In 1969, the federal government first made a specific appeal to food companies to lower sodium levels in their products as a means to reduce population sodium intake and thus prevent disease.1 In the four decades since, the evidence has only grown stronger that excess sodium consumption raises blood pressure, which increases the risk for cardiovascular disease and mortality.2
Nonetheless, mean sodium intake in the United States today remains more than twice the recommended daily limit for half of all adults. 3 Reducing the average intake by 1200 milligrams per day would save up to an estimated 92 000 lives and up to $24 billion in health care costs annually, and would thus be one of the most effective steps this country could take to promote health.4
Why have we failed to make progress on salt reduction? Despite the US government’s early calls for food industry response to the problem, since then government action has relied heavily on public education. The National Institutes of Health’s High Blood Pressure Education Program, the Department of Health and Human Services’ and US Department of Agriculture’s (USDA) Dietary Guidelines for Americans’ recommendations on limiting sodium intake, and the US Food and Drug Administration’s (FDA’s) mandated labeling of sodium content on packaged foods are all examples of major federal efforts intended to address sodium intake through increased consumer awareness. Still, without processed food reformulation, these efforts are doomed to fail. In fact, individuals have little control over their sodium intake. Only about one tenth of total sodium consumed is added during cooking or at the table. The vast majority, 77%, is already in packaged and restaurant foods at the time of purchase. For individuals to reduce sodium intake meaningfully requires diligent attention to packaged food labels when shopping and knowledge of the sodium content of menu items before ordering in restaurants—a nearly impossible task to sustain.
In 2009, an Institute of Medicine (IOM) Committee was convened and tasked with recommending strategies to lower sodium intake in the US. The Committee’s primary recommendation: reduce sodium in the food supply through federal regulation of the amount allowed in packaged and standardized restaurant foods. The FDA has this authority. However because FDA rule-making can take years, the IOM Committee also endorsed the continuation of existing voluntary efforts on coordinated industry sodium reductions and cited specifically the National Salt Reduction Initiative (NSRI).5
THE NATIONAL SALT REDUCTION INITIATIVE
Established in 2008, the NSRI is a partnership of now more than 80 local and state health authorities and national organizations, including the American Heart Association and the American Medical Association. The NSRI aims to reduce the sodium content of processed foods gradually by 25% over five years, which would reduce sodium intake by about 20%.
Although it was initiated and is coordinated by the New York City Health Department, the NSRI is a true nationwide effort launched in response to federal government failure to reduce excess sodium in our food supply. Features that set the NSRI apart from earlier US government calls for voluntary industry reductions include the introduction of a surveillance mechanism sensitive enough to monitor changes in food sodium content and population intake within the initiative’s time frame; food industry involvement in setting feasible yet ambitious targets; and a framework to make targets, commitments, and monitoring of progress public.
While the NSRI is the first of its kind in the United States, its inspiration was the United Kingdom Food Standards Agency’s salt campaign. Using a framework similar to that since adopted by the NSRI, the United Kingdom complemented traditional public education campaigns with defined packaged food salt reduction targets, and announced their first voluntary sodium reduction commitments from industry in 2006. It worked. Daily mean population salt intake in that country fell from 3800 milligrams in 2001 to 3240 milligrams in 2011.
INITIATIVE MONITORING AND TARGET SETTING
The NSRI commitment to target setting and monitoring industry progress toward achievement of these targets required the development of two unique databases because existing US food databases were insufficient. The USDA’s National Nutrient Database for Standard Reference is used extensively for nutritional research and is the basis for most US food composition databases; however, for many items information is not available by brand, and it is not updated frequently enough to track industry reformulation.6 Furthermore, the NSRI needed to know the sales volume of those products because large reductions in the sodium content of products with relatively low sales likely would have little influence on population intake, whereas modest reductions in high volume sales products could have remarkable impact.
The NSRI Packaged Food Database was created by linking national sales and nutrition information to fill this need. Preliminary food categories, such as “breads and rolls” and “canned soup,” were identified and nutrition label information was linked for products that accounted for the top 80% of sales in each category. Similarly, the NSRI Restaurant Food Database was created, which includes publicly available nutrition data based on available information from the fifty largest quick-service restaurants, merged with market share data.
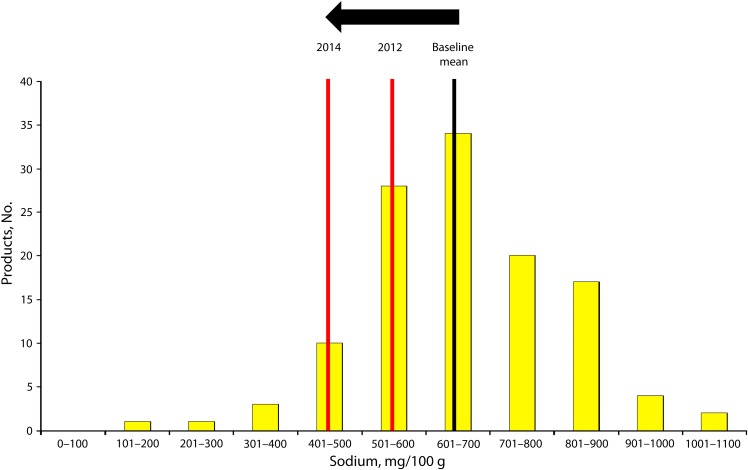
The NSRI developed sodium targets for the years 2012 and 2014 for 62 packaged food and 25 restaurant food categories through an iterative process with the food industry that included a review of the range and distribution of existing sodium levels within categories and consideration of the challenges of sodium reduction in each category (Figure 1). Most of the targets are already being met by one or more widely consumed products. Once established, the NSRI asked food companies to publicly commit to meeting targets and the commitments are posted online.7 A company commitment to a packaged food category target indicates that a company’s overall sales-weighted mean sodium level will meet the relevant category target, even if some individual products do not.
FIGURE 1—
Distribution of sodium levels in food products within a single category, with reduction targets for 2012 and 2014.
Note. The arrow indicates the expected shift in the category mean sodium level from the current baseline to the National Salt Reduction Initiative targets. Repeated over many food categories, this approach aims to shift the distribution of the food supply. Data are for illustration only.
For restaurants, in addition to the food category targets, a maximum sodium level target was established for all items. Restaurants prepare food in servings as intended to be consumed, and 17% of items in the restaurant database contained more than 1500 milligrams of sodium, the recommended daily limit that applies to about half of all adults.
To monitor sodium consumption, in 2010 the New York City Department of Health and Mental Hygiene conducted the first US population survey of sodium intake through 24-hour urine collection and analysis. Based on preliminary results from a representative sample of more than 1700 adult New Yorkers, mean sodium intake was 3150 milligrams per day. The agency plans to repeat this study after sodium levels in foods have been reduced.
THE POTENTIAL OF THE INITIATIVE AND THE CHALLENGES AHEAD
The NSRI has been remarkable in engaging a large, important, and diverse segment of the US food industry around a single public health goal. As of July 2011, commitments to meeting sodium reduction targets were made by 28 companies representing the complexity of the food industry, from superstores (e.g., Target Corporation) to grocery stores (e.g., Delhaize America), from family owned (e.g., Goya) to transnational corporations (e.g., Kraft Foods), and from restaurant chains (e.g., Starbucks) to restaurant suppliers (e.g., McCain Foods). Combined, commitments have been made in over half of all packaged and restaurant food categories.
Creating the NSRI databases highlighted an important public health need: comprehensive, up-to-date, publicly accessible, national food nutrition databases that include packaged and restaurant foods. The federal government is responsible for assuring a safe food supply, and that requires careful monitoring of the food supply’s nutrient balance. A federal requirement for regular electronic reporting by industry of publicly available nutrition information on their products would greatly simplify creation of this database. The government would be free to place these data in the public domain, facilitating transparency and informed response by government and industry and providing a rich source of information for researchers and consumers.
Even with its early accomplishments, the NSRI’s success is far from guaranteed. It is unlikely that the current number of company commitments will substantially alter the sodium composition of our nation’s food supply. The voluntary nature of the initiative relies on individual company motivation to engage. While we commend the 28 companies that have committed to NSRI targets, achieving broad-scale reductions will require commitments from many more food manufacturers and restaurants. The flexibility afforded by the NSRI framework, which allows companies to determine how sodium will be reduced within food categories, is, in our opinion, an effective way to spark industry creativity while assuring progress. Still, if this process does not lead to meaningful industry-wide reductions, it justifies the call for regulation recommended by the IOM committee.
The IOM committee was right to encourage voluntary coordinated efforts as an interim strategy. To date, the federal government has yet to take action on the IOM’s recommendation for regulation of sodium levels in processed food, leaving little besides the NSRI to address this health imperative. In the United Kingdom, the national government was central to encouraging structured voluntary industry reductions and we believe the US federal government can play a crucial role here. The US government and the food industry should broadly endorse and join the NSRI effort now to reduce sodium consumption and prevent tens of thousands of needless deaths.
Acknowledgments
We would like to thank Christine J. Curtis and Jenifer Clapp for their comments on this article, along with Lynn Silver, Stella Yi, Laura Cobb, and our National Salt Reduction Initiative partners who have contributed to the development, implementation and leadership of this effort.
References
- 1.White House Conference on Food, Nutrition and Health Final Report: Establishing guidelines for the nutrition of vulnerable groups (with special reference to the poor). Available at: http://www.nns.nih.gov/1969/full_report/White_House_Report2_S2.pdf. Accessed December 23, 2011
- 2.US Department of Agriculture and U.S. Department of Health and Human Services Report of the Dietary Guidelines Advisory Committee on the Dietary Guidelines for Americans, 2010. Available at: http://www.cnpp.usda.gov/Publications/DietaryGuidelines/2010/DGAC/Report/2010DGACReport-camera-ready-Jan11-11.pdf. Accessed May 1, 2010
- 3.US Department of Agriculture and US Department of Health and Human Services Dietary Guidelines for Americans, 2010. 7th Edition, Washington, DC: US Government Printing Office, December 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bibbins-Domingo K, Chertow GM, Coxson PGet al. Projected effect of dietary salt reductions on future cardiovascular disease. N Engl J Med. 2010;362(7):90–599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.IOM (Institute of Medicine) Strategies to Reduce Sodium Intake in the United States. Washington, DC: The National Academies Press; 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Merritt RK. Sodium Reduction: An Emerging Issue for Heart Disease and Stroke Surveillance. National Conference on Health Statistics, 2010. Available at: http://www.cdc.gov/nchs/ppt/nchs2010/45_Merritt.pptx. Accessed June 15, 2012 [Google Scholar]
- 7.NSRI Corporate Commitments and Comments New York City Department of Health and Mental Hygiene. Available at: http://www.nyc.gov/html/doh/downloads/pdf/cardio/cardio-salt-nsri-commitments.pdf. Accessed January 10, 2012