Abstract
Background:
Dentine hypersensitivity is a transient condition that often resolves with the natural sclerotic obturation of dentinal tubules. A potent topically applied in-office desensitizing treatment is indicated as the choice of treatment when dentine hypersensitivity is localized to one or two teeth.
Aim:
The present study aimed to evaluate and compare the clinical efficiency of CPP-ACP F, sodium fluoride, propolis, and distilled water that was used as placebo in treating dentinal hypersensitivity.
Materials and Methods:
120 patients aged 20–40 years reporting with dentinal hypersensitivity in relation to canine, premolar and molars with erosion, abrasion, and gingival recession were randomly assigned to four groups of 30 patients each. Response to air jet and tactile stimuli were measured using visual analogue scale initially on 1st, 7th, 15th, 28th, 60th, and final assessment was done on the 90th day.
Statistical Analysis:
A statistical analysis was done using Anova test (Fischer's test) and Tukey HSD test for multicomparison.
Results:
The teeth treated with the test group showed decrease in the mean hypersensitivity values compared to control group, over a period of three months. The results showed propolis to be most efficient in treating dentinal hypersensitivity and CPP- ACPF showed to be the least efficient.
Conclusion:
All test groups were effective in reducing dentinal hypersensitivity, although they differed in rapidity of action over the period of 3 months. Further studies can be done using advanced materials and techniques. Multiple therapeutic modalities have been developed to treat dentinal hypersensitivity including products that impede nerve conduction of pain stimulus, products that mechanically occlude dentinal tubules, and calcium containing products designed to create plugs in the tubules utilizing a demineralization mechanism.
Keywords: Airjet, dentinal hypersensitivity, tactile stimulation, visual analogue scale
INTRODUCTION
Dentin hypersentivity has been defined as a short, sharp pain arising from exposed dentin in response to stimuli, typically thermal, evaporative, tactile, osmotic, or chemical, which cannot be ascribed to any other form of dental pathology.[1] This condition generally involves the facial surfaces of teeth near the cervical border, and is very common in canine, premolars, and molars. Although sensitivity effects all ages, previous reports show that there is a strong correlation between age and dentinal hypersensitivity. Studies have shown that dentinal hypersensitivity was frequently observed between the age group of 20 and 40 years with women showing more prevalence.[2]
The terms abfraction and abrasion describe the cause of lesions found along the cervical margins of teeth. Much stronger evidence suggests the result of cervical wear is a combination of erosion, abrasion, and attrition.[3] There are several theories for dentinal hypersensitivity such as odontoblastic transduction theory, neural theory, and hydrodynamic theory. The most accepted theory for dentinal hypersensitivity is the hydrodynamic theory presented by Brannstorm and others, which suggests that the fluids within the dentinal tubules flow due to thermal, mechanical, evaporative, and osmotic stimuli. The flow of liquids in dentinal tubules can trigger nerves along the pulpal canal of the dentin, causing pain.[4]
The measurement of hypersensitivity has been evaluated by tactile (electronic pressure sensitive probe), air blast from the dental unit air syringe, and thermal stimulus. Tarbet et al. have reported air blast and tactile stimulus to be the accurate methods for the examination of hypersensitivity levels.[5]
Most of published information relates to the prevalence of hypersensitivity; however, currently there does not appear to be globally agreed Gold standard procedure for comparative purposes in clinical trial setting for evaluation of new desensitizing agents.[6]
Three topical desensitizers were employed in this study CPP- ACPF, sodium fluoride, propolis, and placebo as a control group for the treatment of dentinal hypersensitivity. Only a few studies have evaluated the efficiency of desensitizing agents in vivo. Hence, it was considered worthwhile to assess the efficacy of these desensitizing agents in providing relief from the dentinal hypersensitivity and to help the clinicians choose the most effective treatment.
MATERIALS AND METHODS
One hundred and twenty subjects were divided equally into four groups between the ages of 20–40 years who were in good general health were selected with the written informed consent to participate in this 3-month study. At the first screening visit, demographic details were obtained together with medical and dental histories. Sensitivity was assessed by means of tactile and evaporative stimuli. To produce evaporative stimuli a 1 s air blast was delivered using the dental unit triple syringe, blowing a short blast of room temperature air, being held perpendicular and 2 mm away from tooth surface, whilst shielding the adjacent teeth with fingers or cotton rolls. The sensitivity of the tooth to the tactile stimulation was determined using a periodontal probe passed perpendicular to the tooth surface with apical sweeps and the pressure in grams was gradually increased until the subject responded. The patients were given a visual analogue scale upon which they were asked to place a mark at a point on a linear scale marked from 0–10 cm to describe the pain experienced.
APPLICATION OF DESENSITIZERS
In this study, each group was treated using one of the four desensitizing products in accordance with the manufacturer's instructions. The desensitizing agents were applied and rubbed over the tooth surface and left undisturbed for 60 s. The patients were then asked not to rinse, eat, or drink for 30 min after the treatment. Pre- and post-treatment assessment was done at the baseline, 7th day, 15th day, 28th day, 60th day and measurements were recorded by the same investigator. On the 90th day the final assessment was recorded with no treatment rendered.
Statistical analysis
Fischer's test was used to determine the comparative mean and the standard deviations of all the groups and Tukey HSD multiple comparison test was used for air jet and tactile stimulation assessment over a period of three months with a significance level of P<0.05.
RESULTS
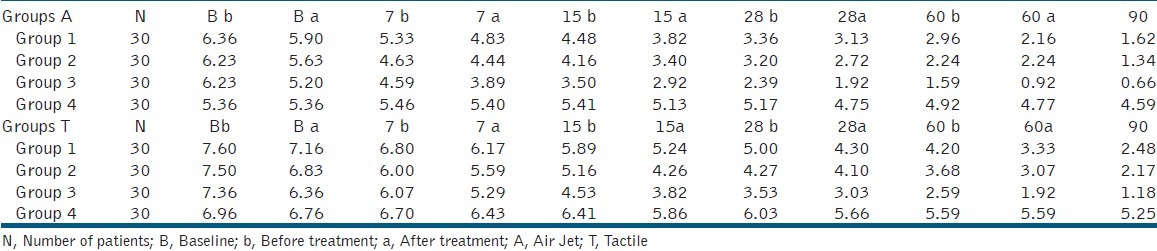
Group 1 (CPP-ACP F), Group 2 (Sodium fluoride), and Group 3 (Propolis) showed decreased mean hypersensitivity values compared to the control group (Group 4) over a period of 3 months from the baseline [Table 1].
Table 1.
Comparison between mean air jet and tactile sensitivity scores for the test groups over a period of months using Anova test
Intergroup comparison of mean scores revealed Group 3 (Propolis) to have the least mean value for air jet and tactile stimulation on all days when compared with other test groups. Significant differences were observed between Group 1 and Group 3 for both air jet and tactile stimulation on the 7th, 15th, 28th, and 60th day [Table 2].
Table 2.
Tukey multiple comparison test for air jet and tactile stimulation from the baseline to 60th day before and after application of desensitizing agents (Significance level 0.05)
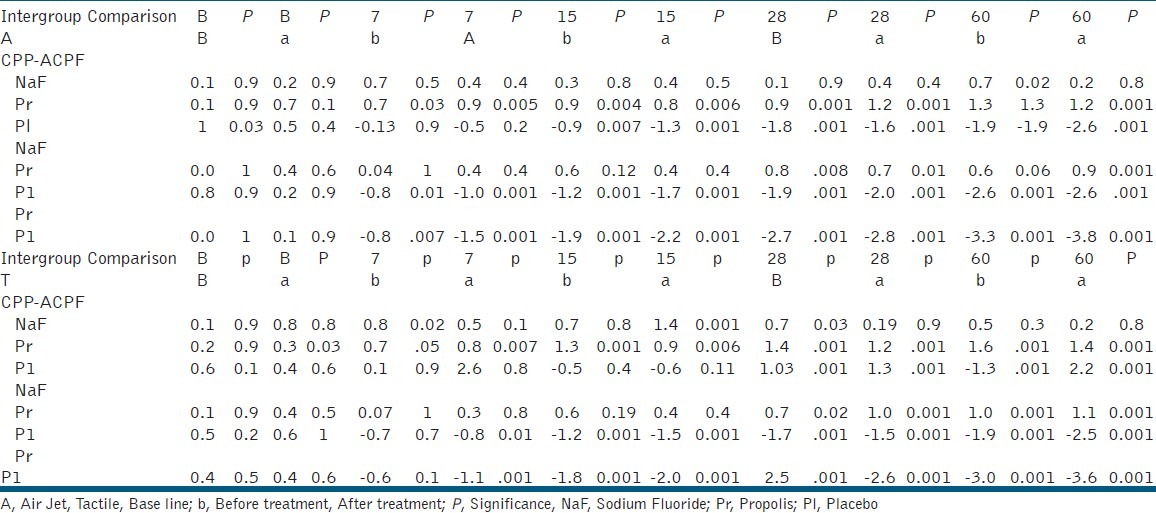
Very high significant differences were observed between Group 2 and Group 3 compared to Group 4 on the 7th day, 15th day, 28th day, 60th, and 90th day for both types of stimulation.
However Group 1 versus Group 4 showed very high significant differences from the 15thday for air jet and from the 28th day for tactile stimulation to the tested period. Very high significant differences were observed between Group 1 and Group 2 and Group 3 (Propolis) for tactile stimulus on the 15th day. The change in sensitivity was much more apparent using the air jet stimulation than tactile stimulation.
DISCUSSION
Dentine hypersensitivity is a clinical situation characterized by a short, sharp pain initiated by many types of stimulation such as tactile, thermal, osmotic, or chemical. It is one of the most common and uncomfortable conditions affecting oral comfort. There is a need to develop new treatment or products which permit the relief of symptoms.[7] This study aimed to evaluate and compare the clinical efficiency of CPP-ACPF, sodium fluoride, propolis, and placebo in treating dentinal hypersensitivity. It is generally recommended that more than one stimulus should be used in clinical studies of dentine hypersensitivity. This would enhance the measurement of sensitivity.[5] This study utilized airjet and tactile stimulation as in concurrence with Sowinski et al., Ide, and Walters.[2,5,8] These two methods were reported to be accurate for the examination of hypersensitivity levels according to Tarbet et al., in 1982 and Clark and Troullous in 1990.[8] Attempts to translate subjective feedback to objective data for research purposes have involved both unidimensional and multidimensional pain measurement systems (Flaherty 1996). The most common unidimensional method is the visual analogue scale. It is widely used in clinical research to assess intensity of acute pain.[5] The result of this study showed all the test groups to have a decrease in mean hypersensitivity values compared to the control group for the tested period from the baseline. The results demonstrated relief of sensitivity for tactile and air stimulation for Group 1 (CPP-ACP F), Group 2 (sodium fluoride), and Group 3 (Propolis). Tung et al., have postulated that the materials CPP-ACP and propolis precipitate and obstruct the dentinal tubules and decrease dentinal permeability by 85% or more.[7]
Intergroup comparisons revealed Group 3 (Propolis) to be more efficient in the treatment of dentinal hypersensitivity compared to the groups tested. Mahmoud et al., studied the effect of Propolis as a desensitizing agent and demonstrated that 85% of subjects were found highly satisfied during the study period as in comparison to this study. The mechanism of action is because of high content of Flavanoids in Propolis.[9] Flavanoids may be able to suppress the information of free radicals by binding heavy metals in ions which are known to catalyze many processes leading to the appearance of full radicals. Propolis is known to be an antioxidant, antimicrobial, anti-inflammatory, immunostimulatory, and heavy metal chelating agent. It also has an effect on tissue regeneration and wound healing.[10]
Clinical impression suggests that dentinal hypersensitivity has a somewhat random cyclical pattern that may reflect a change in balance between the effects of etiological verses protective factors.[11] Placebo effects are commonly referred to in the dentinal hypersensitivity clinical trial literature but not studied. The placebo effect is a response to medical intervention that results from the intervention itself and not from any particular mechanism of action.[12] This study was peculiar in being one of the few where a true placebo, water was applied to the test teeth.
In this study, Group 2 (sodium fluoride) verses and Group 3 (Propolis) showed significant statistical differences on the 28th day, 60th day for both airjet and tactile stimulation and from 28th to 90th day before application of desensitizing agents. High significance was observed on the 7th day with placebo after the application of desensitizing agent. However, the mean sensitivity value was less for Group 2 (sodium fluoride) when compared to Group 1 (CPP-ACPF). Therefore, the efficiency of Group 2 (sodium fluoride) was much better than Group 1 (CPP-ACPF).
This study is in accordance with other clinical studies where treatment of the exposed root surface with fluoride tooth paste and concentrated fluoride solution is very efficient in managing dentinal hypersensitivity. The improvement appears to be due to an increase in the resistance of dentine to acid decalcification as well as precipitation in exposed dentinal tubules.[13]
Poitevin A demonstrated the effectiveness of CPP-ACP for dentine hypersensitivity treatment and concluded that significant reduction was noticed after the air stimulus than the tactile stimuli. In coincidence with our study, CPP-ACP showed the effectiveness from the 28th day. The present in vivo study showed Group 1 (CPP-ACPF) showed to be least efficient when compared to other study groups. The fluoride content that is 900 ppm potentially can interact with ACP component of the casein complex and may precipitate out as calcium fluoride, rendering both inorganic components ineffective.[14]
Dentin hypersensitivity studies are subject based. Therefore, several factors can influence the measurement of pain. To date, none of the methods used to assess the measurements have been seen to be completely successful. However, it may be suggested that the aim in dentin hypersensitivity studies is to relieve patients’ discomfort. Hence, long-term studies and repeated applications of desensitizing agents are necessary. To date no standard procedures have been developed to test products designed for treatment of the condition; hence, comparison of products between trials is fraught with difficulties. In addition, well-designed control groups and working with more subjects may be of great help in obtaining more reliable results.
CONCLUSION
Within the parameters of this study on comparison of the clinical efficacy of CPP ACPF, sodium fluoride, and propolis in treating dentinal hypersensitivity, the following conclusions were drawn.
All test groups were effective in reducing dentinal hypersensitivity although they differed in rapidity of action over a period of 2 months.
Group 3 (Propolis) showed rapid decrease in hypersensitivity values from the baseline compared to other groups.
Group 1 (CPP_ACP F) showed the least performance next to the control group.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Addy M. Bristol, Tooth brushing, tooth wear and dentine hypersensitivity- are they related? Int Dental J. 2005;55:261–7. doi: 10.1111/j.1875-595x.2005.tb00063.x. [DOI] [PubMed] [Google Scholar]
- 2.Walter PA. Dentinal hypersensitivity: A review. J Contemporary Dent Practice. 2005;6:1–10. [PubMed] [Google Scholar]
- 3.Bartletta DW, Shah P. A Critical Review of Non-carious Cervical (Wear) Lesions and the Role of Abfraction, Erosion, and Abrasion. J Dent Res. 2006:306–12. doi: 10.1177/154405910608500405. [DOI] [PubMed] [Google Scholar]
- 4.Hoang BT. Evaluation of a natural resin based new material (Shellac F) as a potential desensitizing agent. Dent mater. 2008;24:1001–7. doi: 10.1016/j.dental.2007.11.014. [DOI] [PubMed] [Google Scholar]
- 5.Ide M, Wilson RF, Ashley FP. The reproducibility of methods of assessment for cervical dentine hypersensitivity’. J Clin Periodontol. 2001;28:16–22. doi: 10.1034/j.1600-051x.2001.280103.x. [DOI] [PubMed] [Google Scholar]
- 6.Nagata T, Ishida H, Shinohara H, Nlshikawa S, Kasahara S, Wakano Y, et al. “Clinical evaluation of a potassium nitrate dentifrice for the treatment of dentinal hypersensitivity”. J Clin Periodontol. 1994;21:217–21. doi: 10.1111/j.1600-051x.1994.tb00307.x. [DOI] [PubMed] [Google Scholar]
- 7.Geiger S, Matalon S, Blasbalg J. ‘The clinical effect Amorphous calcium phosphate on root surface Hypersensitivity’. J Oper Den. 2003:496–500. [PubMed] [Google Scholar]
- 8.Sowinski J, et al. Comparative investigations of the desensitizing efficacy of a new dentifrice. J clin peridontol. 2001;28:1032–6. doi: 10.1034/j.1600-051x.2001.281107.x. [DOI] [PubMed] [Google Scholar]
- 9.Almas K, Mahmoud A. The effect of propolis on dentinal hypersensitivity and level of satisfaction among the patients from a university hospital, Riyadh, Saudi Arabia. Indian J Dent Res. 1999;10:130–37. [PubMed] [Google Scholar]
- 10.Almas K, Mahmoud A, Dahlan A. A comparative study of propolis and saline application on human dentin. A SEM study. Indian J Dent Res. 2001;12:21–7. [PubMed] [Google Scholar]
- 11.Yates R, Owens J, Jackson R, Newcombe RG, Addy M. A split mouth placebo-controlled study to determine the effect of amorphous calcium phosphate in the treatment of dentine hypersensitivity. J Clin Periodontol. 1998;25:687–92. doi: 10.1111/j.1600-051x.1998.tb02506.x. [DOI] [PubMed] [Google Scholar]
- 12.West NX, Addy M, Jackson RJ, Ridge DB. Dentin hypersensitivity and placebo response a comparison of effect of strontium acetate, potassium nitrate and fluoride tooth paste. J Clinc Periodontol. 1997;24:209–15. doi: 10.1111/j.1600-051x.1997.tb01833.x. [DOI] [PubMed] [Google Scholar]
- 13.Bartold P M. Dentinal hypersensitivity: A review. ADJ. 2006;51:212–18. [PubMed] [Google Scholar]
- 14.Azarpazhooh A, et al. Clinical efficacy of casein derivatives, A Systemic review of literature. J Am Dent Assoc. 2008;139:915–24. doi: 10.14219/jada.archive.2008.0278. [DOI] [PubMed] [Google Scholar]


