Abstract
Aims
Care management may improve the quality of diabetes care by enhancing contact between high-risk patients and their providers. This prospective, longitudinal, randomized trial sought to investigate whether telephone or online care management improves diabetes-related outcomes over time compared with usual care supplemented with Internet access and training.
Subjects and Methods
One hundred fifty-one adult subjects with type 2 diabetes mellitus and an elevated hemoglobin A1c (A1c) level (≥8.5%) were randomly assigned to online care management (n=51), telephone-based care management (n=51), or Web training (n=49) groups. Online and telephone participants interacted with a care manager through a diabetes education and care management Web site and by telephone, respectively. The Web training group was provided with online diabetes self-management resources but no care management support. The primary outcome measure was A1c measured every 3 months for a year.
Results
A1c declined significantly and substantially in all groups over 12 months. A1c declined linearly at a rate of 0.32% (P<0.0001) per quarter for the online group, 0.36% (P<0.0001) for the telephone group, and 0.41% for the Web training group (P<0.0001). The rate of change over time did not differ significantly among groups. The groups converged at 12 months with average absolute A1c difference of −1.5%. The number of interactions with care providers was not significantly associated with the change in A1c. Blood pressure, weight, lipid levels, and diabetes distress did not differ among groups over time.
Conclusions
Online, telephone-based care management, and Web training for diabetes patients with elevated A1c were each associated with a substantial improvement in A1c over a 1-year period. Internet access and training alone may be as effective as care management in patients with poorly controlled diabetes.
Introduction
Diabetes is a major component of healthcare expenditures in the United States.1,2 Poor control of glucose, blood pressure, and lipids in patients with diabetes is associated with substantially increased healthcare utilization and cost. In an attempt to address these high-risk, high-cost patients, many healthcare systems have employed care management programs and have engaged nurses or other allied health professionals (e.g., pharmacists, nutritionists) as the point of contact for patients.
As with most chronic diseases, the vast majority of diabetes-related self-care and activity occurs outside the healthcare setting. Nevertheless, traditional models of patient education and care management require that encounters between care managers and patients occur at times convenient for both individuals. Scheduling and travel are potential barriers to completing these connections. Online tools could potentially neutralize geographic and scheduling barriers.3 Patients and providers are increasingly using online platforms to communicate and learn. Online care allows patients to retain a relationship with their primary care provider between visits and can reinforce and track the assigned goals for each patient by facilitating communication and data transfer. We previously demonstrated that online care management can be a useful adjunct in the care of patients with poorly controlled diabetes and can improve the attainment of diabetes goals.4 Nevertheless, few studies have compared the efficacy of different implementation strategies on clinical outcomes in patients with diabetes.
Even in the most successful trials of diabetes care management, many participants do not attend or participate in all sessions. Thus, it is useful to examine the range of different models for effectively engaging patients in their care.5 Some care management programs have demonstrated significant system-wide cost savings despite increased costs in the subcategories of pharmacy and care management administration, but others have not.6–9 Randomized and nonrandomized interventions have shown some efficacy in lowering hemoglobin A1c (A1c), but there are limited data on the efficacy of care management for individual patients.10–17 Consequently the benefits of care management approaches have been questioned. This is particularly relevant as self-management information has become increasingly ubiquitous online where communities of patients can engage in reinforcing group interactions while tracking a range of health outcomes.5,10,18
In this study we examined the efficacy of two methods of diabetes education and care management for patients with particularly poorly controlled diabetes: a traditional model that involved face-to-face encounters and telephone contact and an online model that facilitated asynchronous online communication and data sharing. We compared these interventions with an Internet access and training (“Web training”) group that was directed to a series of diabetes self-management Web sites. We tested the hypotheses that active care management in patients with elevated A1c levels (≥8.5%) using traditional or online methods would (1) reduce A1c levels, (2) improve cardiovascular risk factors, and (3) reduce diabetes-related distress when compared with usual care supplemented with Web training over a 12-month period.
Subjects and Methods
Study protocol
The study was conducted at the Department of Veterans Affairs (VA) Boston Healthcare System. The protocol was reviewed and approved by the Institutional Review Board, and informed, written consent was obtained from each participant. Eligibility criteria included A1c level >8.5%, age >25 years, ability to understand written and spoken English, access to a telephone, and willingness to use a notebook computer and glucose and blood pressure monitoring devices. Participants were required to have a VA-based primary care provider at one of four hospital-based clinics or 10 community-based outpatient clinics.
For recruitment, hospital laboratory data were screened monthly to identify individuals age >25 years and with a recent A1c level encompassing or within 0.5% of the A1c inclusion criterion. Potential participants were sent a letter and/or brochure describing the study, and follow-up telephone calls were attempted at least 2 weeks later to solicit participation. Following in-person screening, eligible participants attended an additional information session to review the study design. Participants were then randomized to one of three study groups through the use of a random number generator and a series of sealed envelopes. Those assigned to the groups afforded computer use received in-person orientation and training.
Telephone-based care management group
Participants randomized to telephone-based care management were given monitoring devices for glucose (AccuChek® Advantage; Roche Diagnostics, Indianapolis, IN) and blood pressure measurements (Omron Medical, North Bend, WA). An advanced practice nurse or clinical pharmacist met with each patient and used a care management intervention and follow-up schedule based on a previously published report.19 Both care managers were Certified Diabetes Educators and between them had 30 years of experience in care management.
Participants assigned to this group met with the care manager for an initial assessment to review glucose and blood pressure monitoring techniques and schedules and received instruction in the core content areas suggested by the American Diabetes Association.20 Care managers used integrated case management software to log and track results (CDMP; Estenda Solutions, Conshohocken, PA). Interim follow-up telephone calls occurred approximately biweekly during which the care manager reviewed the home glucose and blood pressure readings with the participant. These care manager–participant contacts were used to review progress, reinforce nutritional and lifestyle modifications, and make medication changes using the treatment algorithms that were developed from and were consistent with the standards of the American Diabetes Association.20 Medications were adjusted by the care managers and affirmed by the participant's primary care provider, who then implemented the medication changes through the hospital pharmacy.
Online care management group
Participants randomized to online care management received a notebook computer and Internet access, if needed, and the same glucose and blood pressure monitors provided to the telephone-based care management group. Subjects also met with one of the two care managers and were encouraged to perform blood pressure monitoring at least three times weekly; recommendations for glucose testing were individualized for each patient. Participants in this study arm were asked to log-in to the patient portal of an Internet-based care management application at least biweekly. The care management application had a provider portal that allowed the care managers to review a patient panel, assign educational modules covering medications, nutrition, exercise, glucose monitoring, and well-being, review uploaded glucose and blood pressure monitoring data, and communicate securely with the patient via an internal messaging system. The program provided interpretations of the participant's progress using a combination of biochemical data downloaded from the hospital laboratory and process indicators (including vaccinations and foot and dilated eye examinations during the preceding 12 months) provided by the clinician. The care manager used the same medication algorithms as in the telephone-based care management arm and communicated with primary care providers regarding medication changes. Contact with patients was primarily through the sending and receiving of messages via the Web site or, if necessary, through telephone contact. We provided telephone reminders to participants who had not logged into the website within 2 weeks to encourage Web site usage.
Usual care supplemented with Internet access and online self-management resources (“Web training”)
Participants randomized to the Web training group were provided with a laptop computer and Internet access with training in the use of the device as necessary. The home page of the computer's Internet browser was set to a diabetes education Web site designed for the study, containing links to several Web sites with vetted content related to diabetes self-management including sites that facilitated peer-sharing and mutual support. Utilization of these resources was at the private discretion of the patient, and study staff had contact with these participants only to arrange and conduct follow-up visits for the collection of outcome measures.
For all three groups, the follow-up visits occurred every 3 months. Regardless of study group, all participants continued with ongoing care from their primary care provider as determined by their clinical needs.
Outcome measures
The primary outcome measures were change in A1c and blood pressure over time. These outcome measures were collected at baseline and 3, 6, 9, and 12 months after randomization. A1c was measured with methodology that utilized a nonporous ion-exchange high-performance liquid chromatography to separate A1c from other hemoglobin fractions and is certified by the National Glycohemoglobin Standardization Program. Blood pressure was measured with the patient in the seated position after a 5-min rest using an appropriately sized cuff and an automated sphygmomanometer. Three readings were taken 1 min apart, and analyses used the average of these three readings. Fasting serum samples were assayed for cholesterol, its subfractions, and triglycerides using standard laboratory techniques. We analyzed lipid profiles obtained at baseline and 12 months. The patients' primary care providers were generally masked to clinical outcome measures unless they requested access to specific test results to avoid duplicate laboratory testing.
Diabetes distress was measured at baseline and 12 months using the Problem Areas in Diabetes (PAID) questionnaire.21,22 The PAID comprises 20 items, incorporating questions regarding feelings of guilt, anxiety, worry, loneliness, and burnout from diabetes, feelings about diabetes care providers, and level of comfort with social situations, among other things. Each item is coded to indicate the severity of a problem (0=not a problem to 4=serious problem), and the total score for the instrument varies from 0 to 100.
Data on process measures (including number of Web site interactions, number of encounters, and time spent by the care managers per patient encounter) and changes in diabetes and antihypertensive medications were collected every 3 months and analyzed as possible explanations for interindividual differences in change over time in the primary outcomes. Medications prescribed for glucose, lipid, and blood pressure control were tracked at each visit, and clinic and emergency room visits were counted.
Statistical analyses
The goal of the analyses was to compare outcome measures among the telephone-based care management group, the online care management group, and the Web training group. For participants who missed study visits or did not respond to all questions, the study carried forward the last or most recent observations. However, if subjects were missing data at baseline, as was the case for several subjects who were missing baseline lipid values, we did not carry forward observations. We minimized missing data by including A1c data from the medical record for patients who missed follow-up visits but had lab tests within the required time frame for the study protocol.
The analyses first compared the study participants' baseline characteristics using one-way analysis of variance for continuous variables and χ2 tests for qualitative variables. The analyses then compared baseline and 12-month values for the outcomes—within each study group—using paired t tests. Lastly, the analyses examined trajectories of the groups' outcome measures using multilevel models for longitudinal data (PROC MIXED, SAS version 9.2; SAS Institute, Cary, NC). These models included time effects and the interaction of time effects with treatment group to detect within-individual differences as well as differences in the rate of change in the outcomes between the groups over the course of the study. As needed, the analyses included baseline characteristics, usage of the care management portal, and contacts with care managers. All analyses were “intent-to-treat.”
Results
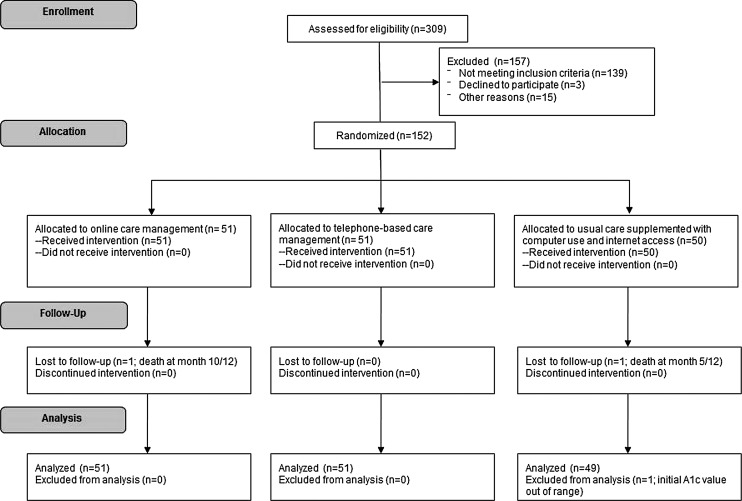
The study enrolled 151 participants (Fig. 1). Table 1 shows baseline characteristics of the study participants according to randomization group. Participants had a mean age of 60 years, 95% were male, 90% had completed a high school education, and 49% had a diabetes diagnosis for >10 years. In the online care, telephone care, and Web training groups, 47, 44, and 41 subjects completed the trial, respectively. Computer training and support were provided for a mean total of 122.4 min (range, 0–256 min) per subject in the Web training and online care groups.
FIG. 1.
Flow of patients through the study. A1c, hemoglobin A1c.
Table 1.
Baseline Characteristics
| Parameter | Total (n=151) | Web training (n=49) | Telephone care (n=51) | Online care (n=51) | Pa |
|---|---|---|---|---|---|
| Age (years) [mean (SD)] | 60.2 (10.8) | 58.9 (10.2) | 58.5 (11.5) | 63.0 (10.5) | 0.07 |
| Male (%) | 94.7 | 95.9 | 98.0 | 90.2 | 0.19 |
| Race/ethnicity (%) | |||||
| Non-Hispanic white | 74.2 | 69.4 | 74.5 | 78.4 | 0.93 |
| Non-Hispanic black | 12.6 | 12.2 | 11.8 | 13.7 | |
| Hispanic | 9.3 | 12.2 | 9.8 | 5.9 | |
| Other | 2.7 | 4.1 | 2.0 | 2.0 | |
| No response | 1.3 | 2.0 | 2.0 | 0.0 | |
| Employment status (%) | |||||
| Employed | 23.8 | 20.4 | 17.7 | 33.3 | 0.26 |
| Retired | 57.0 | 57.1 | 58.8 | 54.9 | |
| Other | 19.1 | 22.5 | 23.5 | 11.8 | |
| Marital status (%) | |||||
| Married/partnered | 49.0 | 40.8 | 52.9 | 52.9 | 0.50 |
| Separated/divorced or widowed | 32.5 | 30.6 | 33.3 | 33.3 | |
| Single | 14.6 | 22.5 | 11.8 | 9.8 | |
| No response | 4.0 | 6.1 | 2.0 | 3.9 | |
| Highest grade completed (%) | |||||
| Less than high school graduate | 9.5 | 14.9 | 6.1 | 7.8 | 0.52 |
| Completed high school | 28.6 | 31.9 | 28.6 | 25.5 | |
| Some college | 36.1 | 31.9 | 42.9 | 33.3 | |
| College graduate or higher | 25.9 | 21.3 | 22.5 | 33.3 | |
| Years since diabetes diagnosis (%) | |||||
| Less than 1 year | 2.1 | 2.3 | 2.1 | 2.0 | 0.91 |
| 1–5 years | 19.0 | 25.0 | 16.7 | 16.0 | |
| 6–10 years | 29.6 | 27.3 | 27.1 | 34.0 | |
| More than 10 years | 49.3 | 45.5 | 54.2 | 48.0 | |
P values are from one-way analysis of variance (continuous variables) and χ2 tests (categorical variables).
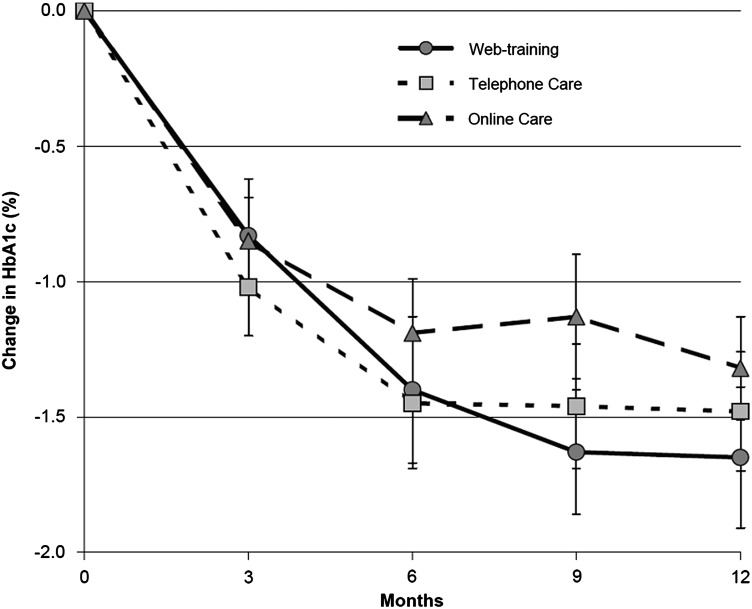
Baseline A1c levels for participants in the online care management, telephone-based care management, and Web training groups were 9.5%, 9.8%, and 10.0%, respectively. As shown in Table 2, there was a marked and significant decrease in A1c in all study groups over the 12-month period with most of the change occurring within the first 6 months (Fig. 2). Also, from the multilevel models, A1c declined linearly from baseline at a rate of 0.32% per 3-month interval for the online group (P<0.0001 for the null hypothesis of no change from baseline), 0.36% (P<0.0001) for the telephone group, and 0.41% for the Web training group. The rate of change over time did not differ significantly between groups (P=0.12 for the online care group compared with the Web training group and P=0.35 for the telephone care group compared with the Web training group), suggesting no significant intervention effects. The groups converged at the end point with average A1c between 8.3% and 8.4% after 12 months in the trial.
Table 2.
Changes in Outcome Variables over a 12-Month Period
| Parameter | Baseline | 12 months | Differencea | Pb |
|---|---|---|---|---|
| A1c (%) | ||||
| Online care | 9.6±1.0 | 8.3±1.1 | −1.3±1.4 | <0.0001 |
| Telephone care | 9.9±1.2 | 8.5±1.6 | −1.5±1.6 | <0.0001 |
| Web training | 10.1±1.4 | 8.4±1.7 | −1.7±1.8 | <0.0001 |
| Systolic BP (mm Hg) | ||||
| Online care | 135.6±17.4 | 135.2±19.2 | −0.3±16.9 | 0.891 |
| Telephone care | 139.9±17.4 | 133.2±17.1 | −6.7±16.7 | 0.006 |
| Web training | 139.8±19.1 | 136.7±19.3 | −3.1±20.4 | 0.297 |
| Diastolic BP (mm Hg) | ||||
| Online care | 75.7±11.8 | 73.2±10.7 | −2.5±12.9 | 0.178 |
| Telephone care | 80.8±13.1 | 74.6±10.7 | −6.3±11.5 | 0.001 |
| Web training | 83.1±15.8 | 77.3±11.5 | −5.8±15.5 | 0.012 |
| Total cholesterol (mg/dL) | ||||
| Online care | 172.3±35.9 | 164.6±32.7 | −7.8±29.3 | 0.071 |
| Telephone care | 167.6±42.7 | 158.3±35.1 | −8.5±29.3 | 0.048 |
| Web training | 174.0±38.2 | 163.1±38.0 | −10.7±29.8 | 0.019 |
| LDL (mg/dL) | ||||
| Online care | 95.1±29.4 | 92.4±27.4 | −4.0±25.8 | 0.290 |
| Telephone care | 91.7±37.8 | 85.9±27.1 | −5.5±24.1 | 0.122 |
| Web training | 92.5±32.3 | 86.3±29.4 | 5.8±24.6 | 0.118 |
| HDL (mg/dL) | ||||
| Online care | 39.1±10.6 | 39.7±11.6 | 0.8±6.8 | 0.413 |
| Telephone care | 39.0±12.0 | 37.2±11.2 | −2.1±4.1 | 0.001 |
| Web training | 38.1±10.0 | 38.0±10.2 | −0.2±5.7 | 0.848 |
| Triglycerides (mg/dL) | ||||
| Online care | 190.5±85.8 | 163.6±75.1 | −25.5±66.3 | 0.010 |
| Telephone care | 186.4±127.6 | 176.3±133.4 | −6.5±108.7 | 0.676 |
| Web training | 225.5±139.6 | 197.2±117.7 | −26.4±98.5 | 0.076 |
| Weight (pounds) | ||||
| Online care | 232.9±46.2 | 234.3±48.0 | 1.4±13.5 | 0.458 |
| Telephone care | 235.2±55.3 | 239.1±55.7 | 4.0±14.8 | 0.062 |
| Web training | 235.6±52.2 | 237.5±48.8 | 0.7±15.1 | 0.747 |
| BMI (kg/m2) | ||||
| Online care | 34.4±6.1 | 34.5±6.2 | 0.2±2.1 | 0.551 |
| Telephone care | 33.7±7.3 | 34.3±7.4 | 0.6±2.2 | 0.066 |
| Web training | 34.2±7.0 | 34.3±6.4 | 0.1±2.2 | 0.725 |
| Diabetes distress | ||||
| Online care | 21.8±21.0 | 19.2±18.5 | 1.8±10.7 | 0.271 |
| Telephone care | 24.5±20.0 | 18.3±15.7 | 6.2±15.0 | 0.008 |
| Web training | 29.0±19.6 | 19.5±14.8 | 8.0±15.6 | 0.003 |
Difference scores were computed for subjects with complete data at baseline. This limitation applied to the lipid values and distress scores only. Rounding affected the difference scores slightly for some parameters.
P values are from paired t tests comparing baseline means with 12-month means within each study group.
A1c, hemoglobin A1c; BMI, body mass index; BP, blood pressure; HDL, high-density lipoprotein; LDL, low-density lipoprotein.
FIG. 2.
Change in hemoglobin A1c (HbA1c) in each of the three study groups over time.
We also examined A1c responses in the 54 (36%) patients with markedly elevated A1c levels (≥10%). Again, all study groups had similar results, with significant (P<0.001) declines in A1c (−2.4% to −2.6%) but no between-group differences.
The engagement of patients with care managers in the intervention groups was not clearly associated with the reduction in A1c or any other health outcome assessed. We separated participants into groups with varying amounts of contact with care managers over the course of the study. Participants in the telephone care group with ≤3 (23%), 4–6 (29%), 7–9 (37%), and >9 (10%) months of successful care manager contact had, respectively, quarterly A1c differences over 12 months of −1.3%, −1.7%, −1.5%, and −1.1%. Participants in the online care group with ≤3 (18%), 4–6 (24%), 7–9 (47%), and >9 (12%) months of successful care manager contact had A1c differences over 12 months of −0.2%, −1.4%, −1.8%, and −0.8%, respectively.
With regard to engagement with the care management Web site, participants in the online care group with ≤3 (18%), 4–6 (14%), 7–9 (25%), and >9 (43%) months of logins to the care management site had, respectively, quarterly A1c differences over 12 months of −0.6%, −1.3%, −1.7%, and −1.5%. Participants with the highest and the lowest frequency of logins had similar changes in A1c.
Changes in parameters were assessed within study groups. Systolic and diastolic blood pressures significantly decreased within the telephone care group, diastolic blood pressure, total cholesterol, and diabetes distress significantly decreased within the telephone care and Web training groups, high-density lipoprotein cholesterol significantly decreased within the telephone care group, and triglycerides significantly decreased within the online care group (Table 2). Weight increased similarly in all groups, ranging from 0.7 to 4.0 pounds. According to the multilevel model results, none of these parameters was significantly different among groups over time. The frequency of provider contacts and usage of the care management portal were not associated with changes in these variables.
Discussion
In this study we evaluated the effectiveness of two care management strategies in patients with elevated A1c in comparison with a Web training group that was provided with a computer and Internet access. Over a 12-month period, A1c improved by 1.2% or greater among all study groups whether or not active care management was offered. The results of this study show that telephone or online care management offered no additional benefits for a variety of diabetes outcomes compared with training in the use of online self-management resources.
Our study suggests that providing access to online resources for patients with poorly controlled diabetes improves outcomes to the same degree as active care management. This builds on prior studies that demonstrated the efficacy of engaging patients in their self-care.7–9 We and others have previously shown that self-management education alone can result in significant improvement in A1c and that online care management is associated with significantly reduced A1c compared with usual care in patients with poorly controlled diabetes.4,10,23–25 A meta-regression analysis of quality improvement strategies in patients with diabetes suggested that case management by individuals with expanded roles (e.g., advanced practice nurses or clinical pharmacists) resulted in significant declines in A1c.26 It has not been previously possible to determine which component of the provided care leads to the improvement in diabetes measures.
With the growing ubiquity of online resources to help keep patients engaged in self-care for chronic diseases, this study builds on prior research that suggests that directing patients to these online resources and providing training in its use may have an important role in chronic disease management.18,27 The robust A1c responses in each group, with an average 1.5% A1c decrement, support the efficacy of improving self-efficacy using online technology.
Web-based learning can benefit both patients and their care providers because time between visits can be used effectively and efficiently to learn self-supporting behaviors that reinforce clinician recommendations. The patient can use these resources and engage in peer-sharing to learn to overcome barriers and to self-document activities. An emerging array of studies has demonstrated that the most effective online self-management education and support programs are rich in content, provide engaging interactive elements, and can tailor the learning to a patient's individual needs.3,10 Encouraging patients to access a series of informational Web sites is substantially less resource intensive than care management. The results of this study suggest that facilitating access to online information is likely to be much more cost-effective than active care management.
Several factors should be considered in interpreting the results of this study. Although we used broad eligibility criteria to produce potentially generalizable findings, the education level of study participants was fairly high, with only 9.5% of participants having less than high school education and 25.6% having completed college. Thus, the enrolled participants may have self-selected into the study because of its focus on online interventions, and this may have affected their use of online resources. Small sample sizes limit the ability to perform more detailed subgroup analyses. The study hypothesis required an open-label design, and participating in a study may itself have prompted behavioral changes that affected outcomes similarly in all groups. In addition, diabetes care in the VA system has improved substantially over time, attributed to increased use and dissemination of performance measures, clinical reminders, and data tracking.28–30 The study was conducted during a period of system-wide declines in A1c. These possibilities would bias the study in favor of similar improvement across groups and in favor of the null hypothesis of no differences between groups.
Our results do raise questions whether care management, regardless of its delivery method, contributes substantively to the care of patients with poorly controlled diabetes above and beyond the gains attained by connecting patients with supporting resources. These results reinforce the imperative to perform appropriately controlled, randomized studies before assuming that care management technologies are cost-effective regardless of how novel the technology may appear. Clinical programs seeking to augment and improve diabetes care may be more effective when efforts are channeled to increasing information exchange and engagement of patients with their own disease management. These results support our prior findings that patient engagement is a key factor driving improved glucose control, and our results indicate that improvement in diabetes care measures may be naive to the mode of engagement.
In summary, the results from this study show that in patients with elevated A1c, active care management whether delivered via telephone or online methods has no significant additional benefit compared with access and training in the use of online diabetes self-management resources. An important implication of these results is that simple measures to improve self-efficacy by engaging patients in the use of self-management resources may be just as effective as active care management.
Acknowledgments
The authors would like to acknowledge the generous participation of patients and the collaborative support of providers within the VA Boston Healthcare System. The study was supported by grants from VA Health Services Research and Development (TEL-02-100), National Institutes of Health (K24 DK063214), and the Department of the Army Cooperative Agreement (DAMD 17-98-2-8017).
Author Disclosure Statement
No competing financial interests exist. G.M. and S.F. researched data and wrote the manuscript. H.G. researched data and contributed to the discussion. G.A. researched data and contributed discussion. P.C. researched data, contributed to the discussion, and reviewed/edited the manuscript.
References
- 1.Wang YC. McPherson K. Marsh T. Gortmaker SL. Brown M. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet. 2011;378:815–825. doi: 10.1016/S0140-6736(11)60814-3. [DOI] [PubMed] [Google Scholar]
- 2.Zhang P. Zhang X. Brown J. Vistisen D. Sicree R. Shaw J. Nichols G. Global healthcare expenditure on diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87:293–301. doi: 10.1016/j.diabres.2010.01.026. [DOI] [PubMed] [Google Scholar]
- 3.Kaufman N. Internet and information technology use in treatment of diabetes. Int J Clin Pract Suppl. 2010;(166):41–46. doi: 10.1111/j.1742-1241.2009.02277.x. [DOI] [PubMed] [Google Scholar]
- 4.McMahon GT. Gomes HE. Hickson Hohne S. Hu TM. Levine BA. Conlin PR. Web-based care management in patients with poorly controlled diabetes. Diabetes Care. 2005;28:1624–1629. doi: 10.2337/diacare.28.7.1624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kaufman ND. Woodley PD. Self-management support interventions that are clinically linked and technology enabled: can they successfully prevent and treat diabetes? J Diabetes Sci Technol. 2011;5:798–803. doi: 10.1177/193229681100500335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eland-de Kok P. van Os-Medendorp H. Vergouwe-Meijer A. Bruijnzeel-Koomen C. Ros W. A systematic review of the effects of e-health on chronically ill patients. J Clin Nurs. 2011;20:2997–3010. doi: 10.1111/j.1365-2702.2011.03743.x. [DOI] [PubMed] [Google Scholar]
- 7.Steffens B. Cost-effective management of type 2 diabetes: providing quality care in a cost-constrained environment. Am J Manag Care. 2000;6(13 Suppl):S697–S703. discussion S704–S699. [PubMed] [Google Scholar]
- 8.Sidorov J. Shull R. Tomcavage J. Girolami S. Lawton N. Harris R. Does diabetes disease management save money and improve outcomes? A report of simultaneous short-term savings and quality improvement associated with a health maintenance organization-sponsored disease management program among patients fulfilling health employer data and information set criteria. Diabetes Care. 2002;25:684–689. doi: 10.2337/diacare.25.4.684. [DOI] [PubMed] [Google Scholar]
- 9.Wakefield BJ. Holman JE. Ray A. Scherubel M. Adams MR. Hillis SL. Rosenthal GE. Effectiveness of home telehealth in comorbid diabetes and hypertension: a randomized, controlled trial. Telemed J E Health. 2011;17:254–261. doi: 10.1089/tmj.2010.0176. [DOI] [PubMed] [Google Scholar]
- 10.Samoocha D. Bruinvels DJ. Elbers NA. Anema JR. van der Beek AJ. Effectiveness of web-based interventions on patient empowerment: a systematic review and meta-analysis. J Med Internet Res. 2010;12:e23. doi: 10.2196/jmir.1286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lorig K. Ritter PL. Laurent DD. Plant K. Green M. Jernigan VB. Case S. Online diabetes self-management program: a randomized study. Diabetes Care. 2010;33:1275–1281. doi: 10.2337/dc09-2153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Heisler M. Vijan S. Makki F. Piette JD. Diabetes control with reciprocal peer support versus nurse care management: a randomized trial. Ann Intern Med. 2010;153:507–515. doi: 10.7326/0003-4819-153-8-201010190-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shea S. Weinstock RS. Teresi JA. Palmas W. Starren J. Cimino JJ. Lai AM. Field L. Morin PC. Goland R. Izquierdo RE. Ebner S. Silver S. Petkova E. Kong J. Eimicke JP. A randomized trial comparing telemedicine case management with usual care in older, ethnically diverse, medically underserved patients with diabetes mellitus: 5 year results of the IDEATel study. J Am Med Inform Assoc. 2009;16:446–456. doi: 10.1197/jamia.M3157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Piette JD. Weinberger M. Kraemer FB. McPhee SJ. Impact of automated calls with nurse follow-up on diabetes treatment outcomes in a Department of Veterans Affairs Health Care System: a randomized controlled trial. Diabetes Care. 2001;24:202–208. doi: 10.2337/diacare.24.2.202. [DOI] [PubMed] [Google Scholar]
- 15.Klonoff DC. Schwartz DM. An economic analysis of interventions for diabetes. Diabetes Care. 2000;23:390–404. doi: 10.2337/diacare.23.3.390. [DOI] [PubMed] [Google Scholar]
- 16.Ishani A. Greer N. Taylor BC. Kubes L. Cole P. Atwood M. Clothier B. Ercan-Fang N. Effect of nurse case management compared with usual care on controlling cardiovascular risk factors in patients with diabetes: a randomized controlled trial. Diabetes Care. 2011;34:1689–1694. doi: 10.2337/dc10-2121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Krein SL. Klamerus ML. Vijan S. Lee JL. Fitzgerald JT. Pawlow A. Reeves P. Hayward RA. Case management for patients with poorly controlled diabetes: a randomized trial. Am J Med. 2004;116:732–739. doi: 10.1016/j.amjmed.2003.11.028. [DOI] [PubMed] [Google Scholar]
- 18.Ramadas A. Quek KF. Chan CK. Oldenburg B. Web-based interventions for the management of type 2 diabetes mellitus: a systematic review of recent evidence. Int J Med Inform. 2011;80:389–405. doi: 10.1016/j.ijmedinf.2011.02.002. [DOI] [PubMed] [Google Scholar]
- 19.Aubert RE. Herman WH. Waters J. Moore W. Sutton D. Peterson BL. Bailey CM. Koplan JP. Nurse case management to improve glycemic control in diabetic patients in a health maintenance organization.A randomized, controlled trial. Ann Intern Med. 1998;129:605–612. doi: 10.7326/0003-4819-129-8-199810150-00004. [DOI] [PubMed] [Google Scholar]
- 20.American Diabetes Association: Standards of medical care in diabetes—2012. Diabetes Care. 2012;35(Suppl 1):S11–S63. doi: 10.2337/dc12-s011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Welch G. Weinger K. Anderson B. Polonsky WH. Responsiveness of the Problem Areas In Diabetes (PAID) questionnaire. Diabet Med. 2003;20:69–72. doi: 10.1046/j.1464-5491.2003.00832.x. [DOI] [PubMed] [Google Scholar]
- 22.Welch GW. Jacobson AM. Polonsky WH. The Problem Areas in Diabetes Scale. An evaluation of its clinical utility. Diabetes Care. 1997;20:760–766. doi: 10.2337/diacare.20.5.760. [DOI] [PubMed] [Google Scholar]
- 23.Raji A. Gomes H. Beard JO. MacDonald P. Conlin PR. A randomized trial comparing intensive and passive education in patients with diabetes mellitus. Arch Intern Med. 2002;162:1301–1304. doi: 10.1001/archinte.162.11.1301. [DOI] [PubMed] [Google Scholar]
- 24.Polonsky WH. Earles J. Smith S. Pease DJ. Macmillan M. Christensen R. Taylor T. Dickert J. Jackson RA. Integrating medical management with diabetes self-management training: a randomized control trial of the Diabetes Outpatient Intensive Treatment program. Diabetes Care. 2003;26:3048–3053. doi: 10.2337/diacare.26.11.3048. [DOI] [PubMed] [Google Scholar]
- 25.Izquierdo RE. Knudson PE. Meyer S. Kearns J. Ploutz-Snyder R. Weinstock RS. A comparison of diabetes education administered through telemedicine versus in person. Diabetes Care. 2003;26:1002–1007. doi: 10.2337/diacare.26.4.1002. [DOI] [PubMed] [Google Scholar]
- 26.Shojania KG. Ranji SR. McDonald KM. Grimshaw JM. Sundaram V. Rushakoff RJ. Owens DK. Effects of quality improvement strategies for type 2 diabetes on glycemic control: a meta-regression analysis. JAMA. 2006;296:427–440. doi: 10.1001/jama.296.4.427. [DOI] [PubMed] [Google Scholar]
- 27.Solomon M. Wagner SL. Goes J. Effects of a Web-based intervention for adults with chronic conditions on patient activation: online randomized controlled trial. J Med Internet Res. 2012;14:e32. doi: 10.2196/jmir.1924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lynch CP. Strom JL. Egede LE. Effect of Veterans Administration use on indicators of diabetes care in a national sample of veterans. Diabetes Technol Ther. 2010;12:427–433. doi: 10.1089/dia.2009.0171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vouri SM. Shaw RF. Waterbury NV. Egge JA. Alexander B. Prevalence of achievement of A1c, blood pressure, and cholesterol (ABC) goal in veterans with diabetes. J Manag Care Pharm. 2011;17:304–312. doi: 10.18553/jmcp.2011.17.4.304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Trivedi AN. Grebla RC. Quality and equity of care in the Veterans Affairs health-care system and in Medicare Advantage health plans. Med Care. 2011;49:560–568. doi: 10.1097/MLR.0b013e31820fb0f6. [DOI] [PubMed] [Google Scholar]