Abstract
Basosquamous carcinoma (BSC) is a rare aggressive epithelial neoplasm with features of both basal cell carcinoma and squamous cell carcinoma, with a tendency toward local recurrence and a propensity for lymph node and distant metastases. The aim of the present study was to report the case of a 63-year-old Caucasian male with BSC in the auricular region.
Keywords: Basosquamous carcinoma, skin, malignancy
Introduction
Basosquamous carcinoma (BSC) is a rare epithelial neoplasm with features of both basal cell carcinoma (BCC) and squamous cell carcinoma (SCC) and is linked by a transition area.[1,2] Like SCC, BSC is more locally invasive, aggressive, and more likely to metastasize than forms of BCC.[3,4] Metastasized BSC is more difficult to treat and has a poor prognosis.[5]
Clinically, most BSCs are located in the head and neck, mainly on the nose and in the auricular and periocular regions. BSC is usually a slow-growing tumor and the low rate of correct diagnosis of BSC is probably due to small biopsy specimens.[6] Moreover, BSC has a nonspecific clinical presentation and diagnosis is made only after biopsy.[7]
Excision is probably the best treatment,[7] and surgical margins should be wider than those for low-risk BCC due to the infiltrative growth pattern of this tumor. Nevertheless, high recurrence rates are reported despite wide local incision,[6] making complete excision essential.
Case Report
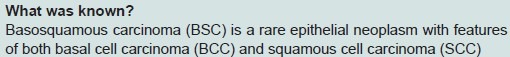
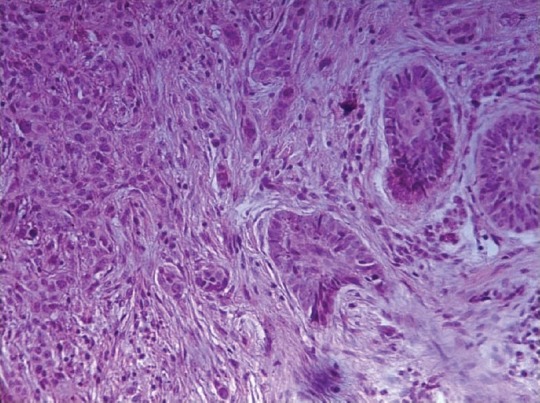
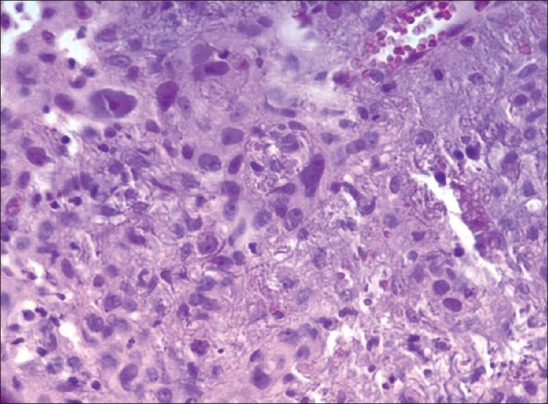
A 63-year-old Caucasian male had a sessile lesion removed from his left ear. Histological analysis revealed a partially excised BCC. Seven years later, a local recurrence was widely excised and histological analysis confirmed BSC.[2] Histological analysis with hematoxylin and eosin (H and E) stain revealed multiple islands of malignant cells throughout the dermis, exhibiting both basaloid and squamous differentiation. The areas had BCC, with large and rounded basaloid cells [Figure 1], and SCC, with polygonal squamoid cells with abundant eosinophilic cytoplasm, large nuclei, and prominent nucleoli. The SCC component exhibited frequent atypical mitosis, cell and nuclear pleomorphism and hyperchromatism of the nuclei [Figure 2]. The transition zone, which appeared abruptly, had intermediate cells and was between the BCC and SCC areas [Figure 1]. The squamoid component exhibited dyskeratotic cells and metastatic cells invading blood vessels [Figure 3]. The patient has been followed up, and after 6 months, with no sign of further disease.
Figure 1.
BSC with a transition zone appearing abruptly (intermediate cells) between SCC and BCC areas (H and E, 200×)
Figure 2.
Squamoid component with cellular and nuclear pleomorphism and nuclear hyperchromatism (H and E, 400×)
Figure 3.
Squamoid component with dyskeratotic cells (star) and invasion of the tumor cell in blood vessel (arrow) (H and E, 400×)
Discussion
Many malignant skin tumors are easily classified as either classic BCC or SCC, with the correct prediction of their biological behavior. Some tumors, however, are intermediate in their histology, while others are somewhat variable from one microscopic field to another. These groups of tumors are classified as BSCs.[2]
The diagnosis of the present case was BSC, with a transition zone between BCC and SCC.[2] The BSC areas have small, uniform, hyperchromatic cells, with peripheral palisading mitoses and stromal collagen deposition with proliferative fibroblasts. In contrast to pure BCC, some basaloid cells in BSC have eosinophilic cytoplasm, often lack the characteristic peripheral palisading and retraction artifact and exhibit variable cytoplasmic keratinization.[8–10] Basaloid cells are mitotically more active than indolent growth BCC, with greater numbers of apoptotic nuclei. SCC areas are characterized by large polygonal squamoid cells with eosinophilic cytoplasm reflecting cytoplasmic keratinization, larger open nuclei with prominent nucleoli, frequent mitosis, dyskeratotic cells, and intercellular bridges. The transition zone between BCC and SCC may or may not exist and has a fibroblast-rich and collagenized stroma.[7] However, according to Martin et al.,[8] BSC is not a collision carcinoma of BCC and SCC and the transition zone between the basal cell and squamous cell types is not necessary for the diagnosis of BSC.
Clinically, BSC is most commonly seen on the head and neck, mainly involving the central face, and has a significant predominance in male Caucasians.[6] In a case series involving 178 patients, Leibovitch[6] found that 95% of the tumors were located in the head and neck, with the nose (33.1%), auricular region (18.5%), and periocular region the most commonly affected sites. The patient in the present case had a tumor located in the auricular region, had a very pale skin and worked in the sun due to his occupation as a farmer. The predilection of BSC for the head and neck region may be explained by the greater exposure to sunlight.[1,6]
There is a significant risk of local recurrence and metastasis with BSC, which is one the most aggressive types of BCC, considering its infiltrative growth and stromal reaction patterns.[7] Long-term follow-up for the detection of local recurrence and distant metastatic spread is recommended. Recurrence is often extremely aggressive and requires extensive resection.[8] In the present case, some metastatic cells were found invading blood vessels, indicating the aggressive potential of the tumor cells.
Excision of the lesion with a surgical margin was performed and the patient has been followed up for 6 months. According to Martin,[8] the more significant indicators of recurrence were positive surgical margins, lymphatic invasion, and perineural invasion, whereas the degree of differentiation and the size of the initial lesion were not significant. There is a high incidence rate of lymph node involvement and patients with perineural invasion have significantly higher rates of metastatic disease and local recurrence when compared to those without perineural invasion.
Conclusion
The importance of distinguishing BSC from SCC and BCC lies in its significant propensity to metastasize. Importantly, the correct and conclusive diagnosis always requires a biopsy.
![]()
Footnotes
Source of Support: Nil
Conflict of Interest: Nil
References
- 1.de Faria JL. Basal cell carcinoma of the skin with areas of squamous cell carcinoma: A basosquamous cell carcinoma? J Clin Pathol. 1985;38:1273–7. doi: 10.1136/jcp.38.11.1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Weedon D. Skin pathology. London: Churchill Livingstone; 2002. p. 1158. [Google Scholar]
- 3.Bowman PH, Ratz JL, Knoepp TG, Barnes CJ, Finley EM. Basosquamous carcinoma. Dermatol Surg. 2003;29:830–3. doi: 10.1046/j.1524-4725.2003.29217.x. [DOI] [PubMed] [Google Scholar]
- 4.Sendur N, Karaman G, Dikicioglu E, Karaman CZ, Savk E. Cutaneous basosquamous carcinoma infiltrating cerebral tissue. J Eur Acad Dermatol Venereol. 2004;18:334–6. doi: 10.1111/j.1468-3083.2004.00856.x. [DOI] [PubMed] [Google Scholar]
- 5.Johnson BF, Moore PJ, Goepel JR, Slater DN. Basosquamous carcinoma, a wolf in sheep's clothing. Report of 3 cases? Postgrad Med J. 1989;65:750–1. doi: 10.1136/pgmj.65.768.750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Leibovitch I, Huilgol SC, Selva D, Richards S, Paver R. Basosquamous carcinoma: Treatment with Mohs micrographic surgery. Cancer. 2005;104:170–5. doi: 10.1002/cncr.21143. [DOI] [PubMed] [Google Scholar]
- 7.Garcia C, Poletti E, Crowson AN. Basosquamous carcinoma. J Am Acad Dermatol. 2009;60:137–43. doi: 10.1016/j.jaad.2008.09.036. [DOI] [PubMed] [Google Scholar]
- 8.Martin RC, Edwards MJ, Cawte TG, Sewell CL, McMasters KM. Basosquamous carcinoma: Analysis of prognostic factors influencing recurrence. Cancer. 2000;88:1365–9. doi: 10.1002/(sici)1097-0142(20000315)88:6<1365::aid-cncr13>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 9.Schuller DE, Berg JW, Sherman G, Krause CJ. Cutaneous basosquamous carcinoma of the head and neck: A comparative analysis. Otolaryngol Head Neck Surg. 1979;87:420–7. doi: 10.1177/019459987908700405. [DOI] [PubMed] [Google Scholar]
- 10.Lopes de Faria J, Nunes PH. Basosquamous cell carcinoma of the skin with metastases. Histopathology. 1988;12:85–94. doi: 10.1111/j.1365-2559.1988.tb01919.x. [DOI] [PubMed] [Google Scholar]


