Abstract
Regular monitoring of trends in sexual health and sexual behaviours among adolescents provides strong evidence to guide intervention programs and health policies. Using the province-wide, school-based British Columbia (BC) Adolescent Health Surveys of 1992, 1998, and 2003, this study documented the trends in sexual health and risk behaviours among adolescents in grades 7 to 12 in BC, and explored the associations between sexual behaviours and key risk and protective factors. From 1992 to 2003, the percentage of youth who had ever had sexual intercourse decreased for both males (33.9% to 23.3%) and females (28.6% to 24.3%) and the percentage who used a condom at last intercourse increased for both males (64.4% to 74.9%) and females (52.9% to 64.2%). Among students who had ever had sexual intercourse, the percentage who had first intercourse before age 14 decreased for both sexes. These encouraging results may be related in part to concurrent decreases in the prevalence of sexual abuse or forced intercourse among both male and female adolescents. Protective factors such as feeling connected to family or school were also associated with lower odds of having engaged in risky sexual behaviours. These findings emphasize the importance of including questions about adolescent sexual health behaviours, risk exposures, and protective factors on national and provincial youth health surveys, to monitor trends, inform sexual health promotion strategies and policies, and to document the effectiveness of population-level interventions to foster sexual health among Canadian adolescents.
Introduction
Healthy sexual development is a key developmental task of adolescence, yet to what extent are we tracking either sexual health behaviours or sexual risk behaviours among young people in Canada? In 2001, Maticka-Tyndale called for better, more regularly gathered population-level sexual health data for adolescents, both nationally and provincially, including information about healthy behaviours, not just the vital statistics about outcomes such as births and abortions or sexually transmitted infection (STI) rates. Some of our national surveys of youth have begun including questions related to sexual behaviour, although they may limit that to older adolescents, as does the Health Behaviour of School-Aged Children (Boyce, King, & Roche, 2008), or to a small number of general questions, most commonly whether the teens have ever had sexual intercourse, ever had or caused a pregnancy, and possibly whether they used contraception or condoms at last intercourse. Sexual behaviour questions are a relatively recent addition to national youth surveys, so trends with three or more points of data are not yet available.
Even at the provincial level, very few population-based adolescent surveys ask about sexual behaviour. Some, such as the Student Drug Use Surveys of the Atlantic provinces, have recently included items related to sexual health and risk (Poulin, 2002; Poulin & Elliott, 2007). As with the national surveys, these include a limited number of behavioural items, although the number of questions increased in the 2007 survey compared to 2002.
British Columbia stands out as an exception in sexual health population monitoring of adolescents in Canada. Since 1992, the McCreary Centre Society has conducted the BC Adolescent Health Survey (BC AHS) every 5–6 years throughout the province, and from the beginning, included several questions related to sexual health behaviours, sexual risk behaviours, and sexual health outcomes. At the same time, the BC AHS has included questions about key risk factors for sexual health problems, and a number of protective factors that have been associated with healthy sexual development for adolescents in population-based research in other countries. The BC AHS remains the oldest and largest cluster-stratified population-based provincial adolescent health survey to assess sexual health information for younger and older adolescents in school.
There are frequent media stories sounding the alarm about possible trends in adolescent sexual behaviour, sometimes based on evidence from other countries, rather than Canada; just recently, for example, Maclean’s magazine ran a cover story asking if teen pregnancy is now “cool,” and suggesting that teen parenthood may be on the rise in Canada after decades of decline (Gulli, 2008). Stories regularly seem to imply young people are beginning sexual activity at younger ages, more casually, and with riskier behaviour than previous generations. In the absence of regular monitoring to document trends in sexual health and risk, these perceptions may lead to policies and practice decisions that are not grounded in evidence. Two recent examples where regular population evidence could provide important support for government decision-making are the law to change the legal age of sexual consent from 14 to 16, and the introduction of the new HPV vaccine, with questions about the age at which it should be offered to girls to ensure most of them receive it before becoming sexually active. Equally important is the need to document the effects of such laws and policies after they have been enacted, to ensure they have had their intended effects. Studies have evaluated two Texas laws requiring parental consent for teen access to contraception and abortion, for example, whose aims were to improve parent-teen communication around sexual health decisions, with a goal of reducing unintended pregnancies, sexually transmitted infections (STIs), and abortions (Franzini et al., 2004; Joyce, Kaestner, & Colman, 2006). Texas does not regularly survey youth about relationships with their parents, so the only way to determine whether the policies had the intended effects was to examine the further outcomes the laws were designed to influence, i.e., births, STIs and abortions. Based on these, the laws did not appear to foster communication, but instead delayed youth from accessing timely sexual and reproductive health care; indeed, the studies documented increased rates of second trimester abortions, teen births, and STIs, with an estimated increase in costs of more than $40 million per year to the state of Texas in added health care for these outcomes.
The purpose of this paper is to provide some of the evidence to help inform policies and practices in Canada, by documenting the trends in sexual health and risk behaviour among adolescents in British Columbia since 1992, as well as the link between sexual health behaviours and key risk and protective factors.
Methods
Sample
This secondary analysis explored the BC Adolescent Health Surveys of 1992, 1998, and 2003. The BC AHS is a province-wide cluster-stratified random survey of classrooms in grades 7 through 12 in public schools (Green, 2003; McCreary Centre Society, 2004). The sampling frame included all students enrolled in regular public schools as of September 30th in the school year of each survey. Stratified both by grade and health service delivery area within each of the five health authorities in the province, the sample was drawn from the participating school districts to be representative at the provincial and regional levels. Participation by school districts has improved, albeit slightly, in each year of the survey, with an overall participation rate of about 72–76% depending on year. The sample size for each area was chosen to ensure standard errors of 3.5% or less within strata of grade and region. Classes were over-sampled in those school districts which required signed parental consent, where response rates were lower than for school districts opting for parental notification and student consent (e.g., in 2003, 58% vs. 84%). Between 25% and 33% of school districts opted for signed parental consent in any survey year. In all, more than 72,000 youth have participated in the BC AHS since 1992.
Survey procedures
The approximately 140-item, pencil-and-paper questionnaire was administered by public health nurses and nursing students during a single class period of about 45 minutes. Topics included demographic items, questions related to health experiences and various risk exposures, health and risk behaviours, as well as protective factors or assets in youth’s lives, such as family, school and community connectedness. Items have been drawn from other large-scale adolescent health surveys in Canada and the U.S., as well as a small number of new items developed and pilot-tested for each survey based on community consultation, and evaluated within that round of the survey, as well as with subsequent surveys with out-of-school groups, such as youth in custody, or street-involved youth. Some questions have been added or dropped in each subsequent cycle, to respond to emerging issues, but the majority of the core questions have remained the same to capture trends. Some questions have been modified in subsequent waves, for example, the question about types of contraception used at last intercourse included new methods such as depo provera, emergency contraception, the patch or the ring after they became available in BC. After survey completion, the data were weighted by Statistics Canada consultants to adjust for differential probability of sampling and differential response rates, then scaled to the provincial enrolment. Although boundaries of health regions have shifted slightly over the years, the sampling procedures have ensured representative sampling within participating school districts, which have not changed; in 2003, the 1992 and 1998 samples were re-weighted to the current health service regions to enable trend comparisons. See Table 1 for weighted sample size and demographic information for each year.
Table 1.
Demographics of the BC Adolescent Health Survey each year
| Male | Female | |||||
|---|---|---|---|---|---|---|
| 1992 | 1998 | 2003 | 1992 | 1998 | 2003 | |
| weighted N | 126,256 | 148,704 | 143,858 | 130,550 | 164,516 | 145,554 |
| % gender | 49.2 | 47.5 | 49.7 | 50.8 | 52.5 | 50.3 |
| mean age (years) (95% CI) | 14.9 (14.7–15.2) | 14.8 (14.7–14.9) | 15.0 (15.0–15.1) | 14.8 (14.6–15.1) | 14.8 (14.7–14.9) | 14.9 (14.9–15.0) |
| Age group (%) | ||||||
| 12 to 14 years | 43.9 | 46.0 | 40.7 | 46.2 | 45.3 | 42.7 |
| 15 to 16 years | 32.9 | 33.0 | 34.4 | 32.2 | 32.9 | 34.5 |
| 17+ years | 23.2 | 21.0 | 24.9 | 21.6 | 21.8 | 22.8 |
Measures
For this analysis, measures included demographic variables, i.e., gender and age, as well as items assessing specific sexual health and risk behaviours, such as: ever having sexual intercourse, age at first intercourse, number of lifetime sexual partners, drug or alcohol use before last intercourse, condom use at last intercourse, and effective contraceptive use at last intercourse (i.e., condoms, the pill, depot medroxyprogesterone (depo-provera) or other hormonal methods, diaphragm or other barrier methods). In addition, we report the prevalence of a sexual health outcome, teen pregnancy involvement, for both males and females. We also examined exposures to various types of sexual violence that have been associated with increased odds of sexual risk behaviours, including verbal and physical sexual harassment in the past year, lifetime history of sexual abuse as well as forced sexual intercourse by youth or by adults. Finally, in the 2003 BC AHS, we explored the relationship between key protective factors that have previously been associated with improved sexual health behaviours in the literature, protective factors such as: family and school connectedness; involvement in extracurricular community activities like sports, clubs, the performing arts, or volunteering; and the perception that friends have pro-social attitudes, i.e., a student’s friends would be upset if he or she engaged in antisocial behaviours such as getting arrested, getting into fights, getting drunk, or dropping out of school. More detailed descriptions of the protective factors measures and psychometric evaluations are described elsewhere (Saewyc, Wang, Chittenden, Murphy, & the McCreary Centre Society, 2005; Saewyc et al., in press).
Analysis
All analyses were conducted using the Complex Samples module of SPSS 15.0, which adjusts for the complex cluster-stratified sampling method and weighted data. Analyses were conducted separately by gender, because the prevalence of sexual health behaviours and risk exposures has been shown to vary between male and female adolescents. Analyses included 95% confidence intervals of prevalence estimates of sexual health and risk behaviours and sexual health outcomes, to test trends over time between 1992 and 2003, and 1998 and 2003, calculated using standard errors that were adjusted for the complex sampling. Prevalence estimates and 95% confidence intervals for most behaviours were reported only among sexually experienced youth where indicated. However, in some cases, reporting trends for the entire cohort of grades 7 through 12 can overstate rates among younger teens and understate behaviours among older teens, as sexual behaviours tend to increase with maturation. Therefore, prevalence data are also reported by age, grouped as early adolescence (12 to 14 years), middle adolescence (15–16 years), and older adolescence (17 years and older), corresponding with key developmental stages among most adolescents. We also explored the relationship between sexual behaviours or outcomes and key protective factors, as well as one key risk factor, sexual abuse history; however, because sexual behaviours generally increase with maturation, and sexual abuse and protective factors alter over adolescence as well, we controlled for age, using multivariable logistic regressions to calculate age-adjusted odds ratios and 95% confidence intervals of the odds of ever having sexual intercourse, early first sexual intercourse, pregnancy involvement, and condom use at last intercourse based on the presence or absence of the risk factor or protective factors.
Results
Trends in sexual health and risk behaviours
The trends in sexual health and risk behaviours among adolescent male (Table 2) and female (Table 3) students in British Columbia since 1992 are generally positive. The prevalence of adolescents reporting ever having sexual intercourse has declined significantly for both males and females since 1992, from approximately one in three teens to just under one in four. Similarly, adolescents appear to be waiting longer before first sexual intercourse. Among those who had ever had intercourse, the percent who had done so before the age of 14 declined by almost one half between 1992 and 2003. This may be due in part to declines in sexual abuse, as both males and females also report significantly lower prevalence of sexual abuse history in 2003 compared to a decade earlier; reports of forced intercourse, however, a question which has only been asked since 1998, were unchanged for males and slightly increased among female students. Similarly, sexual harassment remained unchanged for male students, with about one in three reporting unwanted sexual comments, and less than one in five reporting unwanted sexual touching; however, for female students, the percent experiencing unwanted sexual comments did not significantly change, but unwanted sexual touching slightly increased between 1998 and 2003.
Table 2.
Trends among males in prevalence of sexual behaviours and sexual violence/harassment in BC AHS 1992, 1998, and 2003
| 1992 | 1998 | 2003 | ||||
|---|---|---|---|---|---|---|
| % | 95%CI | % | 95%CI | % | 95%CI | |
| Sexual behaviours | ||||||
| Ever had sexual intercourse | 33.9 | (31.0–37.0) | 24.9 | (23.8–26.1) | 23.3 | (22.1–24.6) |
| Early first intercourse (before age 14)a | 42.8 | (37.3–48.6) | 35.8 | (33.0–38.7) | 25.2 | (23.1–27.3) |
| 3 or more lifetime sexual partnersa | 42.6 | (39.8–45.5) | 37.2 | (35.3–39.2) | 39.0 | (36.4–41.6) |
| Substance use before last intercoursea | 27.2 | (25.1–29.4) | 37.4 | (35.1–39.8) | 31.4 | (29.2–33.7) |
| Contraceptive use | ||||||
| Used condoms at last intercoursea | 64.6 | (62.1–67.0) | 65.3 | (63.0–67.4) | 74.9 | (72.8–76.9) |
| Used birth control pills at last intercoursea | 22.5 | (20.8–24.3) | 38.4 | (36.1–40.8) | ||
| Used effective birth control methodsb at last intercoursea | 77.4 | (75.2–79.4) | 86.9 | (85.3–88.4) | ||
| Sexual violence/harassment | ||||||
| Sexual abuse history | 3.6 | (3.1–4.1) | 3.1 | (2.7–3.4) | 2.4 | (2.1–2.8) |
| Forced intercourse history | 1.6 | (1.3–1.9) | 1.9 | (1.6–2.2) | ||
| Unwanted sexual comments in the past year | 34.5 | (33.3–35.6) | 35.5 | (34.4–36.6) | ||
| Unwanted sexual touching in the past year | 17.3 | (16.5–18.2) | 17.6 | (16.6–18.6) | ||
| Pregnancy involvement | ||||||
| Ever caused a pregnancy | 2.3 | (1.9–2.9) | 1.6 | (1.4–1.9) | 1.3 | (1.0–1.7) |
Among youth who have ever had sexual intercourse
“Effective birth control methods” = condoms, birth control pills, depo provera, and/or diaphragm
Table 3.
Trends among females in prevalence of sexual behaviours and sexual violence/harassment in BC AHS 1992, 1998, and 2003
| 1992 | 1998 | 2003 | ||||
|---|---|---|---|---|---|---|
| % | 95%CI | % | 95%CI | % | 95%CI | |
| Sexual behaviours | ||||||
| Ever had sexual intercourse | 28.6 | (25.6–31.7) | 23.0 | (21.6–24.4) | 24.3 | (23.0–25.5) |
| Early first intercourse (before age 14)a | 30.9 | (26.5–35.8) | 23.5 | (21.4–25.9) | 16.0 | (14.4–17.8) |
| 3 or more lifetime sexual partnersa | 35.8 | (32.5–39.2) | 31.8 | (29.7–34.1) | 31.5 | (29.3–33.8) |
| Substance use before last intercoursea | 22.6 | (20.4–25.0) | 29.2 | (27.0–31.5) | 26.4 | (24.4–28.4) |
| Contraceptive use | ||||||
| Used condoms at last intercoursea | 52.9 | (49.8–56.0) | 52.6 | (50.4–54.8) | 64.2 | (62.1–66.3) |
| Used birth control pills at last intercoursea | 30.6 | (28.4–32.9) | 44.8 | (42.3–47.4) | ||
| Used effective birth control methodsb at last intercoursea | 75.7 | (73.6–77.7) | 86.6 | (85.4–88.0) | ||
| Sexual violence/harassment | ||||||
| Sexual abuse history | 20.8 | (19.1–22.5) | 14.7 | (13.9–15.5) | 12.6 | (11.9–13.4) |
| Forced intercourse history | 4.9 | (4.4–5.5) | 6.1 | (5.6–6.7) | ||
| Unwanted sexual comments in the past year | 54.0 | (52.7–55.3) | 52.8 | (51.5–54.1) | ||
| Unwanted sexual touching in the past year | 35.6 | (34.5–36.7) | 38.4 | (37.1–39.7) | ||
| Pregnancy involvement | ||||||
| Ever caused a pregnancy | 2.9 | (2.2–3.9) | 2.0 | (1.7–2.4) | 1.5 | (1.3–1.8) |
Among youth who have ever had sexual intercourse
“Effective birth control methods” = condoms, birth control pills, depo provera, and/or diaphragm
Some sexual behaviours increase the risk of unintended pregnancy and STIs. Among students in BC who have ever had sexual intercourse, the percentage who reported three or more lifetime sexual partners was not significantly changed over the time period for either male or female students, with approximately one in three sexually active students reporting they have had three or more partners, and males slightly more likely than females to report having done so. The percentage of students who used drugs or alcohol before last intercourse increased significantly between 1992 and 1998, then declined significantly between 1998 and 2003; overall, the rates were unchanged, as about one in three males (Table 2) and one in four females (Table 3) reported substance use before last intercourse.
In contrast to sexual risk behaviours, sexual health behaviours generally showed significant improvement between 1992 and 2003. For both male and female students, condom use at last intercourse significantly increased over the decade, with a 16% increase for males, and a 21% increase for females. The use of birth control pills increased between 1998 and 2003, as did the use of any form of effective birth control at last intercourse, such as condoms or other barrier methods, or hormonal contraception such as birth control pills or depot medroxyprogesterone injections (in 1992, the question was worded differently, so comparisons may not be reliable, and are not reported here).
Unintended pregnancy, whether it is unwanted or mistimed, can pose a significant health burden at any age, and thus could be considered a negative sexual health outcome. Although the BC Adolescent Health Surveys do not assess pregnancy intentions, they do ask whether a teen has been pregnant one or more times (for males, if they have caused a pregnancy one or more times). Adolescent pregnancy involvement also significantly declined by nearly half between 1992 and 2003, for both males (Table 2) and females (Table 3).
Age influences on sexual health and risk behaviours
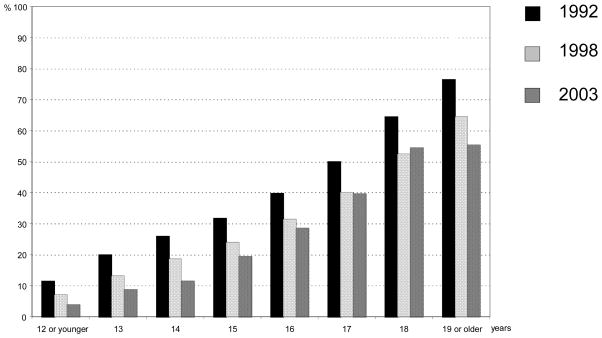
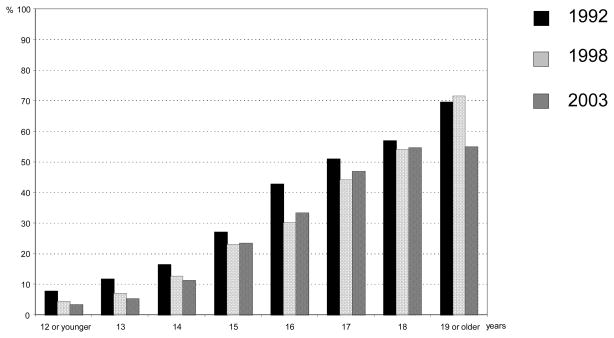
Sexual development accelerates during the adolescent years, and in general, the prevalence of sexual health and risk behaviours increases with age among young people. As a result, the preceding reports of prevalence data for an entire cohort, although useful for tracking trends, can overstate rates among younger teens and understate behaviours among older teens. The clearest example is the percent of youth who have ever had intercourse, which increased with age for males (Fig. 1) and females (Fig. 2) in all three surveys. Table 4 outlines the prevalence of select health and risk behaviours and sexual health outcomes across three age groups of adolescents: early adolescence (age 12 to 14), middle adolescence (15 and 16 years), and older adolescence (17 years and older). These results are reported for BC AHS 2003 only, as the results for previous years of the surveys are quite similar. As would generally be expected, very few younger adolescents reported sexual intercourse, with 7.2% of all female respondents and 8.9% all male respondents age 12 to 14 reporting ever having sex compared to 49.4% of females and 45.1% males age 17 or older. Similarly, the youngest adolescents were far less likely than the oldest to have had pregnancy involvement; 0.4% of females age 12 to 14 compared to 3.8% for females age 17 or older reported pregnancy involvement, comparable values for males were 0.7% and 2.6%. Experience of sexual abuse and/or forced sexual intercourse was more common among older than younger teens of both genders, which is a reminder that vulnerability to sexual violence is not limited to childhood and early adolescence. Females were strikingly more likely than males to have had these experiences, particularly in the case of sexual abuse, which was 4–6 times more common in females than males, depending on the age group (Table 4).
Figure 1.
Age trends in prevalence of sexual intercourse by year, male students, BC AHS
Figure 2.
Age trends in prevalence of sexual intercourse by year, female students, BC AHS
Table 4.
Prevalence among all respondents of sexual health and risk behaviours by age and gender, BC AHS 2003
| Behaviours by gender (%) | 12 to 14 years | 15 to 16 years | 17+ years |
|---|---|---|---|
| Ever had sexual intercourse | |||
| Males | 8.9 | 24.2 | 45.1 |
| Females | 7.2 | 28.5 | 49.4 |
| Pregnancy involvement | |||
| Males | 0.7 | 1.1 | 2.6 |
| Females | 0.4 | 1.3 | 3.8 |
| Early first intercourse (before 14) | |||
| Males | 6.2 | 4.8 | 6.1 |
| Females | 4.5 | 3.7 | 2.8 |
| Ever been sexually abused | |||
| Males | 2.0 | 2.3 | 3.2 |
| Females | 9.0 | 14.4 | 16.9 |
| Forced to have sexual intercourse | |||
| Males | 1.1 | 2.0 | 3.0 |
| Females | 3.9 | 6.7 | 9.3 |
Some of the sexual health-related behaviours of students who had ever had intercourse (Table 5) do not appear to differ by age or gender. Having multiple sexual partners in the past year, for example, did not vary by age, with just under half of males and around 40% of females who have ever had sexual intercourse in each age group reporting more than one partner in the past year. Alcohol or drug use with last intercourse increased sharply for males in middle adolescence, then levelled off, while alcohol or drug use with intercourse for females was highest among younger teens, and declined steadily with age. Contraceptive use was another area of age and gender difference; condom use at last intercourse showed the highest rate among middle adolescent males, while condom use was highest among the youngest sexually active females, and declined with age. In contrast, the use of birth control pills increased steadily by age group for both males and females.
Table 5.
Prevalence among respondents who have ever had sexual intercourse of sexual health and risk behaviours by age and gender, BC AHS 2003
| Behaviours by gender (%) | 12 to 14 years | 15 to 16 years | 17+ years |
|---|---|---|---|
| Used alcohol or drugs at last intercourse | |||
| Males | 23.9 | 32.6 | 32.8 |
| Females | 38.5 | 24.6 | 19.8 |
| More than 1 sexual partner in the past year | |||
| Males | 45.5 | 44.5 | 46.2 |
| Females | 38.5 | 40.6 | 38.5 |
| Used condoms at last intercourse | |||
| Males | 72.3 | 77.7 | 69.8 |
| Females | 78.2 | 68.3 | 54.7 |
| Used birth control pills at last intercourse | |||
| Males | 23.2 | 37.2 | 43.6 |
| Females | 26.3 | 45.0 | 49.3 |
| Used effective contraceptive methods at last intercourse | |||
| Males | 75.9 | 89.8 | 88.1 |
| Females | 83.1 | 87.6 | 87.0 |
Key risk and protective factors and sexual health
History of sexual abuse/forced sexual intercourse
One of the key risk exposures for adolescent and adult sexual health problems is the experience of sexual violence. A history of sexual abuse or sexual assault has been linked to early first intercourse, difficulty negotiating contraception and thus increased risks for unprotected intercourse, and adolescent pregnancy involvement (Saewyc, Magee, & Pettingell, 2004). To determine the link between a history of sexual abuse and/or forced intercourse and the likelihood of ever having sex, early first intercourse, teen pregnancy involvement, and lack of condom use at last intercourse, we calculated odds ratios of these behaviours, adjusted for age. As shown in Table 6, both male and female students who have experienced sexual abuse and/or forced intercourse are up to four times more likely to have ever had sexual intercourse, and twice as likely to have begun having sexual intercourse before age 14 compared to teens their same age and gender in the 2003 cohort. Similarly, they are up to four times more likely to have ever been pregnant or caused a pregnancy. Males who have experienced sexual violence are half as likely to have used a condom at last intercourse, while females who have experienced sexual violence are 20% less likely than their non-abused peers to have used a condom.
Table 6.
Age-adjusted odds ratios (AOR) comparing sexual behaviours and pregnancy involvement by history of sexual abuse/forced sexual intercourse in BC AHS 2003
| Ever had sexual intercourse | Pregnancy involvementa | Early first intercoursea | Condom use at last intercoursea | |||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | |
| Male | 4.17 | (3.22–5.38)** | 4.36 | (2.58–7.36)** | 1.98 | (1.36–2.87)** | 0.50 | (0.34–0.73)** |
| Female | 3.72 | (3.24–4.27)** | 3.58 | (2.45–5.24)** | 2.47 | (1.94–3.15)** | 0.80 | (0.67–0.96)* |
Reference group: no history of sexual abuse or forced sexual intercourse
p < 0.05,
p < 0.01
Among youth who have ever had sexual intercourse
Family, school, and social assets as protective factors
A variety of youth assets or protective factors were also assessed in the BC AHS of 2003, and Table 7 shows the age-adjusted odds ratios (AOR) of the various sexual behaviours with the presence or absence of the protective factors. Scores for family connectedness, school connectedness, and perceived pro-social peer attitudes were standardized on a 0 to 1 scale, such that the age-adjusted odds ratios in Table 7 reflect comparisons between the highest levels and the lowest levels on each of the scales, to allow them to be compared more easily with dichotomous protective factors. For example, among adolescent males, those with the highest family connectedness were 77% less likely to have ever had sex (AOR = 0.23), just over half as likely to have sex before age 14 (AOR = 0.48), and about 85% less likely to have caused a pregnancy (AOR = 0.16) than same-age peers with the lowest family connectedness. Family connectedness shows an equally strong relationship for females, with lower odds of ever having sex, early first intercourse, and teen pregnancy among females with the highest family connectedness compared to females the same age with the lowest family connectedness (Table 7). School connectedness, or the extent to which students feel a part of their school and cared about by teachers, also reduces the odds of sexual activity, early first intercourse, and teen pregnancy for both male and female students. Having friends who have attitudes against most risky behaviours lowers the odds a teen will report ever having sexual intercourse, first sexual intercourse before age 14, or teen pregnancy involvement. None of these protective factors, however, were related to condom use at last intercourse among adolescents who had ever had sexual intercourse.
Table 7.
Age-adjusted odds ratios (AOR) examining relationships between protective factors, sexual behaviours and pregnancy involvement in BC AHS 2003
| Ever had sexual intercourse | Pregnancy involvementa | Early first intercoursea | Condom use at last intercoursea | |||||
|---|---|---|---|---|---|---|---|---|
| AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | |
| Male | ||||||||
| Family connectedness (score, 0–1) | 0.23 | (0.17–0.31)** | 0.16 | (0.07–0.37)** | 0.48 | (0.28–0.82)** | 1.04 | (0.57–1.89) |
| School connectedness (score, 0–1) | 0.11 | (0.09–0.15)** | 0.18 | (0.09–0.37)** | 0.24 | (0.12–0.47)** | 1.55 | (0.89–2.70) |
| Perceived prosocial peer attitudes(score, 0–1) | 0.23 | (.019–0.27)** | 0.37 | (0.16–0.85)* | 0.42 | (0.26–0.67)** | 1.20 | (0.82–1.76) |
| Volunteering in the past year (yes/no) | 0.83 | (0.72–0.95)** | 0.68 | (0.44–1.05) | 0.79 | (0.59–1.05) | 1.02 | (0.80–1.29) |
| Weekly supervised extracurricular activities in the past year (yes/no) | 1.06 | (0.95–1.19) | 0.92 | (0.58–1.46) | 0.83 | (0.60–1.15) | 1.06 | (0.82–1.37) |
| Female | ||||||||
| Family connectedness (score, 0–1) | 0.08 | (0.06–0.11)** | 0.20 | (0.09–.044)** | 0.45 | (0.23–0.86)* | 1.01 | (0.61–1.67) |
| School connectedness (score, 0–1) | 0.07 | (0.05–0.10)** | 0.07 | (0.03–0.17)** | 0.30 | (0.14–0.61)** | 1.55 | (0.91–2.62) |
| Perceived prosocial peer attitudes (score, 0–1) | 0.08 | (0.06–0.09)** | 0.18 | (0.07–0.44)** | 0.44 | (0.26–0.76)** | 1.28 | (0.82–1.99) |
| Volunteering in the past year (yes/no) | 0.67 | (0.57–0.78)** | 0.52 | (0.33–0.81)** | 0.85 | (0.61–1.17) | 1.22 | (0.96–1.55) |
| Weekly supervised extracurricular activities in the past year (yes/no) | 0.72 | (0.64–0.81)** | 0.67 | (0.46–0.97)* | 0.70 | (0.54–0.90)** | 1.38 | (1.13–1.70)** |
p < 0.05,
p < 0.01
Among youth who have ever had sexual intercourse
Two other factors showed inconsistent relationships with sexual health behaviours. Volunteering in the past year was associated with lower odds that male and female students had ever had sexual intercourse, but among females only, those who volunteered were half as likely to have ever been pregnant. Involvement in extracurricular activities that included adult supervision—i. e., sports with a coach, clubs and youth groups, music or arts classes, and dance or aerobic classes—were associated with significantly lower odds of ever having sexual intercourse, early first intercourse, and teen pregnancy for females, and significantly higher odds that sexually active females reported using a condom at last intercourse. In contrast, supervised extracurricular activities among males were not related to any sexual health behaviours.
Discussion
According to results of the BC Adolescent Health Surveys from 1992 to 2003, youth are taking fewer sexual health risks than youth 5–10 years earlier, and many youth are waiting longer to have sex. The proportion of sexually active female students who have had sex before age 14 has dropped by nearly half since 1992, with a similar decline seen among male students. In addition, the rate of self-reported pregnancies declined. This self-report is data supported by declining birth and abortion rates among BC adolescents (Statistics Canada, 2007). In contrast, there were no changing trends in sexual activity reported between 2002 and 2006 in the World Health Organizations’s Health Behaviour in School-Aged Children (HBSC) survey for Canada (Boyce, King, & Roche, 2008). It should be noted that the HBSC survey only asks sexual behaviour questions of students in grades 9 and 10, there are only two data years rather than the three needed to establish trends, and the sample is not large enough to calculate reliable provincial estimates.
Not only are youth in BC waiting longer to become sexually active, but once active, more youth are practising safer sex. Condom use at last intercourse has increased 16–21% for males and females, respectively, with the majority of adolescents using condoms. Concerns about younger adolescents lacking the maturity to engage in responsible sexual practices may be unfounded, as the youngest females who were sexually active reported the highest prevalence of condom use, and younger males were just as likely as older teens to use condoms at last intercourse. The 2006 HBSC (Boyce et al., 2008) shows equally high rates of condom use among youth, and a similar pattern of younger girls reporting higher condom use than older girls. Among older teens, other forms of contraception are increasingly adopted. These two contraceptive patterns may be complementary: as youth develop longer term intimate relationships, they may switch to the more reliable hormonal methods for preventing pregnancy, and decrease their reliance on condoms. As with condom use, rates of birth control pills and other effective methods of contraception are significantly higher among sexually active students in 2003 than in 1992.
What helps explain these improvements in sexual health behaviours? Although school-based monitoring surveys seldom have room to include numerous questions about the various influences that could contribute to healthier development for young people, there is one measure the BC AHS assesses that may have played a role. Improvements in sexual health behaviours may be due in part to significant declines in sexual violence which has been associated with sexual health risks (Saewyc, Magee, & Pettingell, 2004). The rates of teens reporting a history of sexual abuse declined by a third among females, and by half among males. At the same time, the two most recent surveys (1998 and 2003) show unchanged rates of forced intercourse and physical sexual harassment for males, and increasing rates for females. Such preliminary trends in sexual violence are concerning, as they may suggest a turnaround in more serious exposures to sexual violence in future years. Population-level sexual violence prevention initiatives may be an important strategy to continue to improve sexual health among adolescents.
Protective factors in youth’s lives, such as supportive schools and families, and opportunities for community involvement, were also associated with positive sexual health outcomes. We were unable to assess trends in protective factors to date, as most of the measures were only included in the more recent BC AHS. Similar connections between family and school relationships and sexual activity have been documented in other countries, including through longitudinal studies; in Canada, these same relationships were noted for students on the 2006 HBSC (Boyce et al., 2008). The extent to which young people have increasing opportunities for supportive relationships, friends with healthy attitudes, and positive engagement in their schools and communities, may also help explain improving trends in sexual health, although such trends will need to be assessed in future cohorts.
There is still room for improvement, as more than one in 10 sexually active youth did not use effective contraception at last intercourse, and the decline in condom use as older teens switch to hormonal methods reduces their protection against STIs. As well, the number of sexual partners and rates of alcohol and drug use before sex are unchanged for both males and females. Even so, the trends are encouraging, and should reassure adults and young people alike that media portrayals of increasingly risky adolescent sexual behaviours at ever younger ages are not supported by the evidence, at least among high school students in British Columbia, and possibly in Canada.
Strengths and limitations
As with all studies, there are strengths and limitations to this research that should be taken into account when considering these findings. One of the key strengths is the nature of the large-scale, provincially-representative cluster-stratified sample of youth in public schools in British Columbia; it includes youth from all but the most remote regions of BC, from early adolescence through grade 12. There are groups who may not be represented by these data; however, youth who are not attending school, such as homeless and street-involved youth, may have different rates of sexual experience and risk exposures than the general population of youth in school (Smith, Saewyc, Albert et al., 2007). At the same time, a recent survey of 762 street-involved youth age 12–18 in nine communities in BC found two-thirds of the youth were attending school, a third of them in mainstream schools and the remainder in alternate education programs (Smith et al., 2007), which suggests the school-based surveys may be more representative of the general population of high-school aged youth than expected. On the other hand, youth in ESL and special education programs within the public schools, youth in private schools, in alternate education programs, or in custody centres also were not included in this survey. Sub-populations of young people within the BC school population, such as Aboriginal youth, or lesbian, gay and bisexual adolescents, may report different trends in sexual behaviours, and different levels of related risk and protective factors (van der Woerd, Dixon, McDiarmid et al., 2005; Saewyc et al., 2006; Devries, Free, Morrison, & Saewyc, in press; Saewyc, Homma, Skay et al., in press).
The trends are reported for cross-sectional cohorts in time, not longitudinal results from the same students; therefore, the links between risk and protective factors can only suggest relationships, not directly identify causes of these trends. Similarly, these data are self-reported; younger students, those with learning disabilities, and those who speak English as a second language may not understand the questions and response options as readily as older, sexually experienced students, and this may contribute to some error in prevalence estimates. Equally, these are results for a single province, and may not represent the behavioural trends among youth in other provinces and territories of Canada. However, this is one of the few recurring large-scale population-based surveys of youth in Canada that includes questions about sexual health, risk exposures such as sexual violence, and protective factors; the co-occurring declining trends in teen births and abortions from vital statistics sources, and the relatively similar patterns in the more limited national survey data, help support the reliability of these results.
Conclusions and recommendations
Adolescent students in British Columbia public schools in 2003 reported better sexual health and healthier sexual behaviours than their peers over the previous decade. Fewer were having sex at young ages, and the majority of those who are sexually active were engaging in responsible behaviours to protect their health and prevent unintended pregnancy. These improving trends may be related to declines in sexual violence, as well as to protective factors in teens’ lives, such as family and school connectedness. Other provinces may wish to consider the regular monitoring of sexual behaviours, risk exposures and protective factors among their adolescent populations, in order to counteract widespread misperceptions of the state of sexual health among young Canadians, and to provide evidence for informing sexual health promotion strategies and appropriate policies.
Acknowledgments
Analyses for this paper were funded in part by a CIHR/PHAC Research Chair in Applied Public Health (Saewyc), from the CIHR Institutes of Population & Public Health, Human Development, Child & Youth Health, as well as the Public Health Agency of Canada. The paper was also supported in part by a Michael Smith Foundation for Health Research Scholar award (Saewyc). The authors would like to acknowledge the McCreary Centre Society as the source of the BC Adolescent Health Surveys of 1992, 1998, and 2003 that were used in this paper.
References
- Boyce WF, King MA, Roche J. Healthy Settings for Young People in Canada. Ottawa, ON: Public Health Agency of Canada; 2008. Available electronically at www.phac-aspc.gc.ca. [Google Scholar]
- Devries K, Free C, Morrison L, Saewyc E. Factors associated with sexual behaviour of Aboriginal youth: Implications for health promotion. American Journal of Public Health. doi: 10.2105/AJPH.2007.132597. (In press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franzini L, Marks E, Cromwell PF, Risser J, McGill L, Markham C, et al. Projected economic costs due to health consequences of teenager’ loss of confidentiality in obtaining reproductive health care services in Texas. Archives of Pediatrics and Adolescent Medicine. 2004;158:1140–1146. doi: 10.1001/archpedi.158.12.1140. [DOI] [PubMed] [Google Scholar]
- Gulli C. Suddenly teen pregnancy is cool? For the first time in years, more kids are having kids—and not just in the movies. Maclean’s. 2008 Jan 17 [Google Scholar]
- Joyce T, Kaestner R, Colman S. Changes in abortions and births and the Texas Parental Notification Law. The New England Journal of Medicine. 2006;354:1031–1038. doi: 10.1056/NEJMsa054047. [DOI] [PubMed] [Google Scholar]
- Maticka-Tyndale E. Sexual health and Canadian youth: How do we measure up? The Canadian Journal of Human Sexuality. 2001;10:1–17. [Google Scholar]
- Poulin C. Nova Scotia Student Drug Use 2002: Technical Report. 2002 Available at www.gov.ns.ca/hpp/addictionPrevention.html#reports.
- Poulin C, Elliott D. Student Drug Use Survey in the Atlantic Provinces 2007. Technical Report. 2007 Available at www.gov.ns.ca/hpp/addictionPrevention.html#reports.
- Saewyc EM, Homma Y, Skay CL, Bearinger L, Resnick M, Reis E. Protective factors in the lives of bisexual adolescents in North America. American Journal of Public Health. doi: 10.2105/AJPH.2007.123109. (In press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saewyc EM, Magee LL, Pettingell SE. Teenage pregnancy and associated risk behaviors among sexually abused adolescents. Perspectives on Sexual and Reproductive Health. 2004;36:98–105. doi: 10.1363/psrh.36.98.04. [DOI] [PubMed] [Google Scholar]
- Saewyc E, Richens K, Skay CL, Reis E, Poon C, Murphy A. Sexual orientation, sexual abuse, and HIV-risk behaviors among adolescents in the Pacific Northwest. American Journal of Public Health. 2006;96:1104–1110. doi: 10.2105/AJPH.2005.065870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saewyc E, Wang N, Chittenden M, Murphy A the McCreary Centre Society. Building Resilience in Vulnerable Youth. Vancouver, BC: McCreary Centre Society; 2006. Available electronically at www.mcs.bc.ca. [Google Scholar]
- Smith A, Saewyc E, Albert M, MacKay L, Northcott M the McCreary Centre Society. Against the Odds: A Profile of Marginalized and Street-Involved Youth in BC. Vancouver, BC: McCreary Centre Society; 2007. Available electronically at www.mcs.bc.ca. [Google Scholar]
- Statistics Canada. Births 2005. 2007 Catalogue no. 84F0210. Available from http://www.statcan.ca/english/pub/index.htm.
- van der Woerd KA, Dixon BL, McDiarmid T, Chittenden M, Murphy A The McCreary Centre Society. Raven’s Children II: Aboriginal Youth Health in BC. Vancouver, BC: The McCreary Centre Society; 2005. Available electronically at www.mcs.bc.ca. [Google Scholar]