the WISDM. Indeed, the Primary Dependence scale of the WISDM consistently showed the numerically strongest relationships to the behavioral indicators of dependence we tested, perhaps, because its length confers greater reliability. The FTND, TTFC, and NDSS measures performed roughly comparably with correlations consistently slightly less than those seen for WISDM Primary and higher than those seen for WISDM Secondary and HONC. Interestingly, for the variables relating to abstinence rather than smoking rate—the proportion of days smoking and the longest run of abstinence—TTFC on its own seem to do as well or better than the entire FTND (which incorporates TTFC), suggesting that the other elements of FTND actually diluted rather than enhanced the information imparted by TTFC.
Like any study, our study suffered some limitations. This was a limited convenience sample from a single region, so may not be fully representative, particularly in its lack of subjects of Asian and Hispanic descent, who have higher rates of ITS (Trinidad et al., 2009). All the data were collected by self-report, albeit some using real-time EMA. However, reports of abstinence were not biochemically verified, and we examined periods of voluntary abstinence, rather than the outcomes of smoking cessation efforts. The study also had considerable strengths. We assessed several measures of dependence and several different dependence-relevant behavioral outcomes. Smoking behavior was assessed by EMA methods, which have been biochemically validated in other studies (Shiffman, 2009a), and demonstrated superior to time-line follow-back methods for assessing day-to-day smoking patterns.
In summary, the study confirmed that DS have much stronger dependence than ITS and that CITS are more dependent than NITS. At the same time, the data showed that there is meaningful variation in dependence among ITS. The implications of this for ITS’ potential progression to daily smoking and for their success at quitting remains to be explored.
Funding
This work was supported by the National Institutes of Health , National Institute on Drug Abuse (R01-DA020742) to SS, the National Science Foundation Graduate Research Fellowship to MSD, the National Cancer Institute (R25-CA057703-15) to MSD, and Cancer Council Tasmania SGF.
Declaration of Interests
None declared.
Acknowledgments
The authors are grateful to Hilary Tindle, Thomas Kirchner, and Deborah Scharf for help launching this study and for input on study design; to Anna Tsivina, Joe Stafura, Rachelle Gish, and Aileen Butera for their work conducting research sessions; to Chantele Mitchell-Miland and Sarah Felter for data management assistance; and to Laura Homonnay-Demilio for editorial assistance.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders, Fourth Edition (DSM-IV-TR) Washington, DC: Author; 2000. doi:10.1176/appi.books.9780890423349.7060. [Google Scholar]
- Andersson G, Ghaderi A. Overview and analysis of the behaviourist criticism of the Diagnostic and Statistical Manual of Mental Disorders (DSM) Clinical Psychologist. 2006;10:67–77. doi:10.1080/13284200600690461. [Google Scholar]
- Baker TB, Breslau N, Covey L, Shiffman S. DSM criteria for tobacco use disorder and tobacco withdrawal: A critique and proposed revisions for DSM-5. Addiction. 2012;102:263–275. doi: 10.1111/j.1360-0443.2011.03657.x. doi:10.1111/j.1360-0443.2011.03657.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker TB, Piper ME, McCarhty DE, Bolt DM, Smith SS, Kim SY, et al. Time to first cigarette in the morning as an index of ability to quit smoking: Implications for nicotine dependence. Nicotine & Tobacco Research. 2007;9(Suppl. 4):S555–S570. doi: 10.1080/14622200701673480. doi:10.1080/14622200701673480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benowitz N. Clinical pharmacology of nicotine: Implications for understanding, preventing, and treating tobacco addiction. Clinical Pharmacology & Therapeutics. 2008;83:531–541. doi: 10.1038/clpt.2008.3. doi:10.1038/clpt.2008.3. [DOI] [PubMed] [Google Scholar]
- Benowitz N. Nicotine addiction. New England Journal of Medicine. 2010;362:2295–2303. doi: 10.1056/NEJMra0809890. doi:10.1056/NEJMra0809890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benowitz N, Henningfield JE. Establishing a nicotine threshold for addiction: The implications for tobacco regulation. New England Journal of Medicine. 1994;331:123–125. doi: 10.1056/NEJM199407143310212. doi:10.1056/NEJM199407143310212. [DOI] [PubMed] [Google Scholar]
- Carpenter M, Baker N, Gray K, Upadhyaya H. Assessment of nicotine dependence among adolescent and young adult smokers: A comparison of measures. Addictive Behaviors. 2010;35:977–982. doi: 10.1016/j.addbeh.2010.06.013. doi:10.1016/j.addbeh.2010.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Prevalence of current cigarette smoking among adults and changes in prevalence of current and some day smoking—United States, 1996–2001. Morbidity & Mortality Weekly Report. 2003;52:303–307. Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5214a2.htm. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Cigarette smoking among adults—United States, 2006. Morbidity & Mortality Weekly Report. 2007;56:1157–1161. Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5644a2.htm. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Behavioral risk factor surveillance system survey data. Atlanta, GA: Author; 2008a. Retrieved from http://www.cdc.gov/chronicdisease/resources/publications/AAG/brfss.htm. [Google Scholar]
- Centers for Disease Control and Prevention. Cigarette smoking among adults—United States, 2007. Morbidity & Mortality Weekly Report. 2008b;57:1221–1226. Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5745a2.htm. [PubMed] [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. 3rd ed. Mahwah, NJ: Lawrence Erlbaum Associates; 2003. [Google Scholar]
- Cooper TV, Taylor T, Murray AA, DeBon MW, Vander Weg MW, et al. Differences between intermittent and light daily smokers in a population of U.S Military recruits. Nicotine & Tobacco Research. 2010;12:465–473. doi: 10.1093/ntr/ntq025. doi:10.1093/ntr/ntq025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courvoisier D, Etter JF. Using item response theory to study the convergent and discriminant validity of three questionnaires measuring cigarette dependence. Psychology of Addictive Behaviors. 2008;22:391–401. doi: 10.1037/0893-164X.22.3.391. doi:10.1037/0893-164X.22.3.391. [DOI] [PubMed] [Google Scholar]
- Dar R, Frenk H. Can one puff really make an adolescent addicted to nicotine? A critical review of the literature. Harm Reduction Journal. 2010;7:28. doi: 10.1186/1477-7517-7-28. doi:10.1186/1477-7517-7-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiFranza JR, Rigotti NA, McNeill AD, Ockene JK, Savageau JA, St Cyr D, et al. Initial symptoms of nicotine dependence in adolescents. Tobacco Control. 2000;9:313–319. doi: 10.1136/tc.9.3.313. doi:10.1136/tc93313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiFranza JR, Savageau JA, Fletcher K, Ockene JK, Rigotti NA, McNeill AD, et al. Measuring the loss of autonomy over nicotine use in adolescents: The Development and Assessment of Nicotine in Youths (DANDY) Study. Archives of Pediatric Adolescent Medicine. 2002;156:397–403. doi: 10.1001/archpedi.156.4.397. Retrieved from http://archpedi.ama-assn.org/cgi/reprint/156/4/397.pdf. [DOI] [PubMed] [Google Scholar]
- DiFranza JR, Wellman RJ. A sensation-homeostasis model of nicotine craving, withdrawal, and tolerance: Integrating the clinical and basic science literature. Nicotine & Tobacco Research. 2005;7:9–26. doi: 10.1080/14622200412331328538. doi:10.1080/14622200412331328538. [DOI] [PubMed] [Google Scholar]
- DiFranza JR, Wellman RJ, Mermelstein R, Pbert L, Klein JD, Sargent JD, et al. The natural history and diagnosis of nicotine addiction. Current Reviews in Pediatrics. 2011;72:88–96. Retrieved from http://escholarship.umassmed.edu/prevbeh_pp/150/ [Google Scholar]
- Eisenhower D, Mathiowetz NA, Morganstein D, Biemer PP, Groves RM, Lyberg LE, et al. Recall error: Sources and bias reduction techniques Measurement errors in surveys. New York, NY: Wiley; 1991. pp. 127–144. doi:10.1002/9781118150382.ch8. [Google Scholar]
- Etter JF, Vu Duc T, Perneger TV. Validity of the Fagerstrom test for nicotine dependence and the heaviness of smoking index among relatively light smokers. Addiction. 1999;94:269–281. doi: 10.1046/j.1360-0443.1999.94226910.x. doi:10.1046/j.1360-0443.1999.94226910.x. [DOI] [PubMed] [Google Scholar]
- Gilpin E, Cavin S, Pierce J. Adult smokers who do not smoke daily. Addiction. 1997;92:473–480. doi:10.1111/j.1360-0443.1997.tb03379.x. [PubMed] [Google Scholar]
- Goedeker KC, Tiffany ST. On the nature of nicotine addiction: A taxometric analysis. Journal of Abnormal Psychology. 2008;117:896–909. doi: 10.1037/a0013296. doi:10.1037/a0013296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haddock CK, Lando H, Klesges RC, Talcott GW, Renaud EA. A study of the psychometric and predictive properties of the Fagerström Test for Nicotine Dependence in a population of young smokers. Nicotine & Tobacco Research. 1999;1:59–64. doi: 10.1080/14622299050011161. doi:10.1080/14622299050011161. [DOI] [PubMed] [Google Scholar]
- Hanley JA, McNeil BJ. The meaning and use of the area under a receiving operating characteristic (ROC) curve. Radiology. 1982;143:29–36. doi: 10.1148/radiology.143.1.7063747. Retrieved from http://radiology.rsna.org/search?fulltext=the+meaning+and+use+of+an+area+under+a+receiving+operating+characteristic&submit=yes&x=13&y=9. [DOI] [PubMed] [Google Scholar]
- Hassmiller KM, Warner KE, Mendez D, Levy DT, Romano E. Nondaily smokers: Who are they? American Journal of Public Health. 2003;93:1321–1327. doi: 10.2105/ajph.93.8.1321. doi:10.2105/AJPH.93.8.1321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerström K.-O. The Fagerström Test for Nicotine Dependence: A revision of the Fagerström Tolerance Questionnaire. British Journal of Addiction. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. doi:10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Hennrikus DJ, Jeffery RW, Lando HA. Occasional smoking in a Minnesota working population. American Journal of Public Health. 1996;86:1260–1266. doi: 10.2105/ajph.86.9.1260. doi:10.2105/AJPH.86.9.1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes JR, Shiffman S. Conceptualizations of nicotine dependence: A response to DiFranza. Nicotine & Tobacco Research. 2008;10:1811–1812. doi: 10.1080/14622200802488341. doi:10.1080/14622200802488341. [DOI] [PubMed] [Google Scholar]
- Korhonen T, Broms U, Levalahti E, Koskenvuo M, Kaprio J. Characteristic and health consequences of intermittent smoking: Long-term follow-up among Finnish adult twins. Nicotine & Tobacco Research. 2009;11:148–155. doi: 10.1093/ntr/ntn023. doi:10.1093/ntr/ntn023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotz D, Fidler J, West R. Very low rate and light smokers: Smoking patterns and cessation-related behavior in England, 2006–2011. Addiction. 2011 doi: 10.1111/j.1360-0443.2011.03739.x. doi:10.1111/j.1360-0443.2011.03739.x. [DOI] [PubMed] [Google Scholar]
- Lindstrom M, Ostergren P. Intermittent and daily smokers: Two different socioeconomic patterns, and diverging influence of social participation. Tobacco Control. 2001;10:258–266. doi: 10.1136/tc.10.3.258. doi:10.1136/tc.10.3.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luoto R, Uutela A, Puska P. Occasional smoking increases total and cardiovascular mortality among men. Nicotine & Tobacco Research. 2000;2:133–139. doi: 10.1080/713688127. doi:10.1080/713688127. [DOI] [PubMed] [Google Scholar]
- MacPherson L, Strong D, Myers M. Using an item response model to examine the nicotine dependence construct as characterized by the HONC and the mFTQ among adolescent smokers. Addictive Behaviors. 2008;33:880–894. doi: 10.1016/j.addbeh.2008.02.007. doi:10.1016/j.addbeh.2008.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen QB, Zhu S. Intermittent smokers who used to smoke daily: A preliminary study on smoking situations. Nicotine & Tobacco Research. 2009;11:164–170. doi: 10.1093/ntr/ntp012. doi:10.1093/ntr/ntp012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perkins KA. Does smoking cue-induced craving tell us anything important about nicotine dependence? Addiction. 2009;104:1610–1616. doi: 10.1111/j.1360-0443.2009.02550.x. doi:10.1111/j.1360-0443.2009.02550.x. [DOI] [PubMed] [Google Scholar]
- Piper ME, Bolt DM, Kim S, Japuntich SJ, Smith SS, Niederdeppe J, et al. Refining the tobacco dependence phenotype using the Wisconsin Inventory of Smoking Dependence Motives. Journal of Abnormal Psychology. 2008;117:747–761. doi: 10.1037/a0013298. doi:10.1037/a0013298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piper ME, McCarthy DE, Bolt DM, Smith SS, Lerman C, Benowitz N, et al. Assessing dimensions of nicotine dependence: An evaluation of the Nictotine Dependence Syndrome Scale (NDSS) and the Wisconsin Inventory of Smoking Dependence Motives (WISDM) Nicotine & Tobacco Research. 2008;10:1009–1020. doi: 10.1080/14622200802097563. doi:10.1080/14622200802097563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piper ME, Piasecki TM, Federman EB, Bolt DM, Smith SS, Fiore MC. A multiple motives approach to tobacco dependence: The Wisconsin Inventory smoking dependence motives. Journal of Consulting and Clinical Psychology. 2004;72:139–154. doi: 10.1037/0022-006X.72.2.139. doi:10.1037/0022-006X.72.2.139. [DOI] [PubMed] [Google Scholar]
- Russell MAH. Cigarette smoking: The natural history of a dependence disorder. Journal of Medical Psychology. 1971;44:1–16. doi: 10.1111/j.2044-8341.1971.tb02141.x. doi:10.1111/j.2044-8341.1971.tb02141.x. [DOI] [PubMed] [Google Scholar]
- Scragg R, Laugesen M, Wellman RJ, DiFranza JR. Diminished autonomy over tobacco can appear with the first cigarettes. Addictive Behaviors. 2000;33:689–698. doi: 10.1016/j.addbeh.2007.12.002. doi:10.1016/j.addbeh.2007.12.002. [DOI] [PubMed] [Google Scholar]
- Shiffman S. How many cigarettes did you smoke? Assessing cigarette consumption by global report, Time-Line follow-Back, and ecological momentary assessment. Health Psychology. 2009a;28:519–526. doi: 10.1037/a0015197. doi:10.1037/a0015197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S. Light and intermittent smokers: Background and perspective. Nicotine & Tobacco Research. 2009b;11:122–125. doi: 10.1093/ntr/ntn020. doi:10.1093/ntr/ntn020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S, Brockwell SE, Pillitteri JL, Gitchell JG. Smoking cessation attempts and use of smoking cessation treatments in the United States. American Journal of Prevention Medicine. 2008;34:102–111. doi: 10.1016/j.amepre.2007.09.033. doi:10.1016/j.amepre.2007.09.033. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Dunbar M, Kirchner T, Li X, Tindle HA, Anderson S, et al. Smoker reactivity to cues: Effects on craving and on smoking behavior. Journal of Abnormal Psychology. in press doi: 10.1037/a0028339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S, Gwaltney CJ, Balabanis M, Liu KS, Paty JA, Kassel JD, et al. Immediate antecedents of cigarette smoking: An analysis from ecological momentary assessment. Journal of Abnormal Psychology. 2002;111:531–545. doi: 10.1037//0021-843x.111.4.531. doi:10.1037/0021-843X.111.4.531. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Paty JA. Smoking patterns and non-dependent smokers: Contrasting chippers and dependent smokers. Journal of Abnormal Psychology. 2006;115:509–523. doi: 10.1037/0021-843X.115.3.509. doi:10.1037/0021-843X.115.3.509. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Sayette M. Validation of the Nicotine Dependence Syndrome Scale (NDSS): A criterion-group design contrasting chippers and regular smokers. Drug and Alcohol Dependence. 2005;79:45–52. doi: 10.1016/j.drugalcdep.2004.12.009. doi:10.1016/j.drugalcdep.2004.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S, Stone AA, Hufford M. Ecological momentary assessment. Annual Review of Clinical Psychology. 2008;4:1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415. doi:10.1146/annurev.clinpsy.3.022806.091415. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Tindle H, Li X, Scholl S, Dunbar M, Mitchell-Miland C. Characteristics and smoking patterns of intermittent smokers. Experimental and Clinical Psychopharmacology. 2012 doi: 10.1037/a0027546. Mar 5. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S, Waters AJ, Hickcox M. The Nicotine Dependence Syndrome Scale: A multi-dimensional measure of nicotine dependence. Nicotine & Tobacco Research. 2004;6:327–348. doi: 10.1080/1462220042000202481. doi:10.1080/1462220042000202481. [DOI] [PubMed] [Google Scholar]
- Sobell MB, Sobell LC, Maisto SA. Time line follow back assessment method [TLFB] In: Lettieri DJ, Nelson JE, Sayers MA, editors. Alcoholism treatment assessment research instruments. (NIAA treatment handbook series 2) Rockville, MD: National Institute on Alcohol Abuse; 1979. pp. 167–188. [Google Scholar]
- Sterling KL, Mermelstein R, Turner L, Diviak K, Flay B, Shiffman S. Examining the psychometric properties and predictive validity of a youth-specific version of the Nicotine Dependence Syndrome Scale (NDSS) among teens with varying levels of smoking. Addictive Behaviors. 2009;34:616–619. doi: 10.1016/j.addbeh.2009.03.016. doi:10.1016/j.addbeh.2009.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stolerman IP, Jarvis MJ. The scientific case that nicotine is addictive. Psychopharmacology (Berlin) 1995;117:2–10. doi: 10.1007/BF02245088. doi:10.1007/BF02245088. [DOI] [PubMed] [Google Scholar]
- Stone AA, Shiffman S. Ecological momentary assessment (EMA) in behavioral medicine. Annals of Behavioral Medicine. 1994;16:199–202. Retrieved from http://psycnet.apa.org/psycinfo/1995-10701-001. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Substance Abuse and Mental Health Services Administration results from the national survey on drug use and health: National findings. Rockville, MD: NSDUH Series Office of Applied Studies; 2009. Retrieved from http://store.samhsa.gov/product/Mental-Health-Findings-Results-from-the-2009-National-Survey-on-Drug-Use-and-Health-NSDUH-/SMA10-4609. [Google Scholar]
- Tindle HA, Shiffman S. Smoking cessation behavior among intermittent smokers versus daily smokers. American Journal of Public Health. 2011;101:e1–e3. doi: 10.2105/AJPH.2011.300186. doi:10.2105/AJPH.2011.300186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trinidad DR, Perez-Stable EJ, Emery SL, White MM, Grana RA, Messer KS. Intermittent and light daily smoking across racial/ethnic groups in the United States. Nicotine & Tobacco Research. 2009;11:203–210. doi: 10.1093/ntr/ntn018. doi:10.1093/ntr/ntn018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wellman RJ, DiFranza JR, Savageau JA, Godiwala S, Friedman K, Hazelton J. Measuring adults’ loss of autonomy over nicotine use: The Hooked on Nicotine Checklist. Nicotine & Tobacco Research. 2005;7:157–161. doi: 10.1080/14622200412331328394. doi:10.1080/14622200412331328394. [DOI] [PubMed] [Google Scholar]
- Wellman R, DiFranza J, Pbert L, Fletcher K, Flint A, Young M, et al. A comparison of the psychometric properties of the hooked on nicotine checklist and the modified Fagerstrom tolerance questionnaire. Addictive Behaviors. 2006;31:486–495. doi: 10.1016/j.addbeh.2005.05.031. doi:10.1016/j.addbeh.2005.05.031. [DOI] [PubMed] [Google Scholar]
- Wellman RJ, Savagneau JA, Godiwala S, Savagneau N, Friedman K, Hazelton J. A comparison of the Hooked on Nicotine Checklist and the Fagerstrom test for Nicotine Dependence in adult smokers. Nicotine & Tobacco Research. 2006;8:575–580. doi: 10.1080/14622200600789965. doi:10.1080/14622200600789965. [DOI] [PubMed] [Google Scholar]
- World Health Organization. WHO global infobase on-line. 2007. Retrieved from http://www.who.iint/infobase/report.aspx. [Google Scholar]
- Wortley PM, Husten CG, Trosclair A, Chrismon J. Nondaily smokers: A descriptive analysis. Nicotine & Tobacco Research. 2003;5:755–759. doi: 10.1080/1462220031000158753. doi:10.1080/1462220031000158753. [DOI] [PubMed] [Google Scholar]
- Zhu S, Sun J, Hawkins S, Pierce J, Cummings S. A population study of low-rate smokers: Quitting history and instability over time. Health Psychology. 2003;22:245–252. doi: 10.1037/0278-6133.22.3.245. doi:10.1037/0278-6133.22.3.245. [DOI] [PubMed] [Google Scholar]