Abstract
Background
Falls often result from failed responses to unexpected, externally applied perturbations. Whether performance-based, reaction-based and/or adaptation-based assessments tools can predict future falls among community-dwelling older adults is unknown.
Purpose
This preliminary prospective study examined the relationship between older adults’ future fall risk and their reactive responses and adaptation to repeated slips, and their functional status.
Methods
Thirteen community-dwelling adults (>64 years) were exposed initially to a session of repeated slips. About 30-months later, self-reported falls experience data were collected for the preceding year from these participants. Slip outcome (fall, loss-of-balance, or recovery), slip score (weighted sum of slip outcomes), TUG scores, and future fall incidence were recorded.
Results
Four subjects who reported at least one fall had significantly higher slip scores than the rest. In contrast, neither failed recovery on the first slip, nor a higher TUG score predicted greater odds of future falls.
Conclusion
Community-dwelling older adults’ adaptability to externally imposed perturbations may reveal their future fall risk.
Keywords: skill acquisition, Timed Up-and-Go, volitional performance, perturbation recovery, community-dwelling
INTRODUCTION
A large number and variety of tools available for assessment of fall risk can make choosing the most appropriate tool challenging [1], and there is no clear evidence that any one screening tool is most useful for identifying those at risk of falling [2]. Clinical tools typically used for assessing fall risk comprise various self-initiated, volitional activities. Many are practical because they are easy to perform, require little time, equipment and training, and they offer a quantifiable means of documenting patient progress and status. For example, the Timed Up and Go test (TUG) is an excellent instrument for fall prediction,[3] with evidence of high sensitivity and specificity.[4] However, certain evidence does indicate that this test is more appropriate for older people who are frail, use walking aids, or who have other co-morbidities, than for community-dwelling older adults.[5] Another class of clinical tests of balance and stability, posturography, quantifies postural sway in standing using force platforms.[6] Measuring volitional postural sway to test individuals’ limits of stability has demonstrated potential to detect balance deficits and differentiate older individuals with a history of falling from those without;[7] however, its ability to predict future falls in community-dwelling older adults is debatable,[8].
One factor that can limit clinical tools in identification of community-dwelling individuals who are at risk for falls relates to the ceiling effect, in which the sensitivity of the measurement is compromised by a lack of variability in maximum performance scores. Another potential limitation is that they are not designed to test reactive responses, which are most often one’s critical defense against a fall. Efforts have been made to assess “dynamic” posturography,[9] by introducing perturbations during quiet standing, as in the postural stress test[10] or the Motor Control Test.[11] The validity of using “static”, “dynamic”, and “reactive” components of standing balance to identify healthy older adults, who are nonetheless at heightened risk of falling, has been questioned.[12] Limitations may arise with such tests because they involve quiet standing, whereas most falls occur during dynamic activities (e.g., walking, stair-climbing, sit to stand transfers).[13] Additionally, the perturbation magnitude may be insufficient to induce balance losses and falls in healthy older adults.
To address these issues, a series of experiments has been conducted which mimic real-life conditions. In these studies, falls are induced experimentally with unannounced, large perturbations (i.e., sufficient to induce balance loss or falls) during functional activities, in a well protected laboratory environment.[14–17] Further, a previous study revealed that, upon repeated slip exposure during sit-to-stand, subjects adapted rapidly to reduce fall incidence from 73% initially to less than 5% by the fifth repeated slip.[15] When they were subjected to another slip after a block of nonslip trials, only 41% of subjects experienced a loss of balance (versus 100% for the first, novel slip) and 20% a fall.[15] Based on these observations, a connection was hypothesized between poor adaptation and retention of fall-resisting skills in the laboratory [17] (or clinical setting) and a greater risk for balance loss and falls in everyday living. Few studies address this essential question.[18]
The purpose of this study of community-dwelling older adults was to determine, whether future risk of falls in everyday living could be predicted by: a) their initial reaction (ie, fall, loss of balance, or successful recovery) to an unannounced, novel slip induced during chair rise, b) their subsequent adaptability to repeatedly induced slips, or c) their functional status measured by the TUG. The ability to adapt to the slips was defined by how successfully and how rapidly throughout the session individuals reduced the incidence of backward losses of balance or falls. Operationally, “good” adaptation within a test session would involve fewer losses of balance and falls (i.e., lower overall slip score) and/or a successful recovery upon the second slip (indicating rapid adaptation) which would be maintained through the last slip (indicating an adaptation plateau) [17]. In this preliminary study, it was postulated that all three measures (initial slip reaction, adaptability, and TUG score) would correlate with the likelihood of future falls, because each reflects a different aspect of a person’s capacity for resisting falls.
METHODS
Subjects
The laboratory assessment session included 13 older adults [9 men; age mean (SD): 72+5, range 65–85 years], who gave written informed consent and were paid to participate. Older adults were ambulatory, community-dwelling individuals, free of musculoskeletal, neurological, cognitive, or other systemic disorders, as assessed by a health questionnaire. Subjects who were classified as osteopenic or osteoporotic,[19] scored below 25 on the Folstein Mini Mental State Exam, or demonstrated symptomatic postural hypotension were also excluded. Institutional Review Board approval was obtained.
Assessment protocols
For the TUG test, subjects were seated in a chair, asked to rise and walk to a line on the floor (3 m ahead), turn around, return to the chair and sit, “at your normal pace.” One practice trial was given for each subject. They were made aware that they would be timed.[3] Scores were the time, in seconds, to complete the task.[3]
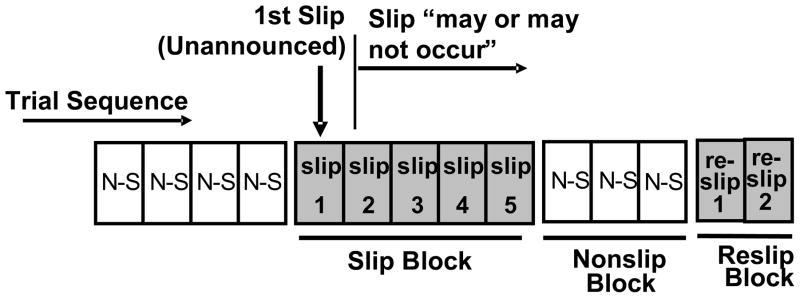
Experimental slips were induced, at seat-off during a sit-to-stand task, by computer -controlled release of two sliding platforms beneath the subject’s feet.[15, 20] Once released, the platforms were free to translate in the anterior direction on low-friction linear bearings, until they reached the maximum slip displacement of 24 cm. Platform movement was terminated by a latch mechanism at the end of the low friction tracks. All subjects wore a full body safety harness, attached by ropes at the shoulders to a ceiling mounted support. All subjects wore their own, comfortable, walking shoes. Once the foot was in contact with the plate, there was very little relative movement between the plate and the subject’s foot. Thus, the shoe characteristics could not influence the slip properties.[21] Subjects were informed that they would initially be performing trials of sit-to-stand, “as fast as possible”, and that “later on” a slip would take place. There were four nonslip trials prior to the first slip, during which subjects were entirely unaware of any forthcoming trial condition. Following the first slip, subjects were informed of the possibility of slipping on subsequent trials. It was emphasized that they should “try not to fall,” by remaining standing “still” after platform movement. After the first slip, subjects underwent a block of 4 consecutive slipping trials, followed by a nonslip block of at least 3 consecutive unperturbed trials, then 2 further slipping trials. Thus, there were a total of 7 slip trials (Figure 1).
Figure 1.
The sequence of trials comprised four initial nonslip (N-S) trials, followed by a slipping block, a nonslip block, then 2 reslip trials. Slip trials are shown in gray, nonslip trials in white. The first slip was without warning. Thereafter, subjects were only aware that a slip “may or may not occur.”
Slip-recovery outcomes
A computer algorithm determined the outcomes based on preset, objective criteria input from the collected kinematic and kinetic data. When the recovery heel marker was posterior to the slipping heel marker, as indicated by motion data collected at 60 Hz (Peak Performance Motion Capture System, Englewood, CO), the trial was classified, “loss of balance with recovery stepping.” Trials in which the subject stood without taking any step(s) were classified as, “successful recovery.” A fall was identified if a line connecting the bilateral hip markers descended to within 5% body height of its initial seated height,[15] and was verified with readings from a load cell in series with the harness (average force exceeding 4.5% body weight over any one-second period). Each slip outcome was scored 0 (successful recovery), 1 (loss of balance), or 2 (fall). The slip outcome scores for the 7 trials were summed for each subject and identified as the “slip score,” ranging from 0 to 14. Higher “slip scores” indicated higher overall incidence of falls and loss of balance.
Follow-up fall experience study
Subjects were contacted by telephone between 29 and 32 months [mean (SD): 30.6 (1.0) months] after their initial laboratory tests (at which time they had not been informed about this future contact) to collect information about fall occurrences. They were informed, both verbally and in writing, that a fall should be considered any event in which they landed unintentionally (emphasized) on a lower surface such as a chair, the floor or the ground. They were asked a series of open-ended questions as to the number of falls they had experienced in the12 months immediately prior to the call. If falls had occurred, they were asked to provide details about the fall. The results were categorized and tallied as in previous studies.[22]
Data analysis
Data were summarized using descriptive statistics. Age and TUG scores between subjects who reported falls in the follow-up interview and those who did not were compared using a t-test (age) or Fisher exact test (slip outcome and slip score). Using an alpha level of 0.05, the sample size used would have an 80% power to detect a 1.7 standard deviation difference between fallers and non-fallers using a two-sided t-test. Because the sample size was small, we also conducted a nonparametric test using the Mann-Whitney U test. A sensitivity, specificity, and likelihood ratio analysis was performed for each predictive variable between fallers and non-fallers. Statistical significance was established at an alpha level of 0.05 throughout. All statistical analyses were performed using SAS 9.1 statistical software (SAS Inc., Cary, NC).
RESULTS
Four of the 13 participants reported a future fall when surveyed after the initial laboratory assessment; 3 fell once and 1 person fell twice. Subjects who fell on the first induced slip were no more likely to report a future fall than those who recovered on the initial slip (P>.05). Similar TUG scores were found for both groups, and they were not significantly associated with future falls (Table 1). In contrast, subjects who reported falls on follow-up had significantly higher overall falls and loss of balance incidence during the initial assessment (higher slip scores) than those who did not experience any future falls (Table 1). In particular, subjects who did not lose balance during the second reslip trial were significantly less likely to report falls experienced in the year preceding the survey than those who lost balance in that same trial.
Table 1.
Sample Characteristics
| Variables | Fall (N=4) | No Fall (N=9) | P value | ||
|---|---|---|---|---|---|
|
| |||||
| Mean | SD | Mean | SD | U-test | |
| Age (years) | 69.8 | 5.0 | 73.6 | 5.0 | .12 |
| Timed Up and Go test (sec) | 9.0 | 1.5 | 8.9 | 1.2 | .94 |
| Slip Score | 7.3 | 0.9 | 5.2 | 1.5 | .03 |
Results organized by self-reported “Fall” versus “No Fall” experienced in the past 12 months
A higher overall slip score or having lost balance during the second reslip trial was associated with greater likelihood of future falls (P=.02, Table 2) than a lower slip score or not having lost balance during the second reslip trial. In comparison, a failed recovery (loss of balance or fall) on the first induced slip did not significantly increase the likelihood of future falls (P>.2) nor did a higher TUG score (P=.85), nor the outcomes of any of the other slip trials (P>0.2 for Slip #2 - #5 and reslip #1). The slip score and the second reslip outcome demonstrated a predictive ability of 85%. Overall slip score had both high sensitivity and specificity (75% and 89% respectively, Table 3). A loss of balance on the second reslip correctly classified 2 of 4 fallers (50% sensitivity), and all 9 non-fallers (100% specificity). Although the TUG had a similar sensitivity as the second reslip trial, it had a lower specificity (56%), affecting its predictive value (46%). Conversely, though failed recoveries on the first initial slip trials accurately classified all 4 fallers, it classified none of the non-fallers.
Table 2.
Slip test Results
| Fall (N =4) | % | No Fall (N=9) | % | Fisher exact test | |
|---|---|---|---|---|---|
|
|
|||||
| Slip #1 | 1.00 | ||||
| Successful recovery | 0 | 0 | 0 | 00 | |
| Loss of balance | 1 | 25 | 3 | 75 | |
| Fall | 3 | 33 | 6 | 67 | |
| Slip #2 | .27 | ||||
| Successful recovery | 0 | 0 | 1 | 100 | |
| Loss of balance | 2 | 22 | 7 | 78 | |
| Fall | 2 | 67 | 1 | 33 | |
| Slip #3 | .53 | ||||
| Successful recovery | 0 | 0 | 3 | 100 | |
| Loss of balance | 3 | 37 | 5 | 63 | |
| Fall | 1 | 50 | 1 | 50 | |
| Slip #4 | .56 | ||||
| Successful recovery | 1 | 17 | 5 | 83 | |
| Loss of balance | 3 | 43 | 4 | 57 | |
| Fall | 0 | 0 | 0 | 0 | |
| Slip #5 | 1.00 | ||||
| Successful recovery | 2 | 33 | 4 | 67 | |
| Loss of balance | 2 | 29 | 5 | 71 | |
| Fall | 0 | 0 | 0 | 0 | |
| Reslip #1 | .47 | ||||
| Successful recovery | 1 | 33 | 2 | 67 | |
| Loss of balance | 2 | 22 | 7 | 78 | |
| Fall | 1 | 100 | 0 | 0 | |
| Reslip #2 | .05 | ||||
| Successful recovery | 2 | 18 | 9 | 82 | |
| Loss of balance | 2 | 100 | 0 | 0 | |
| Fall | 0 | 0 | 0 | 0 | |
Results organized by self-reported “Fall” versus “No Fall” experienced in the past 12 months
Table 3.
Sensitivity, Specificity, and Likelihood Ratios of Fallers and Non-Fallers.
| Predictive Variables | Sensitivity [fallers] % (n) | 95% CI | Specificity [non-fallers] % (n) | 95% CI | Overall prediction % | Likelihood ratios (95% CI) | Likelihood ratios (P value) |
|---|---|---|---|---|---|---|---|
| TUG* score (> 9) | 50 (2/4) | (9.2,90.8) | 56 (5/9) | (40.2,96.1) | 46 | 1.1 (0.14,5.78) | .85 |
| Slip score (>6) | 75 (3/4) | (21.9,98.7) | 89 (8/9) | (50.7,99.4) | 85 | 6.8 (1.23,46.60) | .02 |
| Slip #1† | 100 (4/4) | (39.6,100) | 0 (0/9) | (0,37.1) | 31 | 1.0 (0.17,7.10) | .99 |
| Slip #2† | 100 (4/4) | (39.6,100) | 11 (1/9) | (0.6,49.3) | 38 | 1.1 (0.06,2.81) | .30 |
| Reslip #1† | 75 (3/4) | (21.9,98.7) | 22 (2/9) | (3.9,59.8) | 38 | 1.0 (0.17,7.10) | .91 |
| Reslip #2† | 50 (2/4) | (9.2,90.8) | 100 (9/9) | (62.9,100) | 85 | > 999 (n/a) | .02 |
Timed Up and Go test
Outcome of loss of balance or fall
DISCUSSION
These findings partially support the hypotheses that responses to a series of slips induced experimentally during a sit-to-stand task would serve as a good predictor of future fall risk. Specifically, adaptability to repeated slips, as indicated by a lower slip score (i.e., fewer overall balance losses or falls over repeated slips) and a successful recovery on the second reslip were indeed associated with a lower likelihood of future falls. The initial response to the novel slip and the TUG scores, however, did not yield similar predictions of future falls. The positive findings from the test would be especially important as many falls occur during transitions such as sit-to-stand[13] and this task has often been a key component of fall risk assessment.[23, 24]
The reason that the behavioral outcome on the first, novel slip proved to be a poor predictor of future fall risk may be because, in this trial, all the subjects lost balance and exhibited a failed recovery. Thus, the ability to predict those who would not fall in the future was poor (0% specificity), although the sensitivity was high. Previous studies have indicated that in just 1 or 2 trials of repeated slip exposure, subjects can reach a steady state characterized by improved stability and drastically reduced falls incidence.[15, 25] Just as the recovery outcome of the first slip depends on a person’s reaction to an unexpected perturbation, the outcome of later slips reflects subjects’ ability to adapt. The falls incidence of 31% (4/13) in the previous year reported in our study is about the median of the range reported in previous studies.[26, 27]
Such adaptation may occur through recalibration of an individual’s internal representation of stability limits as a result of sensorimotor feedback inputs received from the repeated perturbation experience. These findings concur with previous findings that older adults with a history of greater fall incidence may also have greater difficulty adapting to different sensory environments,[8, 28, 29] and have difficulty adapting to repeated stance perturbations.[28, 30] As the second reslip was induced after a block of nonslip trials, the performance on this trial signifies that the subjects’ adaptive changes had reached a steady state under unpredictable conditions (slip or nonslip); likewise, this may also indicate a better capacity for short term retention of the acquired adaptation. Typically, the most dramatic improvements in the rate of performance are seen from the first to second and the second to the third repeated slip trials;[15, 31, 32] hence, the expectation was that the second slip outcome would have been a critical fall risk predictor. A future study with a larger sample size may show this to be the case. Nonetheless, this study still provides preliminary evidence to support the idea that a person’s ability to adapt to perturbations could be a key in identifying and reducing fall risk.
Adaptation to repeated perturbations was a better predictor of future falls among community-dwelling older adults than the functional mobility assessment based on a volitional task (the TUG). The control of balance and stability during volitional movements can be fundamentally different from that required during responses to perturbations.[33] For instance, the loading-unloading pattern seen with anticipatory control in volitional stepping can be drastically altered during perturbation-induced (reactive) protective stepping.[34] Moreover, although feed-forward controlled proactive adjustments and changes in reactive control of dynamic stability have been shown to contribute to the successful recovery from a slip during walking,[31] it was proposed that experiencing specific sensory inputs through perturbation was key to modifying the future motor response[35] and improving the outcome of the slip. In line with these findings, recent evidence has raised questions about the ability of clinical balance tests to predict fall risk in a community-dwelling, elderly population.[36] Further, the results are in accordance with previous literature in which the TUG scores for community dwelling older adults have been relatively low (i.e. less than 12 seconds), with poor specificity and responsiveness.[5, 36]
The present study has its limitations; the first is, obviously, the small sample size. Based on the assumption that fall incidence among older adults in real-life is about 30% annually, a sample size of 200 subjects would be needed (adjusted for the estimated annual attrition rate of 35%) to provide adequate statistical power to assess this paradigm that would predict healthy older adults’ annual fall risk. Second, older adults may have over- or under-reported the actual incidence of falls in telephone interviews.[37] The subjects did not keep a fall diary, thus the results depended on their memory. The effects of inaccurate recall and recall bias could be mitigated in a prospective study by using a variety of tools such as falls calendars or periodic telephone interviews. [38, 39] If a retrospective, self-report design is to be used, on the other hand, a longer recall period, namely one year, is preferable to a shorter period. [40, 41] For this study, since the subjects were healthy older adults with no other neuromuscular or systemic disorders, their reporting could be quite accurate. Further, based on the screening of their cognitive ability and memory at the time of the laboratory test, it was assumed that subjects would be in a condition to recall major events (such as a fall) that occurred in the last 12 months. Third, since the subjects were community-dwelling, they constitute a more active and fit sample of the population of older adults. In fact, in this population more typical clinical tools have been shown to encounter ceiling effects and the current paradigm may be relatively more challenging. Fourth, the study examined only slip-related falls because recovery from slip-related falls is very challenging and the resulting fall itself dangerous, causing debilitating injuries (hip fractures) in older adults. However, the prospective study correlated forward slip-related falls induced in the laboratory to all other types of falls experienced in daily-living. Finally, an assessment that requires inducing perturbations during a daily activity will likely be more costly to conduct than volitional performance tests without perturbation. The added cost associated with assessments based on reaction and adaptation to external perturbations would be justified, however, if such tests can accurately demonstrate, in a safe environment, the future risks of falls among community-dwelling older adults. Yet, despite these limitations, the rationale for this innovative conceptual framework, per se, of using one’s adaptability to predict his/her future falls risk, may be sufficiently attractive to warrant further investigation.
In summary, the present study provided direct, yet preliminary evidence that links adaptation to perturbations with falls risk assessment among older adults. This lends credence to a new theoretical framework based on using measures of how quickly and effectively a person is able to adapt to potentially life threatening perturbations in determining the future likelihood of falls induced by similar perturbation in everyday living.
Acknowledgments
The initial laboratory tests were conducted at the Programs in Physical Therapy at Northwestern University Medical School, and funded by NIH R01-AG16727-01 (YCP) and a grant from the Whitaker Foundation. The participants were recruited from the data base established by Buehler Center on Aging at Northwestern University Medical School. The authors appreciated the invaluable comments provided by Mike Pavol, PhD.
References
- 1.Perell-Gerson K, Edelstein J. Guest Editorial: Complexities of fall prevention. J Rehabil Res Dev. 2008;45:vii–viii. [PubMed] [Google Scholar]
- 2.Gates S, Smith LA, Fisher JD, et al. Systematic review of accuracy of screening instruments for predicting fall risk among independently living older adults. J Rehabil Res Dev. 2008;45:1105–16. [PubMed] [Google Scholar]
- 3.Podsiadlo D, Richardson S. The timed “Up & Go”: A test of basic functional mobility for frail persons. J Am Geriatr Soc. 1991;39:142–148. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]
- 4.Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test.[see comment] Phys Ther. 2000;80:896–903. [PubMed] [Google Scholar]
- 5.Lin MR, Hwang HF, Hu MH, et al. Psychometric comparisons of the timed up and go, one-leg stand, functional reach, and Tinetti balance measures in community-dwelling older people. J Am Geriatr Soc. 2004;52:1343–8. doi: 10.1111/j.1532-5415.2004.52366.x. [DOI] [PubMed] [Google Scholar]
- 6.Fernie GR, Gryfe CI, Hilliday PJ, et al. The relationship of postural sway in standing to the incidence of falls in geriatric subjects. Age Ageing. 1982;11:11–16. doi: 10.1093/ageing/11.1.11. [DOI] [PubMed] [Google Scholar]
- 7.Horak FB, Shupert CL, Mirka A. Components of postural dyscontrol in the elderly: a review. Neurobiol Aging. 1989;10:727–38. doi: 10.1016/0197-4580(89)90010-9. [DOI] [PubMed] [Google Scholar]
- 8.Woollacott MJ, Shumway-Cook A, Nashner LM. Aging and posture control: Changes in sensory organization and muscular coordination. Int J Aging Hum Dev. 1986;23:97–114. doi: 10.2190/VXN3-N3RT-54JB-X16X. [DOI] [PubMed] [Google Scholar]
- 9.Wolfson L, Whipple R, Derby CA, et al. A dynamic posturography study of balance in healthy elderly. Neurology. 1992;42:2069–2075. doi: 10.1212/wnl.42.11.2069. [DOI] [PubMed] [Google Scholar]
- 10.Wolfson LI, Whipple R, Amerman P, et al. Stressing the postural response: A quantitative method for testing balance. J Am Geriatr Soc. 1986;34:845–850. doi: 10.1111/j.1532-5415.1986.tb07256.x. [DOI] [PubMed] [Google Scholar]
- 11.Monsell EM, Furman JM, Herdman SJ, et al. Computerized dynamic platform posturography. Otolaryngol Head Neck Surg. 1997;117:394–8. doi: 10.1016/S0194-5998(97)70132-3. [DOI] [PubMed] [Google Scholar]
- 12.Topp R, Mikesky A, Thompson K. Determinants of four functional tasks among older adults: an exploratory regression analysis. J Orthop Sports Phys Ther. 1998;27:144–53. doi: 10.2519/jospt.1998.27.2.144. [DOI] [PubMed] [Google Scholar]
- 13.Rubenstein LZ, Josephson KR, Robbins AS. Falls in the nursing home. Ann Intern Med. 1994;121:442–451. doi: 10.7326/0003-4819-121-6-199409150-00009. [DOI] [PubMed] [Google Scholar]
- 14.Bortolami SB, DiZio P, Rabin E, et al. Analysis of human postural responses to recoverable falls. Exp Brain Res. 2003;151:387–404. doi: 10.1007/s00221-003-1481-x. [DOI] [PubMed] [Google Scholar]
- 15.Pavol MJ, Runtz EF, Edwards BJ, et al. Age influences the outcome of a slipping perturbation during initial but not repeated exposures. J Gerontol A Biol Sci Med Sci. 2002;57:M496–503. doi: 10.1093/gerona/57.8.m496. [DOI] [PubMed] [Google Scholar]
- 16.Pijnappels M, Bobbert MF, van Dieen JH. Control of support limb muscles in recovery after tripping in young and older subjects. Exp Brain Res. 2005;160:326–33. doi: 10.1007/s00221-004-2014-y. [DOI] [PubMed] [Google Scholar]
- 17.Bhatt T, Wang E, Pai Y-C. Retention of Adaptive Control over Varying Intervals: Prevention of Slip-induced Backward Balance Loss during Gait. J Neurophysiol. 2006;95(5):2913–2922. doi: 10.1152/jn.01211.2005. [DOI] [PubMed] [Google Scholar]
- 18.Brauer SG, Burns YR, Galley P. A prospective study of laboratory and clinical measures of postural stability to predict community-dwelling fallers. J Gerontol A Biol Sci Med Sci. 2000;55:M469–76. doi: 10.1093/gerona/55.8.m469. [DOI] [PubMed] [Google Scholar]
- 19.Thompson PW, Taylor J, Oliver R, et al. Quantitative ultrasound (QUS) of the heel predicts wrist ad osteoporosis-related fractures in women aged 45–75 years. Journal of Clinic Densitom. 1998;1:219–225. doi: 10.1385/jcd:1:3:219. [DOI] [PubMed] [Google Scholar]
- 20.Pavol MJ, Pai YC. Feedforward adaptations are used to compensate for a potential loss of balance. Exp Brain Res. 2002;145:528–538. doi: 10.1007/s00221-002-1143-4. [DOI] [PubMed] [Google Scholar]
- 21.Yang F, Pai Y-C. Correction of the inertial effect resulting from a plate moving under low friction conditions. J Biomech. 2007;40:2723–2730. doi: 10.1016/j.jbiomech.2006.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Talbot LA, Musiol RJ, Witham EK, et al. Falls in young, middle-aged and older community dwelling adults: perceived cause, environmental factors and injury. BMC Public Health. 2005:5. doi: 10.1186/1471-2458-5-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Berg KO, Wood-Dauphinee SL, Williams JI, et al. Measuring balance in the elderly: validation of an instrument. Can J Public Health. 1992;83(Suppl 2):S7–11. [PubMed] [Google Scholar]
- 24.Tinetti ME. Performance-oriented assessment of mobility problems in elderly patients. J Am Geriatr Soc. 1986;34:119–126. doi: 10.1111/j.1532-5415.1986.tb05480.x. [DOI] [PubMed] [Google Scholar]
- 25.Pavol MJ, Runtz EF, Pai YC. Young and older adults exhibit proactive and reactive adaptations to repeated slip exposure. J Gerontol A Biol Sci Med Sci. 2004;59:494–502. doi: 10.1093/gerona/59.5.m494. [DOI] [PubMed] [Google Scholar]
- 26.Myers AM, Powell LE, Maki BE, et al. Psychological indicators of balance confidence: relationship to actual and perceived abilities. J Gerontol A Biol Sci Med Sci. 1996;51:M37–43. doi: 10.1093/gerona/51a.1.m37. [DOI] [PubMed] [Google Scholar]
- 27.Sattin RW. Falls among older persons: a public health perspective. (Review) Annu Rev Public Health. 1992;13:489–508. doi: 10.1146/annurev.pu.13.050192.002421. [DOI] [PubMed] [Google Scholar]
- 28.Camicioli R, Panzer VP, Kaye J. Balance in the healthy elderly: posturography and clinical assessment. Arch of Neurol. 1997;54:976–81. doi: 10.1001/archneur.1997.00550200040008. [DOI] [PubMed] [Google Scholar]
- 29.Wrisley DM, Stephens MJ, Mosley S, et al. Learning effects of repetitive administrations of the sensory organization test in healthy young adults. Arch Phys Med Rehabil. 2007;88:1049–54. doi: 10.1016/j.apmr.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 30.Lin SI, Woollacott M. Association between sensorimotor function and functional and reactive balance control in the elderly. Age Ageing. 2005;34:358–63. doi: 10.1093/ageing/afi089. [DOI] [PubMed] [Google Scholar]
- 31.Bhatt T, Wening JD, Pai Y-C. Adaptive Control of Gait Stability in Reducing Slip-related Backward Loss of Balance. Exp Brain Res. 2006;170:61–73. doi: 10.1007/s00221-005-0189-5. [DOI] [PubMed] [Google Scholar]
- 32.Marigold DS, Patla AE. Strategies for dynamic stability during locomotion on a slippery surface: effects of prior experience and knowledge. J Neurophysiol. 2002;88:339–353. doi: 10.1152/jn.00691.2001. [DOI] [PubMed] [Google Scholar]
- 33.Mansfield A, Peters AL, Liu BA, et al. A perturbation-based balance training program for older adults: study protocol for a randomised controlled trial. BMC Geriatrics. 2007 May 31;7:12. doi: 10.1186/1471-2318-7-12. Online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McIlroy WE, Maki BE. Do anticipatory postural adjustments precede compensatory stepping reactions evoked by perturbation? Neurosci Lett. 1993;164:199–202. doi: 10.1016/0304-3940(93)90891-n. [DOI] [PubMed] [Google Scholar]
- 35.Pai Y-C, Bhatt T. Repeated-Slip Training: An Emerging Paradigm for Prevention of Slip-Related Falls Among Older Adults. Phys Ther. 2007;87:1478–91. doi: 10.2522/ptj.20060326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Thrane G, Joakimsen RM, Thornquist E. The association between timed up and go test and history of falls: the Tromso study. BMC Geriatrics. 2007 Jan 12;7:1. doi: 10.1186/1471-2318-7-1. Online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Coughlin SS. Recall bias in epidemiologic studies.[see comment] J Clin Epidemiol. 1990;43:87–91. doi: 10.1016/0895-4356(90)90060-3. [DOI] [PubMed] [Google Scholar]
- 38.Stel VS, Pluijm SM, Deeg DJ, et al. A classification tree for predicting recurrent falling in community-dwelling older persons. J Am Geriatr Soc. 2003;51:1356–64. doi: 10.1046/j.1532-5415.2003.51452.x. [DOI] [PubMed] [Google Scholar]
- 39.Wolf SL, Sattin RW, Kutner M, et al. Intense tai chi exercise training and fall occurrences in older, transitionally frail adults: a randomized, controlled trial. J Am Geriatr Soc. 1693;51:1693–701. doi: 10.1046/j.1532-5415.2003.51552.x. [DOI] [PubMed] [Google Scholar]
- 40.Cummings SR, Nevitt MC, Kidd S. Forgetting falls: the limited accuracy of recall of falls in the elderly. J Am Geriatr Soc. 1988:36. doi: 10.1111/j.1532-5415.1988.tb06155.x. [DOI] [PubMed] [Google Scholar]
- 41.Zwerling C, Sprince NL, Wallace RB, et al. Effect of recall period on the reporting of occupational injuries among older workers in the Health and Retirement Study. Am J Ind Med. 1995;28:583–90. doi: 10.1002/ajim.4700280503. [DOI] [PubMed] [Google Scholar]