Abstract
Coronary artery disease is the leading cause of death in advanced countries and its prevalence is increasing among the developing countries. Cardiac computed tomography (CT) has been increasingly used in the diagnosis of coronary artery disease due to its rapid improvements in multislice CT scanners over the last decade, and this less-invasive technique has become a potentially effective alternative to invasive coronary angiography. Quantifying the amount of coronary artery calcium with cardiac CT has been widely accepted as a reliable non-invasive technique for predicting risk of future cardiovascular events. However, the main question that remains uncertain is whether routine, widespread coronary artery calcium scoring in an individual patient will result in an overall improvement in quality of care and clinical outcomes. In this commentary, we discuss a current issue of the clinical value of coronary artery calcium scoring with regard to its value of predicting adverse cardiac events. We also discuss the applications of coronary artery calcium scores in patients with different risk groups.
Keywords: Cardiac computed tomography, Coronary artery calcium, Coronary artery disease, Predictive value, Plaque
INVITED COMMENTARY ON HOT ARTICLES
We read Grayburn’s[1] recent perspective on interpreting the coronary artery calcium score with great enthusiasm, and would like to discuss the potential value of using coronary artery calcium (CAC) scoring in patients with different risk factors of cardiovascular disease.
Grayburn[1] presented a case vignette with a patient having a low Framingham risk score (less than 10% risk of a coronary event over the next 10 years); then highlighted a common clinical problem of how to utilize CAC scoring in asymptomatic and symptomatic populations with suspected coronary artery disease (CAD). Evidence supporting different strategies was presented, followed by the author’s clinical recommendations.
The first of the three comments in this commentary is that CAC scoring should be wisely used by physicians. CAC scoring is usually performed as a screening method with the use of low radiation dose scanning techniques. The purpose of the scan is to detect and calculate the calcium density, volume or mass. The total coronary calcium is used as a way of predicting and stratifying the risk of CAD. The rationale behind it is that coronary artery calcification is part of the atherosclerotic degeneration of the arterial vessel wall, and coronary atherosclerosis is the only disease associated with calcium in the coronary arteries[2]. Thus, measurement of the amount of calcium allows accurate estimation of the amount of coronary atherosclerosis and therefore the risk of coronary artery disease. Quantifying the amount of CAC scoring has been widely accepted as a reliable non-invasive technique for screening risk of future cardiac events, and is usually quantified by using the Agatston score[3].
Clinical application of CAC has been supported by evidence showing that the absence of calcium reliably excludes obstructive coronary artery stenoses, and that the amount of CAC is a robust predictor for risk assessment of incident cardiovascular events, independent of conventional coronary risk factors. However, the prognostic value of CAC depends on the risk groups as to whether patient risk is reclassified and patient management can be changed based on CAC scores when compared to traditional risk assessments[4].
The Framingham risk score is one of the most commonly used risk-estimation systems, which enables clinicians to estimate cardiovascular risk in asymptomatic patients. It is calculated using traditional risk predictors, including age, gender, total cholesterol, high-density lipoprotein cholesterol, smoking status, and systolic blood pressure, and is represented as a 10-year risk score for the prediction of coronary artery disease events[5]. However, there is growing evidence to show that these traditional risk assessment methods, based on risk factor analysis, have significant limitations when used to guide individual patient therapy. CAC scoring by multislice CT has been increasingly used as an additional assessment tool to evaluate the risk of developing major cardiac events in asymptomatic and symptomatic patients. Guidelines vary on the question of whether CAC is indicated for screening asymptomatic patients at intermediate risk for CAD[6-8], however, CAC screening of symptomatic patients with known CAD is generally believed to be not helpful[9]. As Grayburn pointed out in this article, it is important for physicians to evaluate the CAC score within the clinical context before further tests are recommended for patients.
The second comment is that CAC is added to traditional risk factors, and it leads to a significant improvement in the classification of risk for the prediction of cardiac events in an asymptomatic population. Since the CAC score indicates the presence or absence and measures the extent of coronary atherosclerosis, it is not unexpected that a high CAC score is regarded as a marker for an increased risk of coronary events. Thus, a CAC score of zero is associated with a very low risk of subsequent cardiac events[10,11], whereas increasing CAC scores are associated with a step-wise increase in the risk of events.
The goal of CAC screening in asymptomatic persons is to refine the risk assessment with the aim of determining whether preventive strategies should be intensified, not identifying persons with asymptomatic coronary stenosis[12]. Polonsky et al[7] in their multi-ethnic cohort consisting of 5878 participants without known cardiovascular disease investigated the additional value of CAC score to traditional cardiovascular risk factors with regard to the potential role for risk stratification. Their results showed that when CAC score was added to traditional risk factors, it contributed to a significant improvement in the classification of risk for the prediction of cardiac events in an asymptomatic population.
In asymptomatic individuals, zero CAC is associated with a very low (< 1% per year) risk of major cardiac events over the next 3-5 years, whereas in asymptomatic patients with extensive coronary calcification, the major cardiac events have been reported to be increased by up to 11-fold[13]. The recent population-based multi-ethnic study of atherosclerosis, conducted in 6722 asymptomatic patients belonging to four racial ethnic groups and followed for 3.8 years, showed a significant difference in the prevalence of CAC among different ethnic groups. Nonetheless, CAC has demonstrated incremental prognostic value over traditional risk factors, with a seven-fold increase in the incidence of cardiac events for Agatston scores > 100 when compared with patients with zero CAC[14].
Other studies evaluating the prognostic value of the measurement of CAC have shown that coronary calcification is predictive of cardiac events in asymptomatic patients with different age groups[15-17]. In the Prospective Army Coronary Calcium Project among men and women 40 to 45 years of age, Taylor et al[15] concluded that the presence of coronary calcium was associated with an increase in the risk of coronary events by a factor of 12 during 3 years of follow-up. LaMonte et al[16] in their study consisting of nearly 11 000 patients ranging from 22 to 96 years of age who underwent a screening medical examination, reported increased cardiac events in patients with coronary calcium scores of 400 or more during a mean follow-up of 3.5 years. Similarly, higher calcium scores were found to be associated with the relative risks of coronary events in the population-based Rotterdam Study of elderly asymptomatic patients[17].
Although the association between CAC scores and cardiovascular events has been well documented, a clinical question arises regarding whether CAC scoring has a favourable effect on clinical outcomes, and there are concerns about the associated radiation exposure[18-21]. The radiation dose associated with CAC scoring is small but real, which ranges from 0.9 to 2.4 mSv with multislice CT[22], and some cardiac CT imaging protocols are associated with estimated radiation doses higher than 10 mSv[18,22,23]. This results in a small but measurable increase in the risk of radiation-induced cancer[18], thus, this should be considered if CAC scoring (and repeated testing) were used for widespread population screening.
The third comment is that CAC scoring is not recommended for screening of symptomatic patients. Coronary calcification is considered only marginally related to the degree of coronary stenosis and it is well known that both obstructive and non-obstructive CAD can occur in the absence of calcification[24,25]. Significantly, coronary stenoses are frequently found to be non-calcified (Figure 1), and highly calcified plaques are frequently non-occlusive or obstructive (Figure 2). Thus, the value of a zero or low calcium score in symptomatic patients remains unclear.
Figure 1.
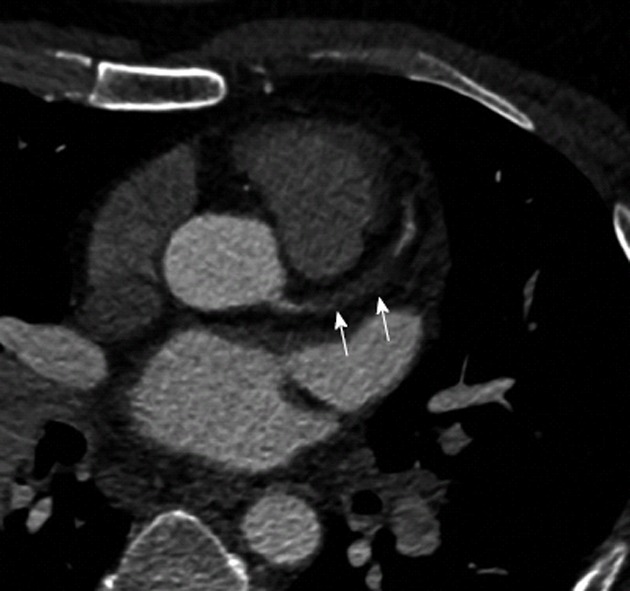
Coronary computed tomography angiography in a 43-year-old male presenting with chest pain and raised cardiac enzymes shows non-calcified plaque at the left main and left anterior descending arteries (arrows) causing a complete total occlusion of these vessels.
Figure 2.
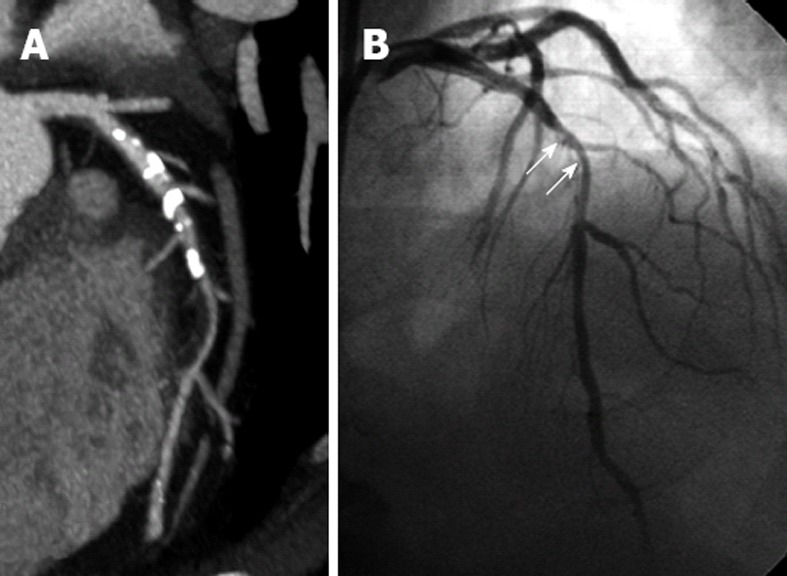
Calcified plaques and stenosis of left anterior descending. A: Extensive calcified plaques are noticed in the proximal and middle segments of left anterior descending (LAD) on curved planar reformatted image, resulting in significant stenosis or total lumen occlusion; B: A 50% stenosis of LAD is confirmed on invasive coronary angiography (arrows).
Several studies have reported the presence of obstructive non-calcified plaque in up to 8.7% of symptomatic patients with zero or low calcium score[26,27]. The question has been raised as to whether only using CAC score is a reliable tool to determine the extent of CAD, since non-calcified coronary artery plaque may not be detected. Cheng et al[26] reported that low but detectable CAC scores are less reliable in predicting plaque burden due to their association with high overall non-calcified coronary artery plaque. They concluded that low CAC scores are significantly less predictive of prevalence or severity of underlying non-calcified coronary plaque.
Villines et al[9] in their recently published international multi-centre study, concluded that in symptomatic patients with a CAC score of 0, obstructive CAD is possible and is associated with increased cardiovascular events. Thus, low but detectable CAC scores are considered less reliable in predicting disease burden due to the association with high overall non-calcified coronary plaques. Symptomatic patients should be referred for coronary CT angiography to determine the extent of CAD and predict disease outcomes, as there is no significant incremental value of CAC scoring beyond the CCTA prognostic information in symptomatic patients[28].
In summary, the author has raised an important issue of whether CAC scoring should be widely used in cardiovascular prevention strategies. There are many limitations of applying CAC scoring as a screening tool to broad populations and this has been systematically reviewed[12]. There is a lack of prospective randomized controlled trials showing that an abnormal CAC score impacts treatment decisions or clinical outcomes. However, an abnormal CAC score may be helpful in encouraging some patients to take their prescribed medications and follow recommended lifestyle changes[8,29,30]. Until these data is available, CAC scoring should be judiciously used by physicians in patients with different risk factors of developing cardiovascular events.
Footnotes
Peer reviewer: Pil-Ki Min, MD, PhD, Cardiology Division, Heart Center, Gangnam Severance Hospital, Yonsei University College of Medicine, 712 Eonjuro, Gangnam-gu, Seoul 135-720, South Korea
S- Editor Cheng JX L- Editor A E- Editor Li JY
References
- 1.Grayburn PA. Interpreting the coronary-artery calcium score. N Engl J Med. 2012;366:294–296. doi: 10.1056/NEJMp1110647. [DOI] [PubMed] [Google Scholar]
- 2.Sun Z, Ng KH. Multislice CT angiography in cardiac imaging. Part II: clinical applications in coronary artery disease. Singapore Med J. 2010;51:282–289. [PubMed] [Google Scholar]
- 3.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15:827–832. doi: 10.1016/0735-1097(90)90282-t. [DOI] [PubMed] [Google Scholar]
- 4.Sun Z, Aziz YF, Ng KH. Coronary CT angiography: how should physicians use it wisely and when do physicians request it appropriately? Eur J Radiol. 2012;81:e684–e687. doi: 10.1016/j.ejrad.2011.06.040. [DOI] [PubMed] [Google Scholar]
- 5.National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–3421. [PubMed] [Google Scholar]
- 6.Budoff MJ, Achenbach S, Blumenthal RS, Carr JJ, Goldin JG, Greenland P, Guerci AD, Lima JA, Rader DJ, Rubin GD, Shaw LJ, Wiegers SE; American Heart Association Committee on Cardiovascular Imaging and Intervention; American Heart Association Council on Cardiovascular Radiology and Intervention; American Heart Association Committee on Cardiovascular Imaging Council on Clinical Radiology. Assessment of coronary artery disease by cardiac computed tomography: a scientific statement from the American Heart Association Committee on Cardiovascular Imaging and Intervention, Council on Cardiovascular Radiology and Intervention, and Committee on Cardiac Imaging, Council on Clinical Cardiology. Circulation. 2006;114:1761–1791. doi: 10.1161/CIRCULATIONAHA.106.178458. [DOI] [PubMed] [Google Scholar]
- 7.Polonsky TS, McClelland RL, Jorgensen NW, Bild DE, Burke GL, Guerci AD, Greenland P. Coronary artery calcium score and risk classification for coronary heart disease prediction. JAMA. 2010;303:1610–1616. doi: 10.1001/jama.2010.461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rozanski A, Gransar H, Shaw LJ, Kim J, Miranda-Peats L, Wong ND, Rana JS, Orakzai R, Hayes SW, Friedman JD, et al. Impact of coronary artery calcium scanning on coronary risk factors and downstream testing the EISNER (Early Identification of Subclinical Atherosclerosis by Noninvasive Imaging Research) prospective randomized trial. J Am Coll Cardiol. 2011;57:1622–1632. doi: 10.1016/j.jacc.2011.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Villines TC, Hulten EA, Shaw LJ, Goyal M, Dunning A, Achenbach S, Al-Mallah M, Berman DS, Budoff MJ, Cademartiri F, et al. Prevalence and severity of coronary artery disease and adverse events among symptomatic patients with coronary artery calcification scores of zero undergoing coronary computed tomography angiography: results from the CONFIRM (Coronary CT Angiography Evaluation for Clinical Outcomes: An International Multicenter) registry. J Am Coll Cardiol. 2011;58:2533–2540. doi: 10.1016/j.jacc.2011.10.851. [DOI] [PubMed] [Google Scholar]
- 10.Khot UN, Khot MB, Bajzer CT, Sapp SK, Ohman EM, Brener SJ, Ellis SG, Lincoff AM, Topol EJ. Prevalence of conventional risk factors in patients with coronary heart disease. JAMA. 2003;290:898–904. doi: 10.1001/jama.290.7.898. [DOI] [PubMed] [Google Scholar]
- 11.Grundy SM, Cleeman JI, Merz CN, Brewer HB, Clark LT, Hunninghake DB, Pasternak RC, Smith SC, Stone NJ. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation. 2004;110:227–239. doi: 10.1161/01.CIR.0000133317.49796.0E. [DOI] [PubMed] [Google Scholar]
- 12.Bonow RO. Clinical practice. Should coronary calcium screening be used in cardiovascular prevention strategies? N Engl J Med. 2009;361:990–997. doi: 10.1056/NEJMcp0902177. [DOI] [PubMed] [Google Scholar]
- 13.Johnson KM, Dowe DA, Brink JA. Traditional clinical risk assessment tools do not accurately predict coronary atherosclerotic plaque burden: a CT angiography study. AJR Am J Roentgenol. 2009;192:235–243. doi: 10.2214/AJR.08.1056. [DOI] [PubMed] [Google Scholar]
- 14.Budoff MJ, Nasir K, McClelland RL, Detrano R, Wong N, Blumenthal RS, Kondos G, Kronmal RA. Coronary calcium predicts events better with absolute calcium scores than age-sex-race/ethnicity percentiles: MESA (Multi-Ethnic Study of Atherosclerosis) J Am Coll Cardiol. 2009;53:345–352. doi: 10.1016/j.jacc.2008.07.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Taylor AJ, Bindeman J, Feuerstein I, Cao F, Brazaitis M, O’Malley PG. Coronary calcium independently predicts incident premature coronary heart disease over measured cardiovascular risk factors: mean three-year outcomes in the Prospective Army Coronary Calcium (PACC) project. J Am Coll Cardiol. 2005;46:807–814. doi: 10.1016/j.jacc.2005.05.049. [DOI] [PubMed] [Google Scholar]
- 16.LaMonte MJ, FitzGerald SJ, Church TS, Barlow CE, Radford NB, Levine BD, Pippin JJ, Gibbons LW, Blair SN, Nichaman MZ. Coronary artery calcium score and coronary heart disease events in a large cohort of asymptomatic men and women. Am J Epidemiol. 2005;162:421–429. doi: 10.1093/aje/kwi228. [DOI] [PubMed] [Google Scholar]
- 17.Vliegenthart R, Oudkerk M, Hofman A, Oei HH, van Dijck W, van Rooij FJ, Witteman JC. Coronary calcification improves cardiovascular risk prediction in the elderly. Circulation. 2005;112:572–577. doi: 10.1161/CIRCULATIONAHA.104.488916. [DOI] [PubMed] [Google Scholar]
- 18.Kim KP, Einstein AJ, Berrington de González A. Coronary artery calcification screening: estimated radiation dose and cancer risk. Arch Intern Med. 2009;169:1188–1194. doi: 10.1001/archinternmed.2009.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brenner DJ, Hall EJ. Computed tomography--an increasing source of radiation exposure. N Engl J Med. 2007;357:2277–2284. doi: 10.1056/NEJMra072149. [DOI] [PubMed] [Google Scholar]
- 20.Fazel R, Krumholz HM, Wang Y, Ross JS, Chen J, Ting HH, Shah ND, Nasir K, Einstein AJ, Nallamothu BK. Exposure to low-dose ionizing radiation from medical imaging procedures. N Engl J Med. 2009;361:849–857. doi: 10.1056/NEJMoa0901249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lauer MS. Elements of danger--the case of medical imaging. N Engl J Med. 2009;361:841–843. doi: 10.1056/NEJMp0904735. [DOI] [PubMed] [Google Scholar]
- 22.Sun Z, Choo GH, Ng KH. Coronary CT angiography: current status and continuing challenges. Br J Radiol. 2012;85:495–510. doi: 10.1259/bjr/15296170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sun Z. Multislice CT angiography in coronary artery disease: Technical developments, radiation dose and diagnostic value. World J Cardiol. 2010;2:333–343. doi: 10.4330/wjc.v2.i10.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gottlieb I, Miller JM, Arbab-Zadeh A, Dewey M, Clouse ME, Sara L, Niinuma H, Bush DE, Paul N, Vavere AL, et al. The absence of coronary calcification does not exclude obstructive coronary artery disease or the need for revascularization in patients referred for conventional coronary angiography. J Am Coll Cardiol. 2010;55:627–634. doi: 10.1016/j.jacc.2009.07.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chang SM, Nabi F, Xu J, Peterson LE, Achari A, Pratt CM, Mahmarian JJ. The coronary artery calcium score and stress myocardial perfusion imaging provide independent and complementary prediction of cardiac risk. J Am Coll Cardiol. 2009;54:1872–1882. doi: 10.1016/j.jacc.2009.05.071. [DOI] [PubMed] [Google Scholar]
- 26.Cheng VY, Lepor NE, Madyoon H, Eshaghian S, Naraghi AL, Shah PK. Presence and severity of noncalcified coronary plaque on 64-slice computed tomographic coronary angiography in patients with zero and low coronary artery calcium. Am J Cardiol. 2007;99:1183–1186. doi: 10.1016/j.amjcard.2006.12.026. [DOI] [PubMed] [Google Scholar]
- 27.Hausleiter J, Meyer T, Hadamitzky M, Kastrati A, Martinoff S, Schömig A. Prevalence of noncalcified coronary plaques by 64-slice computed tomography in patients with an intermediate risk for significant coronary artery disease. J Am Coll Cardiol. 2006;48:312–318. doi: 10.1016/j.jacc.2006.02.064. [DOI] [PubMed] [Google Scholar]
- 28.Kwon SW, Kim YJ, Shim J, Sung JM, Han ME, Kang DW, Kim JY, Choi BW, Chang HJ. Coronary artery calcium scoring does not add prognostic value to standard 64-section CT angiography protocol in low-risk patients suspected of having coronary artery disease. Radiology. 2011;259:92–99. doi: 10.1148/radiol.10100886. [DOI] [PubMed] [Google Scholar]
- 29.Preventive Services Task Force. Guide to clinical preventive services. 2nd ed. Available from: http://odphp.osophs.dhhs.gov/pubs/guidecps/
- 30.Taylor AJ, Bindeman J, Feuerstein I, Le T, Bauer K, Byrd C, Wu H, O’Malley PG. Community-based provision of statin and aspirin after the detection of coronary artery calcium within a community-based screening cohort. J Am Coll Cardiol. 2008;51:1337–1341. doi: 10.1016/j.jacc.2007.11.069. [DOI] [PubMed] [Google Scholar]


