Abstract
In this article, we review the challenges and opportunities related to developing effective, collaborative relationships between primary care and oncology providers during the initial cancer treatment period. This point in the cancer care continuum is complex and often represents the first major transition in care between primary care providers and oncology specialists. Patients often receive care from multiple providers in a number of different settings and are faced with making treatment decisions in a short, concentrated period of time. Patients consistently report having significant informational and emotional needs that are often unmet during this period. Using the published literature, we have identified a number of challenges during this part of the treatment continuum that may limit providers’ ability to deliver effective care, including provider care discontinuities, information exchange problems, and gaps in provider role clarity that may be especially problematic within the context of managing comorbid health conditions. The limited published literature specific to this step in the cancer care trajectory supports the importance of ongoing primary care–specialist collaboration during this phase in the care continuum for both medical and psychosocial care. How to best achieve effective collaboration between providers requires further research in information exchange and tools to support it, evaluation of shared care models specific to the cancer context, and studies of the potential role of multidisciplinary case conferencing that include the primary care provider.
Introduction: The Primary Treatment Continuum
The care of cancer patients from diagnosis through primary treatment is complex, involving several diagnostic and treatment steps as well as interactions with a wide range of care providers new to the patients. These steps generally include the following: staging, general medical assessments, definitive therapy (surgery or radiation depending on tumor type and stage) to control local disease, and often adjuvant therapy (ie, radiation therapy, chemotherapy, hormonal therapy, or immunotherapy) to reduce the risk of recurrence. Newly diagnosed patients enter an unfamiliar system of care, interacting with surgeons (eg, surgical oncologists, plastic surgeons) and medical and radiation oncologists, who must work together to create an optimal treatment plan specific to the type and stage of cancer while taking into consideration patient comorbidities and treatment preferences.
COMMENTARY
I think that at the time of diagnosis, a conversation should take place between the health care provider and the patient. The provider should inform the patient of the possibilities that might occur during his or her cancer journey (such as confusion, complications, depression) and that someone, whether it be the primary care physician or another physician, will be available throughout the cancer experience to consult, explain, navigate, and support the patient. This planning-ahead process could be analogous to the planning process that takes place at the end of treatment with a survivorship care plan.
From a Survivor
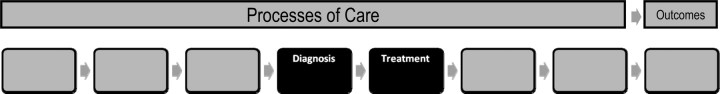
Over a short period of time, newly diagnosed patients who are dealing with the anxiety of their diagnosis are asked to consider a variety of treatment options, each with its own risks and benefits. With the increasing subspecialization of oncology providers, the majority of patients will make multiple transitions between providers and settings (ie, from radiologist, to surgeon, to medical and radiation oncologists) as they move through the various stages of primary treatment. The trajectory of care during this phase of cancer treatment is unique in its complexity, and it is no surprise that cancer patients and their families often report feeling overwhelmed and lost in a system that is a challenge to navigate (1) (Figure 1).
In 2005, the Institute of Medicine released a report entitled From Cancer Patient to Cancer Survivor: Lost in Transition, which outlined the challenges of providing comprehensive care to cancer patients across the continuum (2). In particular, this report emphasized the importance of effective communication between care providers so that providers are clear about the processes of care and their roles within that care. This report also outlined the need to raise awareness of the medical, functional, and psychosocial consequences of cancer and its treatment among all providers. It presented a framework from which to define quality health care, primarily within the context of cancer survivorship, and identified potential strategies to improve care delivery. A fundamental conclusion of this report was the need for better care integration between primary and cancer care systems as a way of ensuring continuity of care and better support for patients, thereby improving quality of care.
In this article, we first consider why integration and coordination of care between primary and cancer care physicians is important, then review challenges and opportunities related to the integration and coordination of care between the primary and cancer care systems for newly diagnosed cancer patients undergoing treatment. Although many of these challenges and opportunities are common to other cancer care phases, we survey the limited published literature specific to this point in the care trajectory to develop recommendations for further research on existing and potential new models of collaborative care between primary and cancer care physicians. Throughout this article, we define the concept of collaboration during the initial treatment phase of cancer as working together to achieve optimal care for a cancer patient (3). Additional concepts that are used throughout this article include the following: “care coordination,” defined as provision of care in an optimal sequence (4); “care integration,” defined as the process of creating and maintaining structure and connection between different providers for the purpose of coordinating patient care (5), at the same time retaining each provider’s unique role; and “continuity of care,” defined as an uninterrupted care relationship between patient and provider (4).
Why Is It Important for Primary Care and Oncology Specialists to Collaborate During the Initial Treatment Phase?
Collaboration may help facilitate three key features of care for cancer patients during the primary treatment phase: 1) continuity of care to help smooth transitions and ensure that all providers have up-to-date knowledge of a patient's health status and treatment decisions, 2) identification and management of preventive care needs and comorbid conditions that may affect cancer treatments, and 3) provision of appropriate supportive care. In this section, we discuss why attending to these three features of care among cancer patients is important.
Continuity of Care.
Before entering the cancer care system, most patients have had ongoing care relationships with primary care providers, who have a detailed knowledge of their medical and social histories (6).
COMMENTARY
Men have a better relationship with their Jiffy Lube guy than with any doctor. Men don't have relationships with their primary care provider.
From a Survivor
Patients identify primary care providers as important sources of information about cancer treatment and potential support for them and their families (7). Very often, it is the primary care provider who has initiated cancer investigations either in response to a presenting symptom or as part of screening. In addition, preliminary discussions between primary care providers and patients may address the implications of a cancer diagnosis and treatment for the patient and family.
Despite primary care physicians’ early involvement in cancer diagnosis, they have reported feeling isolated from the cancer care system (8). They also have reported a loss of continuity in the primary care–patient relationship during the intense cancer treatment period (9). Recent patterns of care research from Ontario have shown this quantitatively with visits to primary care providers falling dramatically in the 6 months after a diagnosis date (10). Even when primary care providers see their cancer patients, they may lack sufficient knowledge regarding the treatment plan and how to support their patients’ medical and psychosocial needs. Not infrequently, it is the patients who must attempt to fill in the knowledge gaps between providers as communications may not be exchanged in a timely fashion or may lack details important to providers (11).
COMMENTARY
To what extent should primary care providers reach out to patients? Or, is it up to the patient to ask for the primary provider to be involved?
From a Supplement Author
These factors limit their ability to effectively help their patients cope during the initial treatment period (12). Most primary care providers report feeling disconnected from the decision-making process during the cancer treatment period, yet cancer patients and their families continue to identify their primary care practitioners as critical providers of both medical and supportive care, especially to help them work through the information and options being presented to them by oncology specialists (13,14). Despite these challenges, a large body of research demonstrates primary care providers’ ongoing commitment to being involved in the care of their cancer patients (15).
COMMENTARY
What kind of guidance can doctors get about collaborating with each other? The primary care provider must feel comfortable with such collaboration.
From a Survivor
Oncologists, on the other hand, generally see cancer patients frequently during the initial treatment period. They must comprehensively assess patients in terms of both their stage of disease, which will dictate the treatment approach, and the risks and benefits of the treatments themselves. This latter assessment is particularly important in patients with significant comorbid conditions or psychosocial issues, yet they do not have the historical relationship or knowledge of these patients’ other medical conditions and psychosocial concerns that primary care physicians offer. In addition, oncologists are more likely to see their role as addressing the cancer care needs of patients rather than the entire scope of medical, psychosocial, spiritual, and informational needs (7). This more limited perceived role in caring for cancer patients supports the importance of maintaining continuity of care for cancer patients with their primary care providers. Additional support for this relationship is research that has associated continuity of primary care with optimal primary health care, more efficient care provision, and greater patient satisfaction (16,17).
COMMENTARY
It's important to recognize co-morbidities going into treatment. Who will address these conditions?
From a Supplement Author
Identifying and Managing Cancer Patients’ Preventive Care Needs and Comorbid Chronic Medical Conditions.
Several population-based, posttreatment studies of Medicare cancer patients in the United States have clearly illustrated that reduced involvement by primary care physicians is associated with inferior overall care and outcomes, especially in managing preventive services and health conditions not related to cancer (18,19). Even more importantly during the initial treatment phase of cancer care, assessing and managing comorbid health conditions is critical to ensure that cancer care is appropriate and safe, particularly for older patients who are more likely to have serious comorbid medical conditions at the time of cancer diagnosis (20). At the time of transition to primary cancer treatment, primary care providers can be an important source of information to the oncology team about patients’ comorbid conditions, psychosocial milieu, resources, and potential needs. Although many studies demonstrate the risks of complications from cancer therapies in patients with serious comorbid health conditions, such as heart disease or diabetes (21), there is a paucity of published research to determine whether active management of these other chronic medical conditions can improve cancer care outcomes.
Supportive Care for Newly Diagnosed Cancer Patients.
Supportive cancer care involves the provision of care to meet the informational, physical, emotional, spiritual, and economic needs of patients (22). Although it is widely acknowledged that meeting the supportive care needs of cancer patients is important, many population-based surveys from a variety of cancer care systems consistently show that up to 40% of newly diagnosed cancer patients have reported unmet needs, predominantly in the informational (about the cancer, its treatment, and the cancer care system procedures) and psychosocial domains of supportive care (23). There is emerging evidence that unmet needs may be associated with worse care experiences and functional outcomes. For example, one recently published study has shown that cancer patients’ unmet physical and daily living needs are associated with worse physical and emotional function (24).
Comprehensive care for cancer patients requires the involvement of primary care providers who can attend to patients’ continued noncancer health-care needs as well as provide supportive care in informational and psychosocial domains. This is clearly illustrated in an observational study by Sisler et al. (13), which examined the degree to which higher quality-of-life scores were associated with cancer patients’ receipt of care from their primary care providers. This study found that cancer patients who received more care from their primary care physicians in the areas of psychosocial support, noncancer medical problems, information provision about cancer and cancer treatment, and support of the cancer patients’ families had higher quality-of-life scores. Research has also shown that cancer patients receive improved supportive care if comprehensive assessments of need and quality of life are made available to physicians (25). However, many oncologists do not routinely assess these needs despite patients reporting that it is important to them to have these supportive care needs met, especially during the early treatment phase of care (26).
Perhaps most importantly, patients themselves acknowledge the importance of having both oncologists and primary care providers offer supportive care for their cancer. A survey of more than 2500 patients recently diagnosed with cancer in Ontario, Canada, found that more than 80% of patients identified either their oncologists or primary care providers as their preferred source of information about cancer and its treatment. This study also demonstrated the value that patients place on having their primary care provider as a knowledgeable support in treatment decision making and in the provision of emotional support (6). In the same study, a survey of providers revealed that most responding primary care providers, surgeons, and oncologists identified information provision as one of their key responsibilities to cancer patients, but that primary care providers were likely to acknowledge much more responsibility for assessing patients’ psychological and social needs and less for providing informational support about cancer treatments or the cancer care system. A qualitative study in Australia identified the value that newly diagnosed patients placed upon the role of their primary care physicians as medical interpreters, communication facilitators, and advocates when the patients had concerns or needed clarifications about their specialty care (27).
Challenges to Developing Strong Collaborative Primary Care–Oncology Physician Partnerships
Promoting a continuity care relationship through a collaborative primary care–oncology provider partnership has the potential of ensuring that the full range of cancer patients’ medical and psychosocial needs are met during the primary treatment period, yet numerous challenges undermine this goal. In the next section we review three major challenges to the development of strong collaborative practices: provider role clarity, information exchange between providers, and provider compensation.
Provider Role and Role Clarity
Several largely qualitative studies across Europe and Canada have documented that lack of clarity about the appropriate roles of primary care and oncology physicians is a barrier to patients’ receipt of collaborative care from them during their cancer care course. Primary care providers in both a Canadian study by Dworkind et al. (8) and a study from Norway by Anvik et al. (28) related confusion regarding who was responsible for cancer patients’ care as a barrier to their involvement in their patients’ care. These same primary care providers reported more satisfaction in caring for cancer patients when they had a clear agreement regarding their respective roles. Lack of role clarity between physicians also has been expressed by cancer patients. In one study of 183 patients completing primary treatment, 36% of respondents were unsure who was primarily responsible for their cancer care and follow-up (29).
These findings are further supported and reinforced by the findings of Klabunde et al. (30) of a national survey in the United States conducted by the Cancer Care Outcomes Research and Surveillance Consortium. This survey of more than 3000 primary care providers and cancer specialists showed that there is a clear distinction in self-reported roles between providers, with the management of comorbid conditions and supportive care predominantly reported by primary care providers rather than by oncologists. The authors concluded that although this study helped clarify the current roles of primary care and cancer care providers, determining the optimal interface and roles of these providers and how to organize and negotiate these roles are areas that require ongoing research.
Information Exchange Between Providers
The timing and content of medical information exchanged between care providers is the backbone of coordinated care because it supports the most appropriate care by the most appropriate provider in the most appropriate setting. Timely exchange of meaningful information also can reduce the chance for duplication of services and medical errors. In cancer care, a number of studies have illuminated problems in information exchange between providers.
In the United Kingdom and Australia, surveys of primary care providers have documented that in a significant proportion of cases, consultation notes from oncologists never arrive (11,31). This obviously undermines the ability of primary care providers to participate in the care of their patients during the initial treatment phase or even provide informational support to patients. Even with timely correspondence, the content of consultation letters is frequently reported to be of little use to primary care. The focus is often on detailed disease parameters and complex treatments rather than information on prognosis and treatment side effects that allows primary care providers to participate in the care of their patients (32).
The Canadian study by Dworkind et al. (8) and the Norwegian study by Anvik et al. (28) identified several barriers related to communication between cancer care physicians and primary care providers. Primary care providers related concerns about their knowledge base in cancer care, and reported more satisfaction in caring for cancer patients when they had direct, two-way communication with the cancer care physicians as well as when they were informed about their patients’ treatments, outcomes, and prognosis. A body of research on interventions to address this informational divide is emerging (see “Potential Solutions” below), but much work remains.
One important observation from our review of the literature is that most information exchange research examines a unilateral direction of information flow, namely specialist to primary care provider. There is very little investigation into opportunities to enhance information exchange from the primary care provider to the specialist. This is an important area to explore further, especially during the initial treatment phase in the cancer care continuum, as it has the potential to support role clarity, management of noncancer health conditions, and provision of supportive care.
Financial Compensation
Although professional standards may reasonably expect providers to collaborate to provide the best care to patients, the reality is that without adequate compensation, most providers will not initiate a change in practice patterns and processes of care, especially if the changes involve a complex set of tasks. Research has shown that regardless of professional commitment, the lack of compensation for time spent organizing tests, providing supportive counseling, and interacting with oncologists results in a lower probability of engagement by primary care providers across the cancer continuum (33). This is especially problematic in the initial treatment period as current fee structures and codes in Canada and the United States (as well as other jurisdictions) do not compensate for the detailed activities required by primary care to be full participants in a collaborative team. In a recent study, one of the authors of this review (J. Sussman) found that regardless of the compensation model reported by respondents, which included fee-for-service, capitation, and blended arrangements, none was felt to be adequate to support caring for cancer patients at any point in the care continuum (34). Clearly, provider compensation will need to be considered in the design of any models of collaborative care to support successful implementation.
Potential Solutions to Improve Collaboration Between Primary Care and Cancer Care Physicians
Because cancer is a complex and consuming diagnosis, with most cancer care provided and managed by multiple specialists, improving collaboration between primary care and cancer care physicians may require new or adapted care models. A collaboration paradigm that transcends the individual patient–physician relationship, and focuses instead on continuity of information, management, and relationship across disciplines and providers has been proposed and fits well with the coordination of care needed by cancer patients (4). This cross-disciplinary model of continuity and coordination can help ensure that pertinent information is available to all providers when needed for decision making and patient support.
In this section we review three opportunities to support improved continuity and coordination, and thereby collaboration between providers: shared care models, information exchange mechanisms, and multidisciplinary care conferencing.
Shared Care Models
The key elements of care integration between primary care and specialist care systems include provider communication strategies and mechanisms to support role clarity (4). These elements are also expected to support care efficiency and reduce duplications in care.
A number of models to integrate cancer care across health-care disciplines have been developed, with shared care receiving the most attention (35–37). In the shared care model, health-care professionals, often specialist and primary care physicians, jointly participate in delivering care to patients. This care is enhanced by an expanded information exchange beyond the usual consultation letters and discharge summaries. Although shared care models have been developed and tested in a number of chronic conditions, such as diabetes and cardiovascular diseases, little information about their application to cancer care during the initial treatment phase has been published. A Cochrane review of the impact of shared care in the management of chronic diseases demonstrated little benefit outside of improved prescribing, but did clarify that successful models had common elements, including the use of care paths and guidelines, the identification of a care coordinator (typically a physician or nurse), and enhanced communication mechanisms and templates (eg, common medical records or standardized charts that record key medical or psychosocial parameters) (37). Most models operate on the assumption that all aspects of care and disease management can be delivered or managed by any team member. The challenge in applying a shared care model to cancer care is that aspects of this care cannot be equally shared.
Some insight into how this might be accomplished is demonstrated in the study from Denmark by Nielsen et al. (38). These investigators conducted a randomized controlled trial of a shared care program for newly diagnosed cancer patients. This trial included several elements: 1) oncologists providing information to primary care physicians about patients’ cancer, treatment, and side effects; 2) oncologists providing contact information that facilitated the primary care physicians’ access to cancer care physicians and nurses working with the patients; and 3) patients receiving both written and oral information about the information package that their primary care physicians received and encouragement to contact their primary care providers with any concerns appropriate to this outpatient setting. This intervention increased the number of contacts the newly diagnosed cancer patients had with their primary care physicians and decreased their feelings of being left “in limbo.” These findings were especially true for younger patients and men. It did not demonstrate improvements in patients’ quality of life or performance of daily activities, however.
Recognizing the limitations of implementing shared care models for all aspects of cancer care, a number of cancer care centers and advocacy groups have responded to cancer patients’ needs by developing case management, counseling, and nutritional and navigation resources (39) that use elements of a shared care model. These services are highly rated by patients and cancer care providers, yet not all patients have access to them.
How care is integrated between providers during the early treatment period is important to patients and providers, but our review of the published and unpublished literature reveals that limited research to date has systematically addressed how shared care models should be structured to meet the specific challenges to collaborative care outlined in this article. This is an area ripe for developmental and evaluative research.
Information Exchange
Emerging evidence from the United Kingdom and the Netherlands suggests that interventions targeting communication processes between primary care and cancer care physicians may hold the greatest promise for improving their collaboration, as these interventions resulted in greater care integration, higher patient-reported satisfaction with care, and improvements in meeting patients’ and providers needs (40–43). Communication interventions have included structured information packets addressing patients’ cancer, prognosis, treatment protocol, and side effects, as well as reliable provision of hospital discharge and outpatient visit notes. Primary care physicians uniformly reported satisfaction with these communication tools. Other salutary outcomes related to these tools included improved knowledge about their patients’ cancers and improved ability to support and counsel their cancer patients. An Australian randomized trial by Jefford et al. using tailored chemotherapy information faxed to general practitioners as compared with usual communication specifically demonstrated that this intervention increased primary care providers’ confidence in managing adverse effects of chemotherapy (43).
Multidisciplinary Case Conferences
Multidisciplinary case conferences, or tumor boards, represent a mechanism within the cancer care system that facilitates collaboration between specialist providers to develop comprehensive care plans for patients. These meetings, in which an individual case is reviewed in detail, often include the participation of other professionals such as nurses or nutritionists to develop supportive care plans for patients who are identified as having needs in these areas. In a number of jurisdictions, the multidisciplinary case conference is considered essential to providing high-quality care to patients, as these conferences facilitate best care practices using evidence-based guidelines or policies as well as support consistency (44). They also are a unique mechanism to support continuing medical education around new and emerging treatments for all team members. With new technologies, such as telehealth and videoconferencing, the potential now exists to include the primary care provider in a case discussion of a particular patient. This may have particular benefits in discussions around understanding patient preferences and compliance as well as negotiating roles within the providers’ scope of practice (such as providing supportive care). The opportunity to have a real-time discussion involving all team members holds the promise of a truly collaborative practice that addresses gaps in continuity, care coordination, and role clarity (45). To date, we have found no published literature on inclusion of primary care physicians in the multidisciplinary case conference process, suggesting that this is an area that merits consideration and testing.
Discussion and Recommendations for Further Research
The importance of the primary care physician's role during the initial treatment period as advocate, medical interpreter, provider of noncancer and supportive care, and manager of treatment sequelae has been extensively documented from the perspectives of specialist providers of cancer care, patients, and primary care providers themselves (12,13). Despite literature supporting the role of primary care providers in caring for patients with cancer, numerous published and unpublished studies have demonstrated ongoing difficulties in the overall organization of cancer care and in particular, integration of services by specialty and primary care physicians. Several studies examining tools that facilitate communication between primary care and cancer care physicians have demonstrated benefits to patients, including patients feeling less in limbo during cancer care as well as physicians feeling more capable of supporting their patients and managing side effects of their treatment. Although these studies hold promise for improving the care of cancer patients, a number of caveats must be invoked when drawing conclusions from this literature.
First, the concept of collaborative care between primary care and cancer care physicians has been variably formulated without clear definition of explicit processes or expected outcomes of care. No single accepted definition of care collaboration exists in general medical care or specifically for cancer care. The shared care model is perhaps the best defined and best developed strategy for care collaboration. Yet the shared care model can be devised in a myriad of ways, making it difficult to identify the exact components of the model that might support collaboration between providers. However, the concepts of role clarity, improved communication, and knowledge exchange between providers are common threads shared by shared care and the communication augmentation strategies tested in the published studies.
Second, the published literature examining strategies to increase primary care and specialty physician collaboration preceded the current era of electronic medical records. Because evidence suggests that interventions with a strong component of information exchange influence outcomes, it is important that future work harness the information technology systems now in place to facilitate this exchange. This is examined in depth in the accompanying article in this Journal by Hesse et al. (46).
Third, many of the information exchange strategies reported in the literature emphasized unidirectional knowledge transfer from cancer care specialists to primary care physicians. These strategies do not recognize the important contribution that a primary care physician's knowledge of a patient's psychosocial status, comorbidity, and personal and family resources may make to a cancer care physician's care. Future interventions should consider testing methods of bidirectional information exchange, perhaps within the context of multidisciplinary case conferences, to examine whether knowledge exchange from primary care physicians to cancer care specialists contributes to high-quality cancer care.
Fourth, few of the published studies were randomized controlled trials. Further research using rigorous study design is needed to confirm the beneficial effects of shared care and augmented communication strategies in a variety of settings and with a range of patients and physicians. It is important to use established conceptual models from other chronic diseases, such as cardiovascular disease and diabetes (47), to define the process of care outcomes that collaborative care models and augmented information exchange may influence.
It is important that collaborative care model development takes place in the context of the health-care system within which patients are situated. It is notable that the literature in shared care and improved communication between primary care physicians and cancer care specialists originates primarily in countries with health-care systems in which primary care serves as the base—Europe, Canada, and Australia. The incentives for collaborative care in these countries may relate to limitations in the availability of cancer care specialists as well as to the intention to improve health-care quality. In the United States, where cancer care specialists are more plentiful and interest in primary care is waning, collaborative care models may be more difficult to implement.
The initial treatment phase of the cancer continuum is an area that is ripe for research. Descriptive research has clearly identified the gaps in coordination of care between primary care and cancer care physicians at this point in the cancer care trajectory. Intervention research is now needed to address these gaps. Some of the preliminary intervention studies presented, particularly in the area of tailored knowledge exchange, suggest that it may be possible to improve care across the interface of primary care and cancer care physicians. Although intervention studies from other chronic diseases, such as diabetes or cardiovascular disease, suggest that it is possible to improve the interface between providers in focused disease-specific outcomes (37) and provider-specific outcomes (eg, knowledge, satisfaction, and care delivery), the complexity of treatment for different cancer types raises questions about whether these findings are generalizable to cancer care.
Our review suggests that there is potential to achieve improvements in care process outcomes such as provider role clarity, knowledge, and satisfaction; in patient outcomes such as level of unmet supportive and other care needs; and in disease management parameters such as appropriateness, timeliness, and quality of care, including care for psychosocial concerns and comorbid medical conditions. To have a meaningful impact on initial cancer care, future research must address the needs of cancer patients and their providers during the primary treatment phase and focus on the specific gaps in processes of collaborative care, which can inform the development of context-specific interventions. These interventions in turn must be evaluated using rigorous, prospective designs so that the most effective strategies for improving the care of cancer patients can be identified.
Figure 1.
Types and transitions in care that constitute the process of care across the cancer continuum.
Funding
Ontario Ministry of Health and Long Term Care and Cancer Care Ontario (J.S.).
References
- 1.Ayanian JZ, Chrischilles EA, Fletcher RH, et al. Understanding cancer treatment and outcomes: the Cancer Care Outcomes Research and Surveillance Consortium. J Clin Oncol. 2004;22(15):2992–2996. doi: 10.1200/JCO.2004.06.020. [DOI] [PubMed] [Google Scholar]
- 2.Hewitt M, Greenfield S, Stovall E, editors. From Cancer Patient to Cancer Survivor: Lost in Transition. Washington, DC: Institute of Medicine; 2005. [Google Scholar]
- 3.Websters Dictionary Online. www.merriam-webster.com. Accessed December 1, 2009. [Google Scholar]
- 4.Haggerty J, Reid R, Freeman G, Starfield B, Adair C, Mckendry R. Continuity of care: a multidisciplinary review. BMJ. 2003;327(7425):1219–1221. doi: 10.1136/bmj.327.7425.1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Contandriopoulos AP, Denis JL, Touati N, Rodriguez C. The integration of health care. dimensions and implementation. University of Montreal working paper N04-01. Published June 2003. [Google Scholar]
- 6.Phillips R, Dodoo M, Green L, et al. Usual source of care: an important source of variation in health care spending. Health Aff. 2009;28(2):567–577. doi: 10.1377/hlthaff.28.2.567. [DOI] [PubMed] [Google Scholar]
- 7.Whelan T, Grunfeld E, Sussman J, et al. An evaluation of continuity of cancer care through regional supportive cancer care. Ottawa, ON: Canadian Health Services Research Foundation; http://www.chsrf.ca/final_research/ogc/pdf/whelan_e.pdfAccessed November 15, 2009. [Google Scholar]
- 8.Dworkind M, Towers A, Murnaghan D, Guibert R, Iverson D. Communication between family physicians and oncologists: qualitative results of an exploratory study. Cancer Prev Control. 1999;3(2):137–144. [PubMed] [Google Scholar]
- 9.Smith GF, Toonen TR. Primary care of the patient with cancer. Am Fam Physician. 2007;75(8):1207–1214. [PubMed] [Google Scholar]
- 10.Institute for Clinical and Evaluative Sciences. Patterns of cancer care in Ontario. 2006 chap 10. http://www.ices.on.ca/file/PC_atlas_chapter_10.pdfAccessed November 15, 2009. [Google Scholar]
- 11.McConnell D, Butow P, Tattersall M. Improving the letters we write: an exploration of doctor-doctor communication in cancer care. Br J Cancer. 1999;80(3–4):427–437. doi: 10.1038/sj.bjc.6690374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Braun TC, Hagen NA, Smith C, Summers N. Oncologists and family physicians. Using a standardized letter to improve communication. Can Fam Physician. 2003;49(7):882–886. [PMC free article] [PubMed] [Google Scholar]
- 13.Sisler JJ, Brown JB, Stewart M. Family physician's roles in cancer care: survey of patients on a provincial cancer registry. Can Fam Physician. 2004;50(6):889–896. [PMC free article] [PubMed] [Google Scholar]
- 14.Hickner J, Kent S, Naragon P, Hunt L. Physicians’ and patients’ views of cancer care by family physicians: a report from the American Academy of Family Physicians National Research Network. Fam Med. 2007;39(2):126–131. [PubMed] [Google Scholar]
- 15.Grunfeld E. Primary care physicians and oncologists are players on the same team. J Clin Oncol. 2008;26(14):2246–2247. doi: 10.1200/JCO.2007.15.7081. [DOI] [PubMed] [Google Scholar]
- 16.Christakis D. Continuity of care: process or outcome? Ann Fam Med. 2003;1(3):131–133. doi: 10.1370/afm.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Starfield B. Primary and specialty care interfaces: the imperative of disease continuity. Br J Gen Pract. 2003;53(494):723–729. [PMC free article] [PubMed] [Google Scholar]
- 18.Earle CC, Neville BA. Underuse of necessary care among cancer survivors. Cancer. 2004;101(8):1712–1719. doi: 10.1002/cncr.20560. [DOI] [PubMed] [Google Scholar]
- 19.Snyder CF, Frick KD, Kantsiper ME, et al. Prevention, screening and surveillance care for breast cancer survivors compared with controls: changes from 1998 to 2002. J Clin Oncol. 2009;27(7):1054–1061. doi: 10.1200/JCO.2008.18.0950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Aziz N, Bellizzi K. Older survivors and cancer care. J Natl Cancer Inst. 2008;100(1):4–5. doi: 10.1093/jnci/djm278. [DOI] [PubMed] [Google Scholar]
- 21.Piccirillo J, Tierney R, Costas I, Grove L, Spitznagel E. Prognostic importance of co-morbidity in an hospital-based cancer registry. JAMA. 2004;291(20):2441–2447. doi: 10.1001/jama.291.20.2441. [DOI] [PubMed] [Google Scholar]
- 22.Fitch M. Supportive care for cancer patients. Hosp Q. 2000;3(4):39–46. doi: 10.12927/hcq..16542. [DOI] [PubMed] [Google Scholar]
- 23.Sanson-Fisher R, Girgis A, Boyes A, Bonevski B, Burton L, Cook P. The unmet supportive care needs of patients with cancer: supportive care review group. Cancer. 2000;88(1):226–237. doi: 10.1002/(sici)1097-0142(20000101)88:1<226::aid-cncr30>3.3.co;2-g. [DOI] [PubMed] [Google Scholar]
- 24.Hwang SS, Chang VT, Cogswell J, et al. Study of unmet needs in symptomatic veterans with advanced cancer: incidence, independent predictors and unmet needs outcome model. J Pain Symptom Manage. 2004;28(5):421–432. doi: 10.1016/j.jpainsymman.2004.02.023. [DOI] [PubMed] [Google Scholar]
- 25.Velikova G, Booth L, Smith AB, et al. Measuring quality of life in routine oncology practice improves communication and patient well-being: a randomized controlled trial. J Clin Oncol. 2004;22(4):714–724. doi: 10.1200/JCO.2004.06.078. [DOI] [PubMed] [Google Scholar]
- 26.Sussman J. Supportive care in cancer: who does what? [Abstract 8267] J Clin Oncol. 2004;22(suppl 14S) [Google Scholar]
- 27.Bulsara C, Ward AM, Joske D. Patient perceptions of the GP role in cancer management. Aus Fam Phys. 2005;34(4):299–301. [PubMed] [Google Scholar]
- 28.Anvik T, Holtedahl KA, Mikalsen H. When patients have cancer they stop seeing me. The role of the general practitioner in early follow-up of patients with cancer—a qualitative study. BMC Family Pract. 2006;7:19–26. doi: 10.1186/1471-2296-7-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Miediema B, Macdonald I, Tatemichi S. Cancer follow-up care. Patients’ perspectives. Can Fam Physician. 2003;49(7):890–895. [PMC free article] [PubMed] [Google Scholar]
- 30.Klabunde C, Ambs A, Keating N, et al. The role of primary care physicians in cancer Care. J Gen Intern Med. 2009;24(9):1029–1036. doi: 10.1007/s11606-009-1058-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Piterman L, Koritsas S. General practitioner-specialist referral process. Intern Med J. 2005;35(8):491–496. doi: 10.1111/j.1445-5994.2005.00860.x. [DOI] [PubMed] [Google Scholar]
- 32.Barnes EA, Chow E, Andersson L, et al. Communication with referring physicians in a palliative radiotherapy clinic. Support Care Cancer. 2004;12(9):669–673. doi: 10.1007/s00520-004-0643-0. [DOI] [PubMed] [Google Scholar]
- 33.Wee CC, Phillips RS, Burstin HR, et al. Influence of financial productivity incentives on the use of preventive care. Am J Med. 2001;110(3):226–228. doi: 10.1016/s0002-9343(00)00692-6. [DOI] [PubMed] [Google Scholar]
- 34.Sussman J, Evans WK, Whelan T, Bainbridge D, Schiff S, Hasler A. Toronto, ON: Research report submitted to the Ministry of Health and Long Term Care of Ontario; 2008. Family physician integration with the cancer system. [Google Scholar]
- 35.Teret C, Zulian G, Naiem A, Albrand G. Multidisciplinary approach to the geriatric oncology patient. J Clin Oncol. 2007;25(14):1876–1881. doi: 10.1200/JCO.2006.10.3291. [DOI] [PubMed] [Google Scholar]
- 36.O'Connell B, Kistjanson L, Orb A. Models of integrated cancer care: a critique of the literature. Aust Health Rev. 2000;23(1):163–178. doi: 10.1071/ah000163. [DOI] [PubMed] [Google Scholar]
- 37.Smith SM, Allwright S, O'Dowd T. Effectiveness of shared care across the interface between primary and specialty care in chronic disease management. Cochrane Database Syst Rev. 2007 doi: 10.1002/14651858.CD004910.pub2. (3):CD004910. doi:10.1002/14651858.CD004910.pub2. [DOI] [PubMed] [Google Scholar]
- 38.Nielsen JD, Palshoff T, Mainz J, Jensen AB, Oelsen F. Randomized controlled trial of a shared care program for newly referred cancer patients: bridging the gap between general practice and hospital. Qual Saf Health Care. 2003;12(4):263–272. doi: 10.1136/qhc.12.4.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Patient Navigation Research Program. Centre to reduce cancer health disparities. Rockville, MD: National Cancer Institute; 2009. http://ncipoet.cancer.gov/PatientNavigator/documents/Patient%20Navigator%20Binder.pdfAccessed March 15, 2010. [Google Scholar]
- 40.James J, Harris DJ, Mott MG, Oakhill A. Paediatric oncology information pack for general practitioners. BMJ. 1988;296(6615):97–98. doi: 10.1136/bmj.296.6615.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Johansson B, Berglund G, Hoffman K, Glimelius B, Sjoden P- O. The role of the general practitioner in cancer care and the effect of an extended information routine. Scand J Prim Health Care. 2000;18(3):143–148. doi: 10.1080/028134300453331. [DOI] [PubMed] [Google Scholar]
- 42.Kousgaard KR, Nielsen JD, Olesen F, Jensen AB. General practitioner assessment of structured oncological information accompanying newly referred cancer patients. Scand J Prim Health Care. 2003;21(2):110–114. doi: 10.1080/02813430310001725. [DOI] [PubMed] [Google Scholar]
- 43.Jefford M, Baravelli C, Dudgeon P, et al. Tailored chemotherapy information faxed to general practitioners improves confidence in managing adverse effects and satisfaction with shared care: results from a randomized controlled trial. J Clin Oncol. 2008;26(14):2272–2277. doi: 10.1200/JCO.2007.14.7710. [DOI] [PubMed] [Google Scholar]
- 44.US Department of Health and Social Services. Accelerating success against cancer. A National Cancer Institute report. NIH publication No. 06-6080. http://cancercenters.cancer.gov/documents/Accelerating_Successes_Against_Cancer_Report.pdfAccessed October 23, 2009. [Google Scholar]
- 45.Gagliardi A, Smith A, Goel V, Depetrillo D. Feasibility of multidisciplinary oncology rounds by videoconference for surgeons in remote locales. BMC Med Inform Dec Mak. 2003;3(7):3–7. doi: 10.1186/1472-6947-3-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hesse BW, Hanna C, Massett HA, Hesse NK. Outside the box: will information technology be a viable intervention to improve the quality of cancer care? J Natl Cancer Inst. 2010;40:81–89. doi: 10.1093/jncimonographs/lgq004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bodenheimer T, Wagner E, Grumbalch K. Improving primary care for patients with chronic illness. JAMA. 2002;288(14):1775–1779. doi: 10.1001/jama.288.14.1775. [DOI] [PubMed] [Google Scholar]