Abstract
Xeroderma pigmentosum (XP) is a rare autosomal recessive disorder related to defective deoxyribonucleic acid (DNA) repair. Various cutaneous manifestations related to ultraviolet (UV) damage characterize the clinical course. Primary malignant cutaneous neoplasms like squamous cell carcinoma, basal cell carcinoma and malignant melanoma have been reported. Atypical fibroxanthoma is a rare dermal neoplasm occurring in UV-damaged skin. We report an unusual case of atypical fibroxanthoma in a 20-year-old male with XP.
Keywords: Atypical fibroxanthoma, cutaneous neoplasm, xeroderma pigmentosum
Introduction
Xeroderma pigmentosum (XP) is a rare autosomal recessive disorder characterized by cutaneous photosensitivity, pigmentary changes, photophobia and propensity to develop early malignancy in sun-exposed skin and ocular structures.[1,2] The malignancies described commonly in patients with XP include squamous cell carcinoma (SCC), basal cell carcinoma (BCC), and malignant melanoma (MM).[3] Other types of cutaneous neoplasm including angiosarcoma and fibrosarcoma have also been reported.[1,4] Atypical fibroxanthoma (AFX) is a pleomorphic spindle cell neoplasm of the dermis that occurs in actinically damaged skin of elderly individuals. However, cases also have been reported occurring in the limbs and trunks of younger persons.[5,6] Histologically, it mimics malignant fibrous histiocytoma (MFH), but the tumor usually follows an indolent or locally aggressive course. Only a small number of metastatic cases have been reported. AFX has been regarded as the neoplasm of low-grade malignancy related to MFH. AFX in a patient of XP is very rare. A handful of cases have been reported in the literature.
Case Report
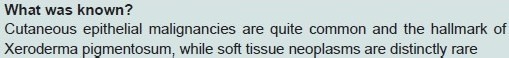
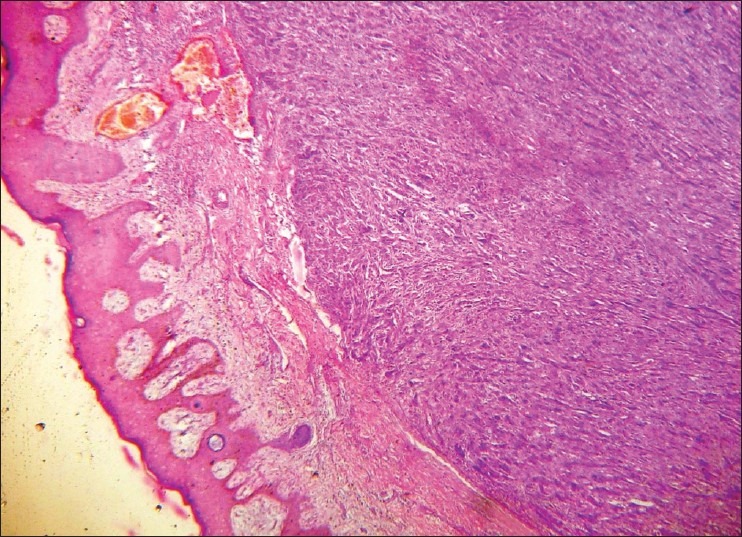
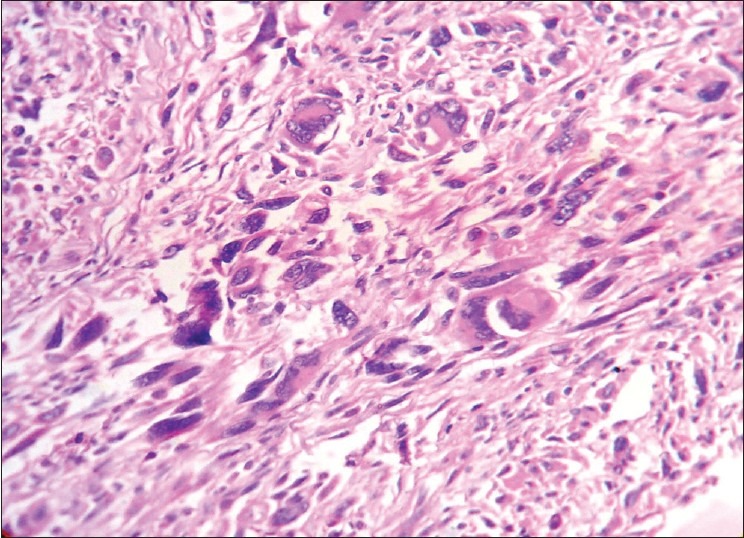
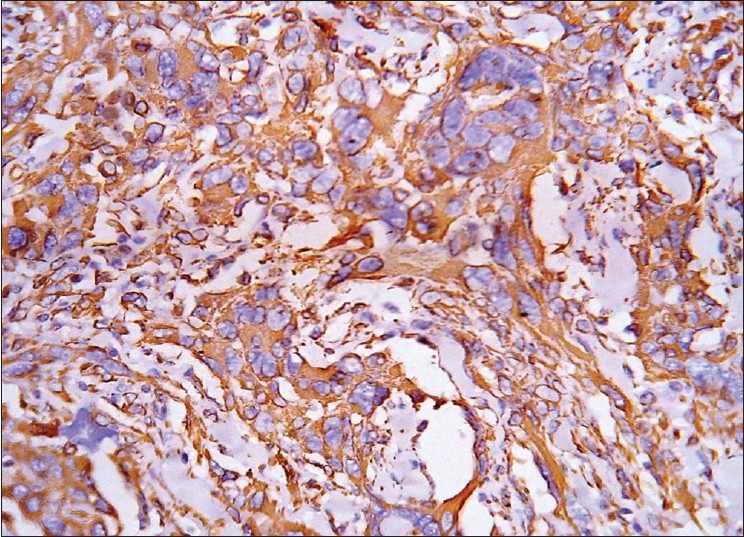
A 20-year-old man, farmer by occupation, presented with two tumors over his cheek. On examination, the patient showed pigmentation and depigmentation all over his body [Figure 1] which, according to him, were present since childhood. On further enquiry, he gave a history of six operations on his face over the last 4 years. On three occasions, the lesions were diagnosed as baso-squamous carcinoma, once as SCC, and on two occasions he developed BCC. Both his parents were phenotypically normal. He had five siblings out of which two were affected by the same disease process and died of metastasizing SCC. The other three, all younger to him, were phenotypically normal with no manifestation of the disease so far. During the present visit, two tumors were excised from his cheek. On gross examination, one of the tumors measured 3.5 × 2 × 2 cm and showed ulceration of the skin surface. The other tumor was well circumscribed and the skin over the tumor was intact. Histology of the first tumor showed features of a baso-squamous carcinoma. Sections showed a relatively well-circumscribed mass with tumor cells occupying papillary and reticular dermis. The overlying epidermis was intact [Figure 2]. The tumor cells comprised polygonal- to spindle-shaped cells with bizarre and multinucleated tumor giant cells showing marked pleomorphism [Figure 3]. Mitotic figures were present but not brisk. With the differential of a poorly differentiated epithelial neoplasm and a soft tissue tumor in mind, immunohistochemistry was performed and the cells showed strong positivity for vimentin [Figure 4], and were negative for pancytokeratin, S-100 and HMB45. The tumor cells also showed positivity for CD68 [Figure 5], suggesting a histiocytic differentiation. Taking into account the gross, histomorphologic, and immunohistochemical features, a diagnosis of AFX was made. In the 8-month follow-up period, the patient did not develop any metastases.
Figure 1.

Mottled pigmented and depigmented areas of facial skin along with scars of previous surgeries
Figure 2.
Photomicrograph showing a well-circumscribed dermal neoplasm with intact epidermis (Hematoxylin and Eosin, ×40)
Figure 3.
Photomicrograph showing highly pleomorphic spindle-shaped cells with bizarre giant cells (H and E, ×400)
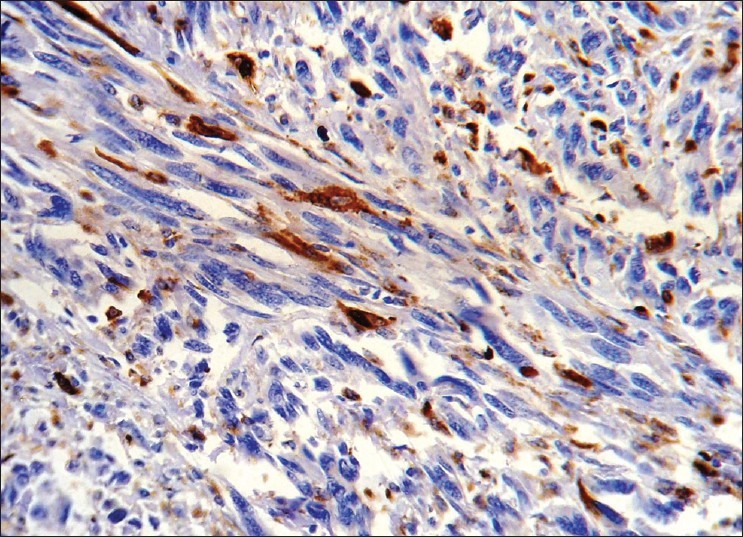
Figure 4.
Photomicrograph showing tumor cells expressing vimentin (Immunohistochemistry for vimentin, ×400)
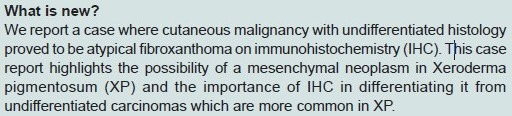
Figure 5.
Photomicrograph showing tumor cells expressing CD68 (Immunohistochemistry for CD68, ×400)
Discussion
XP is an autosomal recessive disorder characterized by defective deoxyribonucleic acid (DNA) repair.[7] It has a prevalence of 1 in 250,000.[1,2] To date, the precise mechanism of XP is not known. The skin cells from patients with XP have an impaired ability to repair ultraviolet (UV)-induced DNA damage.[8] Defective DNA repair is also reflected in dermal fibroblasts, lymphocytes of peripheral blood, and conjunctival cells. XP being an autosomal recessive disease, the heterozygous parents are normal and both the sexes are equally affected. In the present case, out of five siblings of the patient, two were affected by the same disease process and succumbed to repeated development of SCC.
Malignant skin neoplasms have been reported in 45-60% of XP patients in different studies.[1,2] The skin neoplasms include SCC, BCC, and MM. Other malignancies including carcinoma of tongue have been reported. Robbins has shown 10-20 times higher incidence of internal neoplasm in XP patients compared to normal controls.[9] But soft tissue tumors are very rare in these patients. Only five cases of fibrosarcomas, three angiomas, two AFX, two MFH, and one angiosarcoma have been demonstrated so far.[1,3,10–12]
The histogenesis of AFX is controversial. However, electron microscopic and immunohistochemical studies indicate that as for MFH, the progenitor cell is an undifferentiated mesenchymal cell, capable of showing histiocytic, fibroblastic, and myofibroblastic differentiation.[13,14] The concept that AFX is a form of pleomorphic MFH has received further support from a study in which no significant difference between AFX and MFH was demonstrated in their apoptotic behavior, proliferation indices, p53 protein expression and presence of the bcl2 product. Despite marked cytological atypia, Dilek et al. have found few mitotic figures in AFX.[3] Similarly, in our case we could detect only modest increase in mitotic figures. However, other studies have shown numerous mitotic figures including abnormal forms.[5] Despite its apparently malignant histologic features, the tumor usually follows an indolent or locally aggressive course. Due to the small number of metastatic cases reported, AFX has been regarded as the neoplasm of low-grade malignancy related to MFH from which it is indistinguishable histologically.[13] According to this view, the more favorable prognosis of AFX is related to its superficial location and small size.[15]
The data regarding the outcome of AFX are mostly available from the cases not associated with XP. The outcome of the cases of AFX in patients with XP has not been discussed in literature. The differential diagnosis in the present case, occurring in a patient of XP, included a poorly differentiated epithelial neoplasm. Immunohistochemistry for cytokeratin, S100, vimentin, and CD68 helped confirmation of the diagnosis. Dilek et al. have recommended cytokeratin, S100, HMB45, and histiocytic markers in difficult cases.[3] Cases of AFX are usually associated with severe actinic damage and few have arisen in areas treated by radiation. Deficient repair of UV-induced DNA damage is directly involved in the development of cancer in XP.[3]
Footnotes
Source of Support: Nil
Conflict of Interest: Nil
References
- 1.Kraemer KH, Lee MM, Scotto J. Xeroderma pigmentosum - cutaneous, ocular and neurologic abnormalities in 830 published cases. Arch Dermatol. 1987;123:241–50. doi: 10.1001/archderm.123.2.241. [DOI] [PubMed] [Google Scholar]
- 2.Robbins JH, Kraemer KH, Lutzner MA, Festoff BW, Coon HG. Xeroderma pigmentosum. Ann Intern Med. 1974;80:221–48. doi: 10.7326/0003-4819-80-2-221. [DOI] [PubMed] [Google Scholar]
- 3.Dilek FH, Akpolat N, Metin A, Ugras S. Atypical fibroxanthoma of skin and lower lip in xeroderma pigmentosum. Br J Dermatol. 2000;143:618–20. doi: 10.1111/j.1365-2133.2000.03721.x. [DOI] [PubMed] [Google Scholar]
- 4.Lambert WC, Kuo H, Lambert MW. Xeroderma pigmentosum. Dermatol Clin. 1995;13:169–209. [PubMed] [Google Scholar]
- 5.Vargas-Cortes F, Winkelmann RK, Soule EH. Atypical fibroxanthoma of the skin. Mayo Clin Proc. 1973;48:211–28. [PubMed] [Google Scholar]
- 6.Dahl I. Atypical fibroxanthoma of the skin. Acta Pathol Microbiol Imuunol Scand. 1976;84:183–97. [PubMed] [Google Scholar]
- 7.Goyal JL, Rao VA, Srinivasan R, Agrawal K. Oculocutaneous manifestation in xeroderma pigmentosum. Br J Ophthalmol. 1994;78:295–7. doi: 10.1136/bjo.78.4.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cleaver JE. Defective repair replication of DNA in XP. Nature. 1968;218:652–6. doi: 10.1038/218652a0. [DOI] [PubMed] [Google Scholar]
- 9.Robbins JH. Xeroderma pigmentosum: Defective DNA repair causes skin cancer and neurodegeneration. JAMA. 1988;260:384–8. doi: 10.1001/jama.260.3.384. [DOI] [PubMed] [Google Scholar]
- 10.Patterson JW, Jordan WP. Atypical fibroxanthoma in a patient with xeroderma pigmentosum. Arch Dermatol. 1987;123:1066–70. [PubMed] [Google Scholar]
- 11.Pe’er J, Levinger S, Chirambo M, Ron N, Okon E. Malignant fibrous histiocytoma of the skin and the conjunctiva in xeroderma pigmentosum. Arch Pathol Lab Med. 1991;115:910–4. [PubMed] [Google Scholar]
- 12.Leake J, Sheehan MP, Rampling D, Ramani P, Atherton DJ. Angiosarcoma complicating xeroderma pigmentosum. Histopathology. 1992;21:179–81. doi: 10.1111/j.1365-2559.1992.tb00370.x. [DOI] [PubMed] [Google Scholar]
- 13.Barr RJ, Wuerker RB, Graham JH. Ultrastructure of atypical fibroxanthoma. Cancer. 1977;40:736–43. doi: 10.1002/1097-0142(197708)40:2<736::aid-cncr2820400222>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 14.Longacre TA, Smoller BR, Rouse RU. Atypical fibroxanthoma: Multiple immunohistologic profiles. Am J Surg Pathol. 1993;17:1199–2009. doi: 10.1097/00000478-199312000-00001. [DOI] [PubMed] [Google Scholar]
- 15.Westermann FN, Langlois NEI, Simpson JG. Apoptosis in atypical fibroxanthoma and pleomorphic malignant fibrous histiocytoma. Am J Dermatopathol. 1997;19:228–31. doi: 10.1097/00000372-199706000-00005. [DOI] [PubMed] [Google Scholar]


