Abstract
Objectives. We examined the association between US workers’ access to paid sick leave and the incidence of nonfatal occupational injuries from the employer’s perspective. We also examined this association in different industries and occupations.
Methods. We developed a theoretical framework to examine the business value of offering paid sick leave. Data from the National Health Interview Survey were used to test the hypothesis that offering paid sick leave is associated with a reduced incidence of occupational injuries. We used data on approximately 38 000 working adults to estimate a multivariate model.
Results. With all other variables held constant, workers with access to paid sick leave were 28% (95% confidence interval = 0.52, 0.99) less likely than workers without access to paid sick leave to be injured. The association between the availability of paid sick leave and the incidence of occupational injuries varied across sectors and occupations, with the greatest differences occurring in high-risk sectors and occupations.
Conclusions. Our findings suggest that, similar to other investments in worker safety and health, introducing or expanding paid sick leave programs might help businesses reduce the incidence of nonfatal occupational injuries, particularly in high-risk sectors and occupations.
Paid sick leave is one of the nonwage benefits that US employers can offer to their workers. Although the 1993 Family and Medical Leave Act requires public agencies and private-sector establishments to provide up to 12 weeks of leave to eligible workers,1 this leave can be paid or unpaid.2,3 At the state level, only California and New Jersey have implemented paid family leave systems that provide workers with partial wage replacement.4 For workers, paid sick leave is associated with shorter recovery times3 and reduced complications from minor health problems.5–10 Paid sick leave also enables workers to care for loved ones when they most need it,11 can help prevent the spread of contagious diseases in day-care facilities and schools,12–15 and would enable compliance with pandemic influenza mitigation recommendations.16
Employers can realize gains from offering paid sick leave through the reduction of productivity losses associated with sick workers who continue to work but are not fully productive (i.e., “presenteeism”).3,7,17–19 Paid sick leave also can help prevent the spread of contagious diseases to coworkers, which reduces the cost of unscheduled leave (absenteeism).20 The costs associated with sick workers who continue to work can be substantial. For example, Goetzel et al.21 estimated presenteeism costs to be the largest component of the overall costs of absenteeism, productivity losses, and short-term disability.
Working while sick also can increase workers’ probability of suffering an injury.22 Sick or stressed workers who continue to work are likely to take medications, experience sleep problems, or be fatigued.23–25 These factors can impair their ability to concentrate or make sound decisions, which can in turn increase their probability of suffering an additional illness or sustaining a workplace injury. A recent study comparing workers with severe occupational injuries and those with nonsevere injuries demonstrated that a family member’s hospitalization, which is likely to be a major stressor for the entire family, increased by 9% the probability that a worker would suffer a severe occupational injury.26
Despite the advantages of paid sick leave for both workers and employers, the number of private-sector workers who have access to it remains low. For example, between 1996 and 1998 nearly 90% of workers in state and local governments had access to paid sick leave, compared with only 45% of workers in the private sector.3 A more recent study concluded that in 2010, after consideration of the average job tenure requirement of 78 days that is imposed by employers before workers have access to paid sick leave, only 40 million workers in the private sector had access to this job benefit, a figure well below the 44 million workers who were estimated to be eligible for such leave by the Bureau of Labor Statistics (BLS).27
Additional empirical evidence on the advantages and costs of paid sick leave would help inform employers’ decisions about offering or expanding paid sick leave benefits to workers. We examined the hypothesis that offering paid sick leave to workers would be associated with a lower incidence of nonfatal occupational injuries. We also assessed whether this association varied by occupation and industry sector, with the expectation that greater differences would be observed in occupations and sectors in which workers are at higher risk of suffering nonfatal occupational injuries. To our knowledge, this is the first US study to empirically examine these issues.
METHODS
According to our conceptual framework and economic theory, profit-maximizing firms would provide paid sick leave to their workers up to the point at which the marginal benefit of providing paid sick leave equals its marginal cost. Employers would consider the effects of paid sick leave on the incidence of occupational injuries, the cost of these injuries, and the cost of providing paid sick leave to determine whether offering or expanding access to paid sick leave helps maximize their profits. If the benefits to employers of providing paid sick leave include decreasing the incidence of occupational injuries, the cost of occupational injuries borne by employers, including workers’ compensation costs, also would decrease as a result. Therefore, if the impact of paid sick leave on the incidence of occupational injuries is high, it would be in the employer’s interest to offer or expand access to paid sick leave.
The employer also would weigh the expected cost of paid sick leave against the expected cost of occupational injuries. For example, employers that self-insure for workers’ compensation (i.e., employers that do not buy insurance but pay out of pocket to compensate injured workers for the cost of wages lost and medical care) or whose workers’ compensation premiums are experience rated might have a higher incentive to provide paid sick leave, if it reduces the incidence of occupational injuries, than employers that pay a fixed workers’ compensation premium.
In practice, it might not be easy for employers to assess the business value of paid sick leave or the relationship between profits and paid sick leave. Employers might have a good understanding of how the cost of paid sick leave and the cost of occupational injuries may affect their profits. However, the effects of paid sick leave on the incidence of occupational injuries and, consequently, on profits might be more difficult to assess or quantify. In addition, specific worker characteristics (e.g., hourly vs salaried) or firm characteristics (e.g., establishment size) can influence the incidence of occupational injuries and make it difficult for employers to distinguish those effects from the effects of paid sick leave. Therefore, we focused on clarifying the impact of paid sick leave on the incidence of nonfatal occupational injuries, after controlling for several worker and firm characteristics, to help employers better understand how offering paid sick leave can be a profit-maximizing strategy.
On the basis of the cross-sectional household-level data available to us in the National Health Interview Survey (NHIS), we specified the following equation to test empirically the 2 hypotheses of our study:
R, the dependent variable, was a binary variable with a value of 1 if worker i reported a nonfatal occupational injury during the previous 3 months and 0 otherwise (incidence of occupational injuries). The explanatory variables were broadly divided into available worker and firm characteristics. Vector X included worker characteristics such as gender, age, education, marital status, family size, and occupation type (hourly vs salaried). Vector Z included firm characteristics such as industry sector, size, location, and whether the firm offered employer-sponsored health insurance. A firm-specific variable, availability of paid sick leave (S), was included separately in the equation. β and φ are vectors of coefficients, and γ is a coefficient to be estimated. We hypothesized that γ would be negative and statistically significant. The final term in the equation was the error term, which was assumed to be normally and independently distributed with a mean of 0 and constant variance. The same equation was used to estimate the predicted probabilities of occupational injuries by industry sector and occupation. These predicted probabilities were estimated separately for each industry and occupation.
Other potentially relevant firm characteristics were not available in the NHIS data, such as information on incentives for providing sick leave, employer preference for risk that might influence actions to reduce the probability of occupational injuries, whether and how much a firm invested in occupational injury and illness prevention, the direct and indirect costs of occupational injuries for specific employers, flexible work schedules and other paid or unpaid benefits offered to workers, and whether a workforce was unionized.
Data Sample
We analyzed the adult NHIS sample for the years 2005 through 2008; the sample is representative of the civilian noninstitutionalized population of the United States. The data are publicly available at the National Center for Health Statistics Web site28 (more information about the survey is also available at that site29).
Variable Descriptions
All adults in the NHIS sample were asked whether they had access to paid sick leave through their main job or business. They were also asked whether they had suffered any injury or poisoning that required medical consultation during the 3 months prior to the survey. Injured respondents were asked to provide detailed information about the injury, including the date, body parts injured, activity at the time of injury (such as working at a paid job, driving, or working around the house), and events or exposures contributing to occupational injuries. Work-relatedness was determined through respondents’ reports that they were working at a paid job at the time of the injury.
Respondents who were not employed during the week preceding the survey (9.7%) or who had more than 1 job at the time of the survey (8.3%) were not considered. The NHIS also collected information on occupation and sector via standard classification codes.30 We converted detailed industry codes into 8 sectors based on the original National Occupational Research Agenda,31 according to which the program portfolio of the National Institute for Occupational safety and Health is organized.32
Only private-sector workers were considered because most public-sector workers have access to paid sick leave. In our sample, more than 80% of public-sector workers had access to paid sick leave, compared with less than 60% of workers in the private sector. Overall, more than 38 000 individuals with complete information were included in our univariate and multivariate analyses.
RESULTS
To assess the reliability of self-reported occupational injuries, we compared nonfatal injury incidence rates computed from the NHIS data with rates reported by the BLS. The NHIS respondents in our sample averaged 40.5 hours (i.e., full-time work) during the week that preceded the interview. Therefore, we estimated the annual number of full-time equivalent (FTE) workers by multiplying NHIS respondents’ reported hours worked during the week that preceded the interview by 50 weeks and dividing the product by 2000 hours. These FTE estimates were the basis for our calculations of the incidence rates that were compared with rates reported by the BLS.
We found that during 2005 to 2008, 0.8% of workers reported an occupational injury that required medical attention, resulting in an average annual incidence rate of 3.24 per 100 FTE workers. The nonfatal injury incidence rate per 100 FTE workers with access to paid sick leave was 2.59 compared with 4.18 among workers without access to paid sick leave. These rates were lower than the 2005 to 2008 average incidence rate of 4.27 calculated through annual rates reported by the BLS.33 The annual rates reported by the BLS, however, would be expected to be higher because they are based on all nonfatal occupational injury and illness cases recorded by employers, irrespective of whether workers received medical attention. On the basis of our incidence rate comparison, we concluded that the NHIS self-reported data reasonably reflected the US working population seeking medical attention for work-related injuries.
Descriptive Statistics
Descriptive statistics for the sample are presented in Table 1. The percentage of workers with access to paid sick leave remained relatively constant at 57% between 2005 and 2008. However, significant variation among industry sectors was observed. Between 2005 and 2008 fewer than 30% of workers in the agriculture and construction sectors had access to paid sick leave, compared with more than 65% of workers in the mining and health care sectors (Figure A, available as a supplement to the online version of this article at http://www.ajph.org). The overall difference in the availability of paid sick leave across different sectors was statistically significant (F = 36, P = .001).
TABLE 1—
Sample Descriptive Statistics: National Health Interview Survey, 2005–2008
| Sample, % | |
| Worker characteristics | |
| Injured | 0.80 |
| Male | 55.00 |
| Married | 56.00 |
| Hourly worker | 64.13 |
| Firm characteristics | |
| Paid sick leave available | 57.00 |
| Health insurance available | 70.98 |
| Sector | |
| Agriculture, forestry, and fishing | 1.09 |
| Construction | 8.13 |
| Health care and social assistance | 12.99 |
| Manufacturing | 15.43 |
| Mining | 0.61 |
| Services | 39.82 |
| Transportation, warehousing, and utilities | 5.00 |
| Wholesale and retail trade | 16.63 |
| Size | |
| Very small (1–9 workers) | 21.87 |
| Small (10–49 workers) | 40.72 |
| Medium (50–499 workers) | 20.67 |
| Large (≥500 workers) | 17.74 |
| Region | |
| Midwest | 25.81 |
| South | 36.16 |
| West | 20.53 |
| Northeast | 17.50 |
Note. The mean age of the sample was 39.64 years; the mean number of years of education was 14.95; and the mean family size was 2.92. The total number of observations 38 139, the total weighted number of observations was 353 189 392, and the average weighted number of observations per year was 88 297 348 (all values are for 2005–2008).
There also was a difference in the availability of paid sick leave by worker gender. The percentages of female and male workers with access to paid sick leave were 59% and 55%, respectively (Figure B, available as a supplement to the online version of this article at http://www.ajph.org), and the difference was statistically significant (2-sample test of proportion: z = 8.36, P < .001). Higher educational levels were associated with a higher level of access to paid sick leave. More workers in the northeastern part of the country (64%) than workers in other regions (56% on average) had access to paid sick leave. With respect to differences in access to paid sick leave for events or exposures contributing to occupational injuries (Figure C, available as a supplement to the online version of this article at http://www.ajph.org), workers without paid sick leave were more likely than workers with paid sick leave to have injuries caused by machines (z = 1.68, P = .05) and to be struck by objects (z = 1.28, P = .09).
Multivariate Analysis
The equation we used to test our hypotheses (see Methods section) was estimated with a logistic regression model that included paid sick leave and the worker- and firm-specific variables shown in Table 1 as explanatory variables. A variable for each survey year also was added to capture other unobserved potential differences between 2005 and 2008. The occupational injury outcome of the equation was modeled as a binary variable equal to 1 if an injury had occurred.
As shown in Table 2, the coefficient of the paid sick leave variable was negative and statistically significant. Most of the control variables also were statistically significant in expected directions. For example, the odds of male workers suffering a nonfatal occupational injury were more than twice the odds for female workers. The probability of suffering a nonfatal occupational injury also increased with age at a decelerating rate, as shown by the negative coefficient of the age-squared variable. Hourly paid workers were more than twice as likely as salaried workers to be injured.
TABLE 2—
Logistic Regression Results for Paid Sick Leave and Incidence of Nonfatal Occupational Injuries: National Health Interview Survey, 2005–2008
| Characteristic | OR (95% CI) | Robust SE |
| Male | 2.187** (1.630, 2.934) | 0.328 |
| Age | 1.083 (1.010, 1.160) | 0.038 |
| Age squared | 0.999** (0.998, 1.000) | 0.001 |
| Married | 0.937 (0.684, 1.283) | 0.150 |
| Education, y | 0.961* (0.923, 1.001) | 0.020 |
| Family size | 0.927 (0.846, 1.015) | 0.043 |
| Hourly worker | 2.204** (1.488, 3.264) | 0.442 |
| Paid sick leave available | 0.724* (0.528, 0.993) | 0.117 |
| Health insurance available | 1.743** (1.220, 2.489) | 0.317 |
| Occupational sector | ||
| Agriculture, forestry, and fishing | 1.205 (0.310, 4.679) | 0.834 |
| Construction | 1.844** (1.113, 3.056) | 0.475 |
| Health care and social assistance | 1.192 (0.709, 2.006) | 0.316 |
| Manufacturing | 1.311 (0.817, 2.106) | 0.317 |
| Mining | 1.077 (0.144, 8.030) | 1.104 |
| Services | 0.913 (0.588, 1.418) | 0.205 |
| Transportation, warehousing, and utilities | 0.935 (0.500, 1.745) | 0.298 |
| Wholesale and retail trade (ref) | 1.000 | |
| Firm size | ||
| Very small (1–9 workers) | 1.022 (0.619, 1.687) | 0.261 |
| Small (10–49 workers) | 1.244 (0.810, 1.909) | 0.272 |
| Medium (50–499 workers) | 1.132 (0.705, 1.815) | 0.273 |
| Large (≥500 workers) (ref) | 1.000 | |
| Region | ||
| Midwest | 1.496* (0.989, 2.265) | 0.316 |
| South | 0.798 (0.521, 1.221) | 0.173 |
| West | 1.220 (0.778, 1.912) | 0.280 |
| Northeast (ref) | 1.000 | |
| Survey y | 0.917 (0.812, 1.036) | 0.057 |
Note. CI = confidence interval; OR = odds ratio. The total number of observations was 38 139; Wald χ223 = 148.78 (P < .000), log-pseudolikelihood = −1685, pseudo-R2 = 0.055.
*P < .05; **P < .01.
After control for all of the other variables we considered, firm size did not have a significant effect on injury incidence, although workers employed in small (10–49 workers) and medium-sized (50–499 workers) firms tended to suffer more injuries than those working in very small (1–9 workers) and large (500 or more workers) firms. As level of worker education increased, the probability of suffering an occupational injury decreased; each additional year of education decreased the odds of suffering an injury by approximately 4%. Finally, the incidence of nonfatal occupational injuries was higher among workers with access to employer-sponsored health insurance.
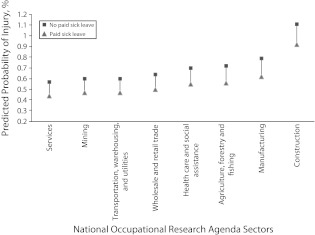
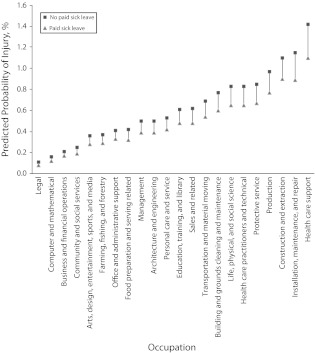
Predicted probabilities of occupational injury as a function of access to paid sick leave by industry sector and occupation are presented in Figures 1 and 2, respectively. The predicted values in these figures, which were estimated in separate equations for each industry sector and occupation, controlled for all worker and firm characteristics.
FIGURE 1—
Predicted probabilities of nonfatal occupational injuries, by availability of paid sick leave and occupational sector: National Health Interview Survey, 2005–2008.
FIGURE 2—
Predicted probabilities of nonfatal occupational injuries, by availability of paid sick leave and occupation: National Health Interview Survey, 2005–2008.
DISCUSSION
Firms may not recognize the potential contribution of paid sick leave to profit maximization. There is limited recognition, however, of the benefits of paid leave (of any sort) to employers. For example, according to Appelbaum and Milkman,4 employers in California reported either a positive or no noticeable effect on worker productivity, turnover, and morale following statewide implementation of paid family leave. However, there is a lack of empirical evidence on the overall business value of paid leave in general and paid sick leave in particular.
Our conceptual framework suggests that offering paid sick leave could be profitable if it helps reduce the incidence of occupational injuries, thus increasing profit. Our results are consistent with that hypothesis. Both the univariate and multivariate analyses demonstrated that workers with access to paid sick leave were significantly less likely to suffer nonfatal occupational injuries than were workers without access to paid sick leave. With all of the other variables we considered held constant, the odds of a nonfatal occupational injury were 28% lower among workers with paid sick leave.
Our results varied by industry sector, with the greatest differences in sectors with an above-average rate of nonfatal occupational injuries, such as construction, manufacturing, agriculture, and health care and social assistance. For instance, holding constant all other variables we considered, a construction worker without access to paid sick leave had a 21% higher predicted probability of suffering a nonfatal occupational injury than did a construction worker with access to paid sick leave. The differences were small in sectors such as services and mining that did not have a high overall rate of nonfatal occupational injuries. Similar variations were observed across occupations with a high risk of nonfatal occupational injuries, such as health care support; installation, maintenance, and repair; and protective services.
Our results suggest that offering paid sick leave to workers in industry sectors or occupations with a high risk of injury could contribute the most to reducing occupational injuries. Paid sick leave might reduce the pressure felt by employees to work while ill out of fear of lost income. Fewer sick workers performing at reduced functional capacity could result in safer operations and fewer injuries. Variations in events or exposures contributing to injuries (the largest paid sick leave differences were among workers with injuries caused by machines and workers struck by objects) suggest that workers in jobs with those exposures could realize the greatest gains.
Surprisingly, we observed a higher incidence of occupational injuries among workers with access to employer-sponsored health insurance. Given that we analyzed only those injuries that required medical attention, this outcome might simply indicate that employer-sponsored health insurance makes it easier for a worker to report an injury and obtain care. This outcome also suggests that our results are not solely a function of the availability of benefits, in that the associations of paid sick leave and health insurance with injury incidence were in opposite directions. This unexpected finding also could be a result of the lack of detailed firm-level data or more complete information on other worker benefits available to the population we studied, such as access to short- and long-term disability insurance. A better understanding of the interactions among these benefits might clarify this finding.
Limitations
Interpretation of our results is subject to some limitations. The cross-sectional nature of the data did not allow us to establish a causal relationship between the availability of paid sick leave and the incidence of nonfatal occupational injuries. In addition, other variables not available in the NHIS data may have influenced our results.
For example, our findings could have been influenced by whether a workforce is unionized, whether employers have occupational safety and health programs in place, or the level of employer risk aversion. If employers would prefer to bear less risk for occupational injuries, they might be willing to offer more paid sick leave than employers that are less risk averse. Another potential limitation is that injuries were considered occupational if they were self-reported as such by NHIS respondents. However, we have no reason to believe that this reporting may have differed systematically between respondents with and without access to paid sick leave.
Conclusions
Additional research could move us closer to demonstrating the business value of introducing or expanding paid sick leave. As outlined earlier, this would require demonstrating that the cost of occupational injuries would be higher than the cost of offering paid sick leave. If the necessary data were available, the consequences of sick workers infecting coworkers; the association between paid sick leave and fatalities, illnesses, or nonoccupational injuries; and the interactions among employer-sponsored benefits (e.g., access to paid sick leave and health insurance) could be empirically examined. From a societal perspective, understanding the potential consequences of worker access to paid sick leave for entire communities, especially in the case of contagious diseases, might point to additional opportunities for prevention.
Acknowledgments
We thank Dawn Castillo, Florence Tangha, John Piacentino, Frank Hearl, and the 3 anonymous referees for their valuable comments on earlier versions of the article.
Human Participant Protection
No protocol approval was needed for this study because publicly available data were used.
References
- 1.US Dept of Labor The Family Medical Leave Act. Available at: http://www.dol.gov/compliance/laws/comp-fmla.htm. Accessed May 17, 2012 [Google Scholar]
- 2.Treble J. A Tale of Two Continents: Sickness Absence and the Household Division of Labour in North America and Europe. Cardiff, Wales: University of Wales; 2007 [Google Scholar]
- 3.Lovell V. No Time to Be Sick: Why Everyone Suffers When Workers Don’t Have Paid Sick Leave. Washington, DC: Institute for Women’s Policy Research; 2004 [Google Scholar]
- 4.Appelbaum E, Milkman R. Leaves that pay: employer and worker experiences with paid family leave in California. Available at: http://www.cepr.net/documents/publications/paid-family-leave-1-2011.pdf. Accessed May 17, 2012 [Google Scholar]
- 5.Palmer SJ. Care of sick children by parents: a meaningful role. J Adv Nurs. 1993;18(2):185–191 [DOI] [PubMed] [Google Scholar]
- 6.Heymann SJ, Earle A, Egleston B. Parental availability for the care of sick children. Pediatrics. 1996;98(2):226–230 [PubMed] [Google Scholar]
- 7.Grinyer A, Singleton V. Sickness absence as risk-taking behavior: a study of organizational and cultural factors in the public sector. Health Risk Soc. 2000;2(1):7–21 [Google Scholar]
- 8.Kivimäki M, Head J, Ferrie Jet al. Working while ill as a risk factor for serious coronary events: the Whitehall II Study. Am J Public Health. 2005;95(1):98–102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Taylor MRH, O’Connor P. Resident parents and shorter hospital stay. Arch Dis Child. 1989;64(2):274–276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harris KM. Work and welfare among single mothers in poverty. Am J Sociol. 1993;99(2):317–352 [Google Scholar]
- 11.Heymann SJ, Earle A. The impact of welfare reform on parents’ ability to care for their children’s health. Am J Public Health. 1999;89(4):502–505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Loda FA, Glezen WP, Clyde WA., Jr Respiratory disease in group day care. Pediatrics. 1972;49(3):428–437 [PubMed] [Google Scholar]
- 13.Strangert K. Respiratory illness in preschool children with different forms of day care. Pediatrics. 1976;57(2):191–196 [PubMed] [Google Scholar]
- 14.Sullivan P, Woodward WE, Pickering LKet al. Longitudinal study of occurrence of diarrheal disease in day care centers. Am J Public Health. 1984;74(9):987–991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Oyediran MA, Bamisaiye A. A study of the child-care arrangements and the health status of pre-school children of employed women in Lagos. Public Health. 1983;97(5):267–274 [DOI] [PubMed] [Google Scholar]
- 16.Blake KD, Blendon RJ, Viswanath K. Employment and compliance with pandemic influenza mitigation recommendations. Emerg Infect Dis. 2010;16(2):212–218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Skatun JD. Take some days off, why don’t you? Endogenous sick leave and pay. J Health Econ. 2003;22(3):379–402 [DOI] [PubMed] [Google Scholar]
- 18.Hemp P. Presenteeism: at work—but out of it. Harv Bus Rev. 2004;82(10):49–58 [PubMed] [Google Scholar]
- 19.Hansen CD, Andersen HJ. Going ill to work: what personal circumstances, attitudes and work-related factors are associated with sickness presenteeism? Soc Sci Med. 2008;67(6):956–964 [DOI] [PubMed] [Google Scholar]
- 20.Li J, Birkhead GS, Strogatz DS, Coles FB. Impact of institution size, staffing patterns, and infection control practices on communicable disease outbreaks in New York State nursing homes. Am J Epidemiol. 1996;143(10):1042–1049 [DOI] [PubMed] [Google Scholar]
- 21.Goetzel RZ, Long SR, Ozminkowski RJet al. Health, absence, disability, and presenteeism cost estimates of certain physical and mental health conditions affecting U.S. employers. J Occup Environ Med. 2004;46(4):398–412 [DOI] [PubMed] [Google Scholar]
- 22.Bellaby P. Sick From Work: The Body in Employment. Brookfield, VT: Ashgate; 1999 [Google Scholar]
- 23.Aronsson G, Gustafsson K, Dallner M. Sick but yet at work: an empirical study of sickness presenteeism. J Epidemiol Community Health. 2000;54(7):502–509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Loeppke R, Hymel PA, Lofland JHet al. Health-related workplace productivity measurement: general and migraine-specific recommendations from the ACOEM expert panel. J Occup Environ Med. 2003;45(4):349–359 [DOI] [PubMed] [Google Scholar]
- 25.Lamberg L. Impact of long working hours explored. JAMA. 2004;292(1):25–26 [DOI] [PubMed] [Google Scholar]
- 26.Asfaw AG, Bushnell PT, Ray TK. Relationship of work injury severity to family member hospitalization. Am J Ind Med. 2010;53(5):506–513 [DOI] [PubMed] [Google Scholar]
- 27.Williams C, Drago R, Miller K. 44 Million U.S. Workers Lacked Paid Sick Days in 2010. Washington, DC: Institute for Women’s Policy Research; 2011 [Google Scholar]
- 28.National Center for Health Statistics National Health Interview Survey: questionnaires, data sets, and related documentation. Available at: http://www.cdc.gov/nchs/nhis/nhis_questionnaires.htm. Accessed May 17, 2012 [Google Scholar]
- 29.National Center for Health Statistics About the National Health Interview Survey. Available at: http://www.cdc.gov/nchs/nhis/about_nhis.htm. Accessed May 17, 2012 [Google Scholar]
- 30.National Center for Health Statistics National Health Interview Survey: 2009 data release. Available at: http://www.cdc.gov/nchs/nhis/nhis_2009_data_release.htm. Accessed May 17, 2012 [Google Scholar]
- 31.National Institute for Occupational Safety and Health National Occupational Research Agenda sector classification. Available at: http://www.cdc.gov/niosh/nora/sector.html. Accessed May 17, 2012 [Google Scholar]
- 32.National Institute for Occupational Safety and Health Program portfolio. Available at: http://www.cdc.gov/niosh/programs. Accessed May 17, 2012 [Google Scholar]
- 33.Bureau of Labor Statistics Workplace injuries. Available at: http://www.bls.gov/data/#injuries. Accessed May 17, 2012 [Google Scholar]