Abstract
Objective
To explore associations between specific interpersonal constructs and the developmental progression of behaviors leading to binge eating disorder (BED).
Method
Eighty-four consecutively evaluated, treatment-seeking obese (BMI ≥ 30) men and women with BED were assessed with structured diagnostic and clinical interviews and completed a battery of established measures to assess the current and developmental eating- and weight-related variables as well as interpersonal functioning.
Results
Using the interpersonal circumplex structural summary method, amplitude, elevation, the affiliation dimension, and the quadratic coefficient for the dominance dimension were associated with eating and weight-related developmental variables. The amplitude coefficient and more extreme interpersonal problems on the dominance dimension (quadratic)—i.e., problems with being extremely high (domineering) or low in dominance (submissive)—were significantly associated with ayounger age at onset of binge eating, BED, and overweight as well as accounted for significant variance in age at binge eating, BED, and overweight onset. Greater interpersonal problems with having an overly affiliative interpersonal style were significantly associated with, and accounted for significant variance in, ayounger age at diet onset.
Discussion
Findings provide further support for the importance of interpersonal problems among adults with BED and converge with recent work highlighting the importance of specific types of interpersonal problems for understanding heterogeneity and different developmental trajectories of individuals with BED.
Binge eating disorder (BED) is defined bythe recurrent consumption of unusually large amounts of food in a discrete period of time with a sense of loss of control without inappropriate weight-compensatory (e.g., purging) behaviors. BED affects 2-3.5% of the population [1] and is strongly associated with obesity, weight-related medical problems, and heightened eating disorder and general psychopathology [1,2]. Relatively little is known about risk factors and the development of BED. In contrast to restraint models posited initially for bulimia nervosa, it appears that a sizeable proportion of patients with BED report an onset of binge eating prior to dieting[3,4].
Initial research has suggested that differences in the developmental trajectories—timing and sequence of binge eating onset—may reflect significant differences in etiological or maintenance factors for BED [4,5]. Research has found that when binge eating onset precedes dieting, individuals report a younger age at binge onset [3,5,6], a younger age at BED onset [7], a younger age when first overweight [7], more psychiatric problems, and more family members with psychological difficulties [5]. In contrast, Manwaring et al [3] found that those who dieted first reported more eating disorder pathology and higher rates of substance use disorders than those who binged first. Manwaring et al [3] did not find any differences between individuals who binged first versus those who dieted first on eating disorder risk factors, including mental health, physical health, environmental experiences, family weight and eating concerns, quality of parenting, and parental psychopathology.
Wilfley and colleagues [8]proposed an interpersonal model of binge eating, which specifies an etiological course of BED development. This model posits that interpersonal problems lead to low self-esteem and negative affect, which in turn lead to binge eating as a way of coping with the low self-esteem and negative affect. Preliminary research has supported various aspects ofWilfley’s interpersonal model[8,9].Cross-sectional studies have found that interpersonal problems are associated with disordered eating, including binge eating [10,11,12,13]. Elliott and colleagues [14] found that negative affect mediated the relation between interpersonal problems and binge eating in youth. In a longitudinal study, Stice and colleagues [15] found that problematic social interactions were associated with increased disordered eating in adolescent girls over the course of two years. Two controlled treatment trials found that interpersonal psychotherapy (IPT) effectively reduced binge frequency as well as decreased interpersonal problems suggesting that social interactions may mediate the relationship with binge eating [16,17].
The majority of research examining the development of BED psychopathology has typically employed a global assessment of interpersonal problems (interpersonal distress) with little exploration of the types of interpersonal problems (e.g., [9,14,16]).Furthermore, there is little research examining the role of interpersonal factors in the developmental course of BED. Fairburn et al [18] investigated risk factors associated with BED development and found that, compared to healthy controls, individuals with BED were more likely to report a history of sexual and physical abuse, bullying, parental criticism, parental neglect, low parental affection and maternal over protection. Stice and colleagues [15] found that perceptions of low peer social support were significantly associated with the development of binge eating in adolescent girls. Womble et al [19] found that a history of weight-related teasing was significantly associated with BED in a sample of 808 obese men and women. In contrast, in a four-year longitudinal study, Killen et al [20] found that interpersonal distrust was not significantly associated with the development of disordered eating in adolescent girls. Similarly, Paxton et al [21] did not find that friendship quality was associated with binge eating in a sample of 523 adolescent girls. No known studies have examined how specific interpersonal styles may contribute to the development of BED.
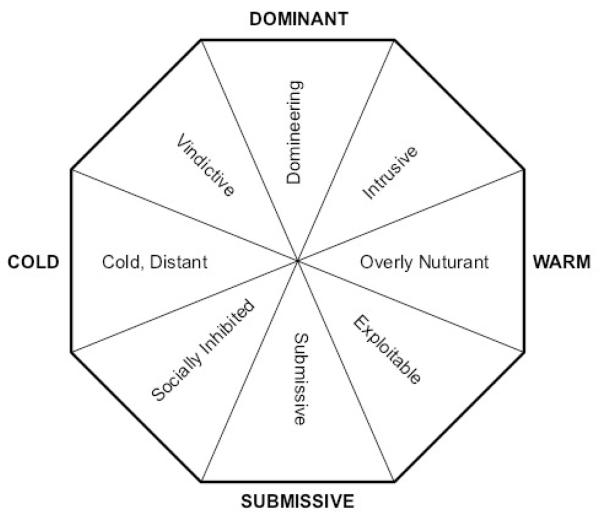
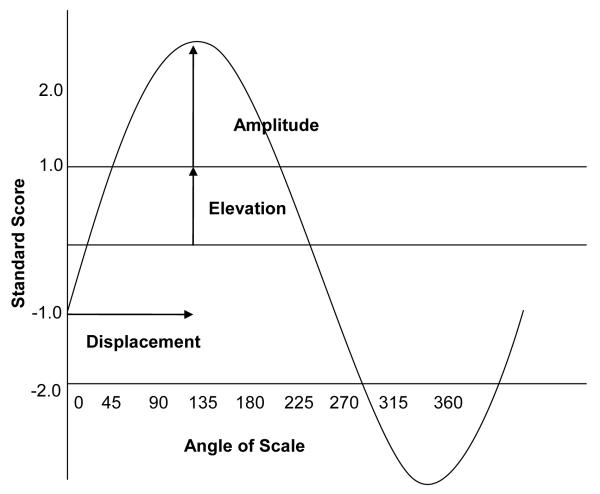
Examining specific interpersonal problems associated with the development of BED psychopathology may help to further refine the interpersonal model of BED as well as to identify specific risk and maintenance factors to address in prevention and treatment interventions. The Interpersonal Circumplex (IPC) model [22] (see Figures 1 and 2) may be particularly useful in elucidating interpersonal styles associated with the development of eating disorder pathology. The IPC is comprised of two orthogonal dimensions, dominance and affiliation. The dominance dimension ranges from dominant to submissive (e.g., controlling or demanding versus passive or submissive in relationships). The affiliation dimension ranges from warm to cold: “warm[ing] up to others too quickly, and [feeling] as though relationships are closer than perceived by others” [10] (p. 248) versus distancing oneself from others[23].Thus, the two orthogonal dimensions can be oriented in two-dimensional space with eight octants representing different blends of dominance and affiliation: dominant, dominant-warm, warm, submissive-warm, submissive, submissive-cold, cold, and dominant-cold (see Figure 1). Using interpersonal circumplex assessment measures also allows for the computation of an interpersonal profile using the structural summary approach[24,25,26]. This approach models an interpersonal profile of octant scores with a cosine-curve function. As Figure 2 shows, the parameters of this curve are its (a) angular displacement; (b) amplitude; and (c) elevation. The amplitude coefficient reflects the peakness of the individual’s profile and has been interpreted in some research as an indicator of interpersonal rigidity or maladaptive behaviors [24,25,27] (see Figure 2). The elevation coefficient refers to the general interpersonal distress an individual is experiencing. This approach also produces a score for each of the underlying dimensions (dominance and affiliation), which can be examined within quadratic functions to ascertain whether extremity on either end of a single dimension is associated with maladaptive outcomes.
Figure 1. Interpersonal Problems Circumplex and Eight Interpersonal Problem Octants.
Figure 2. Interpersonal Circumplex Structural Summary Model.
There is no known research examining associations between specific interpersonal constructs using the IPC model and the development of BED. However, there is some research exploring specific interpersonal constructs in eating disorder pathology. For example, Eldredge, Locke, and Horowitz[28] examined interpersonal octants in a sample of individuals with BED and found that there were fewer problems in the cold-dominant or vindictive octant in BED patients relative to psychiatric norms. Constantino & Smith-Hansen [27] found that interpersonal distress, interpersonal rigidity, and dominant and affiliative interpersonal styles were significantly associated with therapeutic alliance in the treatment of women with bulimia nervosa. Most recently, Ansell, Grilo, and White [29] tested an elaborated interpersonal model, examining the effect of specific interpersonal factors on binge eating and found that negative affect mediated the effect of low affiliation on binge eating. These earlier studies as well as Ansell et al.’s [29] findings demonstrate the relevance of examining the parameters of interpersonal functioning among individuals with binge eating. These findings highlight the need to investigate associations between specific interpersonal constructs and BED development.
Research exploring associations between specific interpersonal problems using the IPC model and the timing and sequencing of BED development may shed light on hypotheses posited by Reiger’s [9] IPT-ED model. Reiger’s [9] model proposes that individuals are more likely to develop disordered eating behaviors during adolescence and early adulthood because during this period of development self-esteem becomes more influenced by peer social approval (versus parental approval) and physical appearance is a prominent influence on peer social approval. That is, disordered eating may develop as a way to achieve peer approval and reduce negative affect.
The current study addresses a gap in the literature by examining interpersonal problems using the IPC model and its associations with the timing and sequencing of BED development. Further research is needed to examine factors potentially associated with these developmental aspects of binge eating (and dieting) to inform our conceptual models regarding the etiology, maintenance, and treatment for binge eating and other disordered eating behaviors. The current investigation explores the developmental trajectory of binge eating, dieting, and obesity onset and their relation to interpersonal functioning in BED. We hypothesized that greater interpersonal distress and interpersonal rigidity would be associated with earlier onsets of binge eating, dieting, and overweight. Associations between interpersonal styles from the IPC model and developmental histories of dieting, binge eating and overweight were explored.
METHODS
Participants
Participants were 84 (29 men, 55 women) consecutively evaluated, treatment-seeking obese (BMI ≥ 30) adults who met full DSM-IV research diagnostic criteria for BED. Participants were recruited via newspaper advertisements to participate in a treatment research study to help people “stop binge eating” and “lose weight” at a medical school based specialty clinic. Participants’ mean age was 47.3 (SD=8.1) and mean BMI was 40.4 (SD=6.8). Participants were 15.5% Black, 78.6% White, 4.8% Hispanic, and 1.2% classified as “other.”Educationally, 80.9% (n=68) reported at least some college. Participants provided informed written consent prior to study procedures, which had received full review and approval by the Yale Human Investigation Committee.
Procedures and Assessments
BED diagnosis and age at BED onset were based on the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I/P)[30] and the diagnosis was confirmed with findings from the Eating Disorder Examination interview (EDE) [31]. Participants completed a battery of measures including the Questionnaire for Eating and Weight Patterns-Revised (QEWP) [32], the Inventory of Interpersonal Problems-Short Circumplex (IIP-SC) [23,33] as well as a weight and eating history interview, which assessed the onset age of binge eating and dieting. Participants’ height and weight were measured at intake assessment using a medical balance beam scale.
Eating Disorder Examination interview (EDE) [31]
The EDE is a well-established investigator-based interview method for assessing eating disorder psychopathology[34,35] with established reliability[36]. The EDE focuses primarily on the previous 28 days, except for diagnostic items which are rated according to the duration stipulations in the DSM-IV.
The developmental trajectory variables in this study are age at first binge, age at BED onset, age at dieting onset, and age at overweight onset. These variables were assessed with the following self-report measure and interview. The Questionnaire for Eating and Weight Patterns-Revised (QEWP-R)[32] is a 28-item measure that assesses participants’ age at first binge and age at overweight onset (10 pounds overweight as a child, 15 pounds overweight as an adult). The Weight and Eating History Interview (WEH), developed for the current research study, is a structured clinical interview that assesses current and historical obesity-related variables of interest. Age at dieting onset was assessed with the following question: “At what age do you remember first going on a diet?”Individuals were categorized as either binge-first or diet-first. Binge-first refers to participants whose binge eating onset preceded their dieting onset. Diet-first refers to participants whose dieting onset preceded their binge eating onset. Participants who reported same-age binge and diet onset (n=6; 7.1%) were excluded from these analyses.
Inventory of Interpersonal Problems-Short Circumplex (IIP-SC; see Figure 1) [23,33]
The IIP-SC is a32-item measure, with each item rated on a scale from 0-not at all to 4-extremely, that assesses interpersonal problems within eight domains (dominant, dominant-warm, warm, submissive-warm, submissive, submissive-cold, cold, and dominant-cold) within the framework of the Interpersonal Circumplex (IPC). In the current sample, Cronbach alphas for the eight interpersonal problem domains ranged from .62 to .88. Using the structural summary method for analyzing IPC data[24,25], the angular location, amplitude, and elevation were computed for each individual. In addition dimensional scores on dominance and affiliation were computed. We also explored whether extremity on a specific interpersonal style was important by computing quadratic variables for each interpersonal dimensions. That is, the quadratic variable, dominance × dominance (dom × dom), represents extremity in dominance (extremely high or low dominance). Similarly, affiliation × affiliation (affil × affil) represents extremity in affiliation (either high or low affiliation).
Statistical Analyses
Pearson’s bivariate correlations assessed associations between interpersonal variables and the developmental variables (e.g., age of onset variables).Based on which variables were significantly correlated, a series of hierarchical regressions explored whether interpersonal styles and extremity on a specific interpersonal style accounted for significant variance in age of first binge, BED, diet, or overweight onset. Analyses of variance (ANOVAs) assessed differences between individuals with a binge-first versus diet-first onset on interpersonal distress, interpersonal rigidity, interpersonal styles, and extremity of specific interpersonal styles.
RESULTS
Participants’ mean age at their first binge was 23.4 years old (SD=12.9), and their mean age at BED onset (full criteria for BED diagnosis) was 28.2 years old (SD=13.7). Participants’ mean age at diet onset was 20.2 years old (SD=10.3), and their mean age at overweight onset was 17.5 years old (SD=11.1).There were no significant gender differences on any of the interpersonal variables, BMI, or age at overweight onset. Women reported a younger age at first binge (women: M=20.9, SD=11.4; men: M=28.4, SD=14.6; F(1,77)=6.175, p=0.015), BED onset (women: M=25.6, SD=13.4; men: M=32.8, SD=13.2; F(1,77)=5.206, p=0.025), and dieting onset (women: M=16.6, SD=8.0; men: M=26.9, SD=11.0; F(1,83)=23.691, p≤0.0001) than men. Participants’ current BMIand weekly mean binge frequency over the past 6 months were not significantly associated with any interpersonal variables.
Table 1 summarizes the Pearson bivariate correlations between the developmental trajectory variables and the interpersonal variables—elevation (global interpersonal distress), amplitude (interpersonal rigidity), and interpersonal dimensions (linear and quadratic: dominance, affiliation). Elevation, or the global interpersonal distress, was significantly and negatively correlated with participants’ age at first binge. Thus, participants who reported more interpersonal problems overall reported a younger age at their first binge. Amplitude and extremity as measured by the quadratic dominance dimension were significantly and negatively correlated with participants’ age at their first binge, age at BED onset, and age at overweight onset. Thus, participants who reported a more narrow range of interpersonal problems and more extreme interpersonal problems with being either overly dominant or overly submissive in interpersonal interactions reported a younger age at first binge, a younger age when met full criteria for BED and a younger age when first became overweight. Affiliation was significantly and negatively correlated with participants’ age at dieting onset. More interpersonal problems with being overly affiliative was significantly associated with a younger age at dieting onset.
Table 1. Correlations between Developmental Trajectory Variables and Interpersonal Profile Variables.
| Age First Binge |
Age BED Onset |
Age Diet Onset |
Age Overweight Onset |
|
|---|---|---|---|---|
| Amplitude | −0.29* | −0.24* | −0.19 | −0.25* |
| Elevation | −0.31** | −0.19 | −0.15 | −0.20 |
| Dominance | 0.03 | 0.03 | 0.10 | 0.10 |
| Affiliation | −0.16 | −0.06 | −0.22* | −0.07 |
Note. Dom=dominant interpersonal problems. Affil=affiliative interpersonal problems.
p≤0.05
p≤0.01.
Table 2 summarizes the hierarchical regressions examining whether interpersonal styles and extremity (quadratic) of an interpersonal style accounted for significant variance in age at first binge, BED, diet, and overweight onset. Extremity on either end of the dominance dimension was significantly associated with age at first binge, age at BED onset, as well as age at overweight onset. That is, more extreme problems with either high dominance (overly assertive or hostile) or low dominance (overly submissive or passive) in interpersonal interactions was associated with a younger age at first binge, a younger age at meeting full BED criteria, and a younger age at first becoming overweight. In contrast, an overly affiliative interpersonal style was significantly associated with age at diet onset. That is, more problems with being overly affiliative in interpersonal interactions were associated with a younger age at dieting onset. Extremity on the affiliation dimension was not significant in any of the regressions.
Table 2. Hierarchical Regressions Examining Whether Interpersonal Dimensions Account for Variance in Developmental Trajectory Variables.
| Age at First Binge | ||||||
|---|---|---|---|---|---|---|
|
| ||||||
| Mean (SD) | Beta | t | AdjustedR2 | R2 Change | F Change | |
| Step 1 | ||||||
| Dominance | −0.09 (0.67) | 0.027 | 0.232 | −0.013 | 0.001 | 0.054 |
| Step 2 | 0.057 | 0.083 | 6.328* | |||
| Dom × Dom | 0.45 (0.74) | −0.313 | −2.516* | |||
|
| ||||||
| Age at BED Onset | ||||||
|
| ||||||
| Step 1 | −0.013 | 0.001 | 0.069 | |||
| Dominance | −0.06 (0.64) | 0.031 | 0.262 | |||
| Step 2 | 0.105 | 0.129 | 10.275** | |||
| Dom × Dom | 0.41 (0.65) | −0.378 | −3.205** | |||
|
| ||||||
| Age at Diet Onset | ||||||
|
| ||||||
| Step 1 | 0.058 | 0.083 | 3.296* | |||
| Dominance | −0.10 (0.67) | 0.065 | 0.572 | |||
| Affiliation | 0.12 (0.60) | −0.272 | −2.409* | |||
|
| ||||||
| Age at Overweight Onset | ||||||
|
| ||||||
| Step 1 | −0.004 | 0.011 | 0.750 | |||
| Dominance | −0.10 (0.69) | 0.104 | 0.866 | |||
| Step 2 | 0.044 | 0.060 | 4.416* | |||
| Dom × Dom | 0.48 (0.76) | −0.270 | −2.102* | |||
Note. Dom=dominant interpersonal style. Affil=affiliative interpersonal style. Dom × Dom=extremity on dominant dimension. Affil × Affil=extremity on affiliative dimension.
p≤0.05.
p≤0.01.
Table 3 summarizes the ANOVAs comparing participants whose binge eating onset preceded (binge-first) or followed (diet-first) their dieting onset on interpersonal variables. Individuals whose binge eating preceded their dieting reported greater global interpersonal distress, greater interpersonal rigidity, as well as more extremity on either end of the dominance dimension (more interpersonal problems with being overly dominant or overly submissive) compared to those whose dieting preceded their binge eating onset. Total IIP-SC mean scores for those with binge-first were M=40.7 (SD=18.7) and for those with diet-first were M=2.7 (SD=17.2).
Table 3. Binge-First versus Diet-First on Amplitude, Elevation, and Interpersonal Problems.
| Binge-First: Mean (SD) |
Diet-First: Mean (SD) |
F | P | |
|---|---|---|---|---|
| Amplitude | 0.97(0.57) | 0.52(0.36) | 13.012 | 0.001** |
| Elevation | 0.20(0.70) | −0.47(0.65) | 14.531 | 0.000** |
| Dominance | −0.11 (0.85) | 0.02 (0.38) | 0.555 | 0.459 |
| Affiliation | 0.20 (0.73) | 0.06 (0.50) | 0.773 | 0.383 |
| Dom × Dom | 0.71 (0.92) | 0.14 (0.19) | 10.311 | 0.002** |
| Affil × Affil | 0.56 (0.84) | 0.25 (0.46) | 3.218 | 0.078 |
Note. Dom=dominant interpersonal style. Affil=affiliative interpersonal style. Dom × Dom=extremity on dominant dimension. Affil × Affil=extremity on affiliative dimension. Binge-First=age at binge eating onset precedes age at dieting onset; Diet-First=age at dieting onset precedes age at binge eating onset.
p≤0.05.
p≤;0.01.
DISCUSSION
The current study explored associations between interpersonal problem profiles and the developmental trajectories of binge eating to elaborate on specific aspects of the interpersonal model of BED. Our primary findings revealed that individuals with greater interpersonal problems reported a younger age at their first binge. Individuals with a more narrow range or rigid interpersonal style (amplitude) as well as individuals with greater problems with being extremely dominant or submissive in interpersonal interactions (interpersonal extremity or quadratic) reported a younger age at their first binge, a younger age when first met full BED criteria, and a younger age at overweight onset. In contrast, being overly affiliative in interpersonal interactions was significantly associated with a younger age at dieting onset. Individuals with more global interpersonal distress (elevation), greater interpersonal rigidity (amplitude), and more interpersonal problems with being extremely submissive or dominant(quadratic) were more likely to have their binge eating onset precede their dieting onset. Furthermore, no interpersonal variable was significantly correlated with BMI and, therefore, BMI did not influence or confound our findings.
Binge eating onset was related to several aspects of the interpersonal profiles: interpersonal distress (elevation), interpersonal rigidity (amplitude), and extreme submissiveness or dominance (quadratic). Diagnostic onset of BED was related to interpersonal rigidity and extreme dominance or submissiveness extremity (quadratic). These findings suggest that individuals who have more problems with flexibility of interpersonal style across interpersonal contexts may be more likely to develop binge eating at a younger age. Individuals who develop binge eating at a younger age may also persist in relating with others in an ineffective interpersonal style and not change their interpersonal approach when it would be helpful and effective to do so. This seems to be particularly true for problems with being overly dominant or overly submissive—too assertive or not assertive enough in interpersonal interactions. It may be that, consistent with interpersonal theories on loss of control [8,9], these problematic interpersonal styles result in negative social evaluation leading to low self-esteem and emotion dysregulation and/or negative affect that trigger maladaptive eating patterns to cope with the negative affect. In addition, Reiger’s IPT-ED model [9] highlights cognitive dysfunction as an important construct associated with disordered eating development and proposes rejection sensitivity and sensitivity to negative self-evaluation as factors associated with cognitive dysfunction. Interpersonal rigidity may be associated with the construct of cognitive rigidity, which has been examined in individuals with anorexia nervosa [37,38]. Given our findings that interpersonal rigidity and interpersonal extremity of submissive or dominant behaviors are associated with disordered eating developmentas well as previous research indicating that individuals with anorexia nervosa tend to have more cognitive rigidity, interpersonal rigidity may be an important addition to the cognitive dysfunction construct within the IPT-ED model.
Interestingly, interpersonal rigidity and interpersonal distress were not associated with age at dieting onset. However, results revealed that a more affiliative interpersonal stylewas significantly correlated witha younger age at dieting onset. That is, although more global interpersonal distress may not contribute to a younger age at dieting onset, it appears that interpersonal problems with feeling too close to others may contribute to a younger age at dieting onset. It is possible that those who feel too close with others may begin dieting at a young age in order to gain social approval [9]. Conversely, individuals with younger age at dieting onset may be using dieting to cope with the negative affect associated with being too close and not setting appropriate boundaries with others. These findings may reflect attempts to diet to alter one’s shape in order to please others or as a means of coping with weight-related teasing as a child[39].
Greater amplitude in interpersonal problems, or interpersonal rigidity as it has been interpreted [27] was significantly correlated with a younger age at overweight onset. Although individuals with more overall interpersonal distress did not reporta younger age at overweight onset, those who reported more problems with being too dominant or too submissive in interpersonal interactions were more likely to report a younger age at overweight onset. It is possible that extreme dominance or submission in interpersonal interactions results in negative affect which leads to binge eating, or simply overeating, to cope with the negative affect and consequently becoming overweight at a younger age. In this sample, the mean age at becoming overweight was about 17.5 years old about 6 years younger than the mean age at binge onset (23.4 years old). Since this study was not prospective, it is not possible to draw temporal or causal inferences. However, perhaps being overweight at a young age results in specific negative interpersonal interactions (e.g., weight-related teasing) by peers and family members that, in the presence of a rigid and/or overly dominant or submissive interpersonal style, leads to lower self-esteem and/or negative effect and then binge eating to cope.
Individuals whose binge eating preceded dieting were characterized by greater interpersonal rigidity, higher overall interpersonal distress, and significantly more interpersonal problems in being overly dominant or overly submissive in interpersonal interactions than individuals whose dieting preceded binge eating. Our findings are consistent with previous research indicating that the sequencing of binge eating and dieting onset may reflect distinct pathways in BED development [4,5,6,7,40]. In a sample of women with BED, Manwaring et al [3] found that there were no significant differences in reported risk factors between those who binged first versus dieted first and concluded that these two developmental trajectories do not differ in etiology or risk factors. In contrast, we found significant interpersonal style differences between those who binged first versus dieted first; those whose binge eating preceded dieting were much more likely to report interpersonal distress, rigidity and extremity on the dominance dimension than those whose dieting preceded binge eating. These findings are consistent with the IPT-ED model proposing that interpersonal problems are associated with the etiology of disordered eating behaviors [9]. Perhaps the IPC model of interpersonal variables and the IIP-SC more accurately captures and measures interpersonal problems associated with disordered eating development than the RFI factors[3,18]. Furthermore, a recent family history study found that a parental history of substance use disorders was associated with binge eating onset preceding dieting onset [40] whereas Manwaring et al [3] found that those who dieted first were more likely to have a history of substance use disorders. These discrepancies highlight the need for more research to elucidate risk factors associated with different developmental trajectories.
Collectively, our findings regarding the timing of binge eating, BED, dieting, and overweight onset suggest that individuals who are engaging in persistent, yet ineffective interpersonal styles and, in particular, exhibiting interpersonal problems in the too warm and too dominant or too submissive domains overweight may be more at risk for binge eating and dieting at a younger age. Our findings that specific interpersonal problems are associated with younger ages at binge eating and dieting onset are consistent with Reiger’s [9] IPT-ED model, which posits that negative social evaluation during adolescence and early adulthood may be associated with the development of disordered eating behaviors. That is, specific interpersonal styles may be more likely to contribute to negative social evaluation from peers which results in low self-esteem and negative affect and triggers binge eating and/or dieting as a way of coping with the negative affect or as a way to obtain peer approval, which is strongly influenced by physical appearance during adolescence and early adulthood. Prospective research is needed to examine the timing and sequencing of interpersonal styles and disordered eating development.
There are several strengths and limitations to our studies. Strengths include the consecutive ascertainment of obese men and women with BED assessed by doctoral clinicians using reliable and validated structured interviews and associated measures. It is noteworthy that the current investigation employed a sophisticated analysis of specific interpersonal problem variables derived from the IPC model using the IIP-SC and is one of very few studies to investigate these specific interpersonal variables in the context of BED development. Generalizability to non-treatment-seeking obese persons with BED or to community samples of obese binge eaters is uncertain; it is possible, for example, that such groups may differ in their developmental trajectories and the severity of the interpersonal difficulties.
Our study was cross-sectional thus precluding any causal statements, which would require prospective and experimental manipulation designs. Retrospective recall of data regarding the onset of binge eating and obesity variables may be inaccurate or potentially biased. Previous studies of obese patients with BED have found that this patient group is reasonably accurate in their self-report of weight and height and that the degree of misreport (i.e., inaccuracy) is unrelated to demographic or clinical variables such as current BMI, eating disorder psychopathology, body image, or current distress[41,42]. Longitudinal studies, which can prospectively assess the developmental trajectory variables, will also allow for formal meditational analyses to test the hypothesized IIP mechanisms leading to binge eating and unhealthy dieting onset.
With these limitations in mind, our findings provide preliminary support for examining specific interpersonal variables with regard to the developmental progression of binge eating. Specifically, we found significant associations between interpersonal rigidity, overall distress, and specific interpersonal styles with younger onset of binge eating, dieting, and becoming overweight. These findings suggest the importance of specific interpersonal problems in the development of BED and shed light on potential developmental differences in this population. Research has established that there is considerable heterogeneity within diagnostic categories and interpersonal problems have been useful in eating disorders and other diagnostic categories for understanding this heterogeneity (e.g., [43]). The current study expands upon this prior research by looking at the etiology of a disorder and how differences in interpersonal problems may also be relevant to explaining diversity in developmental course of a disorder. Future research should continue to explore this heterogeneity in individuals with BED. Our findings also highlight the heterogeneity of this population and suggest more fine-grained understanding of interpersonal areas, which can be used to elaborate upon the interpersonal model as well as to enhance the use of IPT with this population [16,17]. These findings relate to Constantino and Smith-Hansen’s [27] findings that interpersonal rigidity moderated the therapeutic alliance at different points of treatment for bulimia nervosa. Future research could explore the effectiveness of tailoring a treatment approach to those high in interpersonal rigidity, perhaps in a fashion similar to recent promising developments emerging from the integration of cognitive remediation and flexibility for the treatment of anorexia nervosa (e.g., [37,38]). Lastly, our findings highlight the usefulness of the interpersonal circumplex to elucidate interpersonal problems in the context of psychiatric disorders, and our analyses may support a useful model for clinicians and researchers attempting to more deeply explore interpersonal problems in the development and maintenance of psychopathology to further refine prevention and treatment interventions.
Acknowledgements
This research was supported by grants from the National Institutes of Health (R01 DK49587, K24 DK070052, K08 DA029641).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Hudson JI, Hiripi E, Pope HG, Kessler RC. The prevalence and correlates of eating disorders in the NCS Replication. Biol Psychiatry. 2007;61:348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Grilo CM, Hrabosky JI, White MA, Allison KC, Stunkard AJ, Masheb RM. Overvaluation of weight and shape in binge eating disorder and overweight controls: Refinement of a diagnostic construct. AbnormPsychol. 2008;117:414–419. doi: 10.1037/0021-843X.117.2.414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Manwaring JL, Hilbert A, Wilfley DE, Pike KM, Fairburn CG, Dohm F-A, Striegel-Moore RH. Risk factors and patterns of onset in binge eating disorder. Int J Eat Disord. 2006;39:101–107. doi: 10.1002/eat.20208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Reas DL, Grilo CM. Timing and sequence of the onset of overweight, dieting, and binge eating in overweight patients with binge eating disorder. Int J Eat Disord. 2007;40:165–170. doi: 10.1002/eat.20353. [DOI] [PubMed] [Google Scholar]
- 5.Spurrell EB, Wilfley DE, Tanofsky MB, Brownell KD. Age of onset for binge eating: Are there different pathways to binge eating? Int J Eat Disord. 1997;21:55–65. doi: 10.1002/(sici)1098-108x(199701)21:1<55::aid-eat7>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 6.Abbott DW, DeZwaan M, Mussell MP, Raymond NC, Seim HC, Crow SJ, Crosby RD, Mitchell JE. Onset of binge eating and dieting in overweight women: Implications for etiology, associated features and treatment. J Psychosomatic Research. 1998;44:367–374. doi: 10.1016/s0022-3999(97)00261-4. [DOI] [PubMed] [Google Scholar]
- 7.Grilo CM, Masheb RM. Onset of dieting vs. binge eating in outpatients with binge eating disorder. Int J Obes Relat Metab Disord. 2000;24:404–409. doi: 10.1038/sj.ijo.0801171. [DOI] [PubMed] [Google Scholar]
- 8.Wilfley DE, MacKenzie KR, Welch RR, Ayres VE, Weissman MM. Interpersonal psychotherapy for group. Basic Books; New York, NY: 2000. [Google Scholar]
- 9.Rieger E, Van Buren DJ, Bishop M, Tanofsky-Kraff M, Welch R, Wilfley DE. An eating disorder-specific model of interpersonal psychotherapy (IPT-ED): Causal pathways and treatment implications. ClinPsychol Rev. 2010;30:400–410. doi: 10.1016/j.cpr.2010.02.001. [DOI] [PubMed] [Google Scholar]
- 10.Ambwani S, Hopwood CJ. The utility of considering interpersonal problems in the assessment of bulimic features. Eat Behav. 2009;10:247–253. doi: 10.1016/j.eatbeh.2009.07.007. [DOI] [PubMed] [Google Scholar]
- 11.Jackson T, Weiss KE, Lundquist JJ, Soderlind A. Sociotropy and perceptions of interpersonal relationships as predictors of eating disturbances among college women: Two prospective studies. J Genetic Psychol. 2005;166:346–359. doi: 10.3200/GNTP.166.3.346-360. [DOI] [PubMed] [Google Scholar]
- 12.Schutz HK, Paxton SJ. Friendship quality, body dissatisfaction, dieting, and disordered eating in adolescent girls. Br J ClinPsychol. 2007;46:67–83. doi: 10.1348/014466506x115993. [DOI] [PubMed] [Google Scholar]
- 13.Tanofsky-Kraff M, Wilfley DE, Spurrell EB. Impact of interpersonal and ego-related stress on restrained eaters. Int J Eat Disord. 2000;27:411–418. doi: 10.1002/(sici)1098-108x(200005)27:4<411::aid-eat5>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 14.Elliott CA, Tanofsky-Kraff M, Shomaker LB, Columbo KM, Wolkoff LE, Ranzenhofer LM, Yanovski JA. An examination of the interpersonal model of loss of control eating in children and adolescents. BRAT. 2009;48:424–428. doi: 10.1016/j.brat.2009.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stice E, Presnell K, Spangler D. Risk factors for binge eating onset in adolescent girls: A 2-year prospective investigation. Health Psychol. 2002;21:131–138. [PubMed] [Google Scholar]
- 16.Wilfley DE, Welch RR, Stein RI, Spurrell EB, Cohen LR, Saelens BE, Dounchis JZ, Frank MA, Wiseman CV, Matt GE. A randomized comparison of group cognitive-behavioral therapy and group interpersonal psychotherapy for the treatment of overweight individuals with binge-eating disorder. Arch Gen Psych. 2002;59:713–721. doi: 10.1001/archpsyc.59.8.713. [DOI] [PubMed] [Google Scholar]
- 17.Wilson GT, Wilfley DE, Agras WS, Bryson SW. Psychological treatments of binge eating disorder. Arch Gen Psych. 2010;67:94–101. doi: 10.1001/archgenpsychiatry.2009.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fairburn CG, Doll HA, Welch SL, Hay PJ, Davies BA, O’Connor ME. Risk factors for binge eating disorder:A community-based, case-control study. Arch Gen Psych. 1998;55:425–432. doi: 10.1001/archpsyc.55.5.425. [DOI] [PubMed] [Google Scholar]
- 19.Womble LG, Williamson DA, Martin CK, Zucker NL, Thaw JM, Netemeyer R, Lovejoy JC, Greenway FL. Psychosocial variables associated with binge eating in obese males and females. Int J Eat Disord. 2001;30:217–221. doi: 10.1002/eat.1076. [DOI] [PubMed] [Google Scholar]
- 20.Killen JD, Taylor CB, Hayward C, Haydel KF, Wilson DM, Hammer L, Kraemer H, Blair-Greiner A, Strachowski D. Weight concerns influence the development of eating disorders: A 4-year prospective study. J Consult ClinPsychol. 1996;64:936–940. doi: 10.1037//0022-006x.64.5.936. [DOI] [PubMed] [Google Scholar]
- 21.Paxton SK, Schutz HK, Wertheim EH, Muir SL. Friendship clique and peer influences on body image concerns, dietary restraint, extreme weight-loss behaviors, and binge eating in adolescent girls. J AbnormPsychol. 1999;108:255–266. doi: 10.1037//0021-843x.108.2.255. [DOI] [PubMed] [Google Scholar]
- 22.Pincus AL, Gurtman MB. Interpersonal theory and the interpersonal Circumplex: Evolving perspectives on normal and abnormal personality. In: Strach S, editor. Differentiating normal and abnormal personality. 2nd ed. Springer; New York: 2006. pp. 83–111. [Google Scholar]
- 23.Horowitz LM, Rosenberg SE, Baer BA, Ureno G, Villasenor VS. Inventory of interpersonal problems: Psychometric properties and clinical applications. J Consult ClinPsychol. 1988;56:885–892. doi: 10.1037//0022-006x.56.6.885. [DOI] [PubMed] [Google Scholar]
- 24.Ansell EB, Pincus AL. Interpersonal perceptions of the five-factor model of personality: An examination using the structural summary method for circumplex data. Multivariate Behav Res. 2004;39:167–201. doi: 10.1207/s15327906mbr3902_3. [DOI] [PubMed] [Google Scholar]
- 25.Gurtman MB, Balakrishnan JD. Circular measurement redux: The analysis and interpretation of interpersonal circle profiles. ClinPsychol: Science Practice. 1998;5:344–360. [Google Scholar]
- 26.Gurtman MB, Pincus AL. The circumplex model: Methods and research applications. In: Velicer WF, editor. Handbook of psychology: Research methods in psychology, vol. 2. Hoboken. John Wiley & Sons Inc.; NJ US: 2003. pp. 407–428. [Google Scholar]
- 27.Constantino M, Smith-Hansen L. Patient interpersonal factors and the therapeutic alliance in two treatments for bulimia nervosa. Psychother Res. 2008;18:683–698. doi: 10.1080/10503300802183702. [DOI] [PubMed] [Google Scholar]
- 28.Eldredge KL, Locke KD, Horowitz LM. Patterns of interpersonal problems associated with binge eating disorder. IntJEat Disord. 1998;23:383–389. doi: 10.1002/(sici)1098-108x(199805)23:4<383::aid-eat5>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 29.Ansell EB, Grilo CM, White MA. Examining the interpersonal model of binge eating and loss of control over eating in women. Int J Eat Disord. 2012;45:43–50. doi: 10.1002/eat.20897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV Axis I disorders – Patient Edition (SCID-I/P, Version 2.0) New York State Psychiatric Institute, Biometrics Research Department; New York: 1996. [Google Scholar]
- 31.Fairburn CG, Cooper Z. The eating disorders examination (12th ed) In: Fairburn CG, Wilson GT, editors. Binge eating: nature, assessment, and treatment. The Guilford Press; New York: 1993. pp. 317–331. [Google Scholar]
- 32.Spitzer RL, Yanovski SZ, Marcus MD. The questionnaire on eating and weight patterns-revised (QEWP-R) New York State Psychiatric Institute; New York: 1993. [Google Scholar]
- 33.Hopwood CJ, Pincus AL, DeMoor RM, Koonce EA. Psychometric characteristics of the inventory of interpersonal problems-short circumplex (IIP-SC) with college students. J Pers Assess. 2008;90:615–618. doi: 10.1080/00223890802388665. [DOI] [PubMed] [Google Scholar]
- 34.Grilo CM, Masheb RM, Wilson GT. A comparison of different methods for assessing the features of eating disorders in patients with binge eating disorder. J Consult ClinPsychol. 2001a;69:317–322. doi: 10.1037//0022-006x.69.2.317. [DOI] [PubMed] [Google Scholar]
- 35.Grilo CM, Masheb RM, Wilson GT. Different methods for assessing the features of eating disorders in patients with binge eating disorder: A replication. Obesity Res. 2001b;9:418–422. doi: 10.1038/oby.2001.55. [DOI] [PubMed] [Google Scholar]
- 36.Grilo CM, Masheb RM, Lozano-Blanco C, Barry DT. Reliability of the Eating Disorder Examination in patients with binge eating disorder. Int J Eat Disord. 2004;35:80–85. doi: 10.1002/eat.10238. [DOI] [PubMed] [Google Scholar]
- 37.Schmidt U, Treasure J. Anorexia nervosa: Valued and visible. A cognitive-behavioral and interpersonal maintenance model and its implications for research and practice. Br J ClinPsychol. 2006;45:343–366. doi: 10.1348/014466505x53902. [DOI] [PubMed] [Google Scholar]
- 38.Tchanturia K, Anderluh MB, Morris RG, Rabe-Hesketh S, Collier DA, Sanchez P, Treasure JL. Cognitive flexibility in anorexia nervosa and bulimia nervosa. J IntNeuropsychSoc. 2004;10:513–520. doi: 10.1017/S1355617704104086. [DOI] [PubMed] [Google Scholar]
- 39.Jackson TD, Grilo CM, Masheb RM. Teasing history, onset of obesity, current eating disorder psychopathology, body dissatisfaction, and psychological functioning in binge eating disorder. Obes Res. 2000;8:451–458. doi: 10.1038/oby.2000.56. [DOI] [PubMed] [Google Scholar]
- 40.Blomquist KK, Masheb RM, White MA, Grilo CM. Parental substance use history of overweight men and women with binge eating disorder is associated with distinct developmental trajectories and comorbid mood disorder. Comp Psych. 2011;52:693–700. doi: 10.1016/j.comppsych.2010.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Barnes RD, White MA, Masheb RM, Grilo CM. Accuracy of self-reported weight and height and resulting body mass index among obese binge eaters in primary care: Relationship with eating disorder and associated psychopathology. Prim Care Companion J Clin Psychiatry. 2010;12 doi: 10.4088/PCC.09m00868blu. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.White MA, Masheb RM, Grilo CM. Accuracy of self-reported weight and height in binge eating disorder: Misreport is not related to psychological factors. Obesity. 2010;18:1266–1269. doi: 10.1038/oby.2009.347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cain NM, Ansell EB, Wright AG, Hopwood CH, Thomas KM, Pinto A, et al. Interpersonal pathoplasticity in the course of major depression. J Consult ClinPsychol. 2012;80:78–86. doi: 10.1037/a0026433. [DOI] [PMC free article] [PubMed] [Google Scholar]