Abstract
The period after completing primary and adjuvant cancer treatment until recurrence or death is now recognized as a unique phase in the cancer control continuum. The term “survivorship” has been adopted to connote this phase. Survivorship is a time of transition: Issues related to diagnosis and treatment diminish in importance, and concerns related to long-term follow-up care, management of late effects, rehabilitation, and health promotion predominate. In this article, we explore the unique challenges of care and health service delivery in terms of the interface between primary care and specialist care during the survivorship period. The research literature points to problems of communication between primary and specialist providers, as well as lack of clarity about the respective roles of different members of the health-care team. Survivorship care plans are recommended as an important tool to facilitate communication and allocation of responsibility during the transition from active treatment to survivorship. Research questions that remain to be answered with respect to survivorship care plans and other aspects of survivorship care are discussed.
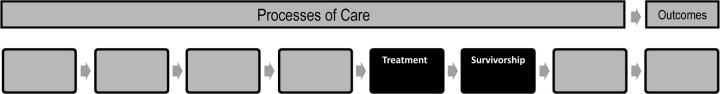
Current data estimate that more than 11 million people in the United States have a personal history of cancer (1). The period after completing primary and adjuvant cancer treatment and before the onset of advanced disease is now recognized as a unique phase in the cancer control continuum (Figure 1). This recognition stems from an important change in cancer epidemiology, as it is now the case that most individuals diagnosed with one of the major adult cancers (breast, colorectal, or prostate) will be a long-term survivor, leading to a marked increase in the prevalence of cancer survivors in the population (2,3). The term “survivorship” has been adopted to connote this phase in the cancer control continuum. It is a phase with important health-care and health service implications.
Survivorship is a time of transition. Issues related to diagnosis and treatment diminish in importance, and concerns related to long-term follow-up care, management of late effects, rehabilitation, and health promotion predominate (4). However, this transition from active cancer treatment to cancer survivorship is increasingly being recognized as one that is fraught with difficulties. In its 2005 report From Cancer Patient to Cancer Survivor: Lost in Transition (4), the Institute of Medicine (IOM) identified this phase as a time when the future role of the various health-care providers is often unclear. For patients, it can be a time of confusion both about what follow-up care involves and about which physician is responsible for follow-up care (5). Some data suggest that this may lead to deficits in the quality of care that cancer survivors receive (6). It also appears that the type of provider seen in follow-up affects the level of attention given to different aspects of their care. To address this, the IOM recommended that “Patients completing primary treatment should be provided with a comprehensive care summary and follow-up plan that is clearly and effectively explained.” (p. 4) (4). The report terms this as the “Survivorship Care Plan” (Appendix 1). Indeed, a strong literature of high-level evidence shows that with simple guidelines, primary care physicians are able to provide care to cancer survivors with outcomes that are equivalent to those achieved by cancer specialists (2,7). Consequently, survivorship care planning has the potential to both improve the quality of care for cancer survivors as well as address anticipated problems in health human resources (8). In this article, we will explore the unique challenges of care and health service delivery in terms of the interface between primary care and specialist care during the survivorship period.
Challenges at the Interface of Primary and Subspecialty Care for Cancer: Current Practice Patterns From Treatment Through Follow-Up Monitoring
Cancer recurrence and late effects of cancer treatments are important and ongoing concerns for cancer survivors. However, the majority will actually die of other causes. For example, an analysis of the causes of death for breast cancer patients who did not die of their cancer indicates that many of the major causes of death are from conditions that are modifiable through lifestyle changes (eg, heart and respiratory disease) or screening (eg, colon cancer) (9). Consequently, care for general medical and preventive health issues are equal in importance to care for the index cancer. We review here some of the problems experienced by cancer survivors in receiving various types of health care and discuss how survivorship care plans can be an important tool to address some of these problems.
Evidence indicates that cancer survivors may be less likely than age-matched noncancer patients to receive recommended care for chronic conditions across a wide range of diseases (6). A study examining 44 quality-of-care indicators in 14 884 five-year survivors of colorectal cancer compared with matched controls found that despite having more medical contacts, survivors were overall less likely to receive recommended follow-up for chronic conditions, such as angina, congestive heart failure, and chronic lung disease, and to receive less of some types of preventive care. For example, diabetic cancer survivors were less likely to have preventive eye examinations, and the data showed a trend toward less intensive monitoring of HbA1c (6). This effect is not universally observed, however. Another study of 5965 five-year breast cancer survivors found that they actually received more health maintenance care, such as influenza vaccination and cholesterol screening, than did matched controls without a history of cancer. In this study, despite having more medical contacts and demonstrated access to care, important disparities also existed based on race and wealth (10).
These and other studies have found that patients who were followed only by primary care physicians were more likely to receive preventive interventions directed at noncancer conditions, whereas those followed by oncologists were more likely to receive interventions directed at cancer surveillance (6,10,11). These findings may reflect different assumptions by patients and providers about providers’ roles after cancer treatment. For example, some patients may expect their oncologist to effectively become their primary care physician, but the oncologist may be unaware of this expectation. Although some oncologists are willing and able to act as a primary care physician, surveys have shown that most are not (12). Indeed, a recent survey of cancer survivors and their physicians found significant discordances in expectations about many aspects of care.
When the patient is ready to transition from active treatment to follow-up care, it is essential that both the patient and the primary care physician are aware of who is primarily responsible for future care (35). The studies cited above, which show that recommended cancer surveillance is more likely to occur when an oncologist is involved in survivorship care, illustrate this point (6,9,11). Underuse of cancer surveillance by primary care physicians may reflect an assumption that an oncologist has remained involved and is leading this aspect of care. In some cases, lack of appropriate surveillance may contribute to negative patient outcomes.
COMMENTARY
The lack of guidelines and providers who understand the very-long-term needs of cancer survivors is an unmet need. My cancer was diagnosed 30 years ago, when I was 13. I have not found a provider who understands both sides of my current needs. Internists do not understand my cancer and oncologists do not understand my non-cancer health maintenance needs, such as monitoring cholesterol and blood pressure. I've seen doctors at the cancer center who specialize in late effects of cancer, but they have not been able to respond well to my particular needs either.
From a Survivor
The fact that primary care physicians are more likely to provide preventive care suggests that oncologists may not see this as part of their area of responsibility. If a primary care physician is not actually involved, or the patient has looked to their specialist to provide all care, these important services may not be delivered, much to the detriment of the patient. Roles are likely even more blurred when it comes to issues, such as the effect of cancer and its treatment on sexuality, psychosocial distress, or employment concerns, potentially leaving these problems unaddressed.
COMMENTARY
As a young adult cancer survivor, the issues I'm concerned with are different than those for children or older adults. I must consider issues such as timing pregnancy (and managing breastfeeding) in between colonoscopies, how my cancer affects my children's need for screening, and how to stay abreast of the research that may change such decisions in the future. It is a challenge to manage how this interacts with my overall health, as that will also change as I get older.
From a Survivor
Most striking is the mismatch in expectations about which provider is to be responsible for screening for cancers other than the index one (eg, which provider is responsible for arranging colonoscopy and Papanicolaou smears in a breast cancer survivor). Survivorship care plans can be used to resolve some of this mismatch by clearly identifying the responsible provider for each aspect of care and ensuring that patients and providers are aware of the allocation of responsibility (11).
From the primary care perspective, traditional approaches to providing cancer care may make it difficult to provide comprehensive care, which is a fundamental principle of primary care and which cancer survivors need. An often-heard complaint is that cancer patients are sequestered into a “black box” of specialist oncology (13). Primary care providers also express concerns about the lack of role clarity, in that neither the patient nor the primary care physician knows who is primarily responsible for follow-up (5). Moreover, most primary care physicians carry a relatively small cancer caseload, making it difficult for some to be confident managing the care of survivors (14). Nevertheless, most studies have shown that primary care physicians are keen to take on responsibility for cancer survivorship care (7,15,16). Several randomized controlled trials have shown that both clinical and quality-of-life outcomes are unaffected when the primary care physician is primarily responsible for routine follow-up care (2,16,17). The need to integrate management of the index cancer, comorbid conditions, and general preventive care underscores the importance of providing comprehensive coordinated care (18,19).
From the examples given above it can be seen that communication is at the core of many of the problems at the interface between primary care and specialist care for cancer (14). Cancer care is frequently multidisciplinary and largely takes place in isolation from primary care physicians. Although primary care physicians are probably involved during the initial cancer diagnosis, they may not be fully aware of the treatments and other modalities of care (such as psychosocial care) that ensue (12,14,15). A clear allocation of responsibility can improve communication at the interface between primary and oncology care. Some patients themselves may wish to take a more active role at the interface of primary and specialty care during this phase of their care.
Potential Solutions: Insights From Research
Several models and tools have been proposed to meet the complex health-care needs of cancer survivors through better integration between primary care and specialist cancer care. Oeffinger and McCabe (20) propose a shared care model that attempts to rectify the current problems of unclear allocation of responsibility and poor communication.
COMMENTARY
Survivorship plans are really needed but I never had one. They need to be sufficiently detailed and clear so that patients can follow them.
From a Survivor
The model describes which tasks and communication issues are primarily the responsibility of primary care vs specialist cancer care along the care trajectory from diagnosis to survivorship. An important tool to achieve this model is the survivorship care plan.
Survivorship care plans, as envisioned by IOM, are designed to address potential deficiencies in communication by explicitly laying out for patients and all involved providers a plan for surveillance and other care in the future (Appendix 1). Ideally, the plan would be used as a general guide for the future as well as a resource for use during specific visits. At this point, however, it is not clear exactly who should be responsible for developing these plans. Nevertheless, the patient and oncologist (or other member of the oncology team) could use the plan to review a summary of the diagnosis and the treatment received, discuss recommendations for surveillance for cancer recurrence, and discuss recommendations for routine health maintenance unrelated to the cancer. This also would be an opportunity to educate the patient about psychosocial support and other resources available for cancer survivors. The treatment summary would indicate the cancer diagnosis, histology, and stage, and list the different primary treatments given and their dates. The treatment summary also should identify and provide contact information for those who provided oncology care and, ideally, identify a key provider for follow-up care. The optimum provider for follow-up care may be different for different types of cancer. For example, for breast cancer patients, there is good evidence that the provider can be either an oncologist or a primary care physician (21,22). In contrast, anal cancer requires endoscopic surveillance, which should be done by a specialist. In most cases, however, many types of providers are able to deliver high quality of care. As a result, preferences of the patient and the involved providers can play a large part in determining who does what. The essential thing is that it is clear to the patient and all involved health-care providers who will be primarily responsible for what aspect of follow-up care.
The care plan should address recommendations regarding both cancer and noncancer care. By being specific to the patient, it is actionable by their providers. It is not reasonable to expect generalists to remain up-to-date on surveillance recommendations and potential side effects of new cancer treatments, but they are well able to act on specific information and implement a care plan. Recommendations for cancer surveillance can be found from several sources. The American Society of Clinical Oncology (ASCO) has evidence-based surveillance guidelines for breast and colorectal cancers that can be found at www.asco.org under the Quality Care and Guidelines tab. Consensus guidelines for surveillance for recurrence of other cancers after treatment are incorporated into the National Comprehensive Cancer Network (NCCN) guidelines, found at www.nccn.org. Unfortunately, no comprehensive guidelines have been developed for monitoring or managing long-term and late effects of cancer therapy for survivors of adult cancer.
COMMENTARY
The growing number of long-term survivors is increasing the salience of late-effects research. What does a symptom that occurs 10-15 years after treatment mean for the type of care that's necessary to address that symptom and the interfaces between primary and specialty care providers?
From a Supplement Author
However, the major issues can be extrapolated from the consensus guidelines of the Children's Oncology Group, found at www.survivorshipguidelines.org. Long-term effects are those that first occur during cancer treatment and persist after completion of primary therapy, such as peripheral neuropathy from some chemotherapy drugs. Late effects are those that were not apparent during primary treatment but become apparent at some later time, such as bone loss and increased risk of hip fracture from pelvic radiation (23).
With respect to noncancer care, it has been suggested that completion of treatment for cancer may be a “teachable moment” (24) when patients may be more receptive to messages about health behaviors, such as quitting smoking or becoming physically active. Moreover, as mentioned above, it is important to know about age- and sex-appropriate screening recommendations for other cancers and other medical conditions and to ensure clarity about which provider will coordinate these activities. Lastly, the IOM recommends that patients be given sources of information related to potential insurance, employment, and financial challenges.
Creating a survivorship care plan is a practical challenge, however (25). Although many providers can make important contributions, one of the patient's oncology providers is usually in the best position to lead it by virtue of specific knowledge of the treatment received and professional knowledge of surveillance and other recommendations related to the cancer and its treatment. But these practitioners are busy, a counseling visit to review these issues is not well reimbursed, and in the end, most of the benefits accrue to the patient and other providers rather than to the oncologist. At this point, it is also unknown whether this saves money or costs money, and so it is unclear to payers whether it is in their interests to fund this activity. Consequently, widespread implementation of survivorship care plans will require a culture change in which it becomes a required part of good cancer practice. Patients and referring physicians, such as the primary care physician, can help effect this change by demanding a care plan.
Two randomized controlled trials of follow-up care for breast cancer patients have shown that, when given what could be considered a brief survivorship care plan in the form of a clinical practice guideline with explicit directions for follow-up care, primary care physicians achieve the same outcomes as specialists (2,3,7,26,27). These trials, which compared primary care physician follow-up with oncologist follow-up, found that the delay in time to diagnosing recurrence was the same (2), as was the rate of recurrence-related serious clinical events (7). Health-related quality of life was unaffected, patient satisfaction was better (27), and both patient and health service costs were less (28). Moreover, these findings confirm the results of surveys showing that primary care physicians are generally willing to take on this role (16,29). In both randomized controlled trials, almost all primary care physicians agreed to provide exclusive follow-up care for their patients. Although such a model may be particularly attractive for breast cancer, where the evidence is strongest and the manpower concerns are greatest (25), a trial with similar methodology that was directed at follow-up care for colorectal cancer patients showed similar results (17). Another important element of this research is that it confirmed the findings of numerous observational studies that most recurrences are symptomatic when detected and that patients present first to their primary care physician with symptoms, regardless of formal follow-up arrangements (30,31).
There is no single best way that survivorship care must be provided. The type of provider—specialists, generalists, physician-extenders, or combination of these in a “shared care” model (19), or in a specialized survivorship clinic—is less important than ensuring there is communication and coordination of care among the multiple providers involved (18). Several tools, such as complete survivorship care plans and individual elements of those plans, such as clinical practice guidelines and structured consultation and discharge letters (32), can facilitate the process of communication, provided that all members of the health-care team are committed to improving coordination of care (33). Information technology also may make an important contribution. The article by Hesse et al. (34) in this supplement explores this issue in depth.
Future Research
Survivorship care plans are viewed as the tool with the greatest potential to address the problems at the interface between primary care and specialist care during the transition period from active treatment to survivorship because of their focus on improving communication. The IOM made the remarkably bold statement that survivorship care plans “have strong face validity and can reasonably be assumed to improve care unless and until evidence accumulates to the contrary” (p. 5) (4). Despite this strong statement, research on a range of questions about survivorship care plans is still needed to make evidence-based recommendations. For example: Who should prepare the plan? Who reviews it with the patient? How is it transmitted to the primary care physician? Moreover, it is important to evaluate the impact on outcomes from both the perspective of the patient and the health-care system, as well as cost-effectiveness. One such evaluation involving breast cancer survivors in a multicenter randomized controlled trial is currently under way (Grunfeld et al., NCIC/CBCRA grant #17423). It also would be valuable to study the potential benefits of other forms of standardized templates, such as structured discharge letters and clinical practice guidelines, as adjuncts to care plans.
In addition to research on survivorship care plans, other important areas require study. Different models for the organization and delivery of survivorship care, from dedicated tertiary care survivorship clinics to community-based nurse-navigators, warrant evaluation. Do these different models improve coordinated and comprehensive care or do they contribute to further fragmentation of care?
Patient preferences and manpower implications also must be considered. These efforts should eventually lead to the establishment of standards of care, clinical practice guidelines, and quality-of-care measures related to cancer survivorship. To date, this area has had a paucity of research. It is vital to understand patients’ views of different models of survivorship care and the optimum time for introducing a discussion about the transition in care. An interesting research question would be the potential value of the patient as the intermediary between primary and specialist physician: Would this form of patient empowerment lead to better outcomes or merely add to patient burden?
Conclusions
The number of cancer survivors is growing exponentially. Survivorship is increasingly recognized as a distinct entity within the cancer care continuum, and the point of transition from active anticancer treatment to survivorship is an important time to set the stage for subsequent care. Empowering patients to take responsibility for their own care and ensuring clarity around where responsibility for cancer surveillance, general preventive care, screening for other cancers, and management of comorbid conditions lies will go a long way toward addressing current gaps at the interface between primary and specialist care during the transition from active treatment to survivorship. In most cases, more important than the details of the plan is that it is clear to all involved what has been done, what should be done going forward, and which providers are responsible for the different aspects of care. The concept of survivorship care planning is a place to start in ensuring quality of care for cancer survivors.
Figure 1.
Types and transitions in care that constitute the process of care across the cancer continuum.
Appendix 1:
The Institute of Medicine survivorship care plan*
| Upon discharge from cancer treatment, including treatment of recurrences, every patient should be given a record of all care received and important disease characteristics. This should include, at a minimum: |
| 1. Diagnostic tests performed and results. |
| 2. Tumor characteristics (eg, site(s), stage and grade, hormone receptor status, and marker information). |
| 3. Dates of treatment initiation and completion. |
| 4. Surgery, chemotherapy, radiotherapy, transplant, hormonal therapy, or gene or other therapies provided, including agents used, treatment regimen, total dosage, identifying number and title of clinical trials (if any), indicators of treatment response, and toxicities experienced during treatment. |
| 5. Psychosocial, nutritional, and other supportive services provided. |
| 6. Full contact information on treating institutions and key individual providers. |
| 7. Identification of a key point of contact and coordinator of continuing care. |
| Upon discharge from cancer treatment, every patient and his/her primary health-care provider should receive a written follow-up care plan incorporating available evidence-based standards of care. This should include, at a minimum: |
| 1. The likely course of recovery from acute treatment toxicities, as well as the need for ongoing health maintenance or adjuvant therapy. |
| 2. A description of recommended cancer screening and other periodic testing and examinations, and the schedule on which they should be performed (and who should provide them). |
| 3. Information on possible late and long-term effects of treatment and symptoms of such effects. |
| 4. Information on possible signs of recurrence and second tumors. |
| 5. Information on the possible effects of cancer on marital/partner relationship, sexual functioning, work, and parenting, and the potential future need for psychosocial support. |
| 6. Information on the potential insurance, employment, and financial consequences of cancer and, as necessary, referral to counseling, legal aid, and financial assistance. |
| 7. Specific recommendations for healthy behaviors (eg, diet, exercise, healthy weight, sunscreen use, immunizations, smoking cessation, and osteoporosis prevention). When appropriate, recommendations that first-degree relatives be informed about their increased risk and the need for cancer screening (eg, breast cancer, colorectal cancer, and prostate cancer). |
| 8. As appropriate, information on genetic counseling and testing to identify high-risk individuals who could benefit from more comprehensive cancer surveillance, chemoprevention, or risk-reducing surgery. |
| 9. As appropriate, information on known effective chemoprevention and behavioral strategies for secondary prevention (eg, tamoxifen in women at high risk of breast cancer; smoking cessation after lung cancer) and monitoring of adherence to these recommendations. |
| 10. Referrals to specific follow-up care providers (eg, rehabilitation, fertility, psychology), support groups, and/or the patient’s primary care provider. |
| 11. A listing of cancer-related resources and information (eg, Internet-based sources and telephone listings for major cancer support organizations). |
Reprinted with permission from From Cancer Patient to Cancer Survivor: Lost in Transition, 2005 by the National Academy of Sciences, Courtesy of the National Academies Press, Washington, DC (4).
References
- 1.Ries LAG, Melbert D, Krapcho M, et al. SEER Cancer Statistics Review, 1975-2005. Bethesda, MD: National Cancer Institute; 2008. [Google Scholar]
- 2.Grunfeld E, Mant D, Yudkin P, et al. Routine follow up of breast cancer in primary care: randomised trial. BMJ. 1996;313(7058):665–669. doi: 10.1136/bmj.313.7058.665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grunfeld E, Yudkin P, Adewuyl-Dalton R, Vessey MP, Mant D. Follow up in breast cancer. Quality of life unaffected by general practice follow up. BMJ. 1995;311(6996):54. doi: 10.1136/bmj.311.6996.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Institute of Medicine. From Cancer Patient to Cancer Survivor: Lost in Transition. Washington, DC: National Academies Press; 2005. [Google Scholar]
- 5.Miedema B, MacDonald I, Tatemichi S. Cancer follow-up care. Patients’ perspectives. Can Fam Physician. 2003;49(7):890–895. [PMC free article] [PubMed] [Google Scholar]
- 6.Earle CC, Neville BA. Underuse of necessary care among elderly colorectal cancer survivors. Cancer. 2004;101(8):1712–1719. doi: 10.1002/cncr.20560. [DOI] [PubMed] [Google Scholar]
- 7.Grunfeld E, Levine MN, Julian JA, et al. Randomized trial of long-term follow-up for early-stage breast cancer: a comparison of family physician versus specialist care. J Clin Oncol. 2006;24(6):848–855. doi: 10.1200/JCO.2005.03.2235. [DOI] [PubMed] [Google Scholar]
- 8.Erikson C, Salsberg E, Forte G, Bruinooge S, Goldstein M. Future supply and demand for oncologists: challenges to assuring access to oncology services. J Oncol Pract. 2007;3(2):79–86. doi: 10.1200/JOP.0723601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schairer C, Mink PJ, Carroll L, Devesa SS. Probabilities of death from breast cancer and other causes among female breast cancer patients. J Natl Cancer Inst. 2004;96(17):1311–1321. doi: 10.1093/jnci/djh253. [DOI] [PubMed] [Google Scholar]
- 10.Earle CC, Burstein HJ, Winer EP, Weeks JC. Quality of non-breast cancer health maintenance among elderly breast cancer survivors. J Clin Oncol. 2003;21(8):1447–1451. doi: 10.1200/JCO.2003.03.060. [DOI] [PubMed] [Google Scholar]
- 11.Snyder CF, Earle CC, Herbert RJ, Neville BA, Blackford AL, Frick KD. Preventive care for colorectal cancer survivors: a 5-year longitudinal study. J Clin Oncol. 2008;26(7):1073–1079. doi: 10.1200/JCO.2007.11.9859. [DOI] [PubMed] [Google Scholar]
- 12.American Society of Clinical Oncology. Status of the medical oncology workforce. J Clin Oncol. 1996;14(9):2612–2621. doi: 10.1200/JCO.1996.14.9.2612. [DOI] [PubMed] [Google Scholar]
- 13.Gilbert R, Willan AR, Richardson S, Sellick S. Survey of family physicians: what is their role in cancer patient care? Can J Oncol. 1994;4(3):285–290. [PubMed] [Google Scholar]
- 14.Grunfeld E. Cancer survivorship: a challenge for primary care physicians. Br J Gen Pract. 2005;55(519):741–742. [PMC free article] [PubMed] [Google Scholar]
- 15.Wood ML, McWilliam CL. Cancer in remission. Challenge in collaboration for family physicians and oncologists. Can Fam Physician. 1996;42(5):899–904. 907–910. [PMC free article] [PubMed] [Google Scholar]
- 16.Worster A, Bass MJ, Wood ML. Willingness to follow breast cancer. Survey of family physicians. Can Fam Physician. 1996;42(2):263–268. [PMC free article] [PubMed] [Google Scholar]
- 17.Wattchow DA, Weller DP, Esterman A, et al. General practice vs surgical-based follow-up for patients with colon cancer: randomised controlled trial. Br J Cancer. 2006;94(8):1116–1121. doi: 10.1038/sj.bjc.6603052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Khan NF, Ward A, Watson E, Austoker J, Rose PW. Long-term survivors of adult cancers and uptake of primary health services: a systematic review. Eur J Cancer. 2008;44(2):195–204. doi: 10.1016/j.ejca.2007.10.005. [DOI] [PubMed] [Google Scholar]
- 19.Bodenheimer T. Coordinating care—a perilous journey through the health care system. N Engl J Med. 2008;358(10):1064–1071. doi: 10.1056/NEJMhpr0706165. [DOI] [PubMed] [Google Scholar]
- 20.Oeffinger KC, McCabe MS. Models for delivering survivorship care. J Clin Oncol. 2006;24(32):5117–5124. doi: 10.1200/JCO.2006.07.0474. [DOI] [PubMed] [Google Scholar]
- 21.Khatcheressian JL, Wolff AC, Smith TJ, et al. American Society of Clinical Oncology 2006 update of the breast cancer follow-up and management guidelines in the adjuvant setting. J Clin Oncol. 2006;24(31):5091–5097. doi: 10.1200/JCO.2006.08.8575. [DOI] [PubMed] [Google Scholar]
- 22.Grunfeld E, Dhesy-Thind S, Levine M. Clinical practice guidelines for the care and treatment of breast cancer: follow-up after treatment for breast cancer (summary of the 2005 update) CMAJ. 2005;172(10):1319–1320. doi: 10.1503/cmaj.045062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Baxter NN, Habermann EB, Tepper JE, Durham SB, Virnig BA. Risk of pelvic fractures in older women following pelvic irradiation. JAMA. 2005;294(20):2587–2593. doi: 10.1001/jama.294.20.2587. [DOI] [PubMed] [Google Scholar]
- 24.Ganz PA. A teachable moment for oncologists: cancer survivors, 10 million strong and growing! J Clin Oncol. 2005;23(24):5458–5460. doi: 10.1200/JCO.2005.04.916. [DOI] [PubMed] [Google Scholar]
- 25.Ganz PA, Hahn EE. Implementing a survivorship care plan for patients with breast cancer. J Clin Oncol. 2008;26(5):759–767. doi: 10.1200/JCO.2007.14.2851. [DOI] [PubMed] [Google Scholar]
- 26.Grunfeld E, Mant D, Vessey MP, Yudkin P. Evaluating primary care follow-up of breast cancer: methods and preliminary results of three studies. Ann Oncol. 1995;6(suppl 2):47–52. doi: 10.1093/annonc/6.suppl_2.s47. [DOI] [PubMed] [Google Scholar]
- 27.Grunfeld E, Fitzpatrick R, Mant D, et al. Comparison of breast cancer patient satisfaction with follow-up in primary care versus specialist care: results from a randomized controlled trial. Br J Gen Pract. 1999;49(446):705–710. [PMC free article] [PubMed] [Google Scholar]
- 28.Grunfeld E, Gray A, Mant D, et al. Follow-up of breast cancer in primary care vs specialist care: results of an economic evaluation. Br J Cancer. 1999;79(7–8):1227–1233. doi: 10.1038/sj.bjc.6690197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Grunfeld E, Mant D, Vessey MP, Fitzpatrick R. Specialist and general practice views on routine follow-up of breast cancer patients in general practice. Fam Pract. 1995;12(1):60–65. doi: 10.1093/fampra/12.1.60. [DOI] [PubMed] [Google Scholar]
- 30.Loprinzi CL, Hayes D, Smith T. Doc, shouldn't we be getting some tests? J Clin Oncol. 2000;18(11):2345–2348. doi: 10.1200/JCO.2000.18.11.2345. [DOI] [PubMed] [Google Scholar]
- 31.Walsh GL, O'Connor M, Willis KM, et al. Is follow-up of lung cancer patients after resection medically indicated and cost-effective? Ann Thorac Surg. 1995;60(6):1563–1570. doi: 10.1016/0003-4975(95)00893-4. [DOI] [PubMed] [Google Scholar]
- 32.Tattersall MH, Butow PN, Brown JE, Thompson JF. Improving doctors’ letters. Med J Aust. 2002;177(9):516–520. doi: 10.5694/j.1326-5377.2002.tb04926.x. [DOI] [PubMed] [Google Scholar]
- 33.Grunfeld E. Primary care physicians and oncologists are players on the same team. J Clin Oncol. 2008;26(14):2246–2247. doi: 10.1200/JCO.2007.15.7081. [DOI] [PubMed] [Google Scholar]
- 34.Hesse BW, Hanna C, Massett HA, Hesse NK. Outside the box: will information technology be a viable intervention to improve the quality of cancer care? J Natl Cancer Inst Monogr. 2010;40:81–89. doi: 10.1093/jncimonographs/lgq004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cheung WY, Neville BA, Cameron DB, Cooke EF, Earle CC. Comparisons of Patient and Physician Expectations for Cancer Survivorship Care. J Clin Oncol. 2009 May;20(27(15)):2489–95. doi: 10.1200/JCO.2008.20.3232. [DOI] [PubMed] [Google Scholar]