Abstract
The US Food and Drug Administration (FDA) has recently warned consumers about the risks of weight loss supplements adulterated with multiple pharmaceutical agents. Some of these supplements combine potent anorectics, such as amphetamines derivatives, with benzodiazepines, beta-blockers, and other medications to suppress the anorectics’ adverse effects. These weight loss supplements represent the most recent generation of rainbow diet pills, named for their bright and varied colors, which date back more than 70 years. Beginning in the 1940s, several US pharmaceutical firms aggressively promoted rainbow pills to physicians and patients. By the 1960s the pills had caused dozens of deaths before the FDA began removing them from the US market. We used a variety of original resources to trace these deadly pills from their origins in the United States to their popularity in Spain and Brazil to their reintroduction to the United States as weight loss dietary supplements.
PHYSICIANS HAVE PRESCRIBED a wide range of combination weight loss regimens for more than a century. Some regimens combine multiple anorectics, and others have included additional classes of pharmaceuticals to mask the anorectics’ unpleasant side effects. The modern use of weight loss regimens with opposing pharmaceutical actions can be traced to the 1890s, when clinicians first began to experiment with desiccated thyroid combined with strychnine and other drugs to ameliorate the thyroid's cardiac effects. By the 1940s, the newly discovered anorectic effects of amphetamine generated tremendous interest in combination weight loss regimens as physicians and pharmaceutical firms attempted to capitalize on amphetamine's actions while suppressing its unwanted adverse effects. New drug companies formed explicitly to market these combination diet pills. These brightly colored capsules and tablets, commonly referred to as rainbow diet pills, combined amphetamines, diuretics, laxatives, and thyroid hormones to maximize weight loss with digitalis, benzodiazepines, barbiturates, potassium, corticosteroids, and antidepressants to suppress the insomnia, palpitations, anxiety, and other common side effects of the weight loss medications.
The pharmaceutical firms marketing rainbow pills used a variety of unconventional promotional techniques to help convince thousands of doctors to prescribe rainbow pills for weight loss. As deaths and injuries linked to these pills accumulated over the years, the US Food and Drug Administration (FDA) eventually removed the rainbow pills from the US market in the late 1960s. Subsequently, these combination diet pills enjoyed widespread popularity in Spain and Brazil in the 1980s and 1990s. Rainbow pills have once again returned to the United States, now in the guise of weight loss dietary supplements, exposing the fragile boundary between the public's desire to have access to self-medication and the need to protect and promote the public health. To more fully understand these recent developments it is necessary to present a brief explanation of the cultural, medical, and commercial contexts that gave rise to the rainbow diet pills.
ORIGINS, 1890S TO 1940S
A cultural shift in body image of the late 19th and early 20th centuries led to increasing demand for prescription weight loss medications. The advertising industry and Hollywood helped to cultivate the ideal image of the slender woman and athletically trim man. The traditional depiction of social status, as Roberta Pollack Seid and others have shown, was turned on its head as the underclass was now increasingly depicted as stout rather than lean. 1 Athleticism, particularly for women—swimming, tennis, horseback riding, and even fast dancing—had been popular with the elite for decades, but in this period these activities began to spread beyond the well-heeled. The flapper distilled this trend: fashionable, mysterious, possessing sex appeal, and thin. Even the sales of penny scales grew. It was an era that practically begged for diet drugs.
For centuries preceding this cultural shift, physicians had noted the value of certain remedies for weight reduction, and the search intensified in the 19th century. Parisian dermatologist Louis-Victor Duchesne-Duparc observed in 1862 that bladderwrack, or sea kelp, caused his psoriatic patients to lose weight.2 James T. Whittaker, professor of physiology and clinical medicine at the Medical College of Ohio, experimented with arsenic to treat obesity. He reported success in a handful of cases in which lifestyle changes had failed.3 After the turn of the century, a vast array of products, most of dubious merit, became available, particularly for self-medication.4
Thyroid emerged as the most significant obesity drug in medical practice. In 1894, British physician Nathaniel Edward Yorke-Davies documented weight loss in obese patients given desiccated thyroid. Physicians in the 1890s began using thyroid to treat an increasing number of overweight patients, sometimes without advising lifestyle changes, and claimed extraordinary results.5 This new therapeutic approach, swept up in the nascence of organotherapy, began reshaping the way clinicians understood obesity, creating a new bipartite paradigm: exogenous,6 in which the root cause of obesity was attributed to overeating (“superalimentation”) in the absence of sufficient activity, and endogenous,7 characterized by diminished thyroid or other internal gland secretion. As weakness, palpitations, and other problems from thyroid preparations began to be recognized in the 1890s, some physicians experimented with using medications to counteract aspects of the hormone's effect; for example, some prescribed strychnine or digitalis leaf as a “tonic” to prevent thyroid's adverse effects on the heart.8
The discovery of amphetamine energized the weight loss industry. Introduced as the Benzedrine inhaler in 1932 by venerable Philadelphia firm Smith, Kline, and French, the American Medical Association (AMA) soon recognized Benzedrine as a treatment of narcolepsy, postencephaletic Parkinsonism, and certain depressive psychopathic conditions.9 Several clinical studies first published in the late 1930s demonstrated amphetamine's anorectic effect.10 The Clark & Clark Company of Camden, NJ, established in 1941, was one of the earliest manufacturers of diet pills combining amphetamine sulfate and thyroid along with phenobarbital, aloin, and atropine sulfate to counteract untoward effects.11 These diet pills, marketed as Clarkotabs, were among the first mass-produced rainbow pills (Figure 1).
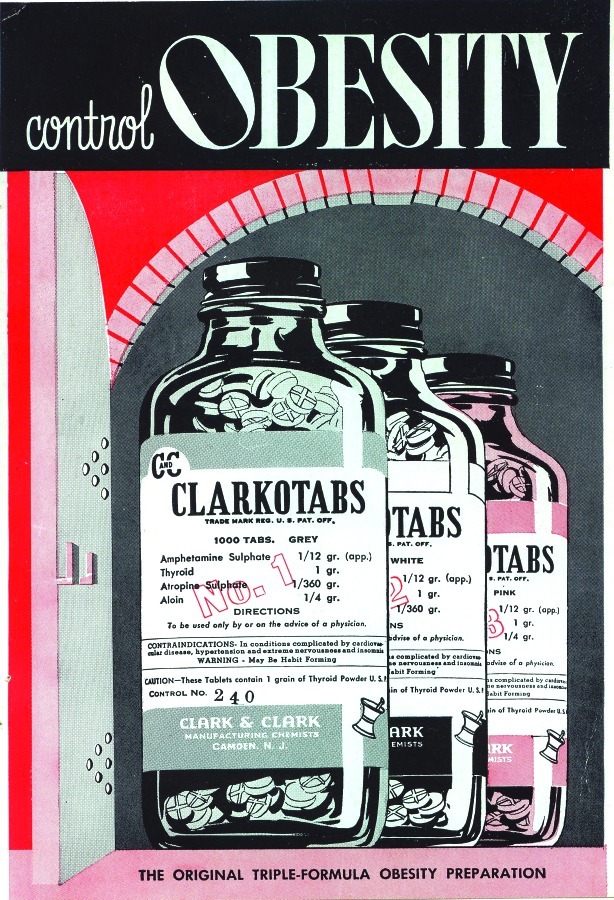
FIGURE 1—
A mailer that Clark & Clark distributed to physicians in March 1945.
Source. Collections of the US Food and Drug Administration History Office. Reprinted with permission.
EXPANDING THE US MARKET FOR RAINBOW PILLS, 1940S TO 1970S
From 1940 to 1950, several other small firms formed for the same purpose, including Western Research Laboratories of Denver,12 the Lanpar Company of Dallas (1950), and Mills Pharmaceuticals of St Louis (1950). These firms were all novices to the business of pharmaceuticals, yet all committed to finding a foothold in a unique approach to weight loss, an approach that the larger and established companies appeared to avoid. These manufacturers did not have the standing with the medical profession that the traditional so-called ethical manufacturers enjoyed. For example, the Dallas County Medical Society and the Texas Medical Association would not accept advertising from a rainbow pill manufacturer that was located in its own backyard, nor would the societies allow the firms to exhibit at their meetings.13
A number of unusual marketing methods set the rainbow pill companies apart from most of the pharmaceutical industry. For example, there were the brightly colored tablets and capsules. Clark & Clark's Clarkotabs came in green, white, blue, pink, gray, and yellow tablets (Figure 1). Firms manufactured different formulations of their diet pills and many formulations came in a half dozen or more different colors. The use of colorful pills was not just aesthetic, but also an important part of the regimen, as a Lanpar brochure explained to prescribers:
You should have at least more than one color of every medication because [imagine] here come two women together. Do not give them the same color tablet. Don't let them go out and say, “Well, all you have got to do is get those blue pills.” Give one of them blue and one of them pink. After all, it is individual medication for that patient. That's a little psychology and is well worth it … it is particularly designed for them.14
Despite the fact that patients moved in and out of the office with little history-taking or evaluation of any form, the fanciful variety of rainbow pill colors was intended to avoid the perception of factory-line therapeutics. Instead, the rainbow colors suggested personalized attention, a treatment uniquely crafted for the patient's individual weight loss requirements; a clearly insidious version of what might otherwise be termed “personalized medicine” today. The patient typically would leave the office with several dozen tablets in a variety of colors.
Rainbow diet pill formulations varied over the years both within a firm's portfolio as well as between firms. Although there was no standard formulation, the pills usually contained a selection of d-amphetamine, chlorthalidone, and thyroid hormone as weight loss agents, and digitalis, barbiturates, potassium, glandular extracts, and belladonna were added to counter side effects (Table 1).15 Particularly troubling was the dosage of medicines a patient might receive. Some dosages were excessive and led to severe complications, such as the death of a 19-year-old who was prescribed a daily regimen of 650 milligrams desiccated thyroid, 50 milligrams digitalis leaf, 25 milligrams amphetamine, 50 milligrams chlorthalidone, and 500 milligrams potassium.16
TABLE 1—
Common Ingredients of Rainbow Diet Pills, 1940s–Present
| Typical Ingredients to Induce Weight Loss | Typical Ingredients to Mask Side Effects | Regulatory Response | |
| United States, 1940s–1960s | d-amphetamine | cardiac glycosides | FDA interdiction and court-ordered injunctions 1968 |
| diuretics | barbiturates | ||
| thyroid hormones | corticosteroids | ||
| laxatives | potassium | ||
| phenolphthalein | belladonna | ||
| herbal ingredients | glandular extracts | ||
| Spain, 1980s–presenta | amphetamine derivatives | benzodiazepines | Spanish regulatory ban 1997 |
| fenproporex | corticosteroids | ||
| diethylpropion | glandular extracts | ||
| fenfluramine | |||
| thyroid hormones | |||
| diuretics | |||
| laxatives | |||
| herbal ingredients | |||
| Brazil, 1980s–presenta | amphetamine derivatives | selective serotonin | Brazilian regulatory ban 2007 |
| fenproporex | uptake inhibitors | ||
| diethylpropion | benzodiazepines | ||
| laxatives | |||
| diuretics | |||
| United States, 1980s–present | sibutramine | selective serotonin | FDA alerts 1987–present |
| fenproporex | uptake inhibitors | ||
| ephedrine | benzodiazepines | ||
| thyroid hormones | beta-blockers | ||
| laxatives | |||
| phenolphthalein | |||
| herbal ingredients |
Note. FDA = US Food and Drug Administration.
In Spain and Brazil, rainbow pills are often referred to as compounded diet pills (fórmulas magistrales para la obesidad [Spanish] and remédio de emagrecer manipulado [Portuguese]) among other names.
The rainbow pill firms sold their products directly to physicians. This uncommon, although not unprecedented arrangement, involved physicians selling the pills directly to patients, often in large quantities, and left pharmacies out of the rainbow pill pipeline. The prescriber would charge from $5 to $40 for brief visits. Physicians specializing in rainbow pill practices could see an impressive number of patients. “On a slow day” one physician was able to see more than 100 patients.17 Companies also assisted physicians in setting up obesity practices and troubleshooting business problems. The rainbow firms reminded their clients that the endgame was to create a weight practice that would allow the physician more leisure time, plus “it is a very nice practice to handle if you ever become physically incapacitated to any more or less extent.”18
Even more novel were some of the measures the companies pursued to “educate” potential clients about the rainbow pills. All-expense-paid pharmaceutical symposia ostensibly educated physicians about the therapeutics of obesity. However, in contrast to the teaching of contemporary medical textbooks,19 physicians at these symposia learned that weight gain was not a function of one's eating or exercising.20 The symposia faculty taught that endocrinologic imbalances led to obesity, and their regimens were rational because overweight patients often suffered from heart failure, low estrogen states, and hypothyroidism. By promoting an all-out endogenous etiology of obesity, the firms justified a wide range of pharmaceutical ingredients.21
By contrast, standard texts of the era emphasized that the first step in treating obesity should be proper diet and exercise. Although they recognized that thyroid hormone would accelerate metabolism, contemporary texts recommended it only when hypothyroidism was documented. In fact, several contemporary sources described a range of serious symptoms, including thyrotoxicosis, when thyroid hormone was used routinely for weight loss. Amphetamines were understood to control appetite, but shortly after their discovery academic physicians also recognized the dangers of long-term cardiac stimulation and other problems.22 Researchers early in this period acknowledged the potential for habituation, but revelation of their addictive properties took a little longer to be included in some texts. Medical textbooks cited amphetamines as, at best, temporary expedients to facilitate restricted eating habits. As for the role of digitalis in weight management, one author remarked that it was “a drastic step to take, for digitalis is very potent.” Some contemporary sources occasionally recommended diuretics in weight control.23
The theoretical foundation of the rainbow pill practice distinctly opposed what physicians would have learned in school and in continuing education about treating obesity.24 Furthermore, the pharmaceutical firms marketing these pills enjoyed little, if any, respect among academic physicians.25 Despite these barriers, the firms were able to attract many physicians to rainbow pill practices. By 1967, 5000 MDs and DOs devoted a majority of their practices to weight loss. Of these, 2000 practices focused exclusively on weight reduction. According to a Congressional investigation that year, weight loss clinics earned $250 million annually just in patient fees, and it was estimated that patients spent an additional $120 million on rainbow pills.26
A rainbow pill clinic could be both profitable and relatively easy to operate compared with other general medical practices, even if it flew in the face of professional standards and ethics. As the practice increased, so did concerns about attendant health risks. The AMA characterized these drugs as having
no rational therapeutic use, and therefore [their] administration for treatment of obesity must be regarded as misuse… . It now remains for organized medicine, through its local societies, to see that these abuses are not being perpetrated by members of the medical profession.27
Although patients were often reluctant to disclose use of rainbow pills to their regular physicians, adverse events, including deaths, began to be reported to the FDA as early as the 1940s. In the early 1950s, additional adverse reactions including deaths prompted a detailed investigation by the agency.28 However, the FDA dithered over whether to intervene, concerned about both the adequacy of the evidence and interfering with physicians’ practice of medicine.
To be sure, there was a striking difference of opinion within the agency regarding whether to take decisive action against the rainbow pills.29 By contrast, FDA dealt quite differently with another diet drug in the 1930s, dinitrophenol. Abandoned by clinicians early in that decade because of a number of severe side effects, several firms introduced about two dozen preparations for self-medication, which was still technically legal under the law at that time. The FDA latched on to therapeutic claims in testimonials to generate misbranding charges against at least one firm, which proved effective in removing at least some products from interstate commerce. In that case, the agency head determined the interests of the public health were worth the risks of taking a regulatory leap to move against a dangerous drug like dinitrophenol in the years that preceded the enhanced powers offered by the 1938 Food, Drug, and Cosmetic Act.30
The FDA continued to monitor the rainbow pill manufacturers. For example, officials in the bureaus of Medicine and Regulatory Compliance met in 1964 to address the problem of regulating thyroid and digitalis used in weight loss. Theoretically, the companies could claim these two drugs could be grandfathered in under the 1938 law, because both had been on the market long before. Mass seizures of the product would be logistically difficult because the rainbow pills were sold to physicians via mail order and, thus, a seizure would have to be made at thousands of the practitioner's offices. Officials with the FDA also considered requiring that the rainbow pill manufacturers provide full disclosure information, but the firms could very well agree to do that, which “might very well defeat the purpose of the seizures; said purpose being to cease the distribution of such irrational products.” Finally, agency officials considered bringing health hazard charges against the rainbow pills, but understood that any expert testimony would be opposed equally by testimonials of satisfied users and prescribing practitioners who would claim that the products were safe and effective. Instead, the FDA decided to continue to collect evidence of animal toxicity and patient injuries.31
Two important events outside of the FDA changed the regulatory landscape in 1968. A slim investigative reporter for Life magazine reported on her experiences posing as a patient at 10 obesity clinics (Figure 2). Despite receiving only perfunctory evaluations and sometimes counseled that she did not need to lose weight, she was prescribed more than 1500 pills.32 That same month, the US Senate, following months of detailed investigations in which the Subcommittee on Antitrust and Monopoly identified at least 60 deaths and many more serious adverse effects (Figure 3), launched hearings into the rainbow diet pill industry.33
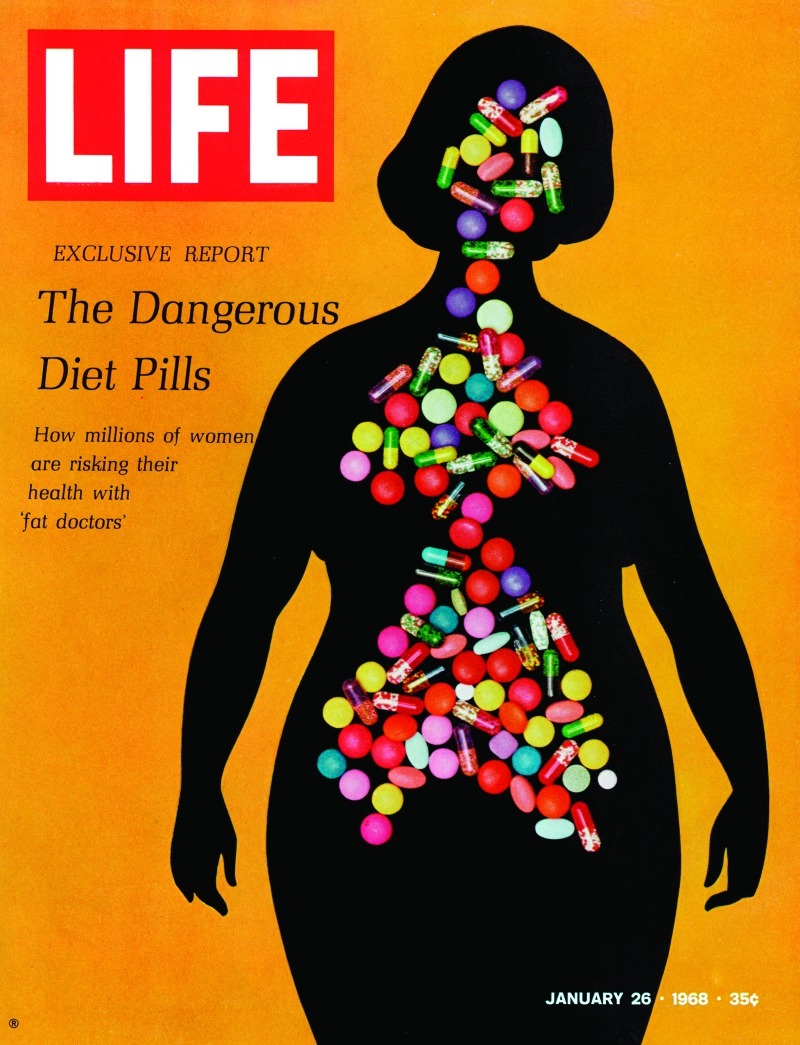
FIGURE 2—
1968 Life magazine exposé on rainbow diet pills. Susanna McBee reported on her experiences at several obesity clinics, in which she received rudimentary or no physical examinations but more than 1500 powerful pills.
Source. Life cover, January 26, 1968. Courtesy of Getty Images. Reprinted with permission
FIGURE 3—
News American front page of March 1, 1968, reported deaths from rainbow diet pills. The US Senate investigation of the rainbow diet pill industry revealed dozens of deaths across the country linked to these pharmaceuticals.
Source. News American, March 1, 1968. Courtesy of the Hearst Corporation. Reprinted with permission.
Armed with detailed postmortem evidence linking rainbow pills to several deaths, the FDA began to respond aggressively by January 1968.34 Within two months the agency seized 43 million tablets from a dozen manufacturers.35 The agency announced in April that any thyroid product intended to treat obesity in conjunction with amphetamines or other drugs would be seized for misbranding.36 Later in the year the agency secured the first of two court decisions against the largest firms.37
The federal government also moved to tighten control of amphetamine. Efforts had been in place at least since the 1965 Drug Abuse Control Amendments to increase accountability of the use of amphetamine in medical practice. Diversion of the drug for recreational use and the concomitant public health concerns had been recognized as a serious problem by the 1950s,38 but prescribing amphetamine—whether alone, as part of the rainbow regime, or for indications other than weight loss—continued to rise in the 1960s.39 Under the Comprehensive Drug Abuse Prevention and Control Act of 1970, which established different schedules for certain drugs based on their medical value vis-á-vis their abuse potential, amphetamine was relegated to Schedule II. This status mandated even greater hurdles for the prescribing and dispensing of the drug as well as production ceilings. In the 1970s, FDA also reconsidered obesity as a safe and effective use of amphetamine and its congeners, ruling that amphetamines were effective but only safe for short-term use, which essentially “marginalized the anorectics and contributed to the eventual decline in their use.”40
Thus, under siege in whole or in part from journalistic exposé, congressional inquiry, FDA mass seizure, court-ordered restriction, and legislated deep accountability, the heyday of rainbow pills as popular prescription drugs in the therapeutics of obesity was on the wane in the 1970s. But they would return, in a different form, to challenge the public health outcomes of consumer-driven demand for the rights to self-medication.
RISE AND FALL IN SPAIN, 1980S TO PRESENT
After the mass seizure of rainbow pills in the United States, Spain and Brazil produced the lion's share of rainbow pills in the 1980s and 1990s. The striking similarities between the American and Spanish rainbow pills make it highly likely that Spanish physicians were aware of and inspired by the US rainbow pill practice, although we are unaware of any documentary evidence directly linking these two practices.41 In Spain, the first documented use of rainbow pills (fórmulas magistrales para la obesidad) was not until the 1980s. It was then that Spanish physicians began to prescribe brightly colored pills that combined amphetamines, thyroid hormones, and diuretics. Corticosteroids, benzodiazepines, and other glandular extracts were added to ameliorate the common side effects (Table 1).42
As in the United States, Spanish physicians who prescribed these rainbow pills usually did so from private obesity clinics.43 In contrast to the United States, the rainbow pills were not manufactured by companies; instead, they were prepared at local compounding pharmacies.44 By the late 1980s Spanish clinics that formulated rainbow pills could be found throughout the country.45 As in the United States, physicians prescribed varying ingredients and dosages to individual patients and these individualized prescriptions provided Spanish patients with the perception of “personal preparations.”46 With time and growing popularity, novel methods of distribution appeared: the rainbow pills were mailed after only speaking to physicians by phone or dispensed from pharmacies directly without a physician's prescription, sometimes as “natural” diet pills.47
As the pills became more widely available, the Spanish academic and public health communities became increasingly concerned about their adverse effects. Electrolyte abnormalities, ischemic stroke, and congestive heart failure were described as complications of the rainbow pills.48 The most commonly reported adverse effects were abnormalities of thyroid function. In one series, rainbow pills led to 30 cases of hyperthyroidism.49 In addition to hyperthyroidism, severe hypothyroidism occurred after the pills were discontinued: a 50-year-old woman stopped using the pills before undergoing surgery for urinary incontinence and required critical care for myxedematous coma.50
Before the publication of the majority of these medical reports, the Spanish Department of Pharmacy and Health Products in 1993 issued a guidance advising that amphetamine derivatives alone should be prescribed for weight loss, and amphetamines should not be combined with other classes of pharmaceuticals unless the patient had a comorbid condition such as heart failure or hypothyroidism.51 As the academic reports of harm continued to accrue, the Ministry of Health took stronger action against the rainbow pills. In 1996 and 1997, the Ministry banned the advertising of rainbow pills; the naming of compounded pills using colors, imaginary names, or trade names; and the compounding of anorectics, psychotropics, hormones, laxatives, and diuretics in the same pill.52
Although the practice has greatly decreased in Spain, there remains an underground market from which consumers continue to obtain rainbow pills in European countries as was tragically illustrated in a recent report.53 One patient died and dozens were hospitalized when a compounding mistake led to consumption of rainbow pills containing greater than 100-fold the prescribed dose of l-thyroxine (30 mg rather than 25 μg) combined with sibutramine, aminophylline, caffeine, metformin, and diazepam.54
EMERGENCE AND RESPONSE IN BRAZIL, 1980S TO PRESENT
As rainbow pills would reenter the US markets as dietary supplements from Brazil, it is also worthwhile to examine the striking similarities between the practice in Brazil to that in the United States and Spain. Although the composition of the pills varied slightly from country to country (Table 1), the popularity and marketing of the pills as well as the serious adverse effects were remarkably similar on all three continents.
As in Spain, to our knowledge, there is no documented use in the 1960s and 1970s, but by the late 1980s the Brazilian rainbow pills (remédio de emagrecer manipulado) were widely prescribed.55 Typical preparations included four to six active ingredients but some prescriptions included more than 20 ingredients.56 In Brazil, amphetamine derivatives, thyroid hormones, laxatives, and diuretics were combined with benzodiazepines, fluoxetine, potassium, and a variety of herbal ingredients to offset the side effects.57
The distribution system for Brazilian rainbow pills was identical to that in Spain.58 Physicians often opened practices focused on obesity and would perform only cursory patient evaluations.59 This allowed prescribers to become quite prolific; a single physician averaged more than 30 prescriptions each working day of the year and many others wrote more than 1000 prescriptions per year.60 The same combinations and dosages of ingredients packaged in multiple colors also provided Brazilian patients the perception of personalized treatment.61
Instead of large pharmaceutical firms, in Brazil and Spain, small, local compounding pharmacies, often with close financial relationships to the prescribing physicians, specialized in rainbow pills. In the early 1990s, the number of pharmacies specializing in rainbow diet pills increased five-fold, 62 but, although the pharmacies flourished, patients suffered. Eighty-six percent of patients experienced side effects and in one study almost 4% of pill users required hospitalization from adverse effects of the pills.63 The Brazilian equivalent of the FDA (Agência Nacional de Vigilância Sanitária) in the late 1990s made an initial attempt to limit prescribing of rainbow pills,64 but prescriptions continued to be easily obtained until compounding of the pills was banned in 2007. However, even this did not eliminate the practice as the pills could still be prescribed as individual components.65 This practice was further restricted in 2011 when, following the lead of the FDA, which had recently withdrawn sibutramine because of risks of strokes and heart attacks, the Brazilian health agency reconsidered the status of all prescription weight loss pills. The Brazilian agency decided to permit the continued prescribing of sibutramine, but all amphetamine derivatives, including those most commonly included in Brazilian rainbow pills, were banned.66
However, as was the case in Spain, some pharmacies provided the diet pills directly to consumers under the guise of “natural” weight loss pills as early as the 1990s.67 Throughout the 2000s, with increasingly restrictive laws governing their prescribing, rainbow pills became more frequently marketed as herbal weight loss products.68 Not only would these direct-to-consumer sales of presumably “natural” diet pills using radio, television, and Internet advertising foreshadow the modern marketing of prescription medicines in the United States, but Brazil also became the major exporter of rainbow pills into the United States in the 1990s and 2000s.69
RETURN TO THE UNITED STATES, 1990S TO PRESENT
The US regulatory climate in the 1990s had changed substantially from the early 1970s, when rainbow pills had fallen out of favor as prescription drugs. The 1970s witnessed rising consumer involvement in regulatory activities. For example, a health activist-led campaign succeeded in securing one of the earliest mandatory patient package inserts for a prescription drug, the oral contraceptive; the Health Research Group petitioned FDA to ban Red No. 2; a mass protest against a possible FDA ban on saccharin triggered congressional action to preserve sales of the sweetener; and a groundswell of public opinion prevented FDA's attempt to establish standards to limit the potency of dietary supplements or to regulate them as drugs, culminating in the Vitamin–Minerals Amendment of 1976.70
The vitamin protest in particular foreshadowed a development two decades later that would have a direct impact on the return of rainbow pills to America. In the early 1990s Congress considered bills to address health fraud by strengthening FDA enforcement powers and restricting advertising of nutritional or health claims on dietary supplements, which the Federal Trade Commission regulated. The supplement and health food industry marshaled broad public support to resist these efforts, resulting in the Dietary Supplement Health and Education Act of 1994.71 This law created a new regulatory framework for supplements, and in so doing turned the clock back to 1906 for products used therapeutically by tens of millions. Former FDA Commissioner David Kessler reflected in 2000 on the law that came during his tenure:
The 1994 Dietary Supplement Act does not require that dietary supplements (defined broadly to include many substances, such as herbs and amino acids, that have no nutritive value) be shown to be safe or effective before they are marketed. The FDA does not scrutinize a dietary supplement before it enters the marketplace. The agency is permitted to restrict a substance if it poses a “significant and unreasonable risk” under the conditions of use on the label or as commonly consumed. The safety standard may sound as if the FDA has all the authority it needs to protect the public. The problem is that the burden of proof lies with the FDA.72
Thus, although the regulatory environment for prescription drugs had tightened considerably in the United States and abroad, rainbow diet pills were able to return to the United States in the 1990s in the guise of herbal weight loss pills. Imports of these pills grew in subsequent years with Brazilian imports initially dominating the modern rainbow pill industry. In 2005, the FDA confiscated thousands of bottles of weight loss supplements adulterated with fenproporex, benzodiazepines, and fluoxetine from two Brazilian companies.73 In California, a 25-year-old woman was hospitalized for progressively severe abdominal pain that was linked to the amphetamine found in the bright yellow and orange diet pills she had bought over the Internet from Brazil.74 In one survey in Massachusetts, two thirds of Brazilian rainbow pill users experienced insomnia, anxiety, palpitations, or other adverse effects.75 In addition to these serious side effects, Brazilian rainbow pills in the United States have also led to physical dependency and loss of employment from amphetamine-positive urine screens.76
Recent reports suggest that rainbow pills are now imported from a variety of countries including Mexico and China. The Texas Poison Center Network identified Mexican-produced rainbow diet pills as responsible for hypertension, tachycardia, and vomiting among other symptoms.77 In 2010 Chinese dietary supplements sold in Kansas were found to be adulterated with fenfluramine, sibutramine, ephedrine, propranolol, and other medications.78
Adulteration has been a violation under food and drug laws since 1906, but after the 1994 law prohibited premarket review, supplements have advanced unimpeded to store shelves until problems were brought to FDA's attention.79 Even after the FDA identifies pharmaceutical adulterants, the agency has significant difficulties removing the product from store shelves. A recent study of weight loss supplements adulterated with two banned medications demonstrated that sales in Massachusetts did not decline after an FDA alert and FDA-announced distributor recall.80
The pharmacologic action and bright colors of rainbow pills remain, but today in the United States the distribution network is quite different than it once was. Because patients can obtain these directly as supplements, physicians are no longer needed to prescribe the pills. Although the aesthetics of the colorful pills remain, there is no longer the deceptive component to their appearance in which they were marketed as treatments tailored to an individual patient's needs. Instead, they are available directly to consumers at local shops, over the Internet, and by person-to-person sales. These networks can be quite extensive, and authorities have indicted individuals for importing hundreds of thousands of rainbow pills and selling them within informal networks.81
CONCLUSIONS
Rainbow diet pills, potent mixtures of multiple prescription medications with complex pharmacodynamic interactions, have been prescribed by physicians for more than 70 years. Laws and regulations eventually prohibited the prescribing of these dangerous diet pills in the United States, but rainbow pills did not fade away. Rather, they emerged in Brazil and Spain in strikingly similar form to what had been prohibited in the United States. As regulators in Spain and Brazil greatly restricted their availability, manufacturers of rainbow pills turned to international markets and provided rainbow pills directly to consumers, repackaged as weight-loss supplements and shielded from the regulatory scrutiny applied to traditional pharmaceuticals.
Consumers of rainbow diet pills today face the adverse effects of the individual ingredients as well as the unknown effects of inappropriate dosages, poorly manufactured products, and lack of information about what they are consuming. Physicians and public health officials concerned with the care of patients suffering adverse effects from weight-loss supplements must understand the complex pharmacology of these products. The long history of rainbow diet pills reminds us of several lessons that should not be forgotten when one is addressing the obesity epidemic: the willingness of some health care professionals to cast aside much of what they learned about the pharmacology and safety of the drugs they prescribe and dispense; a willingness of rogue manufacturers to capitalize, at any cost, on the public's desire to lose weight; a willingness of many patients to grasp at anything that promises hope in the difficult fight against obesity; and a willingness of some regulators and legislators to dither when the exigencies of the public health suggest otherwise. ■
Acknowledgments
We gratefully thank Jeremy Greene and Nicolas Rasmussen for their provocative questions and thoughtful comments.
Endnotes
- 1. Roberta Pollack Seid, Never Too Thin: Why Women Are at War with Their Bodies (New York: Prentice Hall, 1989), 81 ff. See also A. Offer, “Body Weight and Self-Control in the United States and Britain Since the 1950s,” Social History of Medicine 14 (2001): 79–106; and A.A. Brewis, Obesity: Cultural and Biocultural Perspectives (New Brunswick, NJ: Rutgers University Press, 2011) [DOI] [PubMed]
- 2. A.W. Foot, “Clinical Notes of a Remarkable Case of Obesity, Treated with Liquor Potassae and Extract of Fucus Vesiculosis,” Dublin Journal of Medical Science 60 (1875): 499; M. Grieve, A Modern Herbal, 2 vols. (New York: Harcourt Brace, 1931; New York: Dover, 1971), 1: 111–114; and A. Osol ., The Dispensatory of the United States of America, 24th ed. (Philadelphia: J.B. Lippincott, 1947): 1459–1460. Reid Hunt and Atherton Seidell of the US Public Health Service Hygienic Laboratory, as part of their research on thyroid preparations and iodine content, reported in 1910 that sea kelp's action could be attributed to stimulation of the thyroid; see R. Hunt and A. Seidell, “Thyreotropic Iodine Compounds,” Journal of Pharmacology and Experimental Therapeutics 2(1910): 15 ff.
- 3. James T. Whittaker, “On the Use of Arsenic in the Treatment of Obesity,” Cincinnati Lancet and Clinic, n.s. 1 (1878): 133–134.
- 4. See, for example: Nostrums and Quackery, Vol. I, 2d ed. (Chicago: American Medical Association, 1912), 385–414; A.J. Cramp, Nostrums and Quackery, Vol. II (Chicago: American Medical Association, 1921, 657–688; and idem, Nostrums and Quackery and Pseudo-Medicine, Vol. III (Chicago: American Medical Association, 1936), 174–180, especially p. 174, where the author, director of the American Medical Association's Bureau of Investigation and long-time chronicler of popular unscientific medicines, claimed that of the three basic groups of items advertised and sold directly to the public for weight reduction—devices, drugs, and foods—drugs were by far the largest.
- 5. H.G. Wells, “The Physiology and Therapeutics of the Thyroid Gland and Its Congeners,” Journal of the American Medical Association 29 (1897): 1007–1008.
- 6. A. Luria, “Adipositas Universalis: An Inquiry Into the Modern Status of Its Etiology, Pathology, Symptomatology and Rational Treatment,” Medical Council 18 (1913): 306, 388–389 and 19: 23–24; R. Cecil, ed., A Text-Book of Medicine, 1st ed. (Philadelphia: W.B. Saunders, 1927), 594–597. On exercise, see, for example, J. Madison Taylor, “Reduction Cures for Overweight,” Medical Times 45(1917): 218–219. Note that H. Lisser, “The Frequency of Endogenous Endocrine Obesity and Its Treatment by Glandular Therapy,” California and Western Medicine 22, no. 10 (1924): 510, contended that in some cases of exogenous obesity, even if the basal metabolic rate were normal, thyroid could be administered if it were monitored closely by the physician.
- 7. For example, W.J. Hoyten, “Thyroid Gland in Obesity,” British Medical Journal 2 (1906): 197–198; Luria, “Adipositas Universalis,” 18: 388; W. Osler and T. McCrae, The Principles and Practice of Medicine, 8th ed. (New York: D. Appleton, 1914), 451–452; Cecil, A Text-Book of Medicine, 597; and Lisser, “Frequency of Endogenous Endocrine Obesity,” 512.
- 8. J.F. McCone, “Thyroid Extract in Obesity, With Report of a Case,” Pacific Record of Medicine and Surgery 12 (1897): 288–289, and Luria, “Adipositas Universalis,” 19: 61–63.
- 9. Statement by Lester Grinspoon, Competitive Problems in the Drug Industry: Safety and Efficacy of Anti-Obesity Drugs. Hearings before the Subcommittee on Monopoly of the Select Committee on Small Business, US Senate, 94th Cong., 2d Sess., 9 November 1976: 14705–14707.
- 10. Nicolas Rasmussen has related the long arc of amphetamine's unique place in therapeutics, drug policy, and culture; see “America's First Amphetamine Epidemic 1929–1971,” American Journal of Public Health 98, no. 6 (2008): 974–985; and On Speed: The Many Lives of Amphetamine (New York: New York University Press, 2008). See also Grinspoon, Competitive Problems, 14721 ff. [DOI] [PMC free article] [PubMed]
- 11. “Supplementary Factory Inspection Report,” 5 March 1943, attached to O. Olsen to Chief, New York Station, 16 March 1943, AF 10-762 (Clark & Clark), vol. 1, Files, Food and Drug Administration, Suitland, MD. Clark & Clark reformulated its Clarkotabs with methamphetamine later in the decade upon being sued by Smith, Kline and French for patent infringement. See Rasmussen, “America's First Amphetamine Epidemic,” 975; and Council on Pharmacy and Chemistry, “Drugs for Obesity,” Journal of the American Medical Association 134 (1947): 527–529. Rasmussen, On Speed, 106 ff., discusses Smith, Kline and French's strategy to litigate amphetamine interlopers, such as Clark & Clark.
- 12. Western Research Laboratories of Denver may have been established as early as 1929, and indirect, unconfirmed evidence suggests the firm marketed a fixed thyroid–digitalis combination for weight loss at some point in the 1930s (see Diet Pill Industry, Hearings before the Subcommittee on Antitrust and Monopoly of the Committee on the Judiciary, US Senate, 90th Congress, 2d Session, 23–31 January and 2 February 1968: 429, 620). However, there is no evidence to suggest an early Western Research Laboratories weight loss product attracted much attention; their business does not appear to take off until the 1940s.
- 13. Related in H. Doyl Taylor to J.L. Gordon, 29 July 1965, AF 3–404 (Lanpar), Acc. 88-75-8, Files, Food and Drug Administration, Suitland, MD.
- 14. Diet Pill Industry: 95.
- 15. Scrapbook, 1964, folder 5, AF 3–404 (Lanpar), Acc 88-75-8, Files, Food and Drug Administration, Suitland, MD.
- 16. R.W. Jelliffe et al., “Death From Weight-Control Pills,” Journal of the American Medical Association 208, no. 10 (1969): 1843–1847. [PubMed]
- 17. Diet Pill Industry: 91.
- 18. Ibid., 74, 93–95 (quote from p. 95), 100.
- 19. For example, R.L. Cecil and R.F. Loeb, eds. A Textbook of Medicine, 10th ed. (Philadelphia: W.B. Saunders, 1959), 636–641.
- 20. Diet Pill Industry: 386–390.
- 21. Ibid.
- 22. Grinspoon, Competitive Problems, 7–15.
- 23. R.L. Cecil and F. Kennedy, eds., A Textbook of Medicine by American Authors, 4th ed. (Philadelphia: W.B. Saunders, 1939), 659–662; Beckman, Treatment in General Practice, 577–583 (quote is from p. 583); and Cecil and Loeb, Textbook of Medicine, 636–641. See also the testimony of Frederick Wolff, a clinical pharmacologist from George Washington University called as an expert witness, in Diet Pill Industry: 21–24.
- 24. N. Gevitz. The DO's: Osteopathic Medicine in America (Baltimore: Johns Hopkins University Press, 1982), makes clear that, certainly by the early 1940s, osteopathic students were getting similar instruction in drug therapeutics as medical students.
- 25. This is evident, for example, throughout the 1968 Senate hearings; see Diet Pill Industry: passim.
- 26. Sen. Hart reported these figures (Diet Pill Industry: 2). His investigator, Dorothy Goodwin, suggested that the figure given for the number of physicians specializing in weight-control practices actually was conservative. Also, she claimed the practitioners were evenly divided between MDs and DOs, though the FDA believed that about two thirds of the clinics were run by osteopaths. See R. Abramson, “Obesity Doctors Face Senate Investigation,” Los Angeles Times, January 14, 1968, reproduced in Diet Pill Industry: 126; and P. Gall, “Busy Bariatricians: Doctors Who Specialize in Treating Obesity Multiply, Stir Criticism,” Wall Street Journal, January 11, 1967.
- 27. Abramson, “Obesity Doctors,” in Diet Pill Industry: 126; and “Reducing Pills and Digitalis Intoxication,” Journal of the American Medical Association 206, no. 5 (1968): 1078–1079 [quote] [PubMed]
- 28. Diet Pill Industry: 361–398.
- 29. Diet Pill Industry: 398, 405–406; and N.E. Cook, Interview by Robert G. Porter, April 26, 1977, transcript, National Library of Medicine, National Institutes of Health, Bethesda, MD, 20–21.
- 30. J.P. Swann, “Reducing with Dinitrophenol: Self-Medication and the Challenge of Regulating a Dangerous Pharmaceutical Before the U.S. Food, Drug, and Cosmetic Act,” in V. Quirke and J. Slinn, eds., Perspectives on Twentieth-Century Pharmaceuticals (Oxford: Peter Lang, 2010), 285–302.
- 31. J.J. Merendino, Memorandum of Conference, September 30, 1964, AF 3-404 (Lanpar), Acc 88-75-8, Files, Food and Drug Administration, Suitland, MD [quote]. On the agency's actions in the 1930s and 1940s regarding what it believed were inert glandular products, wherein manufacturers agreed to adjust the package labeling and yet that change did not decrease the popularity of the products, see H.M. Marks, The Progress of Experiment: Science and Therapeutic Reform in the United States, 1900–1990 (Cambridge: Cambridge University Press, 1997), 96–97; and Trade Correspondence 13 (December 1, 1939), 343 (December 13, 1940), and 376 (December 10, 1941), in V.A. Kleinfeld and C.W. Dunn, Federal Food, Drug, and Cosmetic Act: Judicial and Administrative Record, 1938–1949 (Chicago: Commerce Clearing House, n.d.), 574, 705–706, and 721.
- 32. Susanna McBee, “The Dangerous Diet Pills,” Life 64 (January 26, 1968): 22–29.
- 33. Diet Pill Industry, 3 ff.; and Susanna McBee, “A Legal Blow at the Diet Pill Business,” Life 64 (September 27, 1968): 86a.
- 34. . Jelliffe, “Death From Weight-Control Pills”; E. Lewis to H.L. Ley Jr, Memorandum, February 16, 1968, Files, FDA History Office, Silver Spring, MD; and R.C. Henry, “Weight Reduction Pills,” Journal of the American Medical Association 201(1967): 217–218.
- 35. US Food and Drug Administration, press release, March 21, 1968, Files, FDA History Office, Silver Spring, MD.
- 36. 33.Fed. Reg. 5616–17 (April 11, 1968)
- 37. Annual Reports, 1950–1974 (Washington, DC: US Food and Drug Administration, c. 1974), 617, 660.
- 38. J.P. Swann, “Drug Abuse Control Under FDA, 1938–1968,” Public Health Reports 112, no. 1 (1997): 83–86. [PMC free article] [PubMed]
- 39. Rasmussen, “America's First Amphetamine Epidemic,” 978–980.
- 40. Rasmussen, “America's First Amphetamine Epidemic,” 980–981; and E. Colman, “Anorectics on Trial: A Half Century of Federal Regulation of Prescription Appetite Suppressants,” Annals of Medicine 143 (2005): 382 [quote] [DOI] [PubMed]
- 41. The rainbow diet pill phenomenon greatly declined in the United States, but the pills had already reached international markets. On February 1, 1955, the Institute Cientifica Corrector de la Obesida opened in Mexico City. The endeavor of an American entrepreneur, the Institute marketed rainbow pill therapy to Mexican citizens and was grossing more than US $150 000 within a year of opening (seeDiet Pill Industry, 573–576). However, we are not aware of any documentary evidence linking this practice to the rainbow pills’ appearance in Spain.
- 42. E. Oria et al., [“Weight-Loss Drugs: Composition of Diet Pills Prescribed in Navarra”], Anales de Medicina Interna (Madrid, Spain) 14, no. 6 (1997): 275–281 [in Spanish]; M.V. Boltó et al., [“Adverse Reactions to a Weight Loss Compounded Formula”], Farmacia Clínica 10, no. 9 (1993): 724–732 [in Spanish]; and [“The Dangerous Style of Weight Loss Formulations,”] Boletin Terapéutico Andaluz 7, no. 12(1990): 45–47 [in Spanish] [PubMed]
- 43. Oria, “Weight-Loss Drugs”.
- 44. Ibid.
- 45. Ibid.; and “Dangerous Style”.
- 46. Oria, “Weight-Loss Drugs”.
- 47. Ibid.
- 48. R. Noguera et al., [“Cardiac Failure Secondary to Facticious Thyroidtoxicosis”] [letter], Medicina Clinica (Barcelona) 106, no. 5 (1996): 197–198 [in Spanish]; and, [“The Risks of Pharmacologic Treatments for Obesity”], Butlletí Groc 6, no. 4(1993): 13–14 [in Catalan] [PubMed]
- 49. A. Goday et al., [“Iatrogenic Hyperthyroidism. Report of an Outbreak”], Medicina Clínica (Barcelona) 105, no. 17 (1995): 658–660 [in Spanish] [PubMed]
- 50. B. Fernández Torres, et al., [“Postoperative Complications in a Case of Iatrogenic Hypothyroidism Induced by Diet Drugs”], Revista Española de Anestesiología y Reanimacion 45, no. 8 (1998): 349–352 [in Spanish] [PubMed]
- 51. Ministerio de Sanidad y Consumo, “Dirección General de Farmacia y Productos Sanitarios: Fórmulas Magistrales para el Tratamiento de la Obesidad,” Madrid, November 18, 1993, Circular Num. 22/93 [in Spanish]
- 52. Ministerio de Sanidad y Consumo, “Real Decreto 1907/1996, de 2 de Agosto, sobre Publicidad y Promoción Comercial de Productos, Actividades o Servicios con Pretendida Finalidad Sanitaria,” Boletín Oficial del Estado (Martes 6 de Agosto) 189, (1996): 24322–24325; and “Orden Ministerial por la que se Establecen Determinados Requisitos en la Prescripción y Dispensación de Fórmulas Magistrales y Preparados Oficinales para Tratamientos Peculiares,” Boletín Oficial del Estado (Miércoles 26 febrero) 49(1997): 6435–6437 [in Spanish]
- 53. H.R. Ramos et al., [“Pharmacologic Treatment of Obesity”], Revista Española de Obesidad 3 (2005): 13–25 [in Spanish]; Sociedad Española para el Estudio de la Obesidad (SEEDO), [“SEEDO 2000 Consensus for the Evaluation of Overweight and Obesity and the Establishment of Criteria for Therapeutic Intervention”], Medicina Clinica (Barcelona) 115, no. 15(2000): 587–597 [in Spanish]; and V. Ioos et al., “A Thyrotoxicosis Outbreak Due to Dietary Pills in Paris,” Therapeutics and Clinical Risk Management 4, no. 6 (2008): 1375–1379 [in Spanish] [DOI] [PMC free article] [PubMed]
- 54. Ioos, “Thyrotoxicosis Outbreak”.
- 55. S.A. Nappo, [“Consumption of Amphetamine-Type Anorectics (Diethylproprion, Fenproporex, Mazindol) and Fenfluramine in Brazil: Health Harm or Benefits”], Jornal Brasileiro de Psiquiatria 41 (1992): 417–421 [in Portuguese]
- 56. S.A. Nappo et al., “Inappropriate Prescribing of Compounded Antiobesity Formulas in Brazil,” Pharmacoepidemiology and Drug Safety 7, no. 3 (1998): 207–212; E.A. Carlini et al., [“Fluoxetine: Indication of Inadequate Use"], Jornal Brasileiro de Psiquiatria 58, no. 2(2009): 97–100 [in Portuguese]; and M.F. Gotijo Carneiro, , [“Prescription, Dispensing, and Regulation of Psychoactive Anorexigenic Drugs in Belo Horizonte, Minas Gerais, Brazil”], Cadernos de Saúde Pública, Rio de Janeiro 24, no. 8 (2008): 1763–1772 [in Portuguese]
- 57. Nappo, “Inappropriate Prescribing”; P.A. Cohen, “Imported Fenproporex-Based Diet Pills from Brazil: A Report of Two Cases,” Journal of General Internal Medicine 24, no. 3 (2009): 430–433; and M. F. Gotijo Carneiro, [“Prescription, Dispensing, and Regulation”] [DOI] [PMC free article] [PubMed]
- 58. Nappo, “Consumption of Amphetamine-Type Anorectics”.
- 59. Ibid., and Nappo, “Inappropriate Prescribing”.
- 60. Nappo, “Consumption of Amphetamine-Type Anorectics”.
- 61. Nappo, “Inappropriate Prescribing”.
- 62. Nappo, “Consumption of Amphetamine-Type Anorectics”.
- 63. S.A. Nappo et al., “Use of Anorectic Amphetamine-Like Drugs by Brazilian Women,” Eating Behaviors 3, no. 2 (2002): 153–165. [DOI] [PubMed]
- 64. Ministério de Saúde, “Portaria no. 344: Aprova o Regulamento Técnico sobre Substâncias e Medicamentos Sujeitos a Controle Especial,” Diário Oficial da União, May 12, 1998 [in Portuguese]
- 65. Agência Nacional de Vigilância Sanitária, “Resolução RDC no. 58, de 5 de Setembro de 2007: Dispõe sobre o Aperfeiçoamento do Controle e Fiscalização de Substâncias Psicotrópicas Anorexígenas e dá Outras Providências,” Diário Oficial da União, 6 (2007): 1–4 [in Portuguese]
- 66. Agência Nacional de Vigilância Sanitária. Dispõe sobre a proibição do uso das substâncias anfepramona, femproporex e mazindol, seus sais e isômeros, bem como intermediários e medidas de controle da prescrição e dispensação de medicamentos que contenham a substância sibutramina, seus sais e isômeros, bem como intermediários e dá outras providências. Resolução RDC no. 52, October 6, 2011.
- 67. A.E. Almeida et al., “Determination of Amfepramone Hydrochloride, Fenproporex, and Diazepam in So-Called ”Natural“ Capsules Used in the Treatment of Obesity,” Journal of Liquid Chromatography & Related Technologies 23, no. 7 (2000): 1109–1118; and M.R. Auricchio et al., “Detection of Anorectics and Benzodiazepines in Galenicals Used in Treatment for Obesity,” Revista do Instituto Adolfo Lutz 51(1991): 105–110.
- 68. H.M. Yano et al., [“Detection of Anorexigen and Benzodiazepinic Drugs in Weight Reducers Compounded Formulations and Analysis on Label Contents Adequacy by Pharmacognosy Laboratory, Instituto Adolfo Lutz, from June 2004 to March 2007”], Revista do Instituto Adolfo Lutz 67 (2008): 78–82 [in Portuguese]
- 69. Ibid.; and US Food and Drug Administration, “Questions and Answers About FDA's Initiative Against Contaminated Weight Loss Products,” January 27, 2011, http://www.fda.gov/Drugs/ResourcesForYou/Consumers/QuestionsAnswers/ucm136187.htm (accessed December 4, 2011)
- 70. R.D. Apple, Vitamania: Vitamins in American Culture (New Brunswick, NJ: Rutgers University Press, 1996), 144 ff; and B.R. Troetel, “Three-Part Disharmony: The Transformation of the Food and Drug Administration in the 1970s” (PhD dissertation, City University of New York, 1996)
- 71. Report of the Commission on Dietary Supplement Labels, November 24, 1997, http://web.health.gov/dietsupp (accessed December 4, 2011), cites a number of sources that discuss the history of DSHEA.
- 72. D.A. Kessler, “Cancer and Herbs,” New England Journal of Medicine 342 (2000): 1742–1743; see also S. Barrett, “How the Dietary Supplement Health Education Act Weakened the FDA,” rev. 2 February 2007, http://www.quackwatch.org/02ConsumerProtection/dshea.html (accessed September 10, 2011)
- 73. US Food and Drug Administration, “FDA Warns Consumers About Brazilian Diet Pills Found to Contain Active Drug Ingredients,” January 13, 2006, http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/2006/ucm108578.htm (accessed December 4, 2011); and M.H. Nguyen et al., “Amphetamine Lacing of an Internet-Marketed Neutraceutical,” Mayo Clinic Proceedings 81(2006): 1627–1629.
- 74. Nguyen, “Amphetamine Lacing”.
- 75. P. A. Cohen et al., “Imported Compounded Diet Pill Use Among Brazilian Women Immigrants in the United States,” Journal of Immigrant and Minority Health 11, no. 3 (2009): 229–236. [DOI] [PubMed]
- 76. Cohen, “Imported Fenproporex-Based Diet Pills.” and B. Smith and P.A. Cohen, “Dependence on the Brazilian Diet Pill: A Case Report,” The American Journal on Addictions 19, no. 3 (2010): 291–292. [DOI] [PubMed]
- 77. M.B. Forrester, “Redotex Ingestions Reported to Texas Poison Centers,” Human and Experimental Toxicology 29, no. 9 (2010): 789–791. [DOI] [PubMed]
- 78. US Food and Drug Administration, “Que She Herbal Supplement: Undeclared Drug Ingredients,” July 8, 2010, http://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm218439.htm (accessed December 4, 2011)
- 79. P.A. Cohen, “American Roulette—Contaminated Dietary Supplements,” The New England Journal of Medicine 361, no. 16 (2009): 1523–1525; and P. A. Cohen, “Assessing Supplement Safety—The FDA's Controversial Proposal,” The New England Journal of Medicine 366, no. 5(2012): 389–391.
- 80. P.A. Cohen . “Use of a Pharmaceutically Adulterated Dietary Supplement, Pai You Guo, Among Brazilian-Born Women in the United States, ” Journal of General Internal Medicine 27, no. 1 (2012): 51-56; and US Food and Drug Administration, “Questions and Answers”; and US Food and Drug Administration, “FDA Warns Consumers”. [DOI] [PMC free article] [PubMed]
- 81. Cohen, “Imported Fenproporex-Based Diet Pills”; US Food and Drug Administration, “Hooksett Woman Pleads Guilty to Four-Count Indictment,” April 28, 2011, http://www.fda.gov/ICECI/CriminalInvestigations/ucm253301.htm (accessed December 4, 2011); Nguyen, “Amphetamine Lacing”; and Cohen, “Imported Compounded Diet Pill Use”.