Abstract
We examine the scope of inquiry into the measurement and assessment of the state public health policy environment. We argue that there are gains to be made by looking systematically at policies both within and across health domains. We draw from the public health and public policy literature to develop the concepts of interdomain and intradomain policy comprehensiveness and illustrate how these concepts can be used to enhance surveillance of the current public health policy environment, improve understanding of the adoption of new policies, and enhance evaluations of the impact of such policies on health outcomes.
The 2011 Institute of Medicine report For the Public’s Health: Revitalizing Law and Policy to Meet New Challenges called public policy “among the most powerful tools to improve population health.”1(p18) However, the institute’s recommendation that legislators and government agencies “familiarize themselves with the array of legal and policy tools available”1(p68) poses substantial challenges in the absence of conceptual and methodological clarity on how these tools should be measured, classified, adopted, and used, especially at the state level.2–4 Categorizing and assessing different provisions of state policies is a complex task, made even more difficult by the absence of standardized methods.5,6 Different approaches to operationalizing policy measures have also led, in some cases, to conflicting evidence of their effectiveness.7–9 Furthermore, these assessments have largely treated public health issues as independent silos, with little reference to how policies may work in concert or at odds with one another either within or across public health domains.10
Several authors have highlighted the important limitations of existing studies that fail to account for the full range of policies that may have contributed to the outcome in question.10,11 To date, however, there is still relatively little systematic surveillance of the complete set of public health policies adopted by states across multiple public health arenas, and there has been even less of a focus on the evolution and impact of these different combinations of policies on health outcomes.
We argue here that an integrated and systematic assessment of public health policies within and across health domains is necessary for measuring the effectiveness of any individual health policy or law. Such an assessment is also necessary to understand how and why US states and localities have constructed vastly different health policy landscapes over time. Note that by “policy” we refer to the enactment or modification of laws, the development or modification of regulatory measures, and the setting of funding priorities, including the development of specific public sphere programs. By “health policy landscape,” we refer to the total number of health policies in place in a given jurisdiction at any given time.
Our objective is to respond to growing interest among policymakers and advocates in understanding the ways policy tools can be used to improve population health both within and across health areas.3 Indeed, findings from a 2007 Association of State and Territorial Health Officials (ASTHO) survey indicated that state health agencies ranked “developing effective health policy” among their top 5 priorities.12 Our argument is thus meant to engage researchers and advocates in considering how to apply a more thorough approach to their work in policy development and analysis and to assist them in communicating these ideas to policymakers.
In developing a framework for conceptualizing the broader state health policy landscape, we begin by introducing 2 new constructs: intradomain policy comprehensiveness and interdomain policy comprehensiveness. We discuss the ways in which these constructs aid in illuminating the composition of different state policy landscapes and discuss how they may influence the study, measurement, and effects of public health policies. To illustrate our arguments, we construct a data set of 27 public health policies in all 50 states between 1980 and 2000 and discuss observed patterns in public health policy adoption. We then review the literature on internal and external determinants of policy adoption and diffusion and consider the ways these determinants may be associated with the comprehensiveness of states’ health policy landscapes. We end with a series of research questions that stem from our approach.
THEORIES OF POLICYMAKING AND POLICY CHANGE
There are numerous ways in which public policies can affect health. At the first, most distal level are what Burris et al.5 term “incidental” laws and policies that affect income, education, housing, or other factors that have an indirect impact on health outcomes. Second are “infrastructural” laws and policies that authorize development and financing of institutions and programs meant to improve the public’s health and facilitate the uptake of social services. Third are “interventional” approaches meant to directly affect population health by limiting exposure to potentially harmful materials, discouraging unhealthy behaviors, encouraging healthy behaviors, or engaging in a combination of such approaches. We focus primarily on the third category because of its unambiguous intention and more proximal association with health outcomes. However, we anticipate that our conclusions may apply to other types of health policies as well.
We focus on states because they have substantial legal authority to intervene in protecting the health and safety of their populations. States use a variety of tools to intervene, including taxation; regulation of commercial activities through licensing and other mechanisms; provision of communication campaigns, subsidies, or incentives; or levying of criminal or civil penalties.13,14 A rich literature in political science has explored the ways in which new policy issues emerge on states’ political agendas,15,16 including the crucial roles of political interest groups, advocacy coalitions, and policy entrepreneurs.15,17–19 Classic works in the field have also investigated the ways in which states may be early leaders or reluctant followers in adopting new laws or policies20,21 and identified factors associated with policy diffusion across different states over time.22
The salience of health policy issues may depend on a number of factors, including the degree to which the public perceives the issue to be important and “actionable.”15 On a few public health issues a politicized national debate has focused attention and created external pressure to enact laws, as in the areas of access to abortion services and sexual education in schools.23,24 Pressure from federal mandates or cost-sharing programs has also created imperatives for state policy action, particularly in the areas of cash transfers and health insurance.25 However, much of public health policymaking takes place without high-profile polarized debate or federal mandate. In these cases, states’ decisions regarding new policy choices may be affected by factors such as past action in the health area, the emergence of interest groups, new evidence regarding policy effectiveness, the strength of the state’s public health infrastructure, and the political orientation of state leaders.22,26–28
Knowledge about the ways in which these factors interact in different states can aid in understanding how different policy landscapes evolve within states. Within the last decade, several scholars have investigated policy choices states have made regarding welfare reform. They have identified important commonalities among states based on the types of policies they adapt, the breadth and scope of these policies, eligibility criteria, and benefit levels.29 Insights from this work have yielded new evidence about the effects of such regulations regarding financial assistance in different environments.30,31 In the next section, we discuss how such an approach applied to health policy might enhance both public health knowledge and practice.
STATE POLICYMAKING WITHIN HEALTH DOMAINS
We define intradomain policy comprehensiveness as the extent to which a given state adopts the entirety of evidenced-based policies within a single public health domain. For example, states wishing to reduce fatalities from motor vehicle crashes have many evidence-based policy choices that could contribute to this outcome, including but not limited to primary enforcement of seatbelt use, adoption of graduated driver’s licenses, lowering speed limits, requiring motorcycle helmets, and requiring the appropriate use of infant and child safety seats. Approaches to studying the range of policies within a given public health domain have the potential to enhance our ability to assess the effectiveness of health policies and provide opportunities for multisectorial approaches to tackling health problems and their myriad determinants.
First, assessments of policy effectiveness depend on accurate characterization of the actions that can reasonably be attributed to it. But in the field of public health, a number of policies have followed an incremental path whereby many states initially adopt modest changes to laws or agency policies to address an issue before gaining the political support, managerial capacity, or new evidence necessary to develop a more robust approach to the problem. For instance, over decades, a state may initially restrict sales of tobacco in vending machines and then move to stricter penalties for sales of tobacco products to minors. Next, they may restrict billboard advertising of tobacco products and ban the sponsorship of certain events by tobacco companies. Only then might they move to raise sales taxes on cigarettes.
Analyses that focus on each new policy adoption as a unique effort can fail to capture the rest of the policy landscape and its possible interactions with the new policy, its implementation, or its effectiveness. For example, researchers working in the area of traffic fatality prevention have increasingly taken a broader view when assessing the impact of new policies (e.g., underage drinking laws) by simultaneously controlling for the existence of other public policies that may reduce the incidence of car crashes (e.g., speed limits) as well as policies that may reduce the likelihood that any given crash will result in injury or death (e.g., safety belt laws).32–35 However, this more comprehensive approach is far less common in other public health domains. The concept of intradomain policy comprehensiveness would aid in policy evaluation efforts through more accurate specification of the policy exposure in question.
Second, given the breadth of many public health issues, there is often a range of agencies that may explicitly or implicitly play a role in addressing any given problem. As such, any given new policy may act in concert (or at odds) with actions administered by other agencies, including schools, law enforcement, and housing, human services, employment, and commerce agencies. Each of these actors has different constituencies and powers and provides sets of services that may touch individuals, localities, or businesses. They may also use different policy tools to achieve their ends. For example, a variety of policy approaches can be used simultaneously to influence alcohol consumption: imposing sales taxes on alcohol, incorporating alcohol abuse training for state workers, or using incentives to increase treatment availability for alcohol addiction. Each of these approaches may involve a different state agency, and each may combine with other policies to create variations in outcomes. A more thorough approach to policy analysis and development within health areas may therefore identify opportunities for cross-agency collaboration, reduction of duplication of resources, and identification of gaps in action or population coverage.
UNDERSTANDING STATE POLICYMAKING ACROSS PUBLIC HEALTH DOMAINS
We define interdomain policy comprehensiveness as the extent to which a state adopts policies across multiple public health domains. For example, states may choose to adopt the policies listed earlier to reduce motor vehicle crashes and adopt a full set of policies aimed at reducing smoking, decreasing alcohol consumption, and improving nutritional outcomes. Exploration of public health policymaking across health domains can enhance our understanding of mechanisms for enhancing policy diffusion, choice and effectiveness of different policy tools, the role of political culture, and the social construction of target populations.
State health professionals participate in a number of organizations that help create learning environments and stimulate new policy efforts. These professional networks may be an important determinant of action across domains in public health for several reasons. First, except in the case of certain epidemics, the severity of many public health problems may be difficult to estimate, both because of an attenuated time period between exposures and health outcomes and because many health problems have multiple determinants. Evidence regarding the severity of some problems may emerge slowly and be hotly disputed (e.g., the link between smoking and lung cancer). State professional associations provide expert testimony, repackage components of contested legislation, and identify allies to aid in passing laws.36 In these ways, they may strengthen the capacities of state governments to act in multiple domains.
Second, organizations such as ASTHO and the National Conference of State Legislatures regularly convene state policy leaders, disseminate results through written and Web-based materials, provide technical assistance, distribute examples of enacted (and defeated) legislation, and suggest strategies for advocacy on specific policy topics. These organizations have agendas that involve multiple domains and varied expertise, which may help explain the increased adoption of interdomain policies over time.37 For example, ASTHO recently summarized evidence on nutrition and advocates that states support certain forms of menu calorie labeling, regulate or ban trans fats, and develop strategies for reducing sodium in foods, including warning labels for high-sodium foods.38 ASTHO also provides testimony to Congress on obesity, highlighting specific state initiatives deemed to be successful.39 Given the charge of such organizations, experience in one domain may be quickly applied to new ones.
Investigating interdomain comprehensiveness may also help us understand ways in which choices among policy tools in one arena may have an impact on the choice of tools in another. That is, the choice of tools may be interdependent, with states acting in sequential years to use the same tool on a number of different health issues.40 States may decide to increase or create taxes for consumers on products linked to poor health outcomes, such as alcohol, and then expand that approach to include tobacco and soda. In these ways, states may become public health “learning laboratories,” applying the lessons of policymaking in public health in one arena to another.41 At the same time, in some states it may be politically feasible to pass a tax only on a single product; as a result, action in one arena may delay or forgo action in another. Adopting this more comprehensive approach in policy evaluations, for example, may shed additional light on reasons for a policy’s effectiveness or lack thereof that stem from experiences states have already had with certain policy tools.
Examining interdomain comprehensiveness also offers the opportunity to test assumptions about the relationship between state political culture and policy adoption and effectiveness. Schneider and Ingram42 have argued that some of the variation in public policies within domains (often involving entitlement programs) is related to the political power of the group affected and the ways in which program recipients are judged to be socially deserving. A number of case studies have examined the proposition that public perceptions of groups judged to be less deserving result in public programs with smaller benefits or greater criminal penalties for “undesirable” behaviors.43–45 For example, states with the largest Black populations tend to provide the least generous welfare benefits, and White adults are less likely to support welfare programs if they believe that the primary users and beneficiaries are members of minority groups.46–50 It may also be that the same states that most severely punish those deemed to be immoral or undeserving of protection in one area (e.g., criminally sanctioning those with HIV/AIDS who fail to inform partners of their status) would adopt the same approach in another (denying parental rights to women whose children have been exposed to alcohol in utero). Finding consistent evidence that groups viewed as “least deserving” are more harshly sanctioned or less generously provided for across multiple health issues would strengthen the argument that social policy choices are driven more by the perceptions of the policy targets than by the nature of the policy concern itself.
Finally, with regard to public health, some states may have relatively consistent patterns of protecting certain groups, particularly children, that stem from state constitutions or legal precedents and reflect varied understandings of state responsibilities. Patterns of protections for such groups may be less related to narrow policy issues of the public health domain and more related to the state’s historic interpretation of its responsibilities and authority. Thus, investigating a state’s pattern of enacting laws targeted toward a specific group across multiple domains may help assess the feasibility of passing any new legislation concerning that target population.
POLICY TRAJECTORIES AND TYPOLOGIES AND THEIR DETERMINANTS
To investigate whether the constructs of intradomain and interdomain policy comprehensiveness might aid in thinking about the public health policy landscape, we investigated whether states adopt more “interventional” public health policies over time and whether there are discernible trajectories in this adoption behavior across domains (interdomain) over time. We assembled data on 27 evidence-based public health policies from existing databases and the peer-reviewed literature, including the National Highway Transportation Safety Administration,51 the Centers for Disease Control and Prevention’s State Legislated Actions on Tobacco Issues,52 and the National Institute on Alcohol Abuse and Alcoholism’s Alcohol Policy Information System,53 for the period 1980 to 2000. We included only policies for which there was evidence of effectiveness and for which data were available for all states for each year between 1980 and 2000 (Table 1 provides a description of each policy). For measures of intradomain comprehensiveness, we assessed the presence of 5 evidence-based policies regarding alcohol regulations. To explore interdomain comprehensiveness, we simply counted the number of policies listed in Table 1 that each state had in place each year.
TABLE 1—
Evidence-Based Health Policies Assessed: US States, 1980–2000
| Health Domain | Public Policy or Law | Evidence | Data Sources |
| Alcohol regulations | Minimum legal drinking age (21 years) | References 34, 54–62 | References 53, 58, 63–65 |
| Beer keg registration requirement | |||
| Beer tax (above yearly median) | |||
| Host legal liability (i.e., dram shop laws) | |||
| Sunday sales restrictions | |||
| Drunk and risky driving | Zero tolerance laws (lower blood alcohol content for individuals younger than 21 years) | References 66–75 | References 51, 53, 65, 76, 77 |
| Blood alcohol levels < 0.08% | |||
| Open container laws | |||
| Graduated driver’s license requirements | |||
| Mandatory prison days for driving under the influence offenses | |||
| Speed limits (< 60 mph) | |||
| Tobacco and smoking | Clean indoor air: restaurants | References 78, 79 | References 52, 80, 81 |
| Clean indoor air: bars | |||
| Clean indoor air: worksites | |||
| Restrictions on cigarette advertising | |||
| Cigarette taxes (above national yearly median) | |||
| Firearms | Juvenile sales restrictions | References 82, 83 | References 84–86 |
| Gun safety locks | |||
| Secondary sale background checks | |||
| Concealed weapons restrictions | |||
| Mandatory wait periods | |||
| Passenger and driver safety | Adult seatbelt requirements | References 54, 87–92 | References 77, 93–95 |
| Seatbelt primary enforcement | |||
| Child restraint device requirements | |||
| Fines for failure to use seatbelt | |||
| Reduced legal liability for failure to use seatbelt | |||
| Motorcycle helmet requirements for all riders |
Note. This list of policies is not exhaustive. It contains only policies for which there is peer-reviewed evidence of effectiveness and impact on health outcomes and for which data are publicly available for all states and years.
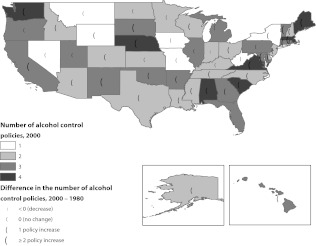
Figure 1 presents the total number of evidence-based policies concerning alcohol regulation (and for which complete data were available) by state. Darker shades represent a higher number of policies in place in 2000. The size of the parenthesis symbol shows the change in number of policies since 1980, with larger symbols representing a greater number of policies adopted. The map shows several concentrations of states with higher numbers of policies, but no single state had all 5 policies in place as of 2000. Seven states had only a single policy in place in 2000. In these states, either no changes in laws had been made since 1980 or the single law in question had been added during that time. Seven other states had 4 of the 5 policies in place in 2000. Most of these states exhibited substantial policy action during the study period. Only 1 state (Indiana) reduced the number of laws in place (from 3 in 1980 to 2 in 2000). Overall, 14 states had no changes in policy between 1980 and 2000.
FIGURE 1—
Intradomain policy comprehensiveness (total number of evidence-based policies) regarding alcohol regulations: US states, 1980–2000.
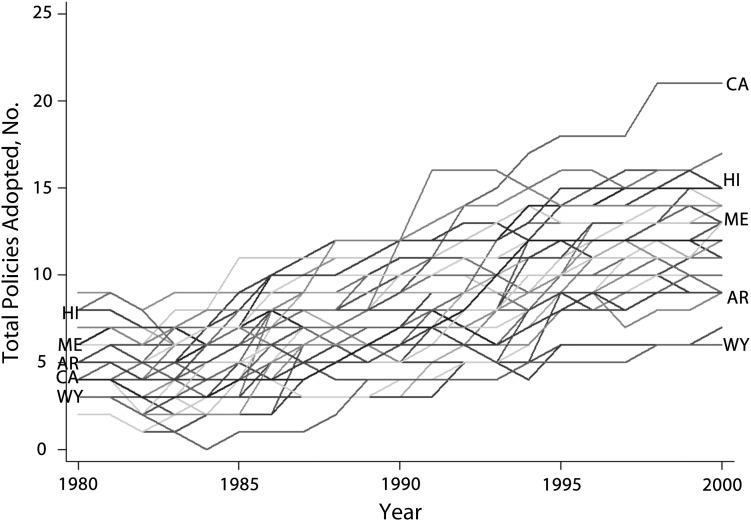
Figure 2 illustrates interdomain policy comprehensiveness. As can be seen, there is wide variation among states in the number of policies they had in place in 1980. There was a mean of 5 (of 27) policies per state, ranging from a low of 2 policies in Colorado and New Hampshire to a high of 9 in Illinois. By 2000, the mean number of policies had increased to 12 and ranged from a low of 7 in Mississippi to a high of 21 in California. Clearly, there was a national trend toward adopting more evidence-based health policies over this period. What is striking is that the variation among states also increased over time instead of regressing toward the mean. To explore these observations further, we characterize states’ policy adoption behaviors into different trajectories over time.
FIGURE 2—
Interdomain policy comprehensiveness (adoption of policies across multiple public health domains): US states, 1980–2000.
Note. Each line represents the total number of policies present within the state during each year. (A color version of this figure is available as a supplement to the online-only version of this article at http://www.ajph.org.)
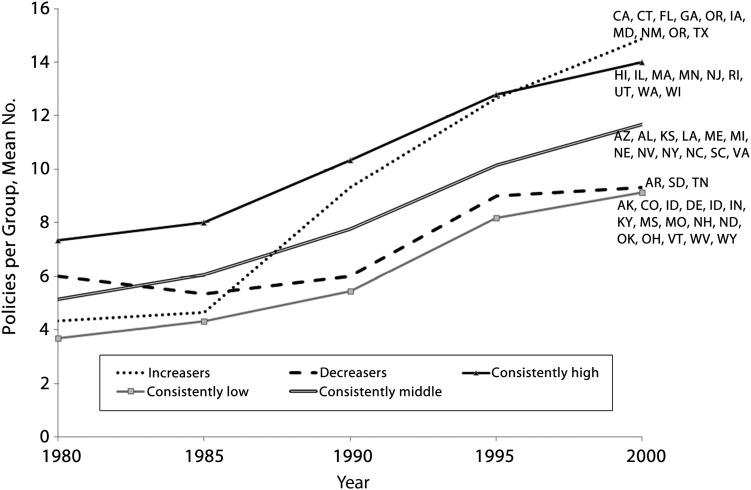
Figure 3 shows the clustering of state policy adoption trajectories. To characterize these trajectories, we calculated the mean intercept (initial number of policies) and slope (rate of change) over time and grouped states according to their relationship to these measures. This descriptive technique resulted in identification of states exhibiting 5 major patterns over time: minimalist states (below-mean intercept and average positive slope, e.g., Wyoming), maximalist states (higher than mean intercept and mean positive slope, e.g., Hawaii), constant increasers (lower than mean intercept and higher than mean positive slope, e.g., California), constant decreasers (mean intercept and negative slope, e.g., Arkansas), and constant midlevel states (mean intercept and mean positive slope, e.g., Maine).
FIGURE 3—
Interdomain policy comprehensiveness clusters: US states, 1980–2000.
These illustrations of state policy adoption behavior, albeit crude, nevertheless suggest that there may be patterns of state policymaking that bear further investigation. Figure 1 resembles maps produced by advocacy groups (see, for example, the Brady campaign state scorecards96 or the Insurance Institute for Highway Safety’s ranking of child restraint laws97) and other agencies that characterize the extent to which states adopt a set of recommended policies, often by constructing scales that attach equal (or at times different) weights to each policy present. These resources have been enormously helpful in identifying gaps in coverage for specific health areas. However, there are numerous areas for which such data are not available or for which the publicly available source does not rigorously document how the data are obtained, coded, updated, or validated.98 Explicit use of concepts such as intradomain comprehensiveness could encourage more systematic data collection regarding the complete set of public health policies intended to address any given health problem, provide opportunities to identify policy gaps, and help focus advocacy on new or continued policy adoption efforts.
Figures 2 and 3 illustrate patterns of interdomain comprehensiveness that also require investigation. These figures suggest that obvious explanations of policy adoption patterns may not suffice. For instance, there is large geographic variation within each cluster of states, suggesting that the comprehensiveness of the health policy landscape is more than a function of regional characteristics. Nor does examination of the states grouped within each cluster suggest a simple “blue state/red state” dichotomy in regard to the number of policies in place at any given time. The figures also demonstrate that, even as of the latest date for which all data were available, no states had adopted the full range of the reduced set of evidence-based policies we examined.
Using the concepts of interdomain and intradomain comprehensiveness to investigate these findings could aid in understanding why states behave differently from one another in responding to new policy options. For instance, the minimalist states, by definition, adopted very few policies within and across public health domains. However, this observation is subject to different interpretations about the state’s role in protecting public health, depending on whether these minimalist states adopted only those policies with the strongest evidence. States that established higher numbers of policies may have done so either by adopting many policies within a single domain (high intradomain comprehensiveness) or by pursuing a minimal approach across many health domains (high interdomain comprehensiveness), perhaps as a result of a strategy of targeting certain population groups (such as children). Finally, maximalist states have a more comprehensive set of policies both within and across public health policy domains, but none have adopted all of the policies under examination.
Identifying the most important factors that explain variations in the adoption of evidence-based public policies at the state level remains a challenge. These factors have been classified as determinants that are internal or external to the state. External determinants of policy adoption include new knowledge or scientific evidence, the geographic region in which states exist, the need to comply with nationally accepted standards or mandates, and the positioning of states for resources in relation to one another.99 Internal determinants include factors such as the demographic characteristics of a state’s population (educational attainment, racial composition, urbanicity, political ideology).22
The presence of a state legislature that is paid and in session a substantial portion of the year is an important internal determinant of whether new policies are adopted,100,101 as is the size of the public workforce.102 The political makeup of the state population103 and of the state legislature and governor28,101,104 is also associated with the numbers and types of policies adopted. Several studies have demonstrated a direct relationship between the percentage of adults with self-identified liberal political values in a state and the passage of hate crime laws105; greater gun purchasing restrictions106; Medicaid reimbursement, eligibility, and services; and mental health and hospital policies.107 State fiscal health is also important, especially with respect to adoption (and repeal) of distributive programs.108 Finally, many of these factors may be interdependent, in that markers of government capacity may themselves reflect the state’s political culture and attitudes toward government and its ability to use information to improve government effectiveness.109
ELEMENTS OF A RESEARCH AGENDA
So far, we have made an argument for more comprehensive approaches to assessing the state health policy landscape, reviewed theories describing why states may exhibit different patterns of health policies over time, and illustrated these concepts empirically. This section outlines elements of an agenda to further research in this area.
First, amassing consistent evidence about the effectiveness of a variety of public health policies has, at times, been hampered by inconsistency and methodological limitations.98 Collecting these data, over multiple years and with sufficient detail, will require substantial and rigorous original research. Beyond data collection, there are several ways to approach the measurement of the proposed constructs. These include simply counting the number of policies in each domain a given state may have in place at any given time (as we have done here), weighing certain policies more heavily on the basis of the evidence supporting their potential impact, or using statistical techniques to capture potential latent factors describing specific policy combinations or clusters of policy adoption trajectories over time.
Measuring these constructs is complicated by the fact that they are neither independent nor static. They evolve over time, reflect learning within and among states, and are often the result of multiple actors working both for and against any new legislative action. They may even be repealed. Adequately capturing the dynamic nature of the health policy landscape may require the development of new techniques or adapting tools from other fields, such as those from the field of complexity or systems science.110,111
Second, how can we identify which factors drive states to adopt more comprehensive policy approaches to public health problems over time? Patterns of increasing policy adoption and demonstrably effective actions within a domain may reflect a growing appetite for action within that domain. As expertise grows among policymakers and government agencies within a given state in implementing policy within a given domain, these leaders and agencies may become important political actors as well, creating policy feedback loops.112 Key research questions include whether early adopters are able to act more comprehensively within a public health domain over time, whether the comprehensiveness of the health policy landscape at any given time increases the likelihood of future policy adoption efforts, and identification of factors associated with sustaining more comprehensive approaches over time.
A third issue is whether the social construction of target groups may favor more comprehensive approaches, but only for some groups such as children. As noted, states may create protections for children, even in areas in which they may recognize the right of adults to make decisions that could harm their own health, such as policies regarding car safety, tobacco, and alcohol. Would such states be less willing to intervene on other issues regarding adults as well? For instance, would such states choose to focus on school-based nutrition and physical activity guidelines or restrictions on school vending machines rather than on calorie labeling or trans-fats bans?
Fourth, are some policy tools favored more consistently in some states than others? Do certain policy tools, to the degree that they create revenue for the state (minus the costs of enforcement and administration), come to be viewed more positively in states as they choose among policy options to address a public health problem? If so, is it possible to identify best practices in implementation across policy contexts?
Fifth, how important is ideology in determining which health domains are addressed and how? Are states with higher percentages of citizens with liberal orientations also more likely to support a larger public workforce on health issues? As noted, this may create greater pressure and capacity for state action across multiple domains. But does ideology also explain state capacity to adopt and implement more comprehensive policy combinations? If this is the case, then some health policies may need to be repackaged to be more politically palatable to laggard states.
Sixth, although states are essential in determining much of health law and policy, localities are also essential. Thus, a broader research agenda on public health policymaking will need to take into account the rise of entrepreneurial localities that compensate for the lack of policy movement at the state level or attempt to restrict state intervention in local affairs. Learning from local experiences (bottom-up diffusion) may be particularly important in the case of policies for which local evidence may be more compelling to lawmakers than experiences from other states,113 but its impact on influencing more comprehensive approaches to public health policymaking is as yet unknown.
Finally, it will be important to understand the cumulative impact of more comprehensive policies on health outcomes over time. Is the mere presence of more policies always better for population health? Are there interactions whereby the presence of one policy (e.g., primary enforcement of seatbelt laws) may enhance the effectiveness of others (e.g., distracted driving regulations)? And, given a menu of policy approaches to any given health problem, have otherwise similar states adopted different combinations of policies that have achieved similar results?
CONCLUSIONS
We have argued that existing approaches to understanding the health policymaking process and its outcomes may obscure important explanations for patterns of policy adoption in public health. They may also complicate attribution of health impacts to individual policies, especially when several different policies together may have had a role in determining the outcome of interest. A broader approach to understanding the state health policy environment, its complexities and dynamics, may ultimately stimulate research on the links between public health and other public policies, their determinants, and their trajectories over time. The aim of this approach is to aid researchers, advocates, and practitioners in identifying whether there are combinations of acceptable policies that would be likely to promote the desired health outcomes and that also would be likely to be adopted in that particular state. That is, are there policy substitutions that might be more feasibly enacted and have similar results in different contexts?
Our discussion here is intended to provoke debate and provide researchers, policymakers, and advocates with new tools to understand the ways in which policy options fit together and how policy decisions may affect a number of important health outcomes. Making more comprehensive assessments of state health policy environments may be more complex than performing single-policy impact evaluations but may open up new vistas for understanding the ways in which policies and policymaking can improve the public’s health.
Acknowledgments
This work was supported by the Robert Wood Johnson Foundation Public Health Law Research Program (grant 67150).
Thanks to Scott Burris and J. Lawrence Aber for helpful comments on a previous version of the article, and thanks to Margaret Paul and Jean Bae for research assistance.
Human Participant Protection
No protocol approval was needed because only publicly available data were used.
References
- 1.Institute of Medicine For the Public’s Health: Revitalizing Law and Policy to Meet New Challenges. Washington, DC: National Academies Press; 2011 [Google Scholar]
- 2.Pomeranz JL, Teret SP, Sugarman SD, Rutkow L, Brownell KD. Innovative legal approaches to address obesity. Milbank Q. 2009;87(1):185–213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McKinnon RA, Orleans T, Kumanyika SKet al. Considerations for an obesity policy research agenda. Am J Prev Med. 2009;36(4):351–357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brownell KD, Warner KE. The perils of ignoring history: big tobacco played dirty and millions died. How similar is big food? Milbank Q. 2009;87(1):259–294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Burris S, Wagenaar AC, Swanson J, Ibrahim JK, Wood J, Mello MM. Making the case for laws that improve health: a framework for public health law research. Milbank Q. 2010;88(2):169–210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chriqui JF. doi: 10.1111/j.1748-720X.2011.00559.x. OCJ, Chaloupka FJ. What gets measured, gets changed: evaluating law and policy for maximum impact. J Law Med Ethics. 2011;39(suppl 1):21–26. [DOI] [PubMed] [Google Scholar]
- 7.Smith RC, Geller ES. Marketing and alcohol-related traffic fatalities: impact of alcohol advertising targeting minors. J Safety Res. 2009;40(5):359–364 [DOI] [PubMed] [Google Scholar]
- 8.Hahn RA, Kuzara JL, Elder Ret al. Effectiveness of policies restricting hours of alcohol sales in preventing excessive alcohol consumption and related harms. Am J Prev Med. 2010;39(6):590–604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nelson JP. Advertising bans, monopoly, and alcohol demand: testing for substitution effects using state panel data. Rev Ind Organ. 2003;22(1):1–25 [Google Scholar]
- 10.Traynor TL. The impact of state level behavioral regulations on traffic fatality rates. J Safety Res. 2009;40(6):421–426 [DOI] [PubMed] [Google Scholar]
- 11.Wagenaar A, Gehan JP, Jones-Webb Ret al. Communities mobilizing for change on alcohol: lessons and results from a 15-community randomized trial. J Community Psychol. 1999;27(3):315–326 [Google Scholar]
- 12.Understanding State Public Health. Arlington, VA: Association of State and Territorial Health Officials; 2007 [Google Scholar]
- 13.Gostin L. Public Health Law: Power, Duty, Restraint. 2nd ed Berkeley, CA: University of California Press and Milbank Memorial Fund; 2008 [Google Scholar]
- 14.Bemelmans-Videc ML, Rist R, Vedung E. Carrots, Sticks, and Sermons: Policy Instruments and Their Evaluation. Piscataway, NJ: Transaction Publishers; 2003 [Google Scholar]
- 15.Kingdon JW. Agendas, Alternatives, and Public Policies. Boston, MA: Little, Brown & Co; 1984 [Google Scholar]
- 16.Jenkins-Smith H, St. Clair GK, Woods B. Explaining change in policy subsystems: analysis of coalition stability and defection over time. Am J Pol Sci. 1991;35(4):851–880 [Google Scholar]
- 17.Sabatier PA, Jenkins-Smith H. An advocacy coalition model of policy change and the role of policy oriented learning therein. Policy Sci. 1988;21(2–3):129–168 [Google Scholar]
- 18.Baumgartner FR, Jones BD. Agendas and Instability in American Politics. Chicago, IL: University of Chicago Press; 1993 [Google Scholar]
- 19.Key VO. Politics, Parties and Pressure Groups. New York, NY: Thomas Y. Crowell; 1947 [Google Scholar]
- 20.Grupp FW, Jr, Richards AR. Variations in elite perceptions of American states as referents for public policy making. Am Polit Sci Rev. 1975;69(3):850–858 [Google Scholar]
- 21.Elazar DJ. American Federalism: A View From the States. 3rd ed New York, NY: Harper & Row; 1984 [Google Scholar]
- 22.Berry FS, Berry W. Innovation and diffusion models in policy research. : Sabatier P, Theories of the Policy Process. 2nd ed Boulder, CO: Westview Press; 2007:223–260 [Google Scholar]
- 23.Norrander B, Wilcox C. Public opinion and policymaking in the states: the case of post-Roe abortion policy. Policy Stud J. 1999;27(4):707–722 [DOI] [PubMed] [Google Scholar]
- 24.Vergari S. Morality politics and the implementation of abstinence-only sex education: A case of policy compromise. : Mooney C, The Public Clash of Private Values. New York, NY: Chatham House; 2000:201–212 [Google Scholar]
- 25.Stream C. Health reform in the states: a model of state small group health insurance market reforms. Polit Res Q. 1999;52(3):499–525 [Google Scholar]
- 26.Volden C. The politics of competitive federalism: a race to the bottom in welfare benefits? Am J Pol Sci. 2003;46(20):352–364 [Google Scholar]
- 27.Volden C. States as policy laboratories: emulating success in the Children’s Health Insurance Program. Am J Pol Sci. 2006;50(2):294–312 [Google Scholar]
- 28.Barrilleaux C, Brace P. Notes from the laboratories of democracy: state government enactments of market and market-based health insurance reforms in the 1990s. J Health Polit Policy Law. 2007;32(4):655–683 [DOI] [PubMed] [Google Scholar]
- 29.Meyers MK, Gornick JC, Peck L. Packaging support for low income families: policy variation across the U.S. states. J Policy Anal Manage. 2001;20(3):457–486 [Google Scholar]
- 30.Bainbridge J, Meyers MK, Waldfogel J. Child care policy reform and the employment of single mothers. Soc Sci Q. 2003;84(4):771–791 [Google Scholar]
- 31.McKernan S-M, Bernstein J, Fender L. Taming the beast: categorizing state welfare policies: a typology of welfare policies affecting recipient job entry. J Policy Anal Manage. 2005;24(2):443–460 [Google Scholar]
- 32.Fell JC, Fisher DA, Voas RB, Blackman K, Tippetts AS. The impact of underage drinking laws on alcohol-related fatal crashes of young drivers. Alcohol Clin Exp Res. 2009;33(7):1208–1219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fell JC, Fisher DA, Voas RB, Blackman K, Tippetts AS. The relationship of underage drinking laws to reductions in drinking drivers in fatal crashes in the United States. Accid Anal Prev. 2008;40(4):1430–1440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fell JC, Fisher DA, Voas RB, Blackman K, Tippetts AS. The relationship of 16 underage drinking laws to reductions in underage drinking drivers in fatal crashes in the United States. Annu Proc Assoc Adv Automot Med. 2007;51:537–557 [PMC free article] [PubMed] [Google Scholar]
- 35.Chaloupka FJ, Grossman M, Saffer H. The effects of price on alcohol consumption and alcohol-related problems. Alcohol Res Health. 2002;26(1):22–34 [PMC free article] [PubMed] [Google Scholar]
- 36.Balla SJ. Interstate professional associations and the diffusion of policy innovations. Am Polit Res. 2001;29(3):221–245 [Google Scholar]
- 37.Heaney MT. Brokering health policy: coalitions, parties, and interest group influence. J Health Polit Policy Law. 2006;31(5):887–944 [DOI] [PubMed] [Google Scholar]
- 38.Prevention of Chronic Disease Through Menu Labeling, Trans Fat Bans, and Sodium Reduction: Position Statement. Arlington, VA: Association of State and Territorial Health Officials; 2009 [Google Scholar]
- 39. Childhood obesity: the declining health of America’s next generation—national problem, southern crisis (testimony of Susan R. Cooper, Tennessee Department of Health). Available at: http://www.help.senate.gov/imo/media/doc/Cooper3.pdf. Accessed May 30, 2012.
- 40.Makse T, Volden C. The role of policy attributes in the diffusion of innovations. J Polit. 2011;73(1):108–124 [Google Scholar]
- 41.Oliver TR. The politics of health policy. Annu Rev Public Health. 2006;27:195–233 [DOI] [PubMed] [Google Scholar]
- 42.Schneider AL, Ingram HM, Deserving and Entitled: Social Constructions and Public Policy. Albany, NY: State University of New York Press; 2005 [Google Scholar]
- 43.Dyson E. Come Hell or High Water: Hurricane Katrina and the Color of Disaster. New York, NY: Perseus; 2006 [Google Scholar]
- 44.Soss J. Lessons of welfare: policy design, political learning, and political action. Am Polit Sci Rev. 1999;93(2):363–380 [Google Scholar]
- 45.Bensonsmith D. Jezebels, matriarchs, and welfare queens: the Moynihan report of 1965 and the social construction of African-American women in welfare policy. : Schneider A, Ingram H, Deserving and Entitled: Social Constructions and Public Policy. Albany, NY: State University of New York Press; 2005:243–260 [Google Scholar]
- 46.Soss J, Fording R, Schram S. The color of devolution: race, federalism, and the politics of social control. Am J Pol Sci. 2008;52(3):536–553 [Google Scholar]
- 47.Fording R. The political response to black insurgency: a critical test of competing theories of the state. Am Polit Sci Rev. 2001;95(1):115–131 [Google Scholar]
- 48.Fording R. Laboratories of democracy or symbolic politics? The racial origins of welfare reform. : Schram S, Soss J, Fording R, Race and the Politics of Welfare Reform. Ann Arbor, MI: University of Michigan Press; 2003:72–100 [Google Scholar]
- 49.Fox C. The changing color of welfare? How whites’ attitudes toward Latinos influence support for welfare. Am J Sociol. 2004;110(3):580–625 [Google Scholar]
- 50.Wright G. Racism and welfare policy in America. Soc Sci Q. 1976;57(1):718–730 [Google Scholar]
- 51.Digest of Alcohol-Highway Safety Related Legislation. Washington, DC: National Highway Traffic Safety Administration; 2002 [Google Scholar]
- 52.Centers for Disease Control and Prevention. State Tobacco Activities Tracking and Evaluation (STATE) System. Available at: http://apps.nccd.cdc.gov/statesystem/Default/Default.aspx. Accessed May 30, 2012.
- 53.National Institute on Alcohol Abuse and Alcoholism. Alcohol Policy Information System. Available at: http://www.alcoholpolicy.niaaa.nih.gov. Accessed May 30, 2102.
- 54.Carpenter CS, Stehr M. The effects of mandatory seatbelt laws on seatbelt use, motor vehicle fatalities, and crash-related injuries among youths. J Health Econ. 2008;27(3):642–662 [DOI] [PubMed] [Google Scholar]
- 55.Voas RB, Tippetts AS, Fell JC. Assessing the effectiveness of minimum legal drinking age and zero tolerance laws in the United States. Accid Anal Prev. 2003;35(4):579–587 [DOI] [PubMed] [Google Scholar]
- 56.Wagenaar AC, Toomey TL. Effects of minimum drinking age laws: review and analyses of the literature from 1960 to 2000. J Stud Alcohol Suppl. 2002;14:206–225 [DOI] [PubMed] [Google Scholar]
- 57.Ringwalt CL, Paschall MJ. The utility of keg registration laws: a cross-sectional study. J Adolesc Health. 2011;48(1):106–108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wagenaar A, Harwood E, Silianoff C. Measuring public policy: the case of beer keg registration laws. Eval Program Plann. 2005;28(4):359–367 [Google Scholar]
- 59.Ruhm CJ. Alcohol policies and highway vehicle fatalities. J Health Econ. 1996;15(4):435–454 [DOI] [PubMed] [Google Scholar]
- 60.Wagenaar AC, Salois MJ, Komro KA. Effects of beverage alcohol price and tax levels on drinking: a meta-analysis of 1003 estimates from 112 studies. Addiction. 2009;104(2):179–190 [DOI] [PubMed] [Google Scholar]
- 61.Dills AK. Social host liability for minors and underage drunk-driving accidents. J Health Econ. 2010;29(2):241–249 [DOI] [PubMed] [Google Scholar]
- 62.Wagenaar AC. Liability of commercial and social hosts for alcohol-related injuries: a national survey of accountability norms and judgments. Public Opin Q. 2001;65(3):344–368 [DOI] [PubMed] [Google Scholar]
- 63.O’Malley PM, Wagenaar AC. Effects of minimum drinking age laws on alcohol use, related behaviors and traffic crash involvement among American youth: 1976–1987. J Stud Alcohol. 1991;52(5):478–491 [DOI] [PubMed] [Google Scholar]
- 64.National Highway Transportation Safety Administration National Survey of Drinking and Driving Attitudes and Behaviors: 2008. Washington, DC: US Dept of Transportation; 2010 [Google Scholar]
- 65.Beer Institute. Brewers’ almanac. Available at: http://www.beerinstitute.org/statistics.asp?bid=200. Accessed May 30, 2012.
- 66.Nelson TF, Naimi TS, Brewer RD, Wechsler H. The state sets the rate: the relationship among state-specific college binge drinking, state binge drinking rates, and selected state alcohol control policies. Am J Public Health. 2005;95(3):441–446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wagenaar A, Maldonado-Molina M, Ma L, Tobler A, Komro K. Effects of Legal BAC Limits on Fatal Crash Involvement. J Safety Res. 2007;38(5):493–499 [DOI] [PubMed] [Google Scholar]
- 68.Grossman M, Kaestner R, Markowitz S. An investigation of the effects of alcohol policies on youth STDs. Adv Health Econ Health Serv Res. 2005;16:229–256 [PubMed] [Google Scholar]
- 69.Baum HM, Wells JK, Lund AK. Motor vehicle crash fatalities in the second year of 65 MPH speed limits. J Safety Res. 1990;21(1):1–8 [Google Scholar]
- 70.Baum HM, Wells JK, Lund AK. The fatality consequences of the 65 mph speed limits, 1989. J Safety Res. 1991;22(4):171–177 [Google Scholar]
- 71.Farmer C, Retting R, Lund AK. Effect of 1996 Speed Limit Changes on Motor Vehicle Occupant Fatalities. Arlington, VA: Insurance Institute for Highway Safety; 1997 [Google Scholar]
- 72.Grabowski DC, Morrisey MA. The effect of state regulations on motor vehicle fatalities for younger and older drivers: a review and analysis. Milbank Q. 2001;79(4):517–545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Wagenaar AC, Streff FM, Schultz RH. Effects of the 65 mph speed limit on injury morbidity and mortality. Accid Anal Prev. 1990;22(6):571–585 [DOI] [PubMed] [Google Scholar]
- 74.Pressley JC, Benedicto CB, Trieu L, Kendig T, Barlow B. Motor vehicle injury, mortality, and hospital charges by strength of graduated driver licensing laws in 36 states. J Trauma. 2009;67(suppl 1):S43–S53 [DOI] [PubMed] [Google Scholar]
- 75.Vanlaar W, Mayhew D, Marcoux K, Wets G, Brijs T, Shope J. An evaluation of graduated driver licensing programs in North America using a meta-analytic approach. Accid Anal Prev. 2009;41(5):1104–1111 [DOI] [PubMed] [Google Scholar]
- 76.Insurance Institute for Highway Safety. State helmet law history. Available at: http://www.iihs.org/laws/helmet_history.html. Accessed May 30, 2012.
- 77.Insurance Institute for Highway Safety. Laws and regulations. Available at: http://www.iihs.org/laws. Accessed May 30, 2012.
- 78.Stark MJ, Rohde K, Maher JEet al. The impact of clean indoor air exemptions and preemption policies on the prevalence of a tobacco-specific lung carcinogen among nonsmoking bar and restaurant workers. Am J Public Health. 2007;97(8):1457–1463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.McMullen KM, Brownson RC, Luke D, Chriqui J. Strength of clean indoor air laws and smoking related outcomes in the USA. Tob Control. 2005;14(1):43–48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.The Tax Burden on Tobacco. Washington, DC: Tobacco Institute; 1997 [Google Scholar]
- 81.National Cancer Institute. State Cancer Legislative Database. Available at: http://www.scld-nci.net. Accessed May 30, 2012.
- 82.Rosengart M, Cummings P, Nathens A, Heagerty P, Maier R, Rivara F. An evaluation of state firearm regulations and homicide and suicide death rates. Inj Prev. 2005;11(2):77–83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ludwig J, Cook PJ. Homicide and suicide rates associated with implementation of the Brady Handgun Violence Prevention Act. JAMA. 2000;284(5):585–591 [DOI] [PubMed] [Google Scholar]
- 84.The Brady Campaign to Prevent Gun Violence. State report cards. Available: http://www.stategunlaws.org/ 1996-2007. Accessed January 3, 2008.
- 85.Bureau of Alcohol Tobacco and Firearms State Laws and Published Ordinances—Firearms. 23rd ed Washington, DC: US Dept of the Treasury; 2007 [Google Scholar]
- 86.Open Society Institute. Gun control in the United States. Available at: http://www.soros.org/reports/gun-control-united-states. Accessed May 30, 2012.
- 87.Briggs NC, Schlundt DG, Levine RS, Goldzweig IA, Stinson JN, Warren RC. Seat belt law enforcement and racial disparities in seat belt use. Am J Prev Med. 2006;31(2):135–141 [DOI] [PubMed] [Google Scholar]
- 88.Elliott MR, Kallan MJ, Durbin DR, Winston FK. Effectiveness of child safety seats vs seat belts in reducing risk for death in children in passenger vehicle crashes. Arch Pediatr Adolesc Med. 2006;160(6):617–621 [DOI] [PubMed] [Google Scholar]
- 89.Dee TS. Motorcycle helmets and traffic safety. J Health Econ. 2009;28(2):398–412 [DOI] [PubMed] [Google Scholar]
- 90.Voas RB, Fell JC, Tippetts AS, Blackman K, Nichols JL. Impact of primary safety belt laws on alcohol-related front-seat occupant fatalities: five case studies. Traffic Inj Prev. 2007;8(3):232–243 [DOI] [PubMed] [Google Scholar]
- 91.Houston DJ, Richardson LE., Jr Safety belt use and the switch to primary enforcement, 1991–2003. Am J Public Health. 2006;96(11):1949–1954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Whetten-Goldstein K, Sloan FA, Stout E, Liang L. Civil liability, criminal law, and other policies and alcohol-related motor vehicle fatalities in the United States: 1984–1995. Accid Anal Prev. 2000;32(6):723–733 [DOI] [PubMed] [Google Scholar]
- 93.Insurance Institute for Highway Safety. Safety belt use laws. Available at: http://www.iihs.org/laws/safetybeltuse.aspx. Accessed May 30, 2012.
- 94.Williams AF, Lund AK. Seat belt use laws and occupant crash protection in the United States. Am J Public Health. 1986;76(12):1438–1442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Cohen A, Einav L. The effects of mandatory seat belt laws on driving behavior and traffic fatalities. Rev Econ Stat. 2003;85(4):828–843 [Google Scholar]
- 96.Brady Campaign to Prevent Gun Violence. State scorecard. Available at: http://www.bradycampaign.org/stategunlaws. Accessed May 30, 2012.
- 97.Insurance Institute for Highway Safety. Safety belt and child restraint laws. Available at: http://www.iihs.org/laws/mapchildrestraintagerequirements.aspx. Accessed May 30, 2012.
- 98.LaFond C, Toomey TL, Rothstein C, Manning W, Wagenaar AC. Policy evaluation research: measuring the independent variables. Eval Rev. 2000;24(1):92–101 [DOI] [PubMed] [Google Scholar]
- 99.True J, Jones B, Baumgartner F. Punctuated-equilibrium theory: explaining stability and change in public policymaking. : Sabatier P, Theories of the Policy Process. 2nd ed Boulder, CO: Westview Press; 2007:155–187 [Google Scholar]
- 100.Soss J, Schram S, Vartanian T, O’Brien E. Setting the terms of relief: explaining state policy choices in the devolution revolution. Am J Pol Sci. 2001;45(2):378–395 [Google Scholar]
- 101.Barrilleaux C, Holbrook T, Langer L. Electoral competition, legislative balance, and American state welfare policy. Am J Pol Sci. 2002;46(2):415–427 [Google Scholar]
- 102.Sapat A. Devolution and innovation: the adoption of state environmental policy innovations by administrative agencies. Public Adm Rev. 2004;64(2):141–151 [Google Scholar]
- 103.Berry W, Fording R, Ringquist E, Hanson R, Klarner C. Measuring citizen and government ideology in the U.S. states: a re-appraisal. State Polit Policy Q. 2010;10(2):117–135 [Google Scholar]
- 104.Grossback LJ, Nicholson-Crotty S, Peterson DAM. Ideology and learning in policy diffusion. Am Polit Res. 2004;32(5):521–545 [Google Scholar]
- 105.Hatzenbuehler ML, Keyes KM, Hasin DS. State-level policies and psychiatric morbidity in lesbian, gay, and bisexual populations. Am J Public Health. 2009;99(12):2275–2281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Ludwig J, Cook PI. Evaluating Gun Policy: Effects on Crime and Violence. Washington, DC: Brookings Institution; 2003 [Google Scholar]
- 107.Miller EA. State health policy making determinants, theory, and methods: a synthesis. Soc Sci Med. 2005;61(12):2639–2657 [DOI] [PubMed] [Google Scholar]
- 108.Lowry WR. Policy reversal and changing politics: state governments and dam removals. State Polit Policy Q. 2005;5(4):394–419 [Google Scholar]
- 109.Berry W, Fording R, Hanson R. Reassessing the ‘race to the bottom’ in state welfare policy. J Polit. 2003;65(2):327–349 [Google Scholar]
- 110.Miller JH, Page SE. Complex Adaptive Systems: An Introduction to Computational Methods of Social Life. Princeton, NJ: Princeton University Press; 2007 [Google Scholar]
- 111.Mabry PL, Marcus SE, Clark PI, Leischow SJ, Mendez D. Systems science: a revolution in public health policy research. Am J Public Health. 2010;100(7):1161–1163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Sabatier PA, Jenkins-Smith HC, Policy Change and Learning: An Advocacy Coalition Approach. Boulder, CO: Westview Press; 1993 [Google Scholar]
- 113.Shipan CR, Volden C. Bottom-up federalism: the diffusion of antismoking policies from U.S. cities to states. Am J Pol Sci. 2006;50(4):825–843 [Google Scholar]