Abstract
Background:
Silicon hydrogel bandage contact lenses are used to enhance epithelial healing, control surface-generated pain, and prevent epithelial erosions after refractive surgery. Considering the importance of faster reepithelialization in preventing complications of photorefractive keratectomy (PRK) and the fact that the features and specifications of these commercially-available lenses are different and their performance as a postoperative bandage lenses would be different also, the aim of this study was comparison the efficacy of senofilcon A and lotrafilcon A after PRK.
Methods:
In this prospective study, 44 patients with PRK in both eyes randomly received a silicon hydrogel contact lens of senofilcon A in one eye and lotrafilcon A in other eye. Then the epithelial defect size, visual acuity and subjective level of pain and discomfort were measured for both eyes and compared on day 1, 3 and 5 postoperatively.
Results:
There was no statistical difference in rate of reepithelialization between senofilcon A and lotrafilcon A (P > 0.05). The mean pain and discomfort index was significantly lower in eyes with senofilcon A (P < 0.05). The mean subjective visual scores were similar with both bandage contact lenses (BCLs) (P > 0.05).
Conclusion:
Silicon hydrogel BCLs are safe and effective for corneal reepithelialization and have great therapeutic outcome on visual outcomes after PRK. But, senofilcon A had better effect on postoperative pain and discomfort which made it superior than lotrafilcon A. However for more conclusive results, it is recommended to study larger sample size with evaluation the possible factors responsible for the obtained findings regarding postoperative pain and discomfort.
Keywords: Bandage contact lens, silicon hydrogel contact lens, photorefractive keratectomy
INTRODUCTION
Refractive surgery is used for refractive error correction. Excimer laser corrects myopia, hyperopia, and astigmatism by ablating the anterior corneal surface. Photorefractive keratectomy (PRK), a well-established flapless refractive procedure, is one of the major refractive surgical techniques, which has been introduced since more than 20 years.[1,2]
Though the use of this technique has been decreased by introduction of laser in situ keratomileusis (LAISIK) procedure, due to its higher postoperative pain and more delayed visual recovery, but it could be an alternative to LAISIK in cases with thin corneas, and epithelial basement membrane disease (often called map-dot-fingerprint-dystrophy), and irregular corneas, and treatment of some LASIK flap complications. With the advent of wave front guided laser ablation the popularity of PRK is increasing. In addition, this technique decreases postoperative higher order optical aberrations and improves quality of vision.[3,4]
Though the therapeutic utilities of soft contact lenses have been introduced since 40 years ago, but their use became more important recently, after introduction of refractive surgery. They are used as a bandage after PRK. First, they were used to decrease postoperative pain but nowadays they used for promoting reepithelialization after PRK.[5–8]
Using hydrogel lenses for bandage purpose after corneal refractive procedures was applied first in photorefractive keratectomy (PRK).[7,9] Silicon hydrogel bandage lenses are used to protect the cornea during healing and provide pain relief.[7,9] Silicon hydrogel bandage contact lenses (BCLs) widely reported to offer improved ocular health and are 5-6 times more O2-permeable than traditional hydrogel soft lenses. Their mechanism is to prevent epithelial erosion, enhance epithelial healing, and to control surface generated pain.[10]
They are used as extended wear basis, and they should have high oxygen permeability for providing corneal metabolism.[11]
Silicon hydrogel bandage contact lenses are made of high oxygen permeability materials; this gas permeability related to the size of the intermolecular voids that allow the transmission of oxygen molecules and the gas solubility of the silicone material.[12]
Different types of silicone hydrogel lenses are available and several methods are used to manufacture them. Two of the most popular of these BCLs are senofilcon A and lotrafilcon A. They have the food and drug administration (FDA) approval for using as BCL after PRK.[13] Considering the importance of faster reepithelialization in preventing complications of PRK and the fact that the features and specifications of these commercially-available lenses are different and their performance as a postoperative bandage lenses would be different also, the aim of this study was comparison the efficacy of senofilcon A and lotrafilcon A after PRK.
METHODS
In this double-masked study, patients who had bilateral low myopia (-6.00D) and anisometropia less than 2.00 D and referred to Faize hospital, affiliated to Isfahan University of Medical Sciences, for binocular PRK surgery, from July to December 2011 were enrolled.
The Medical Ethics Committee of the Isfahan University of Medical Sciences approved the study protocol (Research project number; 390384). Written informed consent was obtained from all participants.
Patients with a history of contact lens wear during 1 month before PRK, previous refractive surgery and any condition that delays epithelial healing were excluded.
The surgical procedure was performed by one surgeon (HR). The corneal epithelium was removed by application of 20% absolute alcohol for 20-45 seconds to the corneal surface to loosen the epithelium and separate it with a hockey knife then laser ablation was performed with the technolas 217z100 excimer laser.
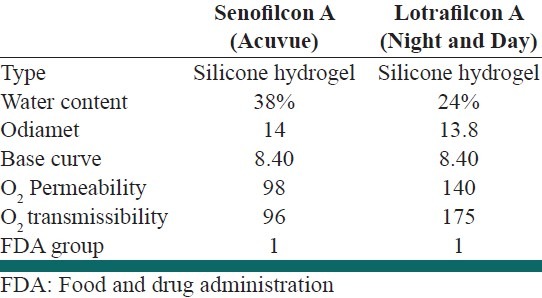
At the end of procedure, patients were randomly selected to be fitted with senofilcon A bandage contact lens in one eye and lotrafilcon A in the fellow eye by the surgeon who performed the procedure. Specifications of two studied lens, senofilcon A and lotrafilcon A are presented in Table 1.
Table 1.
Specifications of two studied lens, senofilcon A and lotrafilcon A
Postoperative medication included a combination of topical ciprofloxacin eye drops four times per day and topical betamethasone eye drops eight times per day and acetaminophen codeine for pain control.
Objective and subjective assessments 1, 3 and 5 days postoperatively were performed by two ophthalmologists unaware of the type of bandage contact lens in each eye. Objective assessments included epithelial defect size, visual acuity and subjective assessment was evaluating the patients’ pain, tearing, photophobia and discomfort using questionnaire. Pain and discomfort evaluated by using a rating scale of 0 to 4 as follows: 0 Z no discomfort or pain; 1 Z mild discomfort; 2 Z moderate burning pain; 3 Z burning pain requiring oral medication (acetaminophen codeine 325/10); 4 Z severe constant or sharp pain not relieved with narcotic pain medications.
Statistical Analysis
Obtained data was analyzed using SPSS version 18 software and chi-square and independent sample t-test. P value < 0.05 were considered as significant.
RESULTS
In this study, 44 patients (16 men and 28 women) were studied. Mean age of studied population was 27.18 ± 3.9 years.
Postoperative details regarding epithelial defect size, visual acuity and subjective level of pain and discomfort in A and lotrafilcon A 1, 3 and 5 days after operation, are presented in Table 2.
Table 2.
Postoperative details regarding epithelial defect size, visual acuity and subjective level of pain and discomfort in senofilcon A and lotrafilcon A 1, 3 and 5 days after operation
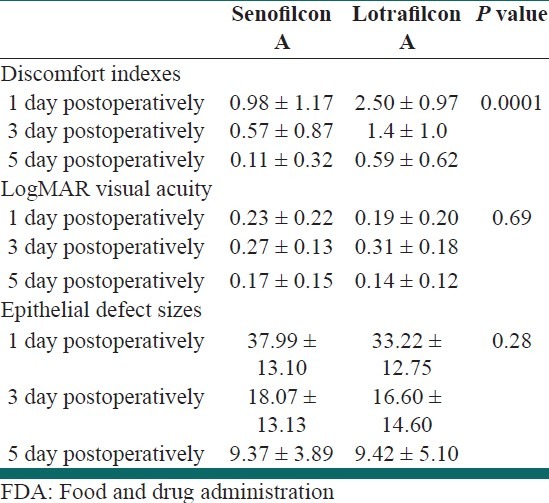
Both, two group patients had worse ucva on third day than the first day. On day five, V/A improved and 97.7% of patients reached at least on ucva of 20/40 [Figure 1].
Figure 1.
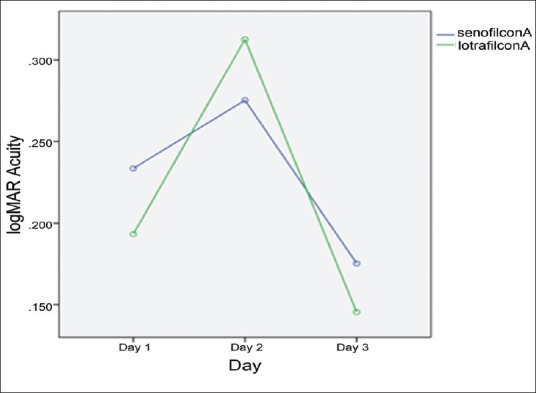
Mean logMAR visual acuity in two studied lens on 1, 3 and 5 days postoperatively (P> 0.05)
Thirty six eyes had completely reepithelialized by the fifth day; 21 (58.3%) eyes with senofilcon A and 15 (41.7%) eyes with lotrafilcon A (P > 0.05).
DISCUSSION
In this study, the outcome and efficacy of two commonly used Silicon hydrogel bandage contact lenses (BCLs) was compared. The results indicated that regarding objective variables there were not significant differences between two studied BCLs. But pain and discomfort indexes, the subjective variables, were significantly lower in eyes with senofilcon A.
As mentioned, PRK is one of the methods of choice for refractive error correction. In this technique, te corneal epithelium should be removed and sculpting of the deepithelialized corneal surface will change its refractive power.[14]
Faster reepithelialization facilitates earlier visual rehabilitation, reduction of discomfort and quicker restoration of barrier. BCLs are used to prevent corneal traumatic damage and promote reepithelialization and reduce discomfort after PRK. BCLs are fitted on deepithelialized corneas and are used on an extended wear basis, therefore, they should have high oxygen permeability. In silicon hydrogel BCLs, silicon material with bulky molecular structure creates an open polymer architecture and great O2 permeability.[15]
Many studies have confirmed the therapeutic effects of silicone hydrogel lenses as bandage contact lenses after corneal refractive surgery, since their introduction in 1998.[16–19]
The general procedure of PRK surgery requires the patient to wear a bandage contact lens for three to five days after surgery on an extended wear schedule to promote epithelial healing. The only contact lenses FDA approved for extended and continuous wear are silicone hydrogels.
Currently there are three silicone hydrogel contact lenses that are FDA approved for therapeutic use as a BCL: Lotrafilcon A, Balafilcon A, and Senofilcon A.[13]
The therapeutic efficacy of the lotrafilcon A BCL after PRK has been reported in some previous studies.[15,19,20] Accordingly, it results in reducing discomfort and faster corneal reepithelialization after the procedure.
Therefore, in this study we compared the efficacy and therapeutic outcome of lotrafilconA with another silicone hydrogel BCL, senofilcon A, from different manufacturer and with different characteristics (such as O2 permeability, O2 transmissibility, diameter and water content)(Table 1) and with same base curve (8.40 mm) after PRK. Both of the selected BCLS have FDA approval. In order to reduce the effect of environmental conditions and patient's individual healing response and achieving more accurate results, all patients were randomly fitted with these lenses and they were masked to which type of BCL was in which eye.
Some similar studies have investigated the efficacy of different BCLs in this regard, but there was not any study which compared senofilcon A with lotrafilcon A. However, mentioned studies compare the outcome of other BCLS with lotrafilcon A.
The findings of this study indicated that the rate of reepithelialization and the mean subjective visual scores of two studied BCLs were not significantly different but the mean pain and discomfort index was significantly lower in eyes with senofilcon A.
The therapeutic efficacy of the lotrafilcon A BCL after PRK has been reported in some previous studies. In a similar study in the USA, Engle and colleagues have compared the efficacy of 2 types of BCLs, etafilcon A and lotrafilcon A, after PRK. They showed that lotrafilcon A is more effective. It was more effective in reducing patient discomfort and faster corneal reepithelialization, especially during the first 48 h after PRK.[15]
Grentzelos et al., in Greece have compared the outcome of two BCLs, lotrafilcon A and lotrafilcon B after PRK and reported similar results for both studied BCLs.[19]
Edwards and colleagues in the USA, have evaluated the efficacy of two BCLs with high and low oxygen permeability, lotrafilcon A and omafilcon A, on visual outcomes after PRK. Their results indicated that rate of reepithelialization, uncorrected visual acuity, contrast sensitivity and goal of emmetropia were similar in two BCLs.[20]
Our results indicated that regarding pain and discomfort senofilcon A had superior effect than lotrafilcon A. It may be due to the difference in stiffness of lens materials. Considering the specifications of studied lenses, the water content of senofilcon A was higher than lotrafilcon A. Regarding to patients' related factors, Grentzelos et al. indicated that higher grade of pain and discomfort due to sensory nerve exposure is associated with larger epithelial defects. Similar to this study, Engle et al. did not report such a correlation, but Grentzelos reported the mentioned association. It seems that other factors as a part of pain sensation may have role, which should be investigated in future studies.[19]
In current study, both two group patients had worse ucva on third day than the first day. On day 5, V/A improved and 97.7% of patients reached at least on ucva of 20/40. A similar result reported by Grentzelos et al.[19] It may be due to that, at that time the epithelial healing process is in the center of the cornea. The findings of the current study are in line with our previous trial for relieving pain after keratectomy.[21]
CONCLUSION
In general our findings indicated that, as reported by previous studies, silicon hydrogel BCLs are safe and effective for corneal reepithelialization and have great therapeutic outcome on visual outcomes after PRK. But, senofilcon A had better effect on postoperative pain and discomfort, which made it superior than lotrafilcon A. However, for more conclusive results, it is recommended to study larger sample size with evaluation the possible factors responsible for the obtained findings regarding postoperative pain and discomfort.
Footnotes
Source of Support: The project is conducted as a thesis funded by Vice-chancellery for Research and Technology, Isfahan University of Medical Sciences
Conflict of Interest: None declared.
REFERENCES
- 1.Sakimoto T, Rosenblatt MI, Azar DT. Laser eye surgery for refractive errors. Lancet. 2006;29(367):1432–47. doi: 10.1016/S0140-6736(06)68275-5. [DOI] [PubMed] [Google Scholar]
- 2.Ghadhfan F, Al-Rajhi A, Wagoner MD. Laser in situ keratomileusis versus surface ablation: visual outcomes and complications. J Cataract Refract Surg. 2007;33:2041–8. doi: 10.1016/j.jcrs.2007.07.026. [DOI] [PubMed] [Google Scholar]
- 3.Anderson NJ, Beran RF, Schneider TL. Epi-LASEK for the correction of myopia and myopic astigmatism. J Cataract Refract Surg. 2002;28:1343–7. doi: 10.1016/s0886-3350(02)01461-x. [DOI] [PubMed] [Google Scholar]
- 4.Huang SC, Chen HC. Overview of laser refractive surgery. Chang Gung Med J. 2008;31:237–52. [PubMed] [Google Scholar]
- 5.Sedlácek J. [Possibilities of application of eye drugs with the aid of gel-contact lenses]. [Czechoslovakian] Cesk Oftalmol. 1965;21:509–12. [PubMed] [Google Scholar]
- 6.Gould HL. Therapeutic contact lenses. Int Ophthalmol Clin. 1970;10:131–41. [PubMed] [Google Scholar]
- 7.Bergenske PD, Caroline PJ, Smythe JK. Contact lens as an adjunct in refractive surgery practice. Contact Lens Spectrum. 2002;17:3037–8. [Google Scholar]
- 8.Nilsson SE. Seven-day extended wear and 30-day continuous wear of high oxygen transmissibility soft silicone hydrogel contact lenses: a randomized 1-year study of 504 patients. CLAO J. 2001;27:125–36. [PubMed] [Google Scholar]
- 9.Emslie R, Claassens A, Walters I. The use of contact lenses after refractive surgery. S Afr Optom. 2007;66:132–8. [Google Scholar]
- 10.Compañ V, Andrio A, López-Alemany A, Riande E, Refojo MF. Oxygen permeability of hydrogel contact lenses with organosilicon moieties. Biomaterials. 2002;23:2767–72. doi: 10.1016/s0142-9612(02)00012-1. [DOI] [PubMed] [Google Scholar]
- 11.Ren DH, Yamamoto K, Ladage PM, Molai M, Li L, Petroll WM, et al. Adaptive effects of 30-night wear of hyper-O2 transmissible contact lenses on bacterial binding and corneal epithelium; a 1-year clinical trial. Ophthalmology. 2002;109:27–39. doi: 10.1016/s0161-6420(01)00867-3. [DOI] [PubMed] [Google Scholar]
- 12.Karlgard CC, jones LW, moresoli C. Survery of bandage lens use in north Amorica, October-December 2002. Eye contact lens. 2004;30:25–30. doi: 10.1097/01.ICL.0000105564.71700.EE. [DOI] [PubMed] [Google Scholar]
- 13.Edwards K, Atkins N. Silicone hydrogel contact lenses, part 2; therapeutic applications. Assoc of Optom. 2002;2:26–30. [Google Scholar]
- 14.McDonald MB, Deitz MR, Frantz JM, Kraff MC, Krueger RR, Salz JJ, et al. Photorefractive keratectomy for low-to-moderate myopia and astigmatism with a small-beam, tracker-directed excimer laser. Ophthalmology. 1999;106:1481–8. doi: 10.1016/S0161-6420(99)90440-2. discussion by RD Stulting, 1488-9. [DOI] [PubMed] [Google Scholar]
- 15.Engle AT, Laurent JM, Schallhorn SC, Toman SD, Newacheck JS, Tanzer DJ, et al. Masked comparison of silicone hydrogel lotrafilcon A and etafilcon A extended-wear bandage contact lenses after photorefractive keratectomy. J Cataract Refract Surg. 2005;31:681–6. doi: 10.1016/j.jcrs.2004.09.022. [DOI] [PubMed] [Google Scholar]
- 16.Ambroziak AM, Szaflik JP, Szaflik J. Therapeutic use of silicone hydrogel contact lens in selected clinical cases. Eye Contact Lens. 2004;30:63–7. doi: 10.1097/01.ICL.0000105563.54932.44. [DOI] [PubMed] [Google Scholar]
- 17.Ozkurt Y, Rodop O, Oral Y, Comez A, Kandemir B, Dogan OK. Therapeutic applications of Lotrafilcon A silicone hydrogel soft contact lenses. Eye Contact Lens. 2004;31:268–9. doi: 10.1097/01.icl.0000163449.92288.71. [DOI] [PubMed] [Google Scholar]
- 18.Montero J, Sparholt J, Mely R, Long B. Retrospective case series of therapeutic applications of Lotrafilcon A silicone hydrogel soft contact lenses. Eye Contact Lens. 2003;29:72–5. doi: 10.1097/01.ICL.0000056622.11813.DA. [DOI] [PubMed] [Google Scholar]
- 19.Grentzelos MA, Plainis S, Astyrakakis NI, Diakonis VF, Kymionis GD, Kallinikos P, et al. Efficacy of 2 types of silicone hydrogel bandage contact lenses after photorefractive keratectomy. J Cataract Refract Surg. 2009;35:2103–8. doi: 10.1016/j.jcrs.2009.07.015. [DOI] [PubMed] [Google Scholar]
- 20.Edwards JD, Bower KS, Sediq DA, Burka JM, Stutzman RD, Vanroekel CR, et al. Effects of lotrafilcon A and omafilcon A bandage contact lenses on visual outcomes after photorefractive keratectomy. J Cataract Refract Surg. 2008;34:1288–94. doi: 10.1016/j.jcrs.2008.04.024. [DOI] [PubMed] [Google Scholar]
- 21.Razmju H, Khalilian A, Peyman A, Abtahi SH, Abtahi MA, Akbari M, et al. Preoperative Topical Diclofenac and Ketorolac in Prevention of Pain and Discomfort Following Photorefractive Keratectomy: A Randomized Double masked Placebo-controlled Clinical Trial. Int J Prev Med. 2012;3(Suppl 1):S199–206. [PMC free article] [PubMed] [Google Scholar]


